Abstract
Ribociclib is an orally bioavailable, selective cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitor. CDK4/6 inhibition by ribociclib leads to retinoblastoma tumor suppressor protein (Rb) reactivation, thereby restoring Rb-mediated cell cycle arrest. Ribociclib is approved for the treatment of patients with hormone receptor-positive/human epidermal growth factor receptor-2-negative (HR+/HER2−) advanced breast cancer (ABC), at the dose of 600 mg once daily (QD) during cycles of 21 days on/7 days off, with optional dose reduction to 400 mg and 200 mg. Ribociclib is rapidly absorbed with a median time to reach maximum plasma concentration of 2.4 h, mean half-life of 32.0 h and oral bioavailability of 65.8% at 600 mg. It is eliminated mainly by hepatic metabolism (~ 84% of total elimination), mostly by cytochrome P450 (CYP) 3A4. Age, body weight, race, baseline Eastern Cooperative Oncology Group status, food, mild hepatic impairment, mild-to-moderate renal impairment, proton pump inhibitors, and combination partners (non-steroidal aromatase inhibitors or fulvestrant) have no clinically relevant impact on ribociclib exposure. Ribociclib inhibits CYP3A at 600 mg leading to increased exposure of CYP3A substrates. Strong CYP3A inhibitors or inducers increase or decrease, respectively, ribociclib exposure. Exposure-safety and exposure-efficacy analyses support the clinical benefit of the 600 mg QD starting dose, with potential individualized dose reductions to 400 mg and 200 mg for effective management of the adverse events neutropenia and QTcF interval prolongation, while maintaining efficacy, in patients with HR+/HER2− ABC. Overall, these clinical pharmacology data informed ribociclib dose justification and clinical development, as well as its prescribing information for clinical use in advanced breast cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This review comprehensively discusses the clinical pharmacokinetics, pharmacodynamics and clinical pharmacology data of ribociclib, a CDK4/6 inhibitor approved worldwide (in combination with endocrine therapy) as first- and second-line treatment for pre-/peri- and postmenopausal women and men with HR+, HER2− advanced breast cancer. |
The data support the use of ribociclib in this patient population at the recommended dose regimen of 600 mg daily (3 weeks on/1 week off), with no dose adjustments required based on age, body weight, race, combination partner (NSAIs or fulvestrant), food intake, proton pump inhibitors, or the presence of mild-to-moderate renal impairment or mild hepatic impairment. |
Individualized dose reductions are warranted by medical necessity, such as moderate-to-severe hepatic impairment or severe renal impairment, concomitant use of a strong CYP3A inhibitor, or for the management of neutropenia and QTcF interval prolongation and have been shown not to compromise efficacy. |
1 Introduction
Breast cancer is the most common malignancy among women worldwide, accounting for an estimated 24–29% of all cancers and an estimated 15% of all cancer deaths in females [1, 2]. The most common breast cancer subtype (approximately 67%) is the hormone receptor–positive (HR+; comprising estrogen receptor-positive [ER+] and/or progesterone receptor-positive [PR+]), human epidermal growth factor receptor-2-negative (HER2−) subtype [3, 4]. Globally, between 3 and 25% of breast cancer patients are diagnosed with de novo metastatic disease (advanced or metastatic breast cancer, thereafter, abbreviated as ABC) [5, 6]. Furthermore, among those diagnosed with early stage HR+ breast cancer, between 13 and 41% will experience cancer recurrence within 20 years, despite treatment [7].
In postmenopausal patients or premenopausal patients receiving ovarian ablation or suppression with HR+/HER2− recurrent unresectable or stage IV disease, the preferred first-line systemic treatment option involves endocrine therapy (targeting hormone receptors, e.g., non-steroidal aromatase inhibitors [NSAI] such as letrozole or anastrozole, or selective estrogen receptor down-regulators such as fulvestrant) combined with an inhibitor of cyclin-dependent kinase 4 and/or 6 (CDK4/6), based on the National Comprehensive Cancer Network® (NCCN®) and the European Society For Medical Oncology (ESMO) [8, 9].
The rationale for targeting hormone receptors as well as CDK4/6 is that both factors play key roles in tumors that are driven by estrogen. Progression from the G1 to the S-phase of the cell cycle is regulated by cyclin D, which is a transcriptional target of the estrogen receptor. In normal cells, mitogenic stimuli lead to an increase in cyclin D levels and association of cyclin D with CDK4 or CDK6. The resulting cyclin D–CDK4/6 complex phosphorylates and inactivates the retinoblastoma tumor suppressor protein (Rb), thereby relieving Rb-mediated repression of transcription factors of cell cycle progression. In breast cancer, cyclin D1 is overexpressed in approximately half of all cases, and hence endocrine therapy aims to block transcriptional activity of the estrogen receptor. On the other hand, CDK4/6 inhibitors lead to reactivation of Rb, thereby allowing to restore Rb-mediated cell cycle arrest. Furthermore, because CDK4/6 activation has also been associated with resistance to endocrine therapy, CDK4/6 inhibitors may delay the development of resistance [10, 11].
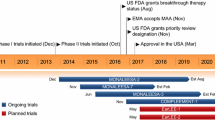
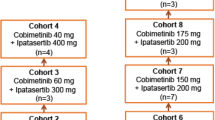
Ribociclib (LEE011; Kisqali®) is an orally bioavailable, highly selective, small-molecule, dual inhibitor of the CDK4/cyclin-D1 and CDK6/cyclin-D3 enzyme complexes. Ribociclib-based combinations are approved worldwide for the first- and second-line treatment of pre-/peri- and post-menopausal women with HR+, HER2− ABC, with a recommended starting dose of 600 mg once daily (QD) for 21 consecutive days, followed by 7 days off treatment, with an option of dose reductions to 400 mg QD or 200 mg QD based on the individual safety and tolerability [12, 13]. Approval of ribociclib was based on the three pivotal Phase 3 studies MONALEESA-2 (NCT01958021; ribociclib plus letrozole as first-line therapy in post-menopausal women [14,15,16]), MONALEESA-3 (NCT02422615; ribociclib plus fulvestrant as first- or second-line therapy in post-menopausal women [17,18,19]), and MONALEESA-7 (NCT02278120; ribociclib plus goserelin and either letrozole or anastrozole as first-line therapy in pre-menopausal women [20,21,22]). The MONALEESA-7 trial also assessed the combination of ribociclib plus goserelin and tamoxifen [20,21,22]. In all three trials, combinations of ribociclib plus endocrine therapy demonstrated significantly prolonged progression-free survival (PFS, primary endpoint), with a 41–45% lower risk of progression or death compared with endocrine therapy alone (median follow-up of 19.2–26.4 months) [15, 17, 20]. Furthermore, across all the three trials, ribociclib plus endocrine therapy demonstrated a significant overall survival (OS) benefit, with a reduced risk of death ranging from 24–27% compared with endocrine therapy alone (median follow-up of 4.5–6.6 years) [16, 19, 22]. Based on these findings, the National Comprehensive Cancer Network (NCCN) guidelines now differentiates ribociclib as the only category 1 preferred first-line treatment option in combination with an AI for post-menopausal patients or pre-menopausal patients receiving ovarian ablation or suppression with HER2−, ER+/or PR+ recurrent unresectable (local or regional) or Stage IV (M1) disease [9]. Most recently, evidence has also become available for ribociclib plus ET as adjuvant treatment after surgery and adjuvant chemotherapy in patients with HR+/HER2− early breast cancer (BC), showing a significant improvement versus standard ET alone in invasive disease-free survival (NATALEE study) [23].
Neutropenia was the most frequent adverse event (AE) in the 3 MONALEESA trials (all grade: 71.6–77.3%; grade 3/4: 57.1–63.6%) and accounted for the majority of dose reductions in patients [18, 21, 24]. Ribociclib has also been shown to prolong the QT interval in a small percentage of patients with minimal contribution to dose reduction [17, 18, 21, 24]. However, both neutropenia and QT interval prolongation associated with ribociclib treatment are reversible and dose dependent, and can be managed with dose modifications for patients [12, 13].
