Abstract
Cladribine is a nucleoside analog that is phosphorylated in its target cells (B and T-lymphocytes) to its active triphosphate form (2-chlorodeoxyadenosine triphosphate). Cladribine tablets 10 mg (Mavenclad®), administered for up to 10 days per year in 2 consecutive years (3.5-mg/kg cumulative dose over 2 years), are used to treat patients with relapsing multiple sclerosis. Cladribine has been shown to be a substrate of various nucleoside transporters (NTs). Intestinal absorption and distribution of cladribine throughout the body appear to be essentially mediated by equilibrative NTs (ENTs) and concentrative NTs (CNTs), specifically by ENT1, ENT2, ENT4, CNT2 (low affinity), and CNT3. Other efficient transporters of cladribine are the ABC efflux transporters, specifically breast cancer resistance protein, which likely modulates the oral absorption and renal excretion of cladribine. A key transporter for the intracellular uptake of cladribine into B and T-lymphocytes is ENT1 with ancillary contributions of ENT2 and CNT2. Transporter-based drug interactions affecting absorption and target cellular uptake of a prodrug such as cladribine are likely to reduce systemic bioavailability and target cell exposure, thereby possibly hampering clinical efficacy. In order to manage optimized therapy, i.e., to ensure uncompromised target cell uptake to preserve the full therapeutic potential of cladribine, it is important that clinicians are aware of the existence of NT-inhibiting medicinal products, various lifestyle drugs, and food components. This article reviews the existing knowledge on inhibitors of NT, which may alter cladribine absorption, distribution, and uptake into target cells, thereby summarizing the existing knowledge on optimized methods of administration and concomitant drugs that should be avoided during cladribine treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cladribine tablets are used to treat patients with relapsing multiple sclerosis. |
In this article, the authors consider how interactions with nucleoside transporters may affect the clinical efficacy of cladribine tablets, provide a summary on optimized approaches to administration, and identify which concomitant drugs should be avoided. |
1 Introduction
Multiple sclerosis (MS) is a chronic and debilitating autoimmune disorder of the central nervous system, affecting about 2.8 million people worldwide [1]. B and T-lymphocytes are believed to play a major role in the pathophysiology of MS [2]. Cladribine tablets 10 mg [3] were shown to have significant efficacy in the treatment of relapsing MS in placebo-controlled phase III trials [2, 4, 5]. A cumulative dose of 3.5 mg/kg body weight (consisting of two annual courses each comprising two treatment weeks; at the start of the first month and at the start of the second month of each year) has been approved in more than 80 countries including across Europe and the USA for the treatment of adults with certain types of relapsing MS [3, 6].
Recent immunophenotyping data demonstrated that effective doses of oral cladribine induced a 20–30% reduction of CD8+ T-cells and a 40–45% reduction of CD4+ T-cells during the first 12 months after initiation of treatment. This was accompanied by a comparable reduction in memory T-cells. The most prominent effect of cladribine, however, was a marked (80–85%) and long-lasting reduction in CD19+ B-cells [7, 8], suggesting that cladribine primarily confers a substantial B-cell reduction characterized by slow re-population kinetics, along with a long-term memory B-cell reduction [9]. Based on this mechanism, cladribine was characterized to act as an immune reconstitution therapy, which means the induction of immune resetting processes resulting in long-term efficacy.
Cladribine is a chlorinated analog of deoxyadenosine. The chlorine substitution for hydrogen in its purine ring renders cladribine largely resistant to deamination by adenosine deaminase, thereby prolonging its intracellular residence time with accumulation in the target cell cytoplasm [10]. Cladribine is a prodrug that is phosphorylated intracellularly to its active form, 2-chlorodeoxyadenosine triphosphate (2-Cd-ATP). Formation of 2-Cd-ATP is a sequential three-step process: first, cladribine is phosphorylated to 2-chlorodeoxyadenosine monophosphate by nuclear/cytosolic enzyme deoxycytidine kinase (DCK) and mitochondrial deoxyguanosine kinase. Thereafter, 2-chlorodeoxyadenosine monophosphate is further phosphorylated by nucleoside monophosphate kinase to 2-Cd-ADP, and nucleoside diphosphate kinase to 2-Cd-ATP. In most cells, 2-chlorodeoxyadenosine monophosphate is promptly dephosphorylated by 5′-nucleotidase (5′-NT) and, consequently, accumulation of 2-Cd-ATP depends on the intracellular ratio of DCK and 5′-NT enzymes [11]. Cells with a high endogenous DCK/5′-NT activity ratio (as is the case in B and T-lymphocytes) accumulate deoxynucleotides to toxic concentrations, resulting in cell death. By this mechanism, cladribine exerts a selective mode of action on B and T-lymphocytes [12, 13]. Thus, constitutive variations in the expression levels and activities of DCK and 5′-NT between immune cell subtypes explain differences in immune cell sensitivity to cladribine.
