Abstract
Background and Objective
Many patients treated for COVID-19 related acute respiratory distress syndrome in the intensive care unit are sedated with the benzodiazepine midazolam. Midazolam undergoes extensive metabolism by CYP3A enzymes, which may be inhibited by hyperinflammation. Therefore, an exaggerated proinflammatory response, as often observed in COVID-19, may decrease midazolam clearance. To develop a population pharmacokinetic model for midazolam in adult intensive care unit patients infected with COVID-19 and to assess the effect of inflammation, reflected by IL-6, on the pharmacokinetics of midazolam.
Methods
Midazolam blood samples were collected once a week between March 31 and April 30 2020. Patients were excluded if they concomitantly received CYP3A4 inhibitors, CYP3A4 inducers and/or continuous renal replacement therapy. Midazolam and metabolites were analyzed with an ultra-performance liquid chromatography–tandem mass spectrometry method. A population pharmacokinetic model was developed, using nonlinear mixed effects modelling. IL-6 and CRP, markers of inflammation, were analyzed as covariates.
Results
The data were described by a one-compartment model for midazolam and the metabolites 1-OH-midazolam and 1-OH-midazolam-glucuronide. The population mean estimate for midazolam clearance was 6.7 L/h (4.8–8.5 L/h). Midazolam clearance was reduced by increased IL-6 and IL-6 explained more of the variability within our patients than CRP. The midazolam clearance was reduced by 24% (6.7–5.1 L/h) when IL-6 increases from population median 116 to 300 pg/mL.
Conclusions
Inflammation, reflected by high IL-6, reduces midazolam clearance in critically ill patients with COVID-19. This knowledge may help avoid oversedation, but further research is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inflammation, reflected by high IL-6, reduces midazolam clearance in critically ill patients with COVID-19. |
Renal failure, reflected by high creatinine, reduces 1-OH-midazolam-glucuronide clearance in critically ill patients with COVID-19. |
This knowledge may help to identify critically ill patients with COVID-19 with a reduced midazolam clearance and therefore at risk for oversedation. |
1 Introduction
Current guidelines for the management of pain, agitation, delirium, immobility and sleep (PADIS) in critically ill patients are widely endorsed and applied at Intensive Care Units (ICUs) worldwide. They include aiming for a comfortably awake state, avoiding benzodiazepine-based continuous sedation and other measures in order to avoid or mitigate delirium [1]. However, titrating analgesia and sedation towards wakefulness has been challenging in acute respiratory distress syndrome (ARDS) related to coronavirus disease 2019 (COVID-19) due to frequent application of neuromuscular blockade and prone positioning, requiring higher levels of sedation [2]. This has translated into high incidence of benzodiazepine-related delirium and an increased number of days spent in coma [3]. It seems likely that benzodiazepine drug dosing may have been too high in many patients in circumstances where deep sedation was perceived as essential to avoid patient-ventilator dyssynchrony and ensure patient comfort during proning.
Midazolam, the most used benzodiazepine for continuous intravenous (iv) sedation, undergoes extensive metabolism by hydroxylation via CYP3A enzymes to form mainly the metabolite 1-OH-midazolam and a very small amount of 4-OH-midazolam. After hydroxylation, hydroxymidazolam is subsequently metabolized to chiefly 1-OH-midazolam-glucuronide as its major metabolite and renally excreted. Both an in vitro study and a study in healthy volunteers showed that the metabolites 1-OH-midazolam and 1-OH-midazolam-glucuronide have a sedative potency compared to midazolam of 60-80% and 10%, respectively [4, 5]. Due to the CYP3A-mediated metabolism of midazolam to 1-OH-midazolam, midazolam is a known indicator for human CYP3A4 activity. CYP3A can be down regulated by cytokine release during inflammation resulting in decreased drug clearance [6,7,8,9]. In an in vitro study, it was found that CYP3A4 activity is reduced by 50% (EC50) at an interleukin 6 (IL-6) concentration of 17.1 pg/mL [10]. Furthermore, Vet et al. demonstrated reduced CYP3A-mediated clearance of midazolam in critically ill children with inflammation and organ failure [11].