Here, we review the clinical pharmacokinetics (PK), pharmacodynamics (PD), and clinical pharmacology data for ribociclib from a range of studies assessing ribociclib as single agent or in combination with endocrine therapy in subjects with or without cancer, which supported the successful clinical development of ribociclib and informed its use in clinical practice in patients with HR+, HER2− ABC (Supplementary Table 1).
2 Biopharmaceutical Properties and Preclinical Pharmacology
2.1 Biopharmaceutical Properties and Formulation
Ribociclib is an orally bioavailable, small-molecule compound, that is formulated as a succinate salt, with a molecular mass of 434.55 g/mol (free base) [12, 13]. Ribociclib succinate is a weak base, and as such its solubility in aqueous media decreases with increasing pH (> 2.4 mg/mL at pH up to 4.5; 0.3 mg/mL at pH 7.5) [25]. In vitro, ribociclib showed moderate permeability in Caco-2 cell monolayers, and high passive permeability in human hepatocytes [26]. In media simulating intestinal fluids, ribociclib retains high solubility regardless of pH (> 2.2 mg/mL at pH 5.0 and > 2.4 mg/mL at pH 6.5 in media simulating fed and fasted stomach conditions, respectively) [25], and simulations using clinical PK data indicate rapid, complete dissolution in the human stomach without intestinal precipitation and with permeation-controlled absorption [27].
Ribociclib is currently marketed as a film-coated tablet formulation, whereas a capsule formulation was used in most clinical studies in patients with cancer or ABC. Bioequivalence between the capsule and film-coated tablet formulations was established [27], supporting the commercial use of the tablet formulation.
2.2 Preclinical Pharmacology
Ribociclib is a highly selective dual inhibitor of the CDK4/cyclin-D1 and CDK6/cyclin-D3 enzyme complexes, with 50% inhibitory concentrations (IC50) of 0.01 μM and 0.039 μM, respectively [28, 29]. Inhibition of these complexes is mediated by binding of ribociclib to the ATP cleft of the CDK4 and CDK6 kinases [10]. In Rb-positive preclinical tumor models, ribociclib demonstrated complete dephosphorylation of Rb, in line with its mode of action as a CDK4/6 inhibitor (Fig. 1), as well as dose-dependent G1 cell cycle arrest and tumor regression [28, 29]. The impact of ribociclib tumor growth reduction was also assessed by immuno-histochemistry of nuclear protein Ki67 (Ki67) [30], a nuclear marker of active cell proliferation in normal and tumor cell populations [31]. In mouse xenograft models derived from CDK4/6-overexpressing cell-lines, ribociclib treatment resulted in reduced Ki67 staining and impaired cell proliferation, together with diminished Rb phosphorylation [30]. In a preclinical study of 50 breast cancer cell lines, ribociclib demonstrated inhibitory activity predominantly against ER+ cell lines, suggesting that ER+ breast cancer cells might be particularly susceptible to CDK4/6 inhibition [10], and in four mouse xenograft models of HR+ breast cancer, significant tumor growth inhibition was observed with single-agent ribociclib [28, 29, 32]. The addition of letrozole or fulvestrant to ribociclib further increased the tumor growth inhibition compared with single agent in mouse xenograft models of HR+ breast cancer [28, 29, 32].
Mode of action of ribociclib-based combination therapy [10, 11, 13]. A In normal cells, external growth stimuli, including estradiol, lead to stimulation of the estrogen receptor, which in turn leads to an increase in levels of cyclin D, thereby promoting formation of the cyclin D/CDK4/6 complex and activation of CDK4/6. The cyclin D/CDK4/6 complex phosphorylates (indicated with a star) and inactivates the Rb tumor suppressor, thereby relieving Rb-mediated repression of the E2F transcription factor (indicated with X). Activation of E2F leads to S phase entry and cell cycle progression. In normal cells, this pathway leads to controlled cell growth, but in cancer cells, this pathway is overactive leading to uncontrolled cell division and growth. B In the treatment of breast cancer, the rationale for combining endocrine therapy and a CDK4/6 inhibitor such as ribociclib is to achieve dual blocking of the estrogen receptor signaling pathway, and hence enhance anti-tumor activity, to stop uncontrolled tumor cell division and growth. Endocrine therapy targets the estrogen receptor and prevents Cyclin D level increase, whereas CDK4/6 inhibitors such as ribociclib block CDK4/6, thereby preventing Rb phosphorylation and restoring Rb-mediated repression of the E2F transcription factor. As a result, ribociclib treatment leads to cell cycle arrest, as well as reduction of Ki67. The structure of ribociclib (free base) is also shown. CDK4/6 cyclin-dependent kinase 4 and 6, E2F transcription factor, ER estrogen receptor, ET endocrine therapy, Ki67 nuclear protein Ki67, Rb retinoblastoma tumor suppressor protein
3 Clinical Pharmacokinetics in Patients with Cancer and Healthy Volunteers
In all patient trials and clinical pharmacology studies of ribociclib during its clinical development, plasma concentrations of ribociclib and/or its metabolite M4 (LEQ803) were measured by validated bioanalytical assays [26].
3.1 Absorption
In the first-in-human dose-escalation study in patients with advanced solid tumors or lymphomas and with tumors that have intact Rb (study CLEE011X2101; [NCT01237236]; thereafter, the pre-fix CLEE011 will be omitted for this study and other ribociclib studies), oral administration of ribociclib as a single-agent (50–1200 mg QD, 3 weeks on/1 week off) resulted in rapid absorption across the entire dose range (Fig. 2), with a median time to reach maximum plasma concentration (Tmax) ranging from 1–5 h [33]. Ribociclib exposure increased slightly more than proportional to dose over the dose range of 50–1200 mg [33]. At the dose of 600 mg QD, the mean effective half-life based on accumulation ratio (T1/2, acc) was 32.0 h (Supplementary Table 2) [33, 34], and steady state was generally reached by day 8 [33]. At steady-state (600 mg QD; cycle 1 day 18/21), the geometric mean (geo-mean) maximum plasma concentration (Cmax) of ribociclib was 1820 ng/mL, geo-mean exposure (area under the curve from 0–24 h [AUC0–24]) was 23,800 ng × h/mL, median Tmax was 2.4 h (Supplementary Table 2), and geo-mean trough plasma concentration (Ctrough) was 483 ng/mL [34]. Over the dose range of 50–1200 mg QD, both Cmax and AUC increases were slightly greater than dose proportional [33]. Inter-patient variability in ribociclib exposure was moderate-to-high, with a geo-mean coefficient of variation (CV) of 62.4% for Cmax and 66.0% for AUC0–24 (600 mg QD steady state) [34].

Adapted with permission from reference [34]
Ribociclib plasma concentration profiles at cycle 1 day 1 (A) and cycle 1 day 18/21 (B), and trough concentration profiles of cycle 1 days 1 to 21 (C) [34]. Shown are geometric mean concentration-time profiles of ribociclib across the dose ranges of 50–1200 mg in study X2101. Ctrough trough plasma concentration.
In a phase 1, open-label, crossover study in healthy volunteers (HV), oral absolute bioavailability (F) of ribociclib was 65.8% (90% confidence interval [CI] 59.1–73.2), based on the dose-normalized AUC ratio of intravenous (150 mg) versus oral administration (600 mg) (study A2117, NCT01872260) [26].
No food effect was observed for ribociclib exposure (i.e., Cmax and AUC) in HV (study A2111), allowing ribociclib to be administered with or without food [25]. Furthermore, physiologically based pharmacokinetic (PBPK) models integrating data from studies A2111, X2101, and A2103 in HV and study X2101 in patients with cancer showed that pH changes (due to concomitant use of proton pump inhibitors [PPIs]) have no effect on ribociclib absorption and bioavailability in patients with cancer [25].
