Abstract
Background and Objective
Information on the distribution of chemotherapeutic drugs to breast milk is scarce, and reports are limited to small sample sizes. Anecdotal pharmacokinetic data have typically been acquired from lactating but non-breastfeeding patients who collect breast milk by means of an expression pump, which might not necessarily be representative for a breastfeeding population due to differences in milk production. Consequently, little is known about the variability of chemotherapy distribution to breast milk and the effect of milk production on the distribution of chemotherapy to breast milk. Our aim was to predict chemotherapy distribution to breast milk in a more realistic breastfeeding population and evaluate the effect of discarding breast milk on the potential chemotherapy exposure in infants.
Methods
We developed a population pharmacokinetic model that described the breast milk production and the chemotherapy distribution to breast milk of a non-breastfeeding population, linked it to plasma pharmacokinetics, and extrapolated this to a breastfeeding population.
Results
We found that cumulative relative infant doses (RID) were higher than 10% for cyclophosphamide and doxorubicin and approximately 1% for paclitaxel. Simulations allowed us to predict the cumulative RID and its variability in the population for patients with different milk productions and the amount of breast milk that has to be discarded to reach cumulative RIDs below 1%, 0.1%, and 0.01%. Discarding 1–2, 3–6, and 0–1 days of breast milk (depending on the milk production of the patient) resulted in cumulative RID below 1% for cyclophosphamide, doxorubicin, and paclitaxel, respectively.
Conclusion
Our results may help clinicians to derive the optimal breast milk discarding strategy for an individual patient that wants to breastfeed during chemotherapy and minimize chemotherapy exposure in their infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We identified breast milk discarding scenarios, enabling a potentially safe combination of breastfeeding and chemotherapy infusion with minimized risks for the infant. Our results can support clinicians in making more informed and individualized estimations of the possible chemotherapy exposure to infants breastfed by mothers treated with chemotherapy, and thereby develop a strategy of intermediate breastfeeding between chemotherapy cycles to minimize risks. |
1 Introduction
Recently, we summarized a limited number of case reports that described the distribution of chemotherapy to breast milk, on which current recommendations not to breastfeed during chemotherapy are based. In the case series, new data were contributed to the distribution of several chemotherapies to the breast milk [1]. Consequences of chemotherapy on breastfeeding involve patients having to express breast milk during long periods of time, which can be tiring and might lead to decreased milk production or complete lactation cessation. Consequently, only 10% of patients diagnosed with breast cancer during pregnancy end up breastfeeding [2]. Additionally, breastfeeding offers overwhelming benefits to both mother and infant. The most important benefits are the contribution to complete psychological rehabilitation for cancer survivors and the reduction of the infant mortality during the first year of life [3]. On the basis of collected pharmacokinetic data in expressed and collected breast milk during chemotherapy, we previously suggested that breastfeeding during chemotherapy treatment might be safe and feasible when breast milk is discarded 3, 5, and 1 day(s) after administration for cyclophosphamide, doxorubicin and paclitaxel, respectively. Then again, it is important to take into consideration other pharmacological characteristics of the used drugs, such as oral bioavailability and drug metabolism in infants.
Although the previously reported results gave more insight in the amounts of chemotherapy that distributes to the breast milk, the non-compartmental analysis approach, with at most two patients per drug, was unable to explore variability within the population, and therefore lacks the possibility to be extrapolated over a wider range of patients with different demographic properties. In addition, no plasma samples were available to establish a milk-to-plasma ratio for the different drugs. Information on the effects of demographic properties on chemotherapy concentrations in plasma are abundant, and a known milk-to-plasma ratio can facilitate extrapolation of these demographic properties to chemotherapy concentrations in breast milk. Another essential point is that breast milk production by non-breastfeeding mothers in an experimental context is not representative, and likely lower, compared with milk production of mothers fully breastfeeding their infant, which complicates the predictions on the basis of the previously collected breast milk pharmacokinetics (PK). Milk production in healthy women is stimulated and maintained by regular removal of milk from the breast by means of suckling, which stimulates the nipple and triggers prolactin release [4]. Previously reported data concern patients expressing milk by means of a pump, and although this method also stimulates the nipple, the stimulating effect of combined movement of the infants lips, tongue, and jaw cannot be matched [5]. More importantly, pumping breast milk approximately ten times a day is a demanding process that is difficult to sustain, especially during chemotherapy treatment [2]. Subsequently, non-breastfeeding mothers have more difficulties with sustaining the same level of breast milk productions due to lower expression frequencies [6].
