Abstract
Background and Objectives
Vericiguat is a soluble guanylate cyclase stimulator indicated to reduce the risk of cardiovascular death and hospitalization due to heart failure. A dedicated QTc study in patients with chronic coronary syndromes demonstrated no clinically relevant QTc effect of vericiguat for exposures across the therapeutic dose range (2.5–10 mg). Interval prolongation concentration-QTc (C-QTc) modeling was performed to complement the statistical evaluations of QTc in the dedicated QTc study.
Methods
Individual time-matched, baseline- and placebo-corrected Fridericia-corrected QT interval values (ΔΔQTcF) were derived. Two approaches for ΔΔQTcF calculation were investigated: (1) ΔΔQTcF correction with data from a single baseline (as in the primary statistical analysis); and (2) ΔΔQTcF correction with a modeled baseline (considering all available individual non-treatment baselines). The ΔΔQTcF values were related to observed vericiguat concentrations with linear mixed-effects modeling.
Results
For both modeling approaches, a positive relationship was found between ΔΔQTcF and vericiguat concentration; however, the slope for the single-baseline approach was not statistically significant, whereas the slope from the modeled-baseline approach was statistically significant. The upper bound of the two-sided 90% confidence interval for model-derived QTc was < 10 ms at the highest observed exposure (745 μg/L; investigated dose range 2.5–10 mg).
Conclusion
By applying a single-baseline approach and a modeled-baseline approach that integrated all available QTc data across doses to characterize the QTc prolongation potential, this study showed that vericiguat 2.5–10 mg is not associated with clinically relevant QTc effects, in line with the conclusion from the primary statistical analysis.
Clinical Trials Registration Number
ClinicalTrials.gov NCT03504982.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Two different concentration-QTc modeling approaches (a single-baseline approach and a modeled-baseline approach) demonstrated that vericiguat 2.5–10 mg once daily was not associated with a clinically relevant QTc effect in patients with chronic coronary syndromes. |
The findings were in agreement with those of the vericiguat dedicated QTc clinical study. |
1 Introduction
Vericiguat is a soluble guanylate cyclase stimulator indicated for the treatment of symptomatic chronic heart failure (HF) in adult patients with reduced left ventricular ejection fraction (EF) who are stabilized after a recent decompensation event requiring intravenous therapy [1, 2]. The phase III VICTORIA study demonstrated that vericiguat 10 mg once daily was associated with a reduction in the composite endpoint of death from cardiovascular causes or hospitalization for HF (hazard ratio 0.90, 95% confidence interval [CI] 0.82–0.98; p = 0.02) in patients with HF and EF < 45% and a recent worsening HF event [3].
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use on QTc assessment (ICH E14 guideline) requires testing of new chemical entities in a so-called ‘thorough QT/QTc’ study at supratherapeutic doses in healthy volunteers [4]. To claim that a drug is devoid of proarrhythmic risk, a QTc prolongation of > 10 ms must be excluded at the peak plasma level (Cmax) and all other time points post dosing (by time point analysis). The ICH E14 guidelines allow concentration-QTc (C-QTc) modeling to be used as an alternative to a dedicated QTc study as the primary analysis for assessing the QTc effect of new drugs [5], while regulatory authorities may request both C-QTc modeling and dedicated QTc studies to support drug approval decisions. As orthostatic reactions were observed in healthy volunteers at higher doses in phase I studies with vericiguat, an alternative study design was employed as part of the early clinical development of vericiguat, with a moxifloxacin arm as the positive control [6]. This was a randomized, dedicated phase Ib study (ClinicalTrials.gov identifier: NCT03504982), conducted at therapeutic doses, in 74 adult patients with chronic coronary syndrome (CCS; stable coronary artery disease) [6] and was performed in accordance with the ICH E14 guideline recommendations for QTc studies in special cases when studies in healthy volunteers are inappropriate [7]. The population of patients with CCS was chosen because it was assumed to have a similar QTc response to vericiguat compared with the VICTORIA study population, while it was expected to be more hemodynamically stable than a population with worsening HF and to be subject to fewer confounders such as pacemakers, atrial fibrillation, and left bundle branch block. The dedicated QTc study demonstrated no clinically relevant effects on the time-matched, baseline- and placebo-adjusted Fridericia-corrected QT interval (QTcF) [ΔΔQTcF] after vericiguat 10 mg once daily at steady state (the primary endpoint) [6].