Metabolite M4 (LEQ803), a main metabolite of ribociclib (see below), has a parallel PK profile as the parent drug [33], suggesting formation-rate limiting metabolism. Following repeated daily administration of ribociclib (600 mg), M4 Tmax was 4.0 h and T1/2 was 31.4 h in patients with cancer, similar to the parent (Supplementary Table 2). At the 600 mg dose level (single dose and after multiple doses), M4 AUC0–24 h was approximately 8% (geo-mean) of the ribociclib AUC0–24 h (Supplementary Table 2) [34,35,36]. Based on its in vivo exposure, as well as its in vitro pharmacological activity relative to the parent (see below), M4 is not considered to have clinically relevant contribution to pharmacological activity of ribociclib [35]. A schematic summary of the key properties for absorption, distribution, metabolism, and excretion of ribociclib, is shown in Fig. 3.
Schematic overview of key ribociclib ADME properties [26, 33,34,35, 37]. All data are presented as geometric mean, except T1/2 and Tmax, which are shown as median. Based on in vitro studies, and clinical studies and population PK analyses using data from healthy volunteers, patients with Rb-positive advanced solid tumors, and patients with breast cancer [26, 33,34,35, 37]. ADME absorption, distribution, metabolism, and excretion, AUC0–24 h area under the plasma concentration curve from 0–24 h, BID twice daily, CL/F apparent clearance, Cmax maximum plasma concentration, CYP3A4 cytochrome P450 3A4, FMO flavin-containing monooxygenase, PK pharmacokinetics, T1/2 half-life, Tmax time to reach Cmax, Vss/F apparent volume of distribution at steady-state
3.2 Distribution
Results from tissue studies in rats showed that radio-labelled ribociclib is extensively distributed into the extravascular compartment except in the brain [35]. In a human phase 1 study in HV (study 2117), the mean apparent volume of ribociclib distribution at steady state (Vss/F) was 1010 L (geo-mean CV%: 25.2) following a single intravenous (IV) dose of 150 mg [26]. Likewise, in a population PK analysis using data from phase 1 and III trials in patients with cancer (see Supplementary Table 1), the mean apparent Vss/F was 1090 L [37]. The finding that Vss/F is much larger than the body’s plasma volume (approximately 5 L) suggests that ribociclib is extensively distributed in humans [26]. In vitro plasma protein binding of ribociclib was found to be moderate and independent of concentration, with approximately 70% of ribociclib bound to human plasma protein (fraction of unbound ribociclib in human plasma, 0.30 ± 0.02). The blood:plasma ratio in humans was 1.0 [35].
3.3 Metabolism and Excretion
In a human absorption, distribution, metabolism, and excretion (ADME) study in HV following a single oral dose of 600 mg ribociclib (study A2102), the median apparent total plasma clearance (CL/F) of ribociclib was 70.2 L/h; the median renal clearance of ribociclib comprised 5.55 L/h, which is more than 10-fold lower than the observed non-renal clearance (64.7 L/h) [35]. Consistent with this observation, most of the total administered, radiolabeled ribociclib dose was excreted in feces (mean 69.1%), with a lesser extent in urine (mean 22.6%). Ribociclib excreted unchanged into urine comprised 6.75% of the dose [35].
Hepatic metabolism of ribociclib occurs predominantly by oxidative pathways. This involves mostly cytochrome P450 (CYP) 3A4, leading to metabolite M4 (N-demethylation) and accounting for 74 % of all oxidative metabolism, and to a smaller extent by flavin-containing monooxygenase 3 (FMO3), leading to metabolite M13 (CCI284, N-hydroxylation) and accounting for 26% of all oxidative metabolism [35].
Considering all available data, ribociclib is estimated to be eliminated by hepatic metabolism (84% of total elimination), renal excretion (7%), intestinal excretion (8%), biliary elimination (1%) and an unknown, likely low contribution from extrahepatic metabolism (FMO1) [35].
A large number of metabolites were identified in excreta, but of all drug-related compounds, unmetabolized ribociclib was present at the highest abundance, representing 17.3% and 6.75% in feces and urine, respectively, of the administered radioactive ribociclib dose [35]. Similarly, the parent compound was the major circulating drug-derived entity in plasma, representing approximately 43.5% of the total radioactivity AUC0–48 h [35]. The most abundant plasma metabolites were M4 and M13, representing an estimated 8.60%, and 9.39% of total radioactivity, and 19.8%, and 21.6% of ribociclib exposure, respectively [35]. The in vitro pharmacological activity of M4 and M13, based on cell cycle profiling using flow cytometry, was 5-fold lower for M4 (IC50 for G1 arrest, 0.24 µM) and 22-fold lower for M13 (IC50 for G1 arrest, 1.137 µM), compared with that of ribociclib (IC50 for G1 arrest, 0.053 µM) [36]. Together with the plasma exposures of M4 and M13 under therapeutic conditions (geo-mean AUC0–24 of 1920 and 5747 ng × h/mL, respectively, vs 23,800 ng × h/mL for ribociclib), the expected contribution of both metabolites to total pharmacological activity in humans is negligible (1.9% for M4, 1.2% for M13) [34,35,36].
4 Effect of Intrinsic Factors on Ribociclib Pharmacokinetics
4.1 Demographic Factors
The effect of demographic factors on ribociclib PK was evaluated in a population PK analysis using pooled data from three phase 1/2 studies in patients with advanced cancer (X1101, X2101, X2107) and three pivotal phase 3 studies (MONALEESA-2, MONALEESA-3, MONALEESA-7) in patients with ABC (see Supplementary Table 1) [37]. Covariate analysis showed that age, body weight, sex, race (Asian or others vs White), and baseline Eastern Cooperative Oncology Group (ECOG) status (grade 1 vs 0) have no effect on ribociclib PK (based on AUC and clearance) [37].
4.2 Hepatic Impairment
The effect of hepatic impairment on ribociclib PK was evaluated in a dedicated phase 1 study (study A2109, NCT02388620) in individuals without cancer and with varying degree of hepatic impairment (measured by the Child-Pugh classification). Ribociclib exposure (400 mg, single-dose) was similar in individuals with mild hepatic impairment and those with normal hepatic function (geometric mean AUCinf ratio 1.03), but was increased by approximately 30% in individuals with moderate or severe hepatic impairment (geometric mean AUCinf ratios moderate/normal, 1.28; severe/normal, 1.29) (see Fig. 4) [38]. Ribociclib 400 mg was generally well tolerated in all participants regardless of the level of hepatic impairment [38]. Population PK analyses using data including patients with advanced cancer and mild hepatic dysfunction provided similar findings, showing no impact of mild hepatic impairment on ribociclib PK in patients with cancer [37].

Adapted with permission from reference [48]
Impact of CYP inhibitors/inducers, food, renal and hepatic impairment on ribociclib PK and the recommendation for clinical use of ribociclib in patients with advanced breast cancer [39, 48]. All data shown are based on clinical studies in non-cancer patients/healthy volunteers receiving a single-dose ribociclib, except for mild and moderate renal impairment data which are based on a study in patients with advanced breast cancer receiving steady-state ribociclib, and gastric-acid-reducing data which are based on PBPK and PopPK modeling. AUC area under the plasma concentration curve, Cmax maximum plasma concentration, CI confidence interval, CYP1A2 cytochrome P450 1A2, CYP3A4 cytochrome P450 3A4, PBPK physiologically based pharmacokinetics, popPK population pharmacokinetics, PK pharmacokinetics, QD once daily.
The observed 30% increase in exposure in otherwise healthy individuals with moderate or severe hepatic impairment may be considered relatively low given the predominantly hepatic turnover of ribociclib. In particular, the abundance of CYP3A4, the main enzyme involved in ribociclib metabolism, is known to be gradually reduced in hepatic impairment. However, there are no data on a reduced abundance of FMO3, which also contributes to ribociclib metabolism. Ribociclib is also eliminated via renal and intestinal pathways that are not directly impacted by hepatic impairment. Therefore, the lack of substantial increase in ribociclib exposure in individuals with hepatic dysfunction (even severe) may be due to the contributions of FMO3 metabolism, renal, and intestinal elimination to the overall ribociclib clearance [38].