Since hyperinflammation plays an important role in COVID-19, altered midazolam pharmacokinetics seem likely. Therefore, we aimed to develop a population pharmacokinetic model for midazolam and to assess the effect of inflammation, reflected by IL-6 and C-reactive protein (CRP), on the pharmacokinetics of midazolam administered as continuous infusion to adult intensive care patients with COVID-19 infection. We hypothesized that a strong proinflammatory response reduces midazolam clearance.
2 Methods
2.1 Setting, Patient Selection and Ethics
We performed a prospective observational study between March 31 and April 30 2020 at the tertiary ICU of Erasmus MC University Medical Center (Rotterdam, the Netherlands). At the end of April 2020, we reached the end of the first COVID-19 wave in the Netherlands. As a result, the study population decreased and no more midazolam samples were obtained. Mechanically ventilated adult patients with COVID-19, receiving intravenous midazolam were eligible for participation in the study. Patients were excluded if they concomitantly received strong CYP3A4 inducers (like e.g. rifampicin) and/or inhibitors (like e.g. erythromycin) or continuous renal replacement therapy (CRRT). Patients receiving CRRT were excluded from analysis, since CRRT may interfere with the clearance of the metabolite 1-OH-midazolam-glucuronide and insufficient information (e.g. sieving coefficient) was present to calculate accurately the clearance. The medical research ethics committee approved the study and waived informed consent requirement, given that all data acquired for this study were part of usual care (MEC 2020-0381).
Data were extracted from the electronic medical records for the duration of the midazolam treatment until end of study, including, Richmond Agitation-Sedation Scale (RASS), Acute Physiology and Chronic Health Evaluation (APACHE) IV score, Kidney Disease: Improving Global Outcomes (KDIGO) stage, Sequential Organ Failure Assessment (SOFA) score, serum creatinine, C-reactive protein (CRP) and interleukin (IL)-6, aspartate aminotransferase (ASAT), alanine transaminase (ALAT), bilirubin, albumin and the use of sedative co-medication.
2.2 Sampling and Measurements
Midazolam samples were obtained and analyzed weekly as part of routine clinical care. Blood samples were collected during continuous midazolam infusions or in some cases after withdrawal of the continuous infusion. Blood samples were centrifuged and plasma was refrigerated until analysis. Midazolam, 1-OH-midazolam and 1-OH-midazolam-glucuronide plasma samples were analyzed by means of an FDA-validated method using ultra-performance liquid chromatography–tandem mass spectrometry (UPLC-MS/MS) with electrospray ionization in the positive ionization mode on a Waters Xevo TQ-S micro 1. The limits of quantification of the method were 2-2400 µg/L for midazolam, 3-2300 µg/L for 1-OH-midazolam and 10-3000 µg/L for 1-OH-midazolam-glucuronide. If concentrations exceeded the upper limit of quantification, the calibration curve was used to extrapolate those concentrations.
2.3 Population Pharmacokinetic Analysis
2.3.1 Structural Model and Choice of Statistical Model
The concentrations time profiles of midazolam and the metabolites 1-OH-midazolam and 1-OH-midazolam-glucuronide were analyzed using the nonlinear mixed effects modeling (NONMEM®) approach with first-order conditional estimates (FOCE) with interaction [version 7.44, ICON, Development Solutions, MD, USA]. Pirana [version 2.9.9, Certara, NJ, USA] was used as modeling environment and data were further analyzed and visualized in R [version 3.6.1, R Foundation for statistical computing, Vienna, Austria]. All concentrations of 1-OH-midazolam and 1-OH-midazolam-glucuronide were corrected to their midazolam equivalent using molecular weight. Initially, one-, two- and three-compartment models were tested for midazolam and its metabolites. Subsequently, the metabolites were added to the model in series.
Throughout the process of pharmacokinetic modeling, different mathematical models were fitted to the data to determine which model best described the data. The models were evaluated both numerically, using precision, objective function values (OFV), shrinkage and condition number, and visually using goodness-of-fit plots and visual predictive checks (VPC). A decrease of 3.84 points in OFV for one degree of freedom was considered statistically significant (p < 0.05). Inter-occasion variability (IOV) was evaluated. Constant, proportional and combined error models were evaluated to describe the residual error for midazolam and metabolites (both combined and separately). The inter-individual variability (IIV) on clearance was estimated for midazolam and both metabolites.