Given the specifics of the QTc study design, which included a multiple-dose aspect with fixed uptitration periods and moxifloxacin as a positive control either at the beginning or end of the titration phase, statistical evaluations were based on ΔΔQTcF correction of data from one single baseline. To complement this single-baseline approach, we conducted two additional C-QTc analyses, one of which utilized non-treatment data from all time points for better assessment of placebo profiles (modeled-baseline approach). Generally, studies with a range of pharmacological agents have demonstrated good agreement between the findings of C-QTc modeling and dedicated QTc studies [8, 9].
Here, we followed the recommendations for C-QTc modeling as outlined in the scientific white paper by Garnett et al. [10], which describes C-QTc modeling of baseline-adjusted QTc data from early-phase clinical studies in healthy volunteers, with slight adjustments accounting for study design differences.
2 Methods
2.1 Dedicated QTc Study Design
The dedicated QTc study was a randomized, phase Ib, placebo-controlled, double-blind, double-dummy, multicenter study (ClinicalTrials.gov identifier: NCT03504982) in patients with CCS, and has been described previously [6]. Patients were randomized to one of two treatment sequences, comprising four treatments each (Fig. 1). In either sequence, oral vericiguat (test drug) once daily initiated at 2.5 mg (treatment A) was uptitrated to 5 mg (treatment B) and then to 10 mg (treatment C) at 14 (±3)-day intervals for a total treatment duration of 42 days, which corresponds to the dosing regimen utilized in the phase III VICTORIA study [3]. A positive control was used for the purpose of testing the sensitivity of the study to detect a QTc effect. Hence, a single dose of moxifloxacin 400 mg was administered (treatment D) on either day 8 (±3 days) or day 50 (±3 days), with placebo administered on other days. The two treatment sequences were thus either (1) A*BCD or (2) DABC*, where the asterisk denotes moxifloxacin placebo administered on day 8 (±3 days) or day 50 (±3 days), respectively, to maintain blinding.

Adapted from Böttcher et al. [6] licensed under CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/)
Study design. *Denotes moxifloxacin placebo was administered on day 8 or day 50.
Triplicate electrocardiograms (ECGs; using modified Goldberger/Einthoven leads according to Mason/Likar and standard chest leads according to Wilson) were recorded within a time span of 2–6 min after the patient was supine for 15 min. Standard 10-s ECGs were recorded using tested digital ECG machines (approved by the European Union [CE marking] and US Food and Drug Administration [FDA]) provided by the ECG core laboratory (Nabios GmbH, Munich, Germany) operated by trained personnel. The ECG machines automatically measured and calculated heart rate (HR), PR (PQ) interval, QRS duration, QT interval, and QTcF.
ECGs were performed at screening (within 28 days before first dosing), predose, and at 1.5, 2.0, 2.5, 3.0, 3.5, 4.0, 4.5, 5.0, and 7.0 h after dosing on visits 1–11 (Fig. 1). Two baseline profiles were measured: baseline at visit 1 (day −1) and a back-up baseline at follow-up (day 63; approximately 7 days after visit 11). The calculation of ΔΔQTcF using these two baselines is described separately for the two C-QTc modeling approaches below.
Blood samples for vericiguat pharmacokinetic (PK) evaluation were collected predose and at 1.5, 2.0, 2.5, 3.0, 3.5, 4.0, 4.5, and 5.0 h after dosing on ECG profile days. The QTcF interval measurements were matched to the PK measurement obtained closest in time to the ECG.