The aim of the current study was to predict chemotherapy distribution to breast milk for a breastfeeding population by extrapolating experimental data of non-breastfeeding patients and linking it to plasma PK. With the resulting predictions, we made an assessment of the potential chemotherapy exposure in infants and the risk reducing effect of discarding days of breast milk after maternal administration of chemotherapy. Hereby, we aim to aid patients and clinicians in making an informed decision about possible risks of chemotherapy exposure to the infant for women that want to breastfeed their infant during the treatment for cancer.
2 Methods
2.1 Data
Three patients diagnosed with breast cancer who received doxorubicin or epirubicin in combination with cyclophosphamide once every 2 weeks for 8 weeks, followed by carboplatin once every 3 weeks and paclitaxel every week for 12 weeks were included. Patient 1 received a dose of 118 mg, 1180 mg, and 156 mg for doxorubicin, cyclophosphamide, and paclitaxel, respectively. Patient 2 received a dose of 130 mg and 1300 mg for doxorubicin and cyclophosphamide, respectively. Patient 3 received a dose of 130 mg and 1060 mg for epirubicin and cyclophosphamide, respectively. Both patient 2 and 3 did not collect samples during paclitaxel treatment. Patients collected 24-h samples of breast milk every day for 1–4 months during chemotherapy treatment. The patients recorded date, time, and volume after each expression of breast milk, after which breast milk was put in storage bags and frozen in the freezer of the patient. Once the samples arrived at the laboratory, a selection of the samples was analyzed for cyclophosphamide, doxorubicin, and paclitaxel. A more detailed description of sampling and bioanalytical method can be found in Damoiseaux et al. [1]. Samples of patients that were below the lower limit of quantification (LLOQ) in the elimination phase were handled as missing data values.
2.2 Structural Model for Milk Production of Non-breastfeeding Patients
First, a structural model for milk production of non-breastfeeding patients was developed, which was later used to make an extrapolation to a breastfeeding population. To characterize the observed breast milk volumes of non-breastfeeding patients treated with chemotherapy over time, all available milk volumes, dates, and times of milk expression recorded by the patients were used. We aimed to develop a model that was as physiologically accurate as possible, without making the model unnecessarily complicated. The main trends in the observed longitudinal breast milk volume data that we tried to describe were: (1) a decreased milk production over time, and (2) a decreased milk production associated with accumulation of milk in the breast. The expressed milk volumes were highest at the start of sampling for all patients, the milk production then decreased to a steady-state milk production (SSMP) over time (Fig. 1). The decrease in the milk production rate (MP) with the dimension volume per time was described using a first order rate constant:
where θCMP is the typical value for change in milk production from start of sampling until SSMP and θCMPR is the typical value for the first order rate constant determining the change in MP over t (time).
The individual total daily (red) and separately sampled (blue) volumes (in mL) of breast milk over time (in days) for patients 1, 2, and 3. Trend lines represent the decline in daily milk production over time until a steady-state milk production is reached (if applicable) and vertical lines represent the start of a new chemotherapy combination. Patients 2 and 3 only received one combination of chemotherapies
MP also decreases between expressions of breast milk. Daly et al. showed that milk production decreases with increased time since last milk expression, suggesting that milk production decreases as milk accumulates in the breast [7]. To account for this, a decrease in MP was modeled when the maximum breast capacity (MBC) was approached:
With an exception for Vmilk = 0, which results in dVmilk/dt = MP. Where MP represents the milk production rate, θMBC represents the typical value for the MBC, and Vmilk the volume of milk in the breasts. At last, maternal sampling times were considered as timepoints at which the entire breast was emptied. To mimic this process, the milk volume compartment was reset to zero at sampling times.
In the stochastic model, between subject variability (BSV) was estimated using an exponential model (Eq. 3):
where θi represents the parameter estimate for individual i, θpop represents the typical population parameter estimate, and ηi represents the BSV effect for individual i with a distribution following N(0, ω2).