Based on these data, no ribociclib dose adjustment from the recommended dose (600 mg QD, 3 weeks on, 1 week off) is necessary for patients with mild hepatic impairment, but a reduced dose of 400 mg QD, 3 weeks on, 1 week off is recommended in ABC patients with moderate or severe hepatic impairment [38].
4.3 Renal Impairment
A phase 1 study in individuals without cancer assessed the impact of renal impairment (based on absolute glomerular filtration rate [GFR]; study A2116, NCT02431481) on ribociclib exposure following a single 400 mg oral dose [39]. In this study, individuals with renal impairment had higher ribociclib exposure than those with normal renal function, with increases in AUCinf by 62%, 94%, and 167%, in individuals with mild, moderate, and severe renal impairment, respectively, and CL/F reduced by 38.4%, 48.5%, and 62.5%, respectively [39].
The impact of mild or moderate renal impairment on ribociclib PK was further assessed in subgroup analyses of patients with advanced cancer or ABC in 3 clinical studies which involved extensive PK collection (X2101, X2107, MONALEESA-7; renal function defined by estimated creatinine clearance by the Cockcroft-Gault formula). In subgroup analyses of all 3 studies, there was no significant change in steady-state ribociclib exposure (AUC, Cmax and Ctrough) between patients with normal renal function and those with mild or moderate renal impairment, respectively (e.g., among patients receiving steady-state ribociclib [C1D18/21] in study X2101, geo-mean ratios AUC0–24 h [95% CI]: mild/normal 0.80 [0.57–1.11], moderate/normal 0.76 [0.48–1.21]) (see Fig. 4) [39].
Furthermore, renal impairment was also included as a covariate in the population PK analysis using pooled data from clinical studies in patients with advanced cancer or ABC (X2101, X1101, X2107, MONALEESA-2, MONALEESA-3, MONALEESA-7). In the pooled data set, 57.8% patients had mild or moderate renal impairment, and 42.2% patients had normal renal function (based on estimated GFR). Model-simulated steady-state AUC24 h and Cmax showed no apparent differences between renal impairment cohorts (normal vs mild/moderate). Finally, PFS was similar in patients with HR+/HER2− ABC, and safety profiles were generally consistent with manageable AEs, across subgroups of patients with normal renal function, or mild or moderate renal impairment (using data from MONALEESA-2, MONALEESA-3, MONALEESA-7, and X2107), confirming the PK findings [39].
Thus, the collective evidence indicates that mild and moderate renal impairment has no clinically relevant impact on the PK of ribociclib and therefore no dose adjustment is needed in these patients. The reason for the difference between patients with and without cancer regarding the effect of mild or moderate renal dysfunction on ribociclib PK is currently unclear but could be due to differences in patient characteristics (e.g., CYP3A4, the key metabolizing enzyme of ribociclib, may be down-regulated in patients with cancer) [40], ribociclib dosing and treatment duration (single vs multiple dosing), and comorbidities.
For patients with cancer and severe renal impairment, no data on the PK of ribociclib are available, due to exclusion of this patient population from clinical development. Based on data in non-cancer individuals (study A2116), a reduced starting dose of ribociclib 200 mg is recommended for this patient population [39].
5 Drug–Drug Interactions
5.1 Proton Pump Inhibitors
Consistent with the evidence showing high solubility of ribociclib in media simulating intestinal fluids of fed and fasted states [25], concomitant use of PPIs was shown to have a negligible effect on ribociclib bioavailability, based on population PK analysis, PBPK modeling and non-compartmental analysis using data from clinical trials in patients with cancer (studies X2101, X1101, X2107, A2301) (see Fig. 4) [25].
5.2 CYP Inhibitors or Inducers and CYP Substrates
Ribociclib is cleared primarily via hepatic oxidative metabolism, mostly by CYP3A4 (~ 63% of total clearance/~ 74% of all oxidative metabolism), with a minor contribution by FMO3 [35]. Ribociclib as a potential victim of a CYP3A inhibitor (ritonavir) or a CYP3A inducer (rifampin) was assessed in a phase 1 drug–drug interaction (DDI) study in HV (study A2101) [41]. Concomitant administration of the strong CYP3A inhibitor ritonavir increased single-dose ribociclib (400 mg) exposure by 3.21-fold (geo-mean ratio for AUCinf; i.e., 221% increase) compared with ribociclib administered alone (see Fig. 4) [41]. This result informed a PBPK model (integrating data from studies A2101, A2106, and A2102) to further characterize DDIs of ribociclib under conditions not tested in clinical trials, e.g., at steady-state of the recommended starting dose and in patients with cancer. The model predicted a 3.16-fold increase (geo-mean ratio for AUCinf) in single-dose ribociclib (400 mg) AUCinf with ritonavir co-administration in HV, indicating the validity of the model [41]. In patients with advanced cancer receiving steady-state ribociclib (daily doses 600 mg), the PBPK model predicted a 1.31-fold increase (geo-mean ratio for AUC0–24 h; i.e., 31% increase) in ribociclib exposure with ritonavir co-administration compared with ribociclib alone [41]. The PBPK model also estimated the DDIs of moderate or weak CYP3A inhibitors with steady-state ribociclib (daily doses 600 mg) in patients with advanced cancer; compared with ribociclib alone, limited increases in ribociclib AUC0–24 h were predicted with co-administration of the moderate CYP3A inhibitor erythromycin (geo-mean ratio for AUC0–24 h 1.07-fold) and the weak CYP3A inhibitor fluvoxamine (geo-mean ratio for AUC0–24 h 1.02-fold) [41]. The magnitude of increase in ribociclib exposure at steady state with each respective CYP3A inhibitor was dose dependent, with a lower predicted increase at higher ribociclib doses [41].
For the strong CYP3A inducer rifampicin, study A2101 demonstrated a reduction in single-dose ribociclib (600 mg) exposure by 89% (geo-mean ratio for AUCinf: 0.107) versus ribociclib alone in HV (see Fig. 4) [41]. In patients with advanced cancer receiving steady-state ribociclib (daily doses 600 mg), the PBPK model predicted a reduction in ribociclib exposure by 70% (geo-mean ratio for AUC0–24 h: 0.3) with rifampicin co-administration compared with ribociclib alone; for the moderate CYP3A inducer efavirenz, the PBPK model predicted a decrease in steady-state ribociclib exposure by 49% (geo-mean ratio for AUC0–24 h: 0.51) [41]. Thus, these data indicate that concurrent use of ribociclib with drugs that act as CYP inhibitors or inducers may potentially alter exposure of ribociclib.
With respect to the role of ribociclib as a potential perpetrator of DDI, in vitro data showed that ribociclib was a competitive inhibitor of CYP1A2 (Ki: 13.1 µM) and CYP3A (Ki: 35 µM), and a time-dependent inhibitor of CYP3A (Ki: 8.60 μM, kinact: 1.0 h−1) [41]. Ribociclib exhibited no capacity to inhibit CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP2D6, and showed no apparent time-dependent inhibition of CYP1A2, CYP2C9, and CYP2D6 at clinically relevant concentrations [36]. No induction of CYP1A2, CYP2B6, CYP2C9 or CYP3A4 was observed in vitro at clinically relevant concentrations [36]. A phase 1 study assessed ribociclib as a potential perpetrator of CYP3A substrates or CYP1A2 substrates in HV (study 2106) [41]. Steady-state ribociclib (daily doses 400 mg) increased AUCinf of midazolam (a sensitive CYP3A substrate) by 3.75-fold (geo-mean ratio for AUCinf; i.e., 275% increase in midazolam exposure vs midazolam alone) (see Fig. 4) [41]. In patients with advanced cancer, the PBPK model predicted that administration of daily doses ribociclib doses at 600 mg increase midazolam exposure by 5.85-fold (geo-mean ratio for AUCinf; i.e., 485% increase in midazolam exposure vs midazolam alone;) indicating strong CYP3A inhibition by ribociclib [41]. The exposure of caffeine (a sensitive CYP1A2 substrate) in HV (study 2106) was only minimally affected by steady state ribociclib (daily doses 400 mg), with an observed increase in caffeine AUCinf by 1.17-fold versus caffeine alone (geo-mean ratio for AUCinf; i.e., 17 % increase) in study 2106, indicating no CYP1A2 inhibition by ribociclib (see Fig. 4) [41].