2.2 Calculating ΔΔQTcF for Concentration-QTc (C-QTc) Modeling
2.2.1 Single-Baseline ΔΔQTcF Estimation
In the single-baseline approach (as applied in the statistical evaluation of the dedicated QTc clinical study), the ΔΔQTcF was adjusted with the baseline profile that was closest to the on-treatment (active or placebo) profile. The specific baselines used per sequence were as follows. For placebo ECG profiles, back-up baseline at day 63 was used for sequence A*BCD, and baseline at day −1 was used for sequence DABC*. For vericiguat/moxifloxacin ECG profiles, baselines used were those closest to the vericiguat block (ABC* or A*BC), i.e. for sequence A*BCD, baseline at day −1 was used; for sequence DABC*, back-up baseline at day 63 was used.
ΔΔQTcF was calculated according to the following equation (Eq. 1):
where \(i\) denotes individual patients and \(j\) denotes specific time points (1.5–7 h) in the randomized treatment arm; \({\mathrm{QTcF}}_{\mathrm{Vericiguat}}\) and \({\mathrm{QTcF}}_{\mathrm{Placebo}}\) denote the QTcF measurements following treatment with vericiguat or placebo, respectively, while \({\mathrm{QTcF}}_{\mathrm{BL},\mathrm{Vericiguat},{i,j}}\) and \({\mathrm{QTcF}}_{\mathrm{BL},\mathrm{Placebo},i,j}\) denote baseline QTcF measurements used to correct the QTcF measurements following treatment with vericiguat or placebo, respectively.
2.2.2 Modeled-Baseline ΔΔQTcF Estimation
In the modeled-baseline approach, data from the baseline and back-up baseline from each participant were integrated. A model of the baseline QTcF was built first according to the following equation (Eq. 2):
where baseline and placebo QTcF measurements serve as dependent variables; \({ \theta }_{\mathrm{BL}}\) denotes baseline QTcF and \({\theta }_{\mathrm{Placebo}=1}\) denotes a placebo effect added in the case of placebo, \({\theta }_{j}\) denotes discrete diurnal effects giving a separate estimate for every jth timepoint, \({\eta }_{i}\) denotes interpatient variability on the intercept, and \(\varepsilon_{i,j}\) denotes the normally distributed residual additive error, with mean 0 and variance \({\omega }^{2}\) and \({\sigma }^{2}\), respectively. In a second step, ΔΔQTcF was calculated analogous to the single-baseline approach but using the individual time-matched and placebo-corrected model-predicted values for QTcFBL,Vericiguat,i,j and QTcFBL,Placebo,i,j.
Thus, the key difference compared with the single-baseline approach was the use of a modeled baseline simultaneously informed with all non-treatment baselines measured per individual.
2.3 Testing of Model Assumptions
Prior to performing the planned C-QTc analysis, data were explored to evaluate whether the assumptions of the prespecified linear mixed-effects model were met, as recommended in the white paper [10]. Model assumptions were (1) absence of relevant drug effect on HR; (2) adequate HR correction of QT, demonstrated by absence of correlation between QTcF and HR, analyzed by Pearson’s correlation; (3) lack of PK/pharmacodynamic (PD) hysteresis (time delay between the measured concentration and the PD response); and (4) no hints for a non-linear C-ΔΔQTcF relationship.
2.4 C-QTc Modeling
After verification of the assumptions of the prespecified linear mixed-effects model were met, calculated ΔΔQTcF from both the single-baseline and modeled-baseline approaches were matched by time point to observed vericiguat concentrations. The following model was applied to ΔΔQTcF data (Eq. 3):
where \(\mathrm{\Delta \Delta QT}{\mathrm{cF}}_{\mathrm{Vericiguat},i,j}\) is the baseline and placebo-adjusted QTcF of subject i and time point ti,j under treatment with vericiguat, \({\mathrm{Conc}}_{i,j}\) is the vericiguat concentration of subject i at time point ti,,j, \(\theta\) denotes the intercept and slope of the linear effect of vericiguat concentration on ΔΔQTcF, and η denotes the interindividual variability therein [normally distributed around 0 and standard deviation SD(\({\eta }_{\mathrm{intercept},i}\)) and SD(\({\eta }_{\mathrm{slope},i}\))]; \({\epsilon }_{i,j}\) denotes the residual error term (normally distributed centered around 0 and with standard deviation sigma). For the model parameters, a 95% CI was derived via bootstrapping (1000 samples).