Recently, an important relationship was shown between DCK activity and the effect of cladribine on B and T-cells, depending on their activation status. Accordingly, cladribine induced apoptosis in stimulated T and B-cells and unstimulated B-cells [10], which may well explain the overall more pronounced activity on B-lymphocytes. Moreover, cells of the innate immune system are generally less affected than cells of the adaptive immune system [13, 14]. The preferential reduction in lymphocyte subpopulations, followed by the pattern of lymphocyte recovery (termed immune reconstitution), is believed to ‘reset’ the immune system to a less autoreactive state [15].
As a nucleoside analog, cladribine is a hydrophilic compound that relies on transporter-mediated cellular uptake as a prerequisite for its downstream metabolic activation, intracellular function, and clinical effectiveness. Numerous studies have shown that the distribution of cladribine across biological membranes is facilitated by a number of uptake and efflux transporters. The role of different ABC, solute carrier (SLC), and nucleoside transporter (NT) proteins in transmembrane permeability of cladribine to facilitate absorption, distribution throughout the body, intracellular uptake into target immune cells, and renal excretion of the compound has been recently reviewed [16].
Among the key ABC (ATP-binding cassette) efflux transporters, only breast cancer resistance protein (BCRP) has been shown to be an efficient transporter of cladribine, while P-glycoprotein (P-gp) does not transport cladribine well. Breast cancer resistance protein modulates the oral absorption of cladribine, while its renal excretion appears to be most likely driven by BCRP, equilibrative NT1 (ENT1), and P-gp [11].
Nucleoside transport in humans is mediated by members of two unrelated protein families, the SLC28 family of cation-linked concentrative NTs (CNTs) and the SLC29 family of energy-independent, equilibrative NTs (ENTs). These families contain three (CNT1, CNT2, and CNT3) and four (ENT1, ENT2, ENT3, and ENT4) members, respectively [17, 18]. Together, they play key roles in nucleoside and nucleobase uptake for salvage pathways of nucleotide synthesis. Moreover, they facilitate cellular uptake of several nucleoside and nucleobase drugs.
Transporter-mediated intestinal absorption, distribution throughout the body, and intracellular uptake of cladribine appear to be essentially mediated by ENTs and CNTs, specifically by ENT1, ENT2, and ENT4, and CNT2 (low affinity) and CNT3, while intestinal efflux of cladribine is modulated by BCRP, and renal excretion of cladribine appears to be most likely driven by BCRP, ENT1, and P-gp. The latter may play a role in the renal excretion of cladribine despite its poor cladribine transport efficiency in view of the high renal abundance of P-gp [19, 20]. There is no evidence that SLC uptake transporters, such as OATPs, OATs, and OCTs, are involved in the transport of cladribine [11].
Nucleoside transporter-based drug interactions affecting absorption and target cellular uptake of a prodrug such as cladribine are unlikely to be relevant in terms of safety, i.e., they are not expected to give rise to clinically notable adverse events. However, they are likely to reduce systemic bioavailability and target cell exposure, thereby possibly hampering clinically efficacy. Alteration of clinical efficacy by drug interactions is clinically hardly notable because decreased efficacy is not necessarily associated with notable adverse events; therefore, this type of interaction has been denoted “silent interactions” [16]. In order to manage optimized therapy, i.e., to preserve the full therapeutic potential of cladribine treatment in clinical practice, it is of critical importance that clinicians are aware of the existence of such “silent interactions” based on inhibition of NTs. This article therefore reviews the potential of certain food components such as dietary purines, various lifestyle drugs, and marketed medicinal products for the alteration of cladribine absorption, distribution, and uptake into target cells by inhibition of NT, thereby summarizing the existing knowledge on optimized methods of administration and concomitant drugs that should be avoided during cladribine treatment.