Residual unexplained variability (RUV) was described using an additive error model (Eq. 4) for the milk production model and a proportional error model for the chemotherapy distribution to breast milk models (Eq. 5):
where Cobs,ij represents the observation for individual i and measurement j, Cpred,ij represents the prediction and εadd,ij and εprop,ij represents the additive and proportional error, respectively, distributed following N (0, σ2).
2.3 Structural Models for Chemotherapy Plasma-Breast Milk Distribution
The observational nature of the previously described case series did not allow the collection of additional materials, besides breast milk samples [1]. Because of this, we lacked plasma concentrations to develop a base model to work from. We therefore started model development from previously established population PK models of doxorubicin [8], cyclophosphamide [9], and paclitaxel [8] that describe the plasma PK in humans. For doxorubicin, the base literature model consisted of three compartments. For paclitaxel, the model consisted of a three-compartment model with Michaelis–Menten elimination, and saturable distribution to one peripheral compartment. For cyclophosphamide, the model consisted of a single compartment. Due to missing patient demographics, we were unable to predict patient plasma exposures using the available covariates in the base models. We therefore chose to use typical plasma PK parameters to describe the plasma PK and removed BSV. Between-occasion variability in the maximal elimination rate and volume of distribution of the central compartment in the paclitaxel model were preserved to account for between-occasion variability that was observed in the paclitaxel containing breast milk observations. We reasoned that this variation was more likely to originate from between-occasion fluctuations in the plasma, rather than only residual variability in breast milk observations.
These models were then extended with breast milk compartments for volumes (Vmilk) and chemotherapy amounts in breast milk (Amilk). The input for Vmilk was described by the milk production model, for which typical values of all parameters were estimated for each patient separately to give the most accurate approximation of collected breast milk volumes per patient. Subsequently, Amilk was added to the model and parameters for the distribution of doxorubicin, cyclophosphamide, and paclitaxel to the breast milk were estimated.
The volumes in Vmilk represent the volumes of milk that were expressed and measured by the patients, and these volumes might not have been representative for the volume of distribution of the drugs within the breast and breast milk. Therefore, a milk volume ratio (Vratio) was evaluated to describe a ratio between Vmilk and the volume of distribution in breast milk. Secondly, the two processes, namely passive diffusion and active transport, were evaluated to describe the distribution of doxorubicin, cyclophosphamide, and paclitaxel to the breast milk. The passive diffusion was described with an intercompartmental clearance (Q) where the distribution constant from the milk compartment to the central compartment was Q divided by Vmilk (the volume of milk in the breast compartment) at the given time, multiplied by Vratio (if applicable). The active transport was described by a saturable transport using the Michaelis–Menten equation for which the PK variables maximal transport rate (VMTR) and the Michaelis–Menten constant (KMTR) were estimated.
Finally, the individual predictions of chemotherapy concentrations in breast milk were calculated by dividing Amilk by Vmilk. Similarly, as in the milk production model, maternal sampling times were considered timepoints at which the entire breast was emptied. To mimic this process, the milk volume compartment and the milk amount compartment were reset to zero at sampling times.
2.4 Model Selection and Evaluation
Models were evaluated by assessing individual predictions and observations versus time plots, goodness-of-fit (GOF) plots, change in objective function value (dOFV), and successful minimizations. dOFVs, following a chi-squared distribution, were considered significant for hierarchical models when < −6.64 (p < 0.01, 1 degree of freedom) or < −9.21 (p < 0.01, 2 degrees of freedom). Parameter estimate precisions were assessed using sampling importance resampling.
2.5 Extrapolation of Milk Production to a Breastfeeding Population
Samples were collected in patients with decreased milk production caused by either chemotherapy treatment, expressing breast milk by means of a pump (no stimulation by means of suckling of the nipple), or both. To evaluate what amount of chemotherapy distributes to the breast milk in the hypothetical situation in which a patient is able to fully breastfeed her infant, we simulated several individuals (IDs) with different MPs and MBCs (Table 1). For the simulations, MPs and MBCs comparable to that in healthy mothers were used, where the storage capacity of each breast is 179 ± 59 g (range 74–382 g) and the overall 24-h milk production for both breasts combined is 788 ± 169 g (range 478–1356 g), with a correlation between the two [10]. Despite the correlation between MP and MBC, we chose to simulate patients with opposite extremes of MP and MBC observed in healthy mothers, since both parameters could possibly be affected by chemotherapy treatment resulting in unexpected combination of parameters. No decrease or rise of MP over time was simulated (CMP and MRPC of 0). Infants between 1 and 6 months of age consume 64% (497 ± 17 g) of its daily milk consumption between 6 AM and 6 PM, and the other 36% (275 ± 13 g) between 6 PM and 6 AM over 6.8 ± 0.3 and 4.0 ± 0.2 feedings, respectively [10]. Within the simulations, the breast compartments for both volumes and amounts were therefore reset 6.8 ± 0.3 times, evenly distributed over the first 12 h of each day and 4.0 ± 0.2 times evenly distributed over the last 12 h of each day; these timepoints were also considered feeding times.