Irrespective of the correction method used, mean predicted ΔΔQTcF values and their 90% CIs can be estimated over the observed range of concentrations using the equations from the white paper [10] independently of whether single or double delta was used as the dependent variable. A clinically relevant QTcF effect was defined as a QTcF effect with an upper limit of the two-sided 90% CI of ≥ 10 ms, as defined in the ICH E14 guidelines [4].
3 Results
The dataset for this modeling study comprised 3785 C-QTcF observations (excluding C-QTcF observations from the pretreatment baseline and placebo arms) from 74 patients enrolled in the dedicated QTc study. Subject disposition is shown in Fig. 2. The observed plasma concentration for vericiguat included in the analysis covered a range up to 745 µg/L.

Reproduced from Böttcher et al. [6] licensed under CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/)
Subject disposition. *Denotes moxifloxacin placebo was administered on day 8 or day 50.
Most deviations in measurement time between the PK sampling and time-matched ECGs were within 5 min (electronic supplementary material [ESM] Fig. S1). A predetermined 30-min limit was exceeded only for predose measurements; therefore, no deviations were considered relevant in this analysis and all data were eligible for a C-QTc modeling approach.
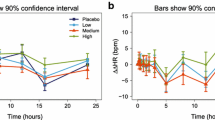
All prerequisites of the models were fulfilled. Mean baseline- and placebo-corrected HR (ΔΔHR) increased in a dose-dependent manner, but neither demonstrated a treatment effect larger than 10 beats/min. The ΔΔHR threshold of concern as specified in the white paper [10] was not observed (Fig. 3). Analysis of off-treatment QT data (uncorrected QT and QTcF) and HR data demonstrated that the correlation between QTcF and HR was sufficiently low (Pearson’s correlation coefficient –0.11; 95% CI –0.17 to –0.06) [ESM Fig. S2], and subsequent analysis was conducted on QTcF data. Visual inspection of the ΔΔQTcF versus concentration plot (ESM Fig. S3) did not reveal a delayed effect; therefore, a direct relationship was assumed. Furthermore, based on visual inspection of the residuals (ESM Figs. S4 and S5), a linear model was considered sufficient to adequately describe the C-QTcF relationship.
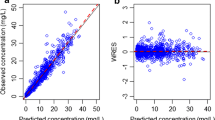
The C-QTc modeling of ΔΔQTcF calculated using the single-baseline approach indicated a positive, but non-significant, slope (estimate, 5.48 ms*L/mg; 95% CI −1.15 to 11.70 ms*L/mg; zero is included in the CI range) (Table 1a). The modeled-baseline approach indicated a positive and statistically significant slope (estimate 7.05 ms*L/mg; 95% CI 1.41–12.70 ms*L/mg) (Table 1b), as evidenced by the positive values of the lower 2.5% CI. For both approaches, the upper bound of the two-sided 90% CI for model-derived QTc was < 10 ms (threshold of regulatory concern) at the highest clinically relevant exposure that was measured for the investigated dose range of 2.5–10 mg (745 μg/L) (Fig. 4). The robustness of the different modeling approaches is recognizable by the similarities of the obtained slopes (5.48 ms*L/mg for the single-baseline approach and 7.05 ms*L/mg for the modeled-baseline approach, with the lower limit of the two-sided 90% CI for both approaches being close to zero) (Fig. 4). Further to this, the vericiguat plasma concentration at which the upper limit of the two-sided 90% CI of the estimated ΔΔQTcF was predicted to reach the 10 ms threshold was similar for the two approaches (757 μg/L for the single-baseline approach and 819 μg/L for the modeled-baseline approach), although it should be noted that according to Garnett et al. [10], C-QTc models should not be extrapolated to concentrations that fall outside the range of observed concentrations used to generate the model. It is also important to note that these results do not indicate an increased risk at higher concentrations, but that the confidence regarding the absence of any risk is declining, e.g. probably only due to lack of any data in this concentration range from this study.