2.3.2 Covariate Analysis
The correlation with PK parameters was evaluated for the following covariates: age, gender, weight, body surface area (BSA), APACHE IV score, SOFA score, creatinine, CRP, IL-6, ASAT, ALAT, bilirubin and albumin. Covariate values closest to the time of observation were used for model predictions except for baseline data. Continuous covariates were centered on the median and missing values were carried forward or backward from last observation. When a covariate was entirely missing, it was replaced by the median. The evaluation of covariates was performed using stepwise covariate model building where a decrease of ≥ 3.84 in OFV was considered significant with P-values of ≤ 0.05. After forward inclusion, a backward exclusion procedure was then performed where a change in OFV of > 10.82 was considered significant with P-values of ≤ 0.001. A covariate was retained in the model if its inclusion resulted in a significant decrease in OFV and decrease in unexplained variability or improved goodness-of-fit plots.
2.3.3 Model Evaluation
The robustness of the population pharmacokinetic model was evaluated using a non-parametric bootstrap procedure. Variables obtained with the bootstrap replicates (n = 500) were compared to the estimates obtained from the original dataset. Goodness-of-fit plots and VPCs were performed for internal validation of the model.
2.3.4 Simulations
A simulation was performed to compare the effect of different concentrations of IL-6 on the midazolam plasma concentrations. In addition to the IL-6 median concentration (116 pg/mL), a simulation was also performed with a normal Il-6 value (10 pg/mL) and an increased IL-6 value (300 pg/mL). Moreover, another simulation was performed to compare 1-OH-midazolam-glucuronide plasma concentrations with different serum concentrations of creatinine of 100 µmol/L, 200 µmol/L and 300 µmol/L. The creatinine values 100 µmol/L an a two and three fold increase to 200 µmol/L and 300 µmol/L represent respectively a normal renal function and stage 2 and 3 for acute kidney injury staging. Finally, to compare our pharmacokinetic results with another pharmacokinetic midazolam model in critically ill adult patients, a simulation was performed using our final model and a previously published model from Swart et al. [12]. The midazolam pharmacokinetics studied by Swart et al. were described by a two-compartment model with alcohol abuses, APAPCHE II score and age as significant covariates. The simulations were performed for a median age of 57 years and median APACHE II score of 26 from the study by Swart et al., with and without alcohol abuse. The plasma concentrations of midazolam and 1-OH-midazolam-glucuronide were simulated over a time course of 200 h after the administration of a 5 mg midazolam loading dose followed by our median infusion rate of midazolam continuous intravenous infusion.
2.4 Intensive Care Management
All patients fulfilling the criteria of moderate to severe ARDS were ventilated with a tidal volume of 6 ml/kg ideal bodyweight, limiting driving pressure to 12 cm H2O when possible. PEEP setting was according to the high-PEEP table of the ARDS-network studies and adjusted by using electrical impedance tomography [13]. Patients admitted with a P/F-ratio of less than 150 mmHg were ventilated in prone position during the first 24 h after admission, and for at least 16 h/day the following 3 days [13]. In case of ventilation in prone position, patients were deeply sedated as per protocol with midazolam (0.05–0.2 mg/kg/h) and sufentanil (0.3–0.7 µg/kg/h) infusion and treated with neuromuscular blockade if needed. Continuous infusion of clonidine (0.2–0.6 µg/kg/h) could be added when deemed necessary. A RASS of at least − 4 was aimed for in case of controlled mechanical ventilation and prone positioning.
3 Results
3.1 Patients and Samples
During the study period, midazolam blood samples were obtained from 38 patients. Of these patients, 7 were excluded for the following reasons: non-COVID-19 (n = 1), concomitant use of erythromycin (n = 1) and use of CRRT (n = 5). The remaining 31 patients were included for population pharmacokinetic modelling. Patients’ characteristics are summarized in Table 1. The median duration of infusion was 166 h (range 11–611 h), with a median infusion rate of 25 mg/h (range 3–80 mg/h) and a median dose of 0.28 mg/kg/h (range 0.03–1.00 mg/kg/h).