2.6 Simulation of Chemotherapy Distribution to Breast Milk in a Breastfeeding Population
Start of chemotherapy infusion was considered 6 AM on the first day. Simulated patients were administered an intravenous dose of 600 mg/m2, 60 mg/m2, and 80 mg/m2, with an infusion time of 2 h, 2 h, and 3 h, for cyclophosphamide, doxorubicin, and paclitaxel, respectively (patient body surface area of 1.7 m2). A total of 500 simulations for cyclophosphamide, doxorubicin, and paclitaxel were performed. Subsequently, the infant daily dose was calculated on the basis of the simulation output by taking the sum of the amount of chemotherapy in all breast milk feeds of the day, divided by the weight of the infant. The body weight of the infant used in the calculations was 4 kg. Two different situations were evaluated: the amount of chemotherapy in all available breast milk and the amount of chemotherapy in 67.3 ± 7.8% of the available breast milk (in line with the average amount of breast milk an infant consumes from the available breast milk at the beginning of the breastfeeding [10]). With the infant daily dose, the relative infant dose (RID) was calculated:
.
The daily RID is the relative amount of drug to which an infant is exposed on a specific day compared with the maternal dose. The maternal body weight used in the calculations was 70 kg.
At last the cumulative RID, the sum of the daily RIDs in a cycle of chemotherapy, was calculated:
where n represents the number of days in the chemotherapy cycle concerned, 7 days for paclitaxel, and 14 days for cyclophosphamide and doxorubicin.
Finally, an overview of the number of days after the start of administration, at which breast milk has to be discarded to reach a cumulative RID below 1%, 0.1%, and 0.01% for cyclophosphamide, doxorubicin, and paclitaxel, respectively, was established. Values of 1%, 0.1%, and 0.01% were chosen for demonstration purposes.
2.7 Software
Nonlinear mixed-effects modeling was performed using NONMEM (version 7.5, ICON Development Solutions, Ellicott City, MD, USA) and Perl-speaks-NONMEM (PsN, version 5.4.0). Pirana (version 2.9.9) was used as the graphical user interface for NONMEM, and R (version 4.2.0) was used for processing the data and graphical and statistical diagnostics.
3 Results
A total of 302, 133, and 131 breast milk samples were collected for patients 1, 2, and 3, respectively (Fig. 1). A selection of 15 samples was analyzed for both doxorubicin and cyclophosphamide in both patients 1 and 2. Of the 30 analyzed samples for cyclophosphamide, 24 samples were below the LLOQ. For paclitaxel a selection of 26 samples was analyzed in patient 1 over three cycles.
3.1 Milk Production Model
Breast milk volumes expressed by three patients with breast cancer treated with chemotherapies was best described by a milk production that was dependent on both MBC and time. A MP that decreased as the MBC of 175 mL was approached (Eq. 2) resulted in a greatly improved fit with a ΔOFV of −653 (1 degree of freedom, p < 0.005). In addition, a CMP of 55 mL/h, until the SSMP of 5.87 mL/h was reached, with a CMPR of 0.0029 1/h (Eq. 1) greatly improved the model fit with a ΔOFV of −294 (2 degrees of freedom, p < 0.005). Due to the high variation within the breast milk samples, BSV was included in the model for all parameters, again greatly improving the model fit with a ΔOFV of −414 (4 degrees of freedom, p < 0.005). Addition of BSV resulted in the final parameter estimates presented in Table S1. Individual predictions and observations of the milk volumes in the breast versus time and GOF plots show adequate description of the data, despite high residual error for several samples (Figs. S1–2). However, high residual errors were expected because of the many variables that influence day-to-day milk production. Estimation of SSMP was difficult for a combined model of all patients because patient 2 did not reach a SSMP before she stopped collecting milk samples. For this reason and because accurate volumes of milk had to be predicted per patient to adequately estimate parameters involved in the distribution of chemotherapy to breast milk we decided to separately estimate the fixed effects for each patient (Table 2). Figure 2 clearly shows the improved predictions of the first and fourth week of sampled breast milk volumes by the milk production model, with separately estimated fixed effects for each patient (Fig. 2B) compared with the original milk production model (Fig. 2A).