ΔΔQTcF versus observed vericiguat concentration. a Single-baseline approach, and b modeled-baseline approach. Black dots represent data of ΔΔQTc versus concentrations. Solid red line shows the estimated typical linear C-QTc effect and the red shaded area is the associated 90% confidence interval. Horizontal dashed lines indicate the range −10 to +10 ms. Blue dots and blue bars indicate the median and 90% confidence interval of ΔΔQTc data in 10 equally sized (regarding sample count) concentration bins, indicated by the vertical black lines. ΔΔQTcF time-matched, baseline- and placebo-adjusted Fridericia-corrected QT interval, C-QTc concentration-QTc
4 Discussion
This C-QTc analysis was performed to complement the statistical evaluations of QT/QTc interval prolongation in the dedicated vericiguat QTc clinical study conducted in patients with CCS. In agreement with the finding of the dedicated QTc clinical study, two different C-QTc modeling approaches demonstrated that vericiguat 2.5–10 mg once daily was not associated with a clinically relevant QTc effect in patients with CCS.
Time-matched PK and ECG measurements covered the time of peak concentration of vericiguat (Tmax, 1–4 h [1]) and were considered sufficiently frequent to capture potential direct or delayed effects of vericiguat on QTc. All prerequisites of the C-QTc models were met: (1) no drug effect on HR; (2) QTcF interval is independent of HR; (3) no time delay between drug concentrations and ΔΔQTcF; and (4) no hints for the non-linear C-ΔΔQTcF relationship. Therefore, the linear mixed-effects model used in this study was applied to evaluate the C-QTc relationship in a modeling approach.
Owing to the alternative study design of the vericiguat-dedicated QTc study, conducted at therapeutic doses in patients with CCS, the C-QTc model was selected, following as close as possible the recommended approach [10], which is based on QTc data at supratherapeutic doses in healthy volunteers. Supratherapeutic doses are recommended to remove the need for a positive control when C-QTc models are based on data from early-phase studies that were not designed specifically to assess the effects on QTc [10]. However, the use of moxifloxacin as a positive control in the vericiguat-dedicated QTc study demonstrated that our study design was sensitive to detect effects on QTc [6].
As the dedicated QTc study was not a typical single/multiple-dose escalation phase I study, but offered baseline, placebo, and treatment data per individual, we were able to directly calculate the ΔΔQTcF, which was used as the dependent variable in our analyses. For both the single-baseline and modeled-baseline approach, the upper limits of the two-sided 90% CI ΔΔQTcF were below the threshold of regulatory concern of 10 ms across the observed concentration range, as defined in the guidelines [4, 10]. Given the confirmation of assay sensitivity, a clinically relevant QTc effect was excluded within the plasma concentration range associated with the recommended target dose of vericiguat 10 mg once daily in the study population. The observed vericiguat plasma concentration in the analysis (≤ 745 µg/L) covered a range that is in line with that reported for patients with HF treated with vericiguat 10 mg once daily [1].
The approach for C-QTc modeling employed in this study followed the white paper recommendations [10] as closely as possible, and it is not anticipated that the modifications to the study design had any material effect on the interpretation of the data. Indeed, consistent with recommendations to utilize data from all doses and time points [10], the two modeling approaches applied in this C-QTc analysis used all available non-treatment baselines, and the modeled-baseline approach considered the totality of the data from both baseline options. Both approaches indicated a positive (but not clinically relevant) relationship between ΔΔQTcF and vericiguat plasma concentration. Although this relationship was statistically significant for the modeled-baseline approach only, results from both approaches were similar and thus confirmed the results of the statistical evaluations of QT/QTc interval prolongation.