From 31 patients, 201 blood samples were in steady state collected (67 midazolam, 67 1-OH-midazolam and 67-OH midazolam-glucuronide). Exclusion of the samples with concentrations below the limit of quantification (3 midazolam and 9 1-OH-midazolam) resulted in, 189 samples eligible for pharmacokinetic analysis. Measured plasma concentrations ranged from 2 to 9400 µg/L for midazolam, 4–1416 µg/L for 1-OH-midazolam and 11–39,000 µg/L for 1-OH midazolam-glucuronide.
3.2 Pharmacokinetics of Midazolam
A one-compartment model was developed for midazolam and the metabolites 1-OH-midazolam and 1-OH midazolam-glucuronide with a proportional error model to describe the residual standard error of midazolam and both metabolites. IIV was included on clearance of midazolam, 1-OH-midazolam and 1-OH-midazolam-glucuronide. Finally, the IIV of 1-OH-midazolam and 1-OH-midazolam-glucuronide clearance were set to be similar. Due to many patients with only 1 or 2 observations, addition of IOV was not possible. Table 2 presents the pharmacokinetic variable estimates of the final model. The population mean estimates for clearance were 6.7 L/h (RSE 14.2%) for midazolam, 132.0 L/h (RSE 14.8%) for 1-OH-midazolam and 8.7 L/h (RSE 11.1%) for 1-OH-midazolam-glucuronide. The population mean estimate for volume of distribution was 135 L (RSE 19.9%) for midazolam, 443 L (RSE 23.0%) for 1-OH-midazolam and 100 L (RSE 16.6%) for 1-OH-midazolam-glucuronide. As a small unknown amount of midazolam is metabolized into 4-OH-midazolam, which is not described in our model, the subsequent compartments after the parent midazolam are expressed per available fraction (F). See Fig. 1 for the schematic representation of the structural model for midazolam and its two main metabolites.
Schematic representation of the structural model for midazolam and its two main metabolites. CL1/F: fractional midazolam clearance and formation of 1-OH-midazolam; CL2/F: fractional 1-OH-midazolam clearance and formtion of 1-OH-midazolam-glucuronide; fractional clearance of 1-OH-midazolam-glucuronide
The covariates were tested once at the time for improvement of the structural model.
In a univariate analysis IL-6 (dOFV − 40.0), CRP (dOFV − 38.1), weight (dOFV − 4.0), albumin (dOFV − 4.4), ALAT (dOFV − 18.5), gender (dOFV − 4.9) and BSA (dOFV − 6.2) on midazolam clearance and age (dOFV − 4.4), ALAT (dOFV − 8.7) and creatinine (dOFV − 38.1) on OH-midazolam-glucuronide clearance were found to provide a significant improvement of the model (p < 0.05). Subsequent iterations resulted in creatinine and ALAT on OH-midazolam-glucuronide clearance as significant improvement of the model (dOFV − 5.9).
The other covariates did not show a significant improvement of the model (P ≥ 0.05). After backward elimination with a lower threshold P ≤ 0.001, only two covariates remained in the final model, namely IL-6 for midazolam clearance (31.8 OFV difference) and creatinine (29.0 OFV difference) for 1-OH-midazolam-glucuronide clearance. Both IL-6 and creatinine were negatively correlated with clearance of midazolam and 1-OH-midazolam-glucuronide respectively, with a covariate effect of − 0.29 (− 0.39 to − 0.20) and − 1.24 (− 1.61 to − 0.88). The addition of IL-6 on midazolam clearance increased the IIV from 42.2 to 57.9%. However, since the proportional error decreased from 54.7 to 47.0 the increase in unexplained IIV was accepted.
Incorporation of creatinine as covariates on 1-OH-midzolam-glucuronide reduced the IIV from 107.4 to 69.7%.
With a condition number of 20.1 (< 1000) the model showed no signs of over-parameterization. Testing the robustness of the model with the bootstrap procedure showed that the estimates of the final model are in accordance with the results of the 500 bootstrap replicates. A total 485 of the 500 runs were successful. Results of the bootstrap are shown in Table 2. The goodness-of-fit plots of the final model also indicated a successful characterization of the data (Fig. 2). The individual predictions for midazolam and metabolites were evenly distributed around the line of unity when plotted against the observations, which indicates that the model is able to properly estimate the individual plasma concentrations. The population predictions for midazolam and metabolites tend to lower concentrations and higher clearance, resulting in an under prediction of the lower concentrations. This were mainly patients with samples after withdrawing of continuous infusion. Other goodness-of-fit plots are presented in the supplementary information. Evaluation of the predictive performance by VPCs showed accurate predictive ability. The VPCs show the median and 95% confidence interval of the observed midazolam, 1-OH-midazolam and 1-OH-midazolam-glucuronide concentrations (Fig. 3).