Overall, the data indicate that ribociclib exposure can be affected by strong CYP3A inhibitors or strong CYP3A inducers, leading to an increase or decrease in ribociclib exposure, respectively. Hence, it is recommended to avoid co-administration of ribociclib and strong CYP3A inhibitors/inducers, or, alternatively, ribociclib dosing should be reduced to 400 mg when combined with strong CYP3A inhibitors in ABC patients [13]. For mild or moderate CYP3A inhibitors/inducers, no clinically relevant DDIs are expected.
On the other hand, ribociclib can act as a CYP3A inhibitor itself, leading to increased exposure of CYP3A substrates; thus, caution is recommended in case of concomitant use of ribociclib with sensitive CYP3A substrates with narrow therapeutic index. The dose of a sensitive CYP3A substrate with a narrow therapeutic index may need to be reduced as ribociclib can increase their exposure.
5.3 Endocrine Therapy Combination Partners
Ribociclib is approved for the treatment of patients with ABC in combination with NSAIs (e.g., letrozole and anastrozole) or fulvestrant. Hence, potential DDIs between ribociclib and its approved combination partners were assessed by cross-study comparisons using PK data with single-agent ribociclib, as observed in study X2101 in patients with advanced solid tumors or lymphomas, and PK data with ribociclib combinations as observed in studies X2107 (letrozole), MONALEESA-2 (letrozole), MONALEESA-3 (fulvestrant), and MONALEESA-7 (letrozole, anastrozole) in patients with breast cancer [34]. For the combination of ribociclib with letrozole, an NSAI agent, geo-mean AUC0–24 h for ribociclib at steady-state was 23,290 h × ng/mL in study X2107, similar to that reported for ribociclib as a single agent in study X2101 (23,800 h × ng/mL [34]). Likewise, steady-state Cmax and Ctrough of ribociclib 600 mg in combination with letrozole was largely consistent across the three combination studies and the ribociclib single-agent study (Fig. 5 and Supplementary Table 3) [22, 34]. Ribociclib also had no clinically relevant effect on the PK of letrozole, as evidenced by comparable letrozole exposure values in the placebo arm and the ribociclib arm in studies X2107 and MONALEESA-7 (Supplementary Table 4) [22]. These data suggest no apparent drug-drug interaction between ribociclib and letrozole.
Impact of endocrine therapy combination partners on ribociclib exposure at steady state across clinical studies [22, 34]. Boxplots of AUC0–24 h, Cmax and Ctrough at steady state across the studies where ribociclib was administered at 600 mg once daily (3 weeks on/1 week off). Horizontal lines in the box are Q1, median, and Q3. Lower and upper whiskers extend to the most extreme points within 1.5 x IQR of Q1 and Q3, respectively. Diamond-shaped symbols represent the mean, and circle symbols represent values outside of 1.5 x IQR. AUC0–24 h area under the plasma concentration curve from 0–24 h, Cmax maximum plasma concentration, Ctrough trough plasma concentration, ML-2 Monaleesa-2 study, ML-3 Monaleesa-3 study, ML-7 Monaleesa-7 study
Similar findings were obtained when comparing the PK of ribociclib monotherapy (X2101) and that of ribociclib when used in combination with anastrozole, another NSAI agent (MONALEESA-7), although the PK sample size for the anastrozole combination was small (Fig. 5 and Supplementary Table 3) [22, 34]. There was also no apparent effect of ribociclib on the PK of anastrozole (Supplementary Table 4) [22]. Overall, the findings indicate no apparent DDI between ribociclib and anastrozole.
For the combination of ribociclib with fulvestrant, geo-mean plasma Ctrough was similar to ribociclib as a single agent in study X2101 (483 ng/mL) and with ribociclib plus fulvestrant in MONALEESA-3 (553–627 ng/mL) (Fig. 5 and Supplementary Table 4) [34], suggesting that fulvestrant has no effect on the PK of ribociclib. Pharmacokinetic data of fulvestrant were not collected in the MONALEESA-3 trial. Given the fact that neither rifampicin (strong CYP3A4 inducer) nor ketoconazole (strong CYP3A4 inhibitor) have an effect on fulvestrant PK [42], ribociclib (moderate to strong CYP3A4 inhibitor) is unlikely to impact the PK of fulvestrant.
A cross-study comparison using data from studies X2101 and MONALEESA-7 showed a potential DDI between ribociclib and tamoxifen, for which the concomitant use is not indicated for ribociclib. Ribociclib exposure values for the tamoxifen combination were slightly lower than with ribociclib single-agent and with the anastrozole- or letrozole-based combinations (Fig. 5 and Supplementary Table 3), and tamoxifen exposure was approximately 2-fold higher in the presence of ribociclib than placebo (Supplementary Table 4) [36]. Since ribociclib is primarily metabolized by CYP3A4, the slight decrease in ribociclib exposure may be due to the induction potential of tamoxifen on CYP3A4 [43]. The increase in the exposure of tamoxifen, which is a CYP3A substrate [44], may be due to ribociclib being a strong CYP3A inhibitor at a dose of 600 mg in ABC patients.
Findings from the cross-study comparisons for NSAI and fulvestrant were further assessed by population PK and PK/PD analyses, using pooled data from three phase 1 studies (X1101, X2101, X2107) and three phase 3 studies (MONALEESA-2, MONALEESA-3, MONALEESA-7) [37]. Covariate analysis confirmed that ribociclib exposure is not affected by concomitant use of letrozole, anastrozole, or fulvestrant [37]. Population PK/PD analyses showed that concomitant use of letrozole, anastrozole, or fulvestrant have no impact on the relationship between ribociclib exposure and absolute neutrophil count (ANC) [37]. Based on both observed PK data in clinical trials and the population PK and PK/PD analyses, there are no clinically relevant interactions between ribociclib and its approved concomitant endocrine therapy partners, NSAIs and fulvestrant.
5.4 Drug Transporters
Ribociclib uptake into hepatocytes is governed by high passive diffusion without involvement of active transport [36]. Consequently, interactions via hepatic uptake transporters are not expected. In vitro, ribociclib was not a substrate for breast cancer resistance protein (BCRP) but is a low-affinity substrate for the gastrointestinal efflux transporter p-glycoprotein (P-gp; Michaelis constant [Km] > 297 μM) [36]. Due to its moderate to high passive permeability, ribociclib absorption in humans is unlikely to be impacted by co-administration of P-gp inhibitors or inducers. In vitro, ribociclib inhibited BCRP (inhibition constant [Ki] 24.0 μM), organic cation transporter 2 (OCT2, Ki 1.90 μM), multidrug and toxin extrusion protein 1 (MATE1, Ki 1.70 μM), and bile salt export pump (BSEP, Ki 4.7 μM) [36], which may translate into clinically relevant inhibition of these transporters at therapeutic ribociclib doses. Ribociclib is unlikely to inhibit P-gp (Ki 143 μM), organic anion transporting polypeptide 1B1 (OATP1B1, Ki 33.4 μM), OCT1 (Ki 17.3 μM), and MATE2K (Ki 31.0 μM) at clinically relevant concentrations [36].