Consequently, the findings of the vericiguat C-QTc analysis agreed with the conclusion from the statistical by time point regression analysis of the dedicated QTc clinical study, which indicated no clinically relevant QTc effect within the plasma concentration range associated with the recommended target dose of vericiguat 10 mg once daily [6]. Similarly, studies with other pharmaceutical agents have shown the C-QTc modeling approach to be concordant with dedicated QTc studies for evaluating the QTc effect in early phase I clinical trials [8, 9]. However, as supratherapeutic concentrations of vericiguat could not be investigated clinically in healthy volunteers owing to the risk of orthostatic reactions, the potential for proarrhythmic risk was investigated in an extended non-clinical package at supratherapeutic concentrations: neither vericiguat nor its pharmacologically inactive major N-glucuronide metabolite inhibited cardiac ion channels (hERG, hNav1.5, or hKvLQT1/mink) at substantial multiples of their unbound maximum concentration values [11], and no clinically relevant QTc effect was observed in a study of vericiguat in conscious telemetered Beagle dogs [11]. Safety findings from the phase III VICTORIA study, which evaluated the effect of vericiguat (2.5 mg once daily, titrated to a target dose of 10 mg) in 5050 patients with HF and EF < 45%, and a recent worsening HF event [3], did not indicate an increased incidence of cardiac arrhythmias in patients treated with vericiguat compared with those receiving placebo. The integrated risk assessment of non-clinical and clinical data supports the conclusion that there was no evidence of proarrhythmic risk associated with vericiguat at the recommended target dose of 10 mg once daily [1].
5 Conclusion
This C-QTc analysis complemented the statistical evaluations of QT/QTc interval prolongation in the dedicated QTc study, which excluded a clinically relevant QTc effect within the plasma concentration range associated with the recommended target dose of vericiguat 10 mg once daily. This was achieved by applying two approaches that integrated all available individual non-treatment data for baseline correction, where one approach considered all baselines simultaneously. Both C-QTc approaches demonstrated a positive (but not clinically relevant) relationship between ΔΔQTcF and vericiguat plasma concentration and led to similar results, thereby confirming the clinical conclusions from the primary statistical analysis.
References
Food and Drug Administration. VerquvoTM (vericiguat) tablets. Highlights of prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214377s000lbl.pdf. Accessed 11 May 2022.
Bayer plc. Verquvo 10 mg film-coated tablets Summary of Product Characteristics. 2021. https://www.medicines.org.uk/emc/product/12775/smpc#gref. Accessed 27 Aug 2021.
Armstrong PW, Pieske B, Anstrom KJ, Ezekowitz J, Hernandez AF, Butler J, et al. Vericiguat in patients with heart failure and reduced ejection fraction. N Engl J Med. 2020;382(20):1883–93.
European Medicines Agency. ICH topic E 14. The clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs. 2005. https://www.ema.europa.eu/en/documents/scientific-guideline/ich-e-14-clinical-evaluation-qt/qts-interval-prolongation-proarrhythmic-potential-non-antiarrhythmic-drugs-step-5_en.pdf. Accessed 1 Dec 2022.
European Medicines Agency. ICH guideline E14/S7B on clinical and nonclinical evaluation of QT/QTc interval prolongation and proarrhythmic potential- questions & answers. 2020. https://www.ema.europa.eu/en/documents/scientific-guideline/ich-guideline-e14/s7b-clinical-nonclinical-evaluation-qt/qtc-interval-prolongation-proarrhythmic-potential-questions-answers-step-2b_en.pdf. Accessed 1 Dec 2022.
Böttcher M, Dungen HD, Corcea V, Donath F, Fuhr R, Gal P, et al. Vericiguat: a randomized, phase Ib, placebo-controlled, double-blind, QTc interval study in patients with chronic coronary syndromes. Am J Cardiovasc Drugs. 2023;23(2):145–55.
Food and Drug Administration. E14 clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs—questions and answers (R3) guidance for industry. 2017. https://www.fda.gov/media/71379/download. Accessed 11 May 2021.
Gaitonde P, Huh Y, Darpo B, Ferber G, Heimann G, Li J, et al. Cardiac risk assessment based on early Phase I data and PK-QTc analysis is concordant with the outcome of thorough QTc trials: an assessment based on eleven drug candidates. J Pharmacokinet Pharmacodyn. 2019;46(6):617–26.
Fostvedt LK, Shaik N, Martinelli G, Wagner AJ, Ruiz-Garcia A. Exposure-response modeling of the effect of glasdegib on cardiac repolarization in patients with cancer. Expert Rev Clin Pharmacol. 2021;14(7):927–35.
Garnett C, Bonate PL, Dang Q, Ferber G, Huang D, Liu J, et al. Scientific white paper on concentration-QTc modeling. J Pharmacokinet Pharmacodyn. 2018;45(3):383–97.