Prediction-corrected (PC) visual predictive check. PC-visual predictive check for midazolam (A), 1-OH-midazolam (B) and 1-OH-midazolam-glucuronide (C). The grey solid line indicates the median observed concentrations and the surrounding grey area the simulation based 95% confidence interval for the median. The grey dashed lines indicates the observed 5% and 95% percentiles, and the surrounding opaque blue areas show the simulated 95% confidence intervals for the corresponding predicted percentiles
3.3 Simulations
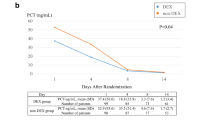
Simulated plasma profiles of midazolam and the effect of various IL-6 levels on midazolam clearance and the comparison to the model previously published by Swart et al. are shown in Fig. 4 [12]. The midazolam clearance was reduced by 24% (from 6.7 to 5.1 L/h) when IL-6 increased from population median 116–300 pg/mL.
Simulated plasma profiles of midazolam after a 5 mg midazolam loading dose followed by 25 mg/h continuous infusion for patients with an estimated IL-6 of 10 pg/mL (black line), 116 pg/mL (black small lines) and 300 pg/mL (black big lines) and compared to critically ill patients with (red line) and without (red line with dots) alcohol abuse as reported by Swart et al.
The effect of serum creatinine on the simulated plasma profiles of 1-OH-midazolam-glucuronide are shown in Fig. 5. The effect of serum creatinine concentration on 1-OH-midazolam-glucuronide clearance resulted in a reduction in clearance of 60% (from 8.7 to 3.5 L/h) when creatinine increased from 100 to 200 μmol/L. A further increase in creatinine to 300 μmol/L reduced the 1-OH-midazolam-glucuronide clearance by another 16% to 2.1 L/h.
4 Discussion
We developed a population pharmacokinetic model of intravenous midazolam provided as a continuous infusion in critically ill COVID-19 patients. The aim of our study was to determine the effect of inflammation on the pharmacokinetics of midazolam. We found that incremental levels of IL-6, an important mediator of inflammation in COVID-19, were significantly associated with decreased midazolam clearance and predicted decreased clearance more significant than CRP. Our finding of a negative correlation between IL-6 levels and midazolam clearance is in line with the study of Vet and colleagues in a pediatric ICU population [11].
We also showed that decreased renal function was significantly associated with decreased 1-OH-midazolam-glucuronide clearance. Similarly, a previous study observed accumulation of 1-OH-midazolam-glucuronide in patients with renal failure [5].
In contrast to previous studies albumin was not found to be correlated to midazolam clearance (midazolam is 94–97% protein bound) [14,15,16]. Although midazolam is highly protein bound, it seems unlikely that midazolam clearance is reduced during hypoalbuminemia. You would expect that a decrease in albumin would increase the unbound midazolam concentration and therefore result in increased clearance. Given the found reduced midazolam clearance, other proteins may also play a role in protein binding of midazolam or as suggested by the authors of Franken et al. the reduced clearance may be due to an inflammatory response and that hypoalbuminemia can be an expression of inflammation and critical illness [14]. However, there may be a difference in patients between our population and the studied terminally ill patients by Franken et al. (43–93 years; median 71 years, albumin 13–39 g/L; median 25 g/L and CRP 1 to 625 mg/L; median 92 mg/L).
The pharmacokinetics of midazolam established in the current study differ from those reported by Swart et al [12]. Swart and colleagues reported midazolam pharmacokinetics in critically ill adults (21–84 years; mean 57 years and APACHE II 6 to 34; median 26) with and without alcohol abuse. Patients with alcohol abuse showed a lower midazolam clearance, which probably is the result of reduced CYP3A activity due to alcoholic cirrhosis. The simulated midazolam pharmacokinetics with normal IL-6 concentration established in the current study are similar to the study of Swart et al. in the patient group without alcohol abuse and so without possible reduced CYP3A4 activity [12]. However, when increased IL-6 levels are taken into account a clearly reduced midazolam clearance was observed.