2 Methodology
This work aims to review food components, lifestyle drugs, and marketed prescription drugs reported to act as inhibitors of ENTs (ENT1, ENT2, and ENT4), and CNTs (CNT2 and CNT3). The NT selection of interest was based on published preclinical and clinical evidence, indicating that cladribine is a substrate of these proteins, and thus may become object of NT-based food/drug interactions in the presence of NT inhibitors. The information on the NT substrate characteristics of cladribine, and the role, function, as well as tissue and immune cell abundance of the NT of interest was part of a comprehensive cladribine transporter review recently published by our group [11]. In addition, a systematic review of published literature on NT inhibitors was undertaken using Medline In-Process (PubMed) and limited to English-language publications. As target cell uptake and efflux are of particular relevance to the disposition (and efficacy) of cladribine, search terms included the keywords “cladribine/2-CdA”, “ENT and CNT inhibitors”, “adenosine”, “adenosine re-uptake inhibitors”, and specific white blood cell subsets, with a particular emphasis on B and T-lymphocytes. Apart from the primary PubMed search that was conducted in May 2019, repeated secondary searches have been conducted on an ongoing basis during the preparation of this article, i.e., the authors continued to screen databases for upcoming relevant publications at regular intervals. Listed references of identified pertinent publications were also systematically reviewed to identify additional relevant publications that were not identified by the primary and secondary database searches.
In the absence of published in vivo drug–drug interaction (DDI) studies for specific NT inhibitors, the assessment of a potential in vivo DDI risk was based on available in vitro data of identified NT inhibitors describing transporter inhibition such as the half-maximal inhibitory concentrations (IC50) and/or the inhibition constants (Ki). These in vitro data were applied to calculate regulatory thresholds for in vivo DDI risk according to current DDI regulatory guidelines [European Medicines Agency (EMA) and US Food and Drug Administration (FDA)] in the context of their available in vivo exposure data, with a particular emphasis on the non-protein-bound free fraction (i.e., fraction unbound = fu) of the compounds and their reported maximum in vivo exposure achieved at steady state after administration of the highest recommended clinical doses. As no NT-specific cut-off values for potential in vivo relevance are currently provided in regulatory guidelines (EMA/FDA) or by the International Transporter Consortium, i.e., commonly accepted cut-off values are only available for unidirectional intestinal, hepatic, renal, and blood–brain barrier uptake and efflux transporters, and bidirectional renal proton antiporters (i.e., MATEs), but not for bidirectional equilibrative (i.e., passive) transporters such as ENTs, and different transporters may have different cut-off values, we decided to apply the most conservative approach recommended in the EMA guideline for renal transporters, which is the use of inhibitor concentrations of 50-fold unbound maximum concentration (Cmax,u) divided by IC50 or Ki, which results in a cut-off value of 0.02. This means that NT-inhibiting activities yielding a cut-off ≥ 0.02 were considered possibly clinically relevant for orally administered drugs. In addition to the generally applicable regulatory thresholds for anticipated in vivo DDI risks of various non-NTs, it was recently proposed specifically for the assessment of clinical significance of ENT1 inhibition as assessed by specific adverse events known to be associated with elevated adenosine levels to define a high degree of ENT1 inhibition in vivo when Cmax,u covers a concentration of ≥ 4 × IC50 as determined by cellular adenosine uptake assays or ≥ 13.3 × Ki as determined by [3H] NBTI (nitrobenzylthioinosine) binding assays [21].