Predictions of the first and fourth week of sampled breast milk volumes by A the milk production model and B the milk production model with separately estimated fixed effects for each patient. We chose to only show the predictions of the first and fourth week to keep the figure comprehensive and to give an idea of the model performance. Red triangles represent the observations, black lines represent the median predictions, and the blue areas represent the 80% prediction intervals. Predictions consisted of 250 simulations each
3.2 Chemotherapy Distribution to Breast Milk Model
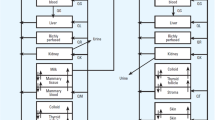
Base models from literature were extended with two additional compartments, one for the volume of breast milk and one for the amount of chemotherapy in breast milk. The distribution of cyclophosphamide to breast milk was best described with only a passive diffusion of 814 L/h. The distribution of doxorubicin to breast milk was best described with a passive diffusion of 618 L/h, combined with a saturable transport to the breast milk (VMTR of 290 µg/h and a KMTR of 0.013 µg/L), resulting in a ΔOFV of −136 (2 degrees of freedom, p < 0.005) and a Vratio (7.26-fold) resulting in a ΔOFV of −76 (1 degree of freedom, p < 0.005). At last, the distribution of paclitaxel to breast milk was best described with a passive diffusion of 2.06 L/h combined with a saturable transport to the breast milk (VMTR of 1.2 µg/h and a KMTR of 0.012 µg/L), resulting in a ΔOFV of −119 (2 degrees of freedom, p < 0.005). No BSV was included in the model. The final parameter estimates are summarized in Table 2 and GOF, VPC, and a schematic model structure are presented in Figs. S3–5 showing adequate description of the data.
3.3 Simulations
Simulations of the population PK model for the distribution of cyclophosphamide, doxorubicin, and paclitaxel to breast milk for nine IDs (Table 1), with different parameter values for milk production and MBC, resulted in the lowest median milk production for ID 1 of 527 mL per day and the highest median milk production for ID 9 of 1170 mL per day (Fig. S6). In Fig. 3 and Fig. S7, the concentration–time curves of the distribution of cyclophosphamide, doxorubicin, and paclitaxel to breast milk are presented for ID 5 (steady-state milk production of 32.8 mL/h and an maximal breast capacity of 358 mL); similar concentrations were observed for the other IDs. To put the simulated concentrations of chemotherapy in breast milk into the perspective of maternal dose, the cumulative RIDs were calculated and presented in Fig. 4 for ID 5. In addition, Fig. 4 shows the number of days that have to be discarded to minimize exposure of the infant to cumulative RIDs below thresholds of 1% and 0.1%. Because of the lack of information regarding safe doses of oral chemotherapies (in breast milk) in infants, we choose to show the cumulative RIDs of each chemotherapy, and the number of days that breast milk has to be discarded to reach a cumulative RID below 1%, 0.1%, and 0.01% at the end of each cycle for each simulated ID, as well as the 95% confidence intervals (Table S2 and Fig. 5). Higher milk production resulted in a higher cumulative RID (ID 1, 2, and 3 versus ID 4, 5, and 6 versus ID 7, 8, and 9). In contrast, higher MBC resulted in only a small increase in cumulative RID for cyclophosphamide in combination with the highest milk production of 50 mL/h (ID 7 versus ID 8 versus ID 9).