We found a median midazolam plasma concentration of 1446 µg/L. This appears to be high compared to previous investigations [17,18,19]. Our median plasma concentration is comparable to the finding by Nies et al. They observed a median midazolam concentration of roughly 1500 µg/L for RASS -5 [20]. The difference in median concentrations are probably due to the fact that on the one hand, the study by Bremer et al. included post-operative ICU patients and the study by Oldenhof et al. included only 17 patients, and on the other hand that the study by Nies et al. included more long term severe ICU patients.
There appears to be a good correlation between both median midazolam and 1-OH-midazolam plasma concentrations with the degree of sedation [19]. However, since there is a large interpatient variability in plasma concentrations of midazolam and metabolites, it is difficult to formulate a target attainment for a particular degree of sedation [19]. Nonetheless, when we simulated an IL-6 concentration of 116 pg/mL in our model, a steady-state midazolam concentration of almost 3500 µg/L was reached. Similar to our study, other studies observed also relatively high midazolam dose requirements in patients with COVID-19-related ARDS [21, 22]. Interestingly, Tapaskar et al. found a higher total median dose of midazolam in COVID-19 ARDS patients compared to non-COVID-19 ARDS patients. However, no difference in median RASS scores were found between their COVID-19 ARDS group and non-COVID-19 ARDS group, suggesting the higher midazolam dose in COVID-19 ARDS patients was required to achieve equivalent levels of sedation targeted in non-COVID-19 ARDS patients. [22] The high sedation requirements in COVID-19 patients are possibly related to patient factors such as agitation, increased patient-ventilator dyssynchrony, challenging mechanical ventilation in prone position and ARDS, and hyperinflammation, which has previously been linked to opioid tolerance [2, 3, 23]. Additionally, the binding of midazolam to the GABA receptor is saturable [24]. Therefore, a so-called ‘ceiling effect’ may occur, due to which greater doses will not produce greater pharmacological effects. However, limited information is known about the effect of COVID-19 and hyperinflammation on the functioning of GABA receptors and more research is needed on the possible saturation of the receptors.
Our results may have implications for more personalized titration of midazolam in COVID-19, mainly to avoid oversedation and subsequently increased length of ICU stay. Our findings indicate that IL-6 is an important biomarker indicative of reduced midazolam clearance. This theoretically contributes to prolonged coma, increased delirium rates and longer ICU stay, which seems to be supported by recent work [3]. Additionally, serum creatinine is an important biomarker for decreased 1-OH-midazolam-glucuronide elimination. Despite the potency of only 10% for 1-OH-midazolam-glucuronide, plasma concentration up to 39,000 µg/L as found in our study can contribute significantly to prolonged sedation effect in patients with kidney injury.
Therefore, increasing levels of IL-6 and renal failure should lead to incentives to decrease midazolam dosage as much as feasible to mitigate adverse consequences of oversedation.
Gordon et al. recently showed that in critically ill patients with COVID-19, an IL-6 receptor antagonist improved outcomes, including survival and becoming standard care of treatment [25]. In our cohort, none of the patients received an IL-6 receptor antagonist. Theoretically, IL-6 inhibition could neutralize the downregulation of CYP3A enzymes and hence also the reduced clearance of midazolam. Therefore, we suggest that the effect of IL-6 receptor antagonists on midazolam clearance should be further investigated.
In this study, we did not relate the pharmacokinetics to the pharmacodynamics of midazolam. Model-based Therapeutic Drug Monitoring (TDM) might be a valuable tool to relate the pharmacokinetics to the pharmacodynamics of midazolam and to identify patients at risk. Model-informed precision dosing has already been used for antibiotics in critically ill patients, but for sedative agents such models are scarce [26, 27]. For the individual patient, model-based TDM may help earlier dose reduction of midazolam or a switch to other sedative drugs, which may contribute to shorter duration of mechanical ventilation and mitigate days in coma and with delirium.