Ribociclib was an in vitro inhibitor of OCT2 (Ki: 1.90 μM), and MATE1 (Ki: 1.70 μM) [36], which are transporters involved in the active secretion of creatinine from the proximal tubules. In vivo, creatinine levels increased slightly from baseline following a single dose of ribociclib 400 mg in HVs [38], suggesting weak inhibition of these transporters after a single dose of ribociclib. The observed slight increase in creatinine is unlikely due to direct renal toxicity of ribociclib, because levels of cystatin C, which is not actively secreted by renal transporters but filtered freely by the renal glomeruli and hence reflects renal function more accurately than creatinine, remained unchanged following a single dose of ribociclib in HVs [38].
6 Pharmacodynamics in Patients
Ribociclib demonstrated in vivo anti-tumor activity and PK/PD correlations for inhibition of Rb phosphorylation in subsets of tumor xenograft models [36]. In the first-in-human dose-escalation study in patients with advanced solid tumors or lymphomas and with tumors that have intact Rb (study X2101), ribociclib treatment-mediated decreases of Rb phosphorylation were observed in paired (pre- vs post-treatment) skin samples at all dose levels, demonstrating the on-target CD4/6 inhibition by ribociclib [33]. Furthermore, ribociclib treatment-mediated reductions of Ki67 from baseline were observed in paired skin and tumor biopsies across all dose levels, consistent with ribociclib-mediated antiproliferative activity [33].
6.1 Recommended Phase 2 Dose
For patients with HR+/HER2− ABC, the recommended ribociclib starting dose is 600 mg QD (3 weeks on/1 week off), with dose reductions to 400 mg and 200 mg as the first and second dose reductions (for AE management), respectively [12, 13]. This dose selection was based on the first-in-human, phase 1 dose-escalation study (study X2101), which tested single-agent ribociclib at doses of 50–1200 mg QD in patients with advanced solid tumors or lymphomas [33]. In this study, the maximum tolerated dose (MTD) of single-agent ribociclib was 900 mg, and the recommended dose for expansion (RDE) was 600 mg QD based on a lower rate of QTcF prolongation versus higher doses [33]. The same starting dose (600 mg) was studied in the phase 1b/2 study X2107 and three pivotal phase 3 trials in patients with ABC (MONALEESA-2, MONALEESA-3, and MONALEESA-7).
To justify the ribociclib dose regimen and modification scheme in patients with ABC, in particular the impact of dose reduction on efficacy, integrated analyses using PK, efficacy, and safety data of multiple studies, including three pivotal phase 3 studies in ABC, were performed to assess the associations of ribociclib exposure with efficacy (PFS, OS, and time to tumor response [TTR]) and the two AEs of special interest that are associated with ribociclib exposure (neutropenia and QTcF prolongation).
6.2 Exposure-Efficacy Analyses
The relationships between ribociclib exposure and the efficacy endpoints PFS, OS, and TTR were evaluated in a series of time-independent and time‑varying Kaplan–Meier (KM) curves and Cox regression analyses using pooled data of the three pivotal phase 3 studies in patients with ABC (MONALEESA-2, MONALEESA-7, MONALEESA-3) [45].
Kaplan–Meier estimates of PFS stratified by model-predicted geometric mean Ctrough quartiles did not show a clear relationship between PFS and ribociclib exposure (Fig. 6A) [45], and a time-independent Cox regression analysis estimated a hazard ratio (HR) for progression or death of 1.04 (95% CI 1.00–1.08) per 100 ng/mL increase in model-predicted geometric mean Ctrough (i.e., geometric mean of all dosing days), indicating no clear clinical impact of ribociclib exposure on PFS over the studied exposure range [45]. These findings were confirmed by a landmark Cox regression analysis which considered only exposure of patients who stayed in the trial beyond the landmark timepoints of 8, 12, and 16 weeks (median time to dose reduction was 12 weeks) to correct for potential bias in the time-independent Cox regression which may have been caused by using average exposure of overall Ctrough (i.e., not accounting for the potential impact of high exposure in patients who experienced events early, and lower exposure in patients with dose reduction/interruption later in the trials). The landmark regression analysis focusing on the time point 12 weeks showed no apparent relationship between ribociclib exposure and PFS (HR 0.979; 95% CI 0.939–1.022; p = 0.339) [45]. Finally, a time-varying Cox regression model, which considered the change in exposure over time due to dose reduction/interruptions, also indicated no apparent relationship between ribociclib exposure and PFS, with an HR estimate for PFS of 0.98 (95% CI 0.93–1.03; p = 0.465) per 100 ng/mL change in time-varying model-predicted geometric mean Ctrough up to event [45].

Adapted with permission from reference [45]
Exposure-efficacy and exposure-safety relationships with ribociclib. Kaplan–Meier curves of PFS (A) and OS (B) stratified by model-predicted ribociclib Ctrough; probability of grade ≥ 3 neutropenia by steady-state ribociclib Ctrough (C), and change in ΔQTcF by ribociclib concentration (D) when used in combination with NSAI (letrozole or anastrozole) [45]. In panels A and B, Ctrough categories are based on quartiles of geometric mean of model-predicted Ctrough on non-zero dosing days up to event. The number of patients in each quartile range were Q1 (n = 58); Q2 (n = 78); Q3 (n = 69), Q4 (n = 67). Event-free probabilities were calculated for each quartile range of geometric mean of model-predicted Ctrough (ng/mL) on non-zero dosing days over the first 8 weeks of treatment in studies MONALEESA-2, MONALEESA-3, and MONALEESA-7. Panel C shows a logistic regression of newly occurring grade ≥ 3 neutropenia versus geometric mean steady-state ribociclib Ctrough, overlaid with observed proportions—patients with cancer pool (PK-neutropenia set; MONALEESA-2, MONALEESA-3, MONALEESA-7, X2107, X1101 and X2101 studies). The curve indicates the median, and the shadowed area shows the 95% CI of the logistic regression model estimation. n/N is the number of patients with cancer with events/total number of patients with cancer in the quartile range. Observed proportions are calculated for each quartile range of geo-mean steady-state ribociclib Ctrough (i.e., < Q1, ≥ Q1 to < Q2, ≥ Q2 to < Q3, and ≥ Q3) from MONALEESA-2, MONALEESA-3, MONALEESA-7, X2107, X1101 and X2107 studies) and are represented as circles and error bars. Panel D shows a scatter plot and 90% CI of ΔQTcF versus ribociclib concentration when used in combination with letrozole or anastrozole. The plot shows a linear mixed model with patient as a random effect, and mean function in the form of ΔQTcF = log (concentration/median concentration + 1) + (baseline QTcF − median baseline QTcF) +combination + combination × log (concentration/median concentration + 1). Vertical lines from left to right are Q1, median, and Q3 of ribociclib Cmax of patients receiving the 600 mg dose on C1D18/C1D21 of study X2101. Horizontal dotted lines are the reference lines at 30 ms and 60 ms. CI confidence interval, Cmax maximum plasma concentration, Ctrough trough plasma concentration, D day, KM Kaplan–Meier, NSAI nonsteroidal aromatase inhibitors, OS overall survival, PFS progression-free survival, PK pharmacokinetics, Q quartile, QTcF QT interval corrected by Fridericia’s formula, ΔQTcF change in QTcF from baseline, ss steady-state, TTR time to response.
Exposure-efficacy analyses were also performed for OS using data of MONALEESA-3 and MONALEESA-7. There was also no clear separation between model–predicted geometric mean ribociclib Ctrough (all dosing days) and OS using Ctrough up to the event (Fig. 6B). A time-independent Cox regression analysis for OS estimated an HR of 1.07 (95% CI 1.02–1.12; p = 0.006) per 100 ng/mL increase in geometric mean Ctrough, a time-varying Cox regression analysis estimated an HR of 0.94 (95% CI 0.93–0.95; p < 0.001) per 100 ng/mL increase in time-varying geometric mean Ctrough up to the event, and a landmark analysis based on Cox regression at the landmark time point of 12 weeks also showed no apparent relationship between exposure and OS (HR 1.014; 95% CI 0.967–1.063; p = 0.563) [45]. Overall, these analyses suggest no apparent relationship between ribociclib exposure and OS.