Simulated median concentrations of cyclophosphamide, doxorubicin, and paclitaxel in breast milk over 3 days, with 80% prediction interval in blue. A total of 500 simulations were performed for a virtual patient with an average steady-state milk production of 32.8 mL/h and an average maximal breast capacity of 358 mL, expressing breast milk seven times between 6 AM and 6 PM and four times between 6 PM and 6 AM. The patient was administered an intravenous dose of 600 mg/m2, 60 mg/m2, and 80 mg/m2 with an infusion time of 2 h, 2 h, and 3 h for cyclophosphamide, doxorubicin, and paclitaxel, respectively (patient body surface area of 1.7 m2)
Simulated cumulative RIDs in breast milk for cyclophosphamide, doxorubicin, and paclitaxel for a virtual patient with an average steady-state milk production of 32.8 mL/h and an average maximal breast capacity of 358 mL with a different amount of days of discarded breast milk. The amount of discarded days of breast milk was based on the amount of days in a cycle of chemotherapy, 14 days for cyclophosphamide and doxorubicin, and 7 days for paclitaxel. Box plots in blue represent the cumulative RIDs in the total volume of milk produced in 1 day, and red represents cumulative RIDs in the volume of milk that is consumed by the average infant in 1 day
A The milk production for each simulated individual, B the cumulative RID for each drug and individual with 95% confidence interval, and C the number of days after the start of maternal chemotherapy administration, for which breast milk has to be discarded to reach a cumulative RID below 1%, 0.1%, and 0.01% (and 95% prediction interval) for the different compounds, with the assumption that the infant drinks all the available milk produced by the nine IDs with corresponding milk production parameters (C). Cumulative RID is calculated until the end of a cycle, 7 days after administration for paclitaxel, 14 days after administration for cyclophosphamide and doxorubicin. Missing averages (dots) and error bars that reach 14 days for doxorubicin and 7 days for paclitaxel indicate that the cumulative RID did not reach this value (< 1%, 0.1%, or 0.01%) within the duration of a cycle (C). The different IDs originate from Table 1. RID relative infant dose
4 Discussion
We developed an approach to extrapolate the distribution of chemotherapy to breast milk in non-breastfeeding to breastfeeding women treated with chemotherapy. Predictions of the population PK model revealed that concentrations in breast milk declined fast after administration (Fig. 3). Despite the rapid decline in concentrations, cumulative RIDs higher than 10% were predicted for doxorubicin and cyclophosphamide if breastfeeding was not interrupted after administration, which is higher than previously found in the case series where the cumulative RIDs did not exceed 10% [1]. This suggests that a non-compartmental analysis of the experimental data from non-breastfeeding patients gives an under prediction of the breast milk exposure in a breastfeeding population. The effect of discarding days of breast milk to reduce infant exposure to chemotherapy, however, resulted in similar amounts of days that have to be discarded to reach cumulative RIDs lower than 1% and 0.1% for cyclophosphamide, doxorubicin, and paclitaxel (Table S2 and Fig. 5). Previously, no variability in the population was reported; our results show that, especially for doxorubicin, variability within the plasma exposure results in a broad range of days that have to be discarded to reach a cumulative RID below 1% or 0.1%. Results indicate that at least for cyclophosphamide and paclitaxel, intermediate breastfeeding between chemotherapy cycles could be possible, while for doxorubicin it is important to first determine to what extent the patient is exposed systemically to have an indication of the exposure in breast milk.
As previously highlighted, the cumulative RID represents a first step to infer infant exposure to chemotherapy [1]. However, the extent of chemotherapy exposure of the infant is dependent on more factors. Other processes, such as immature metabolism, absorption, and other PK processes can result in unexpected differences in oral bioavailability compared with adults and should be taken into consideration [11]. Besides, pharmacodynamic differences between adults and infants can differ as well, and as a consequence even low cumulative doses might result in potential gastrointestinal toxicity, hematological toxicity, and alterations in infant microbioma.
Drug transfer to breast milk takes place from maternal capillaries surrounding milk producing mammary epithelial cells (lactocytes) in the breast. Two pathways mainly govern drug distribution between plasma and breast milk; passive diffusion both in and out of the breast milk and active secretion into the breast milk via transporters. Passive diffusion between blood and breast milk is dependent on pKa, lipophilicity of the drug, and plasma protein binding [12]. Breast milk fat content changes over time but is higher than in plasma, and lipid-soluble drugs may concentrate in the breast milk. All factors considered, protein binding appears to have the most potent effect on drug distribution. With an almost ten-fold higher protein concentration in plasma compared with breast milk, highly protein-bound drugs tend to remain in plasma and only marginally distribute to breast milk. In addition to passive distribution, active transport is believed to play a role for a subset of drugs, as messenger RNA (mRNA) levels of several transporters have been detected in lactocytes, including members of the ATP-binding cassette (ABC) and solute carrier (SLC) super families [13]. Furthermore, excretion of drug metabolites in human milk was not included in this study due to absence of metabolite data in breast milk; this is especially important for the active metabolite doxorubicinol, which has a similar toxicity profile as doxorubicin and also distributes to human milk [14], and should be considered when interpreting the results for doxorubicin.