Himmel H, Lagrutta A, Vömel M, Amin R, Imredy J, Johnson T, et al. Nonclinical cardiovascular assessment of the soluble guanylate cyclase stimulator vericiguat. J Pharmacol Exp Ther. 2023;386(1):26–34.
Acknowledgements
Data from this study were presented in part at the European Society of Cardiology Congress 2021. The authors would like to thank the patients involved in this study. Data collection was conducted by Janine North, Bayer AG, Berlin, Germany. Dr Valentin Demmel of Nabios GmbH, Munich, Germany, was responsible for the central analysis of the triplicate ECGs, including recoding, automated and manual reading, evaluation, and data transfer to the US FDA. Medical writing support, including assisting authors with the development of the outline and initial draft, and incorporation of comments, was provided by Fiona Van, PhD, and editorial support was provided by Ian Norton, PhD, both of Scion, London, UK, supported by Bayer AG and Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, according to Good Publication Practice guidelines (https://www.acpjournals.org/doi/10.7326/M15-0288). Bayer AG and Merck & Co., Inc., Rahway, NJ, USA, were involved in the study design, collection, analysis, and interpretation of data, as well as data checking of information provided in the manuscript; however, ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Hauke Ruehs, Matthias Frei, Alexander Solms, Corina Becker, Dirk Garmann, and Michaela Meyer are employees of Bayer AG and may own stock in the company. Maria E. Trujillo is an employee of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA, and and may own stock in Merck & Co., Inc., Rahway, NJ, USA.
Funding
Funding for this research was provided by Bayer AG, Berlin, Germany, and Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA.
Availability of data and material
Availability of the data underlying this publication will be determined according to Bayer’s commitment to the EFPIA/PhRMA ‘Principles for Responsible Clinical Trial Data Sharing’. This pertains to scope, time point, and process of data access. As such, Bayer commits to sharing, upon request from qualified scientific and medical researchers, subject-level clinical trial data, study-level clinical trial data, and protocols from clinical trials in patients for medicines and indications approved in the United States (US) and European Union (EU) as necessary for conducting legitimate research. This applies to data on new medicines and indications that have been approved by the EU and US regulatory agencies on or after 1 January 2014. Interested researchers can use http://www.vivli.org to request access to anonymized subject-level data and supporting documents from clinical studies to conduct further research that can help advance medical science or improve patient care. Information on the Bayer criteria for listing studies and other relevant information is provided in the Study sponsors’ section of the portal. Data access will be granted to anonymized subject-level data, protocols, and clinical study reports after approval by an independent scientific review panel. Bayer is not involved in the decisions made by the independent review panel. Bayer will take all necessary measures to ensure that participant privacy is safeguarded.
Code availability
The R code used to analyze the data is available upon reasonable request by email to the corresponding author.
Modeling software
The analysis was conducted using linear mixed-effects algorithms implemented in the lme4 or nlme R-packages (R, the R Foundation for Statistical Computing, version 3.2.5, lme4 version1.1-11) with the Navigator workbench (Mango solutions, version 9.4.2) on a Red Hat Enterprise Linux 6.3 environment.
Author contributions
All authors contributed to the conception, design, or planning of the study. Corina Becker contributed to the acquisition of the data. Hauke Ruehs performed the data analysis and all authors contributed to the interpretation of the data. All authors contributed to writing the manuscript, commented on previous versions of the manuscript, and read and approved the final manuscript.
Ethics approval
This study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and the International Conference on Harmonisation (ICH) guideline E6: Good Clinical Practice (GCP), and met all local legal and regulatory requirements.
Consent to participate
All subjects provided informed consent.
Consent for publication
Responsibility for opinions, conclusions, and data interpretation lies with the authors, and all authors provide consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ruehs, H., Solms, A., Frei, M. et al. Assessing QTc Effects of Vericiguat Using Two Different Concentration-QTc Modeling Approaches. Clin Pharmacokinet 62, 1639–1648 (2023). https://doi.org/10.1007/s40262-023-01282-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01282-y