For the relationship between exposure and TTR, the time-independent Cox regression model on TTR estimated an HR of 0.99 (95% CI 0.95–1.04; p = 0.676) per 100 ng/mL increase in model–predicted geometric mean Ctrough (all dosing days; data not shown), suggesting that higher exposure may be associated with a negligible effect on TTR. However, in the time-varying Cox model, the estimate of the HR was 1.06 (95% CI 1.01–1.11; p = 0.019) per 100 ng/mL increase in model–predicted geometric mean Ctrough, suggesting that higher exposure may be associated with a slightly earlier TTR [45].
A caveat of the exposure-efficacy analyses is that the data of the three pivotal phase 3 studies are from a single starting-dose level of 600 mg QD. Therefore, the exposure range is narrow and mainly contributed by dose reduction, besides PK variability. Importantly however, both PFS (the primary efficacy endpoint) [15, 17, 20] and OS [16, 19, 22], were statistically and clinically significant with ribociclib use at the starting dose of 600 mg compared with placebo in all three pivotal studies. In addition, an exploratory post hoc analysis of efficacy by dose reduction (zero, one, or two dose reductions) from the starting ribociclib dose of 600 mg QD showed that median PFS and ORR were still numerically greater than in the placebo arm [45].
Overall, the collective evidence—i.e., both PFS and OS endpoints being met [15,16,17, 19, 20, 22], no apparent exposure-efficacy relationship for PFS and OS [45], and no impact of dose reduction on PFS and ORR [45]—suggests that the ribociclib starting dose of 600 mg QD achieves maximal response and that reducing the dose to 400 mg and 200 mg QD has no impact on the efficacy of ribociclib in patients with ABC.
6.3 Exposure-Safety Analyses
The relationship between ribociclib exposure an45d the two exposure-dependent AEs, neutropenia and QT interval prolongation, was evaluated in analyses of pooled data of several phase 1 to 3 clinical trials [].
6.3.1 Neutropenia
Neutropenia is a class effect for CDK4/6 inhibitors, which was also manifested by ribociclib [46, 47]. A logistic regression analysis of newly occurring grade ≥ 3 neutropenia versus ribociclib steady-state Ctrough (doses ranging from 50–1200 mg) demonstrated that higher ribociclib exposure was associated with a higher probability of grade ≥ 3 neutropenia (Fig. 6C) [45]. This is in line with the longitudinal PK/PD modeling of ribociclib PK and ANC, showing that the risk of neutropenia associated with ribociclib treatment may be mitigated with dose reductions [37], and supports the current prescribing information for the management of neutropenia [12, 13]. Covariate analysis showed that the effect of ribociclib on ANC was not affected by age, body weight, sex, race (Asian or others vs Caucasian), baseline ECOG status (grade 1 vs normal), or the use of letrozole, anastrozole, or fulvestrant [37].
6.3.2 QTcF Prolongation
A concentration-QTcF analysis was conducted to assess the relationship between ribociclib concentration and QTcF prolongation, using pooled data from studies in patients with cancer receiving ribociclib (50–1200 mg) as a single agent or in combination with NSAI (letrozole or anastrozole), fulvestrant, or tamoxifen [45].
The analysis showed that QT prolongation is ribociclib concentration-dependent across all combinations, supporting ribociclib dose reduction to reduce QT prolongation. The estimated mean QTcF at the geometric mean Cmax at steady state was similar for ribociclib 600 mg QD in combination with a NSAI (22.0 ms; Fig. 6D) and with fulvestrant (23.7 ms; data not shown), and both were consistent with the data of the single agent, suggesting no impact of NSAI or fulvestrant on QT prolongation [45]. The estimated mean ΔQTcF for ribociclib 600 mg QD in combination with tamoxifen was higher (34.7 ms) than in combination with NSAI or fulvestrant. This indicates that QTcF prolongation is similar among patients treated with ribociclib plus NSAIs or fulvestrant, but is higher in combination with tamoxifen, likely due to the QT prolongation effect of tamoxifen, which is reported to interfere with cardiac ion channel function [45]. As a result of the QT findings, ribociclib is not indicated for concomitant use with tamoxifen [12, 13].
In summary, exposure-safety analyses showed that neutropenia and QT prolongation are related to ribociclib exposure and can be effectively managed by dose reduction.
7 Summary and Conclusions
The clinical PK/PD and clinical pharmacology data support the use of ribociclib in its approved indication for HR+/HER2− ABC in pre-/perimenopausal and post-menopausal women at the recommended dose regimen of 600 mg daily (3 weeks on/1 week off), with no dose adjustments required based on age, body weight, race, combination partner (NSAIs or fulvestrant), food intake, proton pump inhibitors, or presence of mild-to-moderate renal impairment or mild hepatic impairment. Individualized dose reductions in ABC patients are warranted by medical necessity, such as moderate-to-severe hepatic impairment or severe renal impairment, concomitant use of a strong CYP3A inhibitor, or for the management of neutropenia and QTcF interval prolongation, and have been shown not to compromise efficacy. In conclusion, the clinical PK/PD, and clinical pharmacology data summarized in this review informed dose justification in pivotal trials and decision making during ribociclib clinical development for patients with ABC, and provided prescribing information for the use of ribociclib across patient populations, including dose recommendations in sub-populations and when used with food or concomitant medications.
References
Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29.
Cortet M, Bertaut A, Molinie F, et al. Trends in molecular subtypes of breast cancer: description of incidence rates between 2007 and 2012 from three French registries. BMC Cancer. 2018;18(1):161.
Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiol Biomark Prev: Publ Am Assoc Cancer Res Cospons Am Soc Prev Oncol. 2018;27(6):619–26.
Miao H, Hartman M, Bhoo-Pathy N, et al. Predicting survival of de novo metastatic breast cancer in Asian women: systematic review and validation study. PLoS ONE. 2014;9(4): e93755.
Iqbal J, Ginsburg O, Rochon PA, et al. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA J Am Med Assoc. 2015;313(2):165–73.
Pan HC, Gray R, Braybrooke J, et al. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377(19):1836–46.
Cardoso F, Paluch-Shimon S, Senkus E, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31(12):1623–49.
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Breast Cancer V.4.2023. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed 13 July 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
Tripathy D, Bardia A, Sellers WR. Ribociclib (LEE011): mechanism of action and clinical impact of this selective cyclin-dependent kinase 4/6 inhibitor in various solid tumors. Clin Cancer Res: Off J Am Assoc Cancer Res. 2017;23(13):3251–62.
Kwapisz D. Cyclin-dependent kinase 4/6 inhibitors in breast cancer: palbociclib, ribociclib, and abemaciclib. Breast Cancer Res Treat. 2017;166(1):41–54.
Kisqali (Ribociclib) Summary of Product Characteristics. Novartis Pharma GmbH. https://www.ema.europa.eu/en/documents/product-information/kisqali-epar-product-information_en.pdf. Accessed 24 July 2023.
Kisqali (Ribociclib) Prescribing Information. Novartis Pharmaceuticals Corporation, 2022. https://www.novartis.com/us-en/sites/novartis_us/files/kisqali.pdf. Accessed 24 July 2023.
O’Shaughnessy J, Petrakova K, Sonke GS, et al. Ribociclib plus letrozole versus letrozole alone in patients with de novo HR+, HER2− advanced breast cancer in the randomized MONALEESA-2 trial. Breast Cancer Res Treat. 2018;168(1):127–34.
Hortobagyi GN, Stemmer SM, Burris HA, et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol. 2018;29(7):1541–7.
Hortobagyi GN, Stemmer SM, Burris HA, et al. Overall survival with ribociclib plus letrozole in advanced breast cancer. N Engl J Med. 2022;386(10):942–50.
Slamon DJ, Neven P, Chia S, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018;36(24):2465–72.
Slamon DJ, Neven P, Chia S, et al. Overall survival with ribociclib plus fulvestrant in advanced breast cancer. N Engl J Med. 2020;382(6):514–24.