We observed that the milk volumes sampled per day by patients that expressed milk by means of a pump declined after the initiation of breast milk expression and start of chemotherapy treatment. Reports are available of mothers treated with chemotherapy during pregnancy that reported problems with initiation of breast milk production postpartum, but not necessarily in maintaining milk production [11]. Since initial milk production was high, the decline in milk production more likely originates from a lack of regular removal of milk from the breast by means of suckling, which is known to help stimulate and maintain milk production [4]. Either way, the decline in milk production within this population was something to take into account during the development of the model as volumes declined considerably, which could result in inaccurate predictions for the amount of chemotherapy in breast milk in a breastfeeding population. In the simulations we therefore assumed the hypothetical situations in which mothers are able to fully breastfeed their infant by fixing the CMP and CMPR to zero. This is also a limitation of the simulations, since there is a possibility that chemotherapy treatment is the main contributor for a decrease in milk production over time. If this is the case, the same decrease in milk production over time can be expected in a breastfeeding population. Nevertheless, we present different levels of milk production and lower milk production results in lower cumulative RIDs. In the worst case scenario, we therefore make an over prediction of the possible exposure to the infant, thereby limiting breastfeeding possibilities rather than underestimating the risk of exposure. Additionally, if in the future a clear relationship is found between chemotherapy treatment and milk production over time, both CMP and CMPR can be adjusted accordingly to optimize predictions. Another limitation of the data was the small sample size and absence of plasma concentrations, resulting in a restricted clinical applicability without the option to make individualized recommendations. However, it should be mentioned that obtaining a small sample size within this population, in which hardly any information is available, is highly challenging and very valuable. It concerns a population diagnosed with cancer and treated with chemotherapy, while caring for an infant. To combine this with the intense sampling (milk has to be collected by means of a pump up to 12 times a day, samples have to be labelled and stored during a period of 1–4 months) that is required for this research is therefore very demanding. Nevertheless, to work around this limitation, we used typical parameter estimates of plasma PK models from literature as a base model to start from. In this way, the variability found in plasma could be extrapolated to concentrations found in breast milk, and a relation between plasma and breast milk exposure could be determined. However, a disadvantage of this approach is the assumption that our population showed typical plasma exposures, possibly resulting in under predictions in case actual plasma exposure was low within these patients. Distribution to breast milk turned out to be highly dependent on plasma concentrations based on the estimates of the intercompartmental distribution, especially for cyclophosphamide and doxorubicin. Well perfused blood vessel capsules, surrounding the small volume alveolus in the mammary gland, give a large plasma to milk surface area, which explains the quick distribution between plasma and milk [15]. Ideally, estimates should be updated in the future with additional data to optimize the predictions of chemotherapy distribution to breast milk, since the model was developed based on a limited amount of individuals. Another essential point is the high uncertainty in the model. Uncertainty arises from the small sample size and high residual errors for milk volumes and the distribution of cyclophosphamide to breast milk. Inclusion of these errors in the simulations have led to relatively wide prediction intervals (Fig. 5). From a clinical point of view, the upper limits of the prediction interval are obviously most important, given the safety considerations. Furthermore, we found that a saturable transport from plasma to breast milk significantly improved the model fit for doxorubicin and paclitaxel. The effect of the saturable transport on the distribution to breast milk plays a role at lower plasma concentrations and results in higher exposure in breast milk; however, because only the low concentrations are concerned, the clinical significance will be small. At higher concentrations distribution to breast milk is mainly dependent on the intercompartmental clearance.