Several limitations of the study should be noted. The data was limited with respect to the number of patients and samples. The pharmacokinetic model showed a tendency towards under prediction of midazolam concentrations in the first week after the start of treatment, which could not be described in the pharmacokinetic model due to the limited number of available samples within this interval. In addition, especially for observations after withdrawing infusion, the model tends to an under prediction of the lower concentrations of midazolam and metabolites. Furthermore, depending on how concentrations of midazolam and metabolites behave above the upper limit of quantification (ULQ), the extrapolated samples above the ULQ may influence the model performance with more variability or bias.
We did not correlate the effect of the reduced midazolam clearance with the previous reported risk of delirium with midazolam and other risks, such as prolonged coma and increased ICU length of stay [3]. We also did not elucidate the reasons for the observed high-dose midazolam administration. Therefore, further studies on the pharmacodynamics in this population are needed before any firm conclusions can be drawn on dose adjustments. For future research, we propose a larger study population with more observations and development of a population pharmacodynamic model based on RASS scores. Another possible limitation of our study was that we did not identify patients’ genetic polymorphisms of CYP3A4/5. When expressed, it could potentially affect the metabolism of midazolam [28].
5 Conclusions
This study shows that inflammation, reflected by high IL-6, significantly reduces midazolam clearance in critically ill patients with COVID-19. This knowledge may help to identify COVID-19 patients at increased risk for prolonged sedation due to oversedation. Further studies are warranted to relate the pharmacokinetics to the pharmacodynamics of midazolam.
References
Devlin JW, Skrobik Y, Gelinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–73.
Chanques G, Constantin JM, Devlin JW, Ely EW, Fraser GL, Gelinas C, et al. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020;46(12):2342–56.
Pun BT, Badenes R, Heras La Calle G, Orun OM, Chen W, Raman R, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 2021;9(3):239–50.
Mandema JW, Tuk B, van Steveninck AL, Breimer DD, Cohen AF, Danhof M. Pharmacokinetic–pharmacodynamic modeling of the central nervous system effects of midazolam and its main metabolite alpha-hydroxymidazolam in healthy volunteers. Clin Pharmacol Ther. 1992;51(6):715–28.
Bauer TM, Ritz R, Haberthur C, Ha HR, Hunkeler W, Sleight AJ, et al. Prolonged sedation due to accumulation of conjugated metabolites of midazolam. Lancet. 1995;346(8968):145–7.
Morgan ET, Goralski KB, Piquette-Miller M, Renton KW, Robertson GR, Chaluvadi MR, et al. Regulation of drug-metabolizing enzymes and transporters in infection, inflammation, and cancer. Drug Metab Dispos. 2008;36(2):205–16.
Schmith VD, Foss JF. Effects of inflammation on pharmacokinetics/pharmacodynamics: increasing recognition of its contribution to variability in response. Clin Pharmacol Ther. 2008;83(6):809–11.
Veringa A, Ter Avest M, Span LF, van den Heuvel ER, Touw DJ, Zijlstra JG, et al. Voriconazole metabolism is influenced by severe inflammation: a prospective study. J Antimicrob Chemother. 2017;72(1):261–7.
Alexandre J, Rey E, Girre V, Grabar S, Tran A, Montheil V, et al. Relationship between cytochrome 3A activity, inflammatory status and the risk of docetaxel-induced febrile neutropenia: a prospective study. Ann Oncol. 2007;18(1):168–72.
Dickmann LJ, Patel SK, Rock DA, Wienkers LC, Slatter JG. Effects of interleukin-6 (IL-6) and an anti-IL-6 monoclonal antibody on drug-metabolizing enzymes in human hepatocyte culture. Drug Metab Dispos. 2011;39(8):1415–22.
Vet NJ, Brussee JM, de Hoog M, Mooij MG, Verlaat CW, Jerchel IS, et al. Inflammation and organ failure severely affect midazolam clearance in critically ill children. Am J Respir Crit Care Med. 2016;194(1):58–66.
Swart EL, Zuideveld KP, de Jongh J, Danhof M, Thijs LG, Strack van Schijndel RM. Comparative population pharmacokinetics of lorazepam and midazolam during long-term continuous infusion in critically ill patients. Br J Clin Pharmacol. 2004;57(2):135–45.
van der Zee P, Somhorst P, Endeman H, Gommers D. Electrical impedance tomography for positive end-expiratory pressure titration in COVID-19-related acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;202(2):280–4.