Slamon DJ, Neven P, Chia S, et al. Ribociclib plus fulvestrant for postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer in the phase III randomized MONALEESA-3 trial: updated overall survival. Ann Oncol. 2021;32(8):1015–24.
Tripathy D, Im SA, Colleoni M, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. Lancet Oncol. 2018;19(7):904–15.
Im SA, Lu YS, Bardia A, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381(4):307–16.
Lu YS, Im SA, Colleoni M, et al. Updated overall survival of ribociclib plus endocrine therapy versus endocrine therapy alone in pre- and perimenopausal patients with HR+/HER2− advanced breast cancer in MONALEESA-7: a phase III randomized clinical trial. Clin Cancer Res. 2022;28(5):851–9.
Slamon DJ, Stroyakovskiy D, Yardley DA, et al. Ribociclib and endocrine therapy as adjuvant treatment in patients with HR+/HER2− early breast cancer: primary results from the phase III NATALEE trial. J Clin Oncol. 2023;41(suppl 17):LBA500.
Hortobagyi GN, Stemmer SM, Burris HA, et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol. 2019;30(11):1842.
Samant TS, Dhuria S, Lu Y, et al. Ribociclib bioavailability is not affected by gastric pH changes or food intake: in silico and clinical evaluations. Clin Pharmacol Ther. 2018;104(2):374–83.
Ji Y, Abdelhady AM, Samant TS, Yang S, Rodriguez LK. Evaluation of absolute oral bioavailability and bioequivalence of ribociclib, a cyclin-dependent kinase 4/6 inhibitor, in healthy subjects. Clin Pharmacol Drug Dev. 2020;9(7):855–66.
Laisney M, Heimbach T, Mueller-Zsigmondy M, Blumenstein L, Costa R, Ji Y. Physiologically based biopharmaceutics modeling to demonstrate virtual bioequivalence and bioequivalence safe-space for ribociclib which has permeation rate-controlled absorption. J Pharm Sci. 2022;111(1):274–84.
Kim S, Tiedt R, Loo A, et al. The potent and selective cyclin-dependent kinases 4 and 6 inhibitor ribociclib (LEE011) is a versatile combination partner in preclinical cancer models. Oncotarget. 2018;9(81):35226–40.
Kim S, Tiedt R, Loo A, et al. Correction: The potent and selective cyclin-dependent kinases 4 and 6 inhibitor ribociclib (LEE011) is a versatile combination partner in preclinical cancer models. Oncotarget. 2020;11(14):1289.
Rader J, Russell MR, Hart LS, et al. Dual CDK4/CDK6 inhibition induces cell-cycle arrest and senescence in neuroblastoma. Clin Cancer Res: Off J Am Assoc Cancer Res. 2013;19(22):6173–82.
Zhang A, Wang X, Fan C, Mao X. The role of Ki67 in evaluating neoadjuvant endocrine therapy of hormone receptor-positive breast cancer. Front Endocrinol (Lausanne). 2021;12: 687244.
O’Brien NAea. In vivo efficacy of combined targeting of CDK4/6, ER and PI3K signaling in ER+ breast cancer. Cancer Res. 2014;74(19_Supplement):abstract 4756.
Infante JR, Cassier PA, Gerecitano JF, et al. A phase I study of the cyclin-dependent kinase 4/6 inhibitor ribociclib (LEE011) in patients with advanced solid tumors and lymphomas. Clin Cancer Res. 2016;22(23):5696–705.
Ji YS, Tanay S, Quinlan M, Chakraborty A. Pharmacokinetic assessment of ribociclib, an oral CDK4/6 inhibitor, and the interaction with endocrine therapy partners in patients with advanced cancer. Cancer Res. 2020;80(4_Supplement):P1-19–37. https://doi.org/10.1158/1538-7445.SABCS19-P1-19-37
James AD, Schiller H, Marvalin C, et al. An integrated assessment of the ADME properties of the CDK4/6 Inhibitor ribociclib utilizing preclinical in vitro, in vivo, and human ADME data. Pharmacol Res Perspect. 2020;8(3): e00599.
Novartis data on file.
Lu Y, Yang S, Ho YY, Ji Y. Ribociclib population pharmacokinetics and pharmacokinetic/pharmacodynamic analysis of neutrophils in cancer patients. J Clin Pharmacol. 2021;61(8):1054–68.
Samant TS, Yang S, Miller M, Ji Y. Pharmacokinetics of ribociclib in subjects with hepatic impairment. J Clin Pharmacol. 2021;61(8):1001–9.
Ji Y, et al. Justifying ribociclib dose in advanced breast cancer patients with renal impairment based on PK, safety and efficacy data. Clin Pharmacokinet. 2023;62(3):493–504.
Murray GI, Patimalla S, Stewart KN, Miller ID, Heys SD. Profiling the expression of cytochrome P450 in breast cancer. Histopathology. 2010;57(2):202–11.
Samant TS, Huth F, Umehara K, et al. Ribociclib drug–drug interactions: clinical evaluations and physiologically-based pharmacokinetic modeling to guide drug labeling. Clin Pharmacol Ther. 2020;108(3):575–85.
Faslodex (Fulvestrant) Prescribing Information. AstraZeneca 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/021344s044lbl.pdf. Accessed 24 July 2023.
Desai PB, Nallani SC, Sane RS, et al. Induction of cytochrome P450 3A4 in primary human hepatocytes and activation of the human pregnane X receptor by tamoxifen and 4-hydroxytamoxifen. Drug Metab Dispos. 2002;30(5):608–12.
Nolvadex (Tamoxifen Citrate) Prescribing Information. AstraZeneca Pharmaceuticals LP 2004. https://www.accessdata.fda.gov/drugsatfda_docs/label/2005/17970s053lbl.pdf. Accessed 24 July 2023.
Ji Y, et al. Quantitative assessment of ribociclib dose- and exposure-response relationship in patients with advanced breast cancer. J Clin Pharmacol. 2023;63(12):1359–70.
Spring LM, Zangardi ML, Moy B, Bardia A. Clinical management of potential toxicities and drug interactions related to cyclin-dependent kinase 4/6 inhibitors in breast cancer: practical considerations and recommendations. Oncologist. 2017;22(9):1039–48.
Byers KF. Ribociclib and abemaciclib: CDK4/6 inhibitors for the treatment of hormone receptor-positive metastatic breast cancer. J Adv Pract Oncol. 2021;12(1):100–7.
Abdelhady AM, et al. Ribociclib dose recommendations for potential pharmacokinetic drug interaction and in special patient populations with organ impairment. In: Presented at: 2017 San Antonio Breast Cancer Symposium; December 5-9, 2017; San Antonio, TX, USA Abstract P1-14-05 2017.
Acknowledgements
The authors thank Tanay S. Samant, Yasong Lu, Ahmed Abozeid, and Faye Su for their contributions to this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding provided by Novartis Pharmaceuticals Corporation.
Data Sharing Statement
Patient-level data for 'Data on file' in this manuscript are not available for sharing as there is a reasonable likelihood that individual patients could be re-identified. All other data have been published previously as cited, and are therefore included in the respective main manuscripts. Further information can be requested from the authors of the individual included studies.
Conflict of interest
All authors are employees of Novartis.
Medical Writing Support
Medical writing support under the direction of the authors was provided by Isabella Kaufmann of Novartis Pharmaceuticals UK Ltd, according to Good Publication Practice guidelines.
Ethics approval and Consent to Participate
Not applicable.
Author contribution and Consent for Publication
All authors contributed to the selection and interpretation of data, were involved in the drafting and critically reviewing of the manuscript, provided final approval of the version to be published, and agree to be accountable for all aspects of the work.
Material and Code Availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ji, Y., Schiller, H., Yang, S. et al. Use of Pharmacokinetic and Pharmacodynamic Data to Develop the CDK4/6 Inhibitor Ribociclib for Patients with Advanced Breast Cancer. Clin Pharmacokinet 63, 155–170 (2024). https://doi.org/10.1007/s40262-023-01338-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01338-z