To conclude, the results identified breast milk discarding scenarios, enabling a potentially safe combination of breastfeeding and chemotherapy infusion with minimized risks for the infant. A breastfeeding population treated with cyclophosphamide, doxorubicin, or paclitaxel minimizes the exposure to the infant by discarding breast milk after the administration of chemotherapy. Exposure of cyclophosphamide and paclitaxel is negligible after discarding breast milk for only 2 days, while doxorubicin should be discarded for at least 6 days. Figure 5 provides an overview for clinicians of predicted cumulative RIDs, with the expected variation within a breastfeeding population for different levels of milk production as well as the days of breast milk that have to be discarded to minimize infant exposure. This table can support clinicians in making more informed and individualized estimations of the possible chemotherapy exposure to infants breastfed by mothers treated with chemotherapy and thereby develop a strategy of intermediate breastfeeding between chemotherapy cycles to minimize risks. Nevertheless, results from this model-based study are a first attempt based on limited available data; therefore, caution in interpretation of the prediction intervals is advised and pharmacological characteristics of chemotherapy should be considered in decision-making.
Change history
25 May 2023
The original online version of this article was revised to include the electronic supplementary material figures and tables.
16 June 2023
The original online version of this article was revised to include the electronic supplementary material files.
References
Damoiseaux D, et al. Presence of five chemotherapeutic drugs in breast milk as a guide for the safe use of chemotherapy during breastfeeding: results from a case series. Clin Pharmacol Ther. 2022;112(2):404–10.
Lee GE, et al. Contemporary management of breast cancer during pregnancy and subsequent lactation in a multicenter cohort of young women with breast cancer. Breast J. 2019;25(6):1104–10.
Samuel J. Breastfeeding and the empowerment of women. Can Nurse. 1997;93(2):47–8.
Pillay J, Davis TJ. Physiology, lactation, in StatPearls. 2022, StatPearls Publishing Copyright © 2022. Treasure Island: StatPearls Publishing LLC.
Elad D, et al. Biomechanics of milk extraction during breast-feeding. Proc Natl Acad Sci USA. 2014;111(14):5230–5.
Becker GE, Smith HA, Cooney F. Methods of milk expression for lactating women. Cochrane Database Syst Rev. 2016;9(9):Cd006170.
Daly SE, et al. Frequency and degree of milk removal and the short-term control of human milk synthesis. Exp Physiol. 1996;81(5):861–75.
Janssen JM, et al. Population pharmacokinetics of docetaxel, paclitaxel, doxorubicin and epirubicin in pregnant women with cancer: a study from the international network of cancer, infertility and pregnancy (INCIP). Clin Pharmacokinet. 2021;60(6):775–84.
Joerger M, et al. Population pharmacokinetics and pharmacodynamics of doxorubicin and cyclophosphamide in breast cancer patients: a study by the EORTC-PAMM-NDDG. Clin Pharmacokinet. 2007;46(12):1051–68.
Kent JC, et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3):e387–95.
Alcorn J, McNamara PJ. Pharmacokinetics in the newborn. Adv Drug Deliv Rev. 2003;55(5):667–86.
Anderson PO. Drugs in lactation. Pharm Res. 2018;35(3):45.
Nauwelaerts N, et al. A comprehensive review on non-clinical methods to study transfer of medication into breast milk—a contribution from the ConcePTION project. Biomed Pharmacother. 2021;136: 111038.
Codacci-Pisanelli G, et al. Breastfeeding during R-CHOP chemotherapy: please abstain! Eur J Cancer. 2019;119:107–11.
Jones R, Lopez K. Human reproductive biology. 4th ed. London: Elsevier; 2014.
Acknowledgements
This study was supported by a restricted grant from the Estée-Lauder company.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflict of interest
All authors declared no competing interests for this work.
Author contribution
D.D., J.H.B., A.D.R.H., T.P.C.D., and F.A. wrote the manuscript, D.D., T.P.C.D., and A.D.R.H. designed the research, D.D. performed the research, and D.D. analyzed the data. Authors that contributed new reagents/analytical tools is not applicable
Data availability statements
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Ethics approval
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Damoiseaux, D., Centanni, D., Beijnen, J.H. et al. Predicting Chemotherapy Distribution into Breast Milk for Breastfeeding Women Using a Population Pharmacokinetic Approach. Clin Pharmacokinet 62, 969–980 (2023). https://doi.org/10.1007/s40262-023-01251-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01251-5