Franken LG, Masman AD, de Winter BCM, Baar FPM, Tibboel D, van Gelder T, et al. Hypoalbuminaemia and decreased midazolam clearance in terminally ill adult patients, an inflammatory effect? Br J Clin Pharmacol. 2017;83(8):1701–12.
Vree TB, Shimoda M, Driessen JJ, Guelen PJ, Janssen TJ, Termond EF, et al. Decreased plasma albumin concentration results in increased volume of distribution and decreased elimination of midazolam in intensive care patients. Clin Pharmacol Ther. 1989;46(5):537–44.
Dundee JW, Halliday NJ, Harper KW, Brogden RN. Midazolam. A review of its pharmacological properties and therapeutic use. Drugs. 1984;28(6):519–43.
Bremer F, Reulbach U, Schwilden H, Schuttler J. Midazolam therapeutic drug monitoring in intensive care sedation: a 5-year survey. Ther Drug Monit. 2004;26(6):643–9.
Oldenhof H, de Jong M, Steenhoek A, Janknegt R. Clinical pharmacokinetics of midazolam in intensive care patients, a wide interpatient variability? Clin Pharmacol Ther. 1988;43(3):263–9.
Spina SP, Ensom MH. Clinical pharmacokinetic monitoring of midazolam in critically ill patients. Pharmacotherapy. 2007;27(3):389–98.
Nies RJ, Muller C, Pfister R, Binder PS, Nosseir N, Nettersheim FS, et al. Monitoring of sedation depth in intensive care unit by therapeutic drug monitoring? A prospective observation study of medical intensive care patients. J Intensive Care. 2018;6:62.
Kapp CM, Zaeh S, Niedermeyer S, Punjabi NM, Siddharthan T, Damarla M. The use of analgesia and sedation in mechanically ventilated patients with COVID-19 acute respiratory distress syndrome. Anesth Analg. 2020;131(4):e198–200.
Tapaskar N, Colon Hidalgo D, Koo G, Shingada K, Rao S, Rodriguez R, et al. Sedation usage in COVID-19 acute respiratory distress syndrome: a multicenter study. Ann Pharmacother. 2021:10600280211021925.
Martyn JAJ, Mao J, Bittner EA. Opioid tolerance in critical illness. N Engl J Med. 2019;380(4):365–78.
Young CC, Prielipp RC. Benzodiazepines in the intensive care unit. Crit Care Clin. 2001;17(4):843–62.
Investigators R-C, Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med. 2021;384(16):1491–502.
Abdulla A, Ewoldt TMJ, Hunfeld NGM, Muller AE, Rietdijk WJR, Polinder S, et al. The effect of therapeutic drug monitoring of beta-lactam and fluoroquinolones on clinical outcome in critically ill patients: the DOLPHIN trial protocol of a multi-centre randomised controlled trial. BMC Infect Dis. 2020;20(1):57.
Tängdén T, Ramos Martín V, Felton TW, Nielsen EI, Marchand S, Brüggemann RJ, et al. The role of infection models and PK/PD modelling for optimising care of critically ill patients with severe infections. Intensive Care Med. 2017;43(7):1021–32.
Fromm MF, Schwilden H, Bachmakov I, König J, Bremer F, Schüttler J. Impact of the CYP3A5 genotype on midazolam pharmacokinetics and pharmacodynamics during intensive care sedation. Eur J Clin Pharmacol. 2007;63(12):1129–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflict of interest
Not applicable.
Ethics approval
The medical research ethics committee approved the study and waived informed consent requirement for observational research (MEC 2020-0381).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data is available upon request.
Code availability
Data is available upon request.
Authors' contributions
All authors contributed to the study conception and design. Material preparation were performed by TJLS and AJV and data collection were performed by TJLS and SDTS. The data analyses were performed by SDTS, the manuscript was written by TJLS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Smeets, T.J.L., Valkenburg, A.J., van der Jagt, M. et al. Hyperinflammation Reduces Midazolam Metabolism in Critically Ill Adults with COVID-19. Clin Pharmacokinet 61, 973–983 (2022). https://doi.org/10.1007/s40262-022-01122-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01122-5