3 Background and Role of NTs and Their Inhibition
Inhibition of ENTs and CNTs may affect intestinal absorption of nucleoside derivatives such as cladribine, as well as their distribution into endothelial cells, red and white blood cells, uptake and excretion by the liver and kidney, and permeation of the blood–brain barrier, thereby impeding access to the central nervous system [18, 22]. To date, there are few clinical DDI studies available showcasing the effects of potent ENT/CNT inhibitors on the pharmacokinetics and distribution of sensitive ENT/CNT substrates. However, there are many studies linking NT expression in cells of various hematological malignancies (e.g., CLL, CML) and solid tumors (e.g., pancreatic cancer) to intracellular accumulation and clinical response to nucleosidic anti-cancer drugs. Therefore, NTs could be considered as predictive biomarkers of drug targets and indicators of responsiveness to those treatments [22].
For the assessment of a potential ENT/CNT-based risk for drug interactions, the first step is to review the currently available evidence, as to which marketed products have been identified and characterized by in vitro testing as potent ENT/CNT inhibitors. The second step is an attempt to translate these in vitro findings to potential in vivo relevance by looking for accepted biomarkers of NT inhibition. As adenosine represents the main endogenous substrate of NTs, which are essential for adenosine re-uptake, extracellular adenosine levels can be elevated as a result of NT inhibition in vivo, although other mechanisms (e.g., inhibition of adenosine metabolism) can also result in elevated plasma adenosine levels [23]. Among the NT most relevant for adenosine re-uptake, ENT1 has been identified as a major player. Nevertheless, other transporters such as CNT2 and CNT3 also contribute to purinergic modulation based on their high affinity for adenosine and concentrative capacity, and depending on their tissue or cellular abundance [22, 24]. However, most of the currently available marketed medicinal products that have been reported to inhibit NT display almost exclusively high potencies for inhibition of ENTs, primarily ENT1 and to some extent also ENT2 (Table 1). An exception to this rule is the tyrosine kinase inhibitor (TKI) imatinib, which has been shown to be a potent and fairly selective CNT2 inhibitor (IC50 CNT2 = 2.3 µmol/L) [25] (Table 1). Apart from imatinib, there are few potent or specific pharmacological CNT inhibitors among marketed products. Thus, the few products that have been reported to inhibit CNTs at relatively low µmol/L concentrations are rather to be considered as pan ENT/CNT inhibitors that usually inhibit ENT1 with much higher potency than ENT2 and CNTs. Therefore, the present review primarily focuses on marketed ENT1 inhibitors.
Some pharmacokinetic considerations are relevant for the potential in vivo relevance of in vitro NT inhibition by identified perpetrator drugs. These include Cmax,u achieved with recommended doses, possible accumulation of plasma concentrations upon repeat dosing, and plasma protein binding, as only the free fraction of a perpetrator drug actually can confer transporter inhibition. Other factors include the transporter affinities and dissociation kinetics of putative perpetrator drugs and their mechanism of inhibition, i.e., competitive, non-competitive, or irreversible inhibition. In a recent study, it was shown that currently available ENT1 perpetrator drugs display relatively fast dissociation kinetics, and yield only short-to-moderate residence times between 1 and 44 minutes at the transporter protein [26]. The underlying mechanism of ENT1 inhibition is predominantly competitive with few exceptions of non-competitive inhibition [27]. To the best of our knowledge, there are no irreversible NT inhibitors among currently marketed drugs. The lack of irreversible ENT inhibitors along with the short residence times at the transporter protein allows, in principle, clinical management of such interactions by relatively simple means, namely, by time separation of the intake of the ENT substrate and perpetrator drugs, under careful consideration of the inhibitor’s terminal plasma half-life.
Because of the paucity of in vivo drug interaction studies with potent ENT inhibitors, reliable quantitative assessments that may build the scientific basis for judgments on potential clinical relevance are currently not possible. However, reasonable mechanistic considerations on potential drug interaction risks, based on the criteria detailed above, along with transporter expression pattern and their established roles in the transport of nucleosides and nucleosidic drugs, are considered valuable information to prevent possibly significant drug interactions in the clinical use of ENT/CNT substrates such as cladribine. In this context, it is noteworthy that both alterations of the bioavailability of cladribine and its distribution into target cells (i.e., lymphocytes) by potent ENT inhibition most likely represent a “silent interaction” that cannot be detected by clinical adverse events but may result in altered or sub-optimal clinical efficacy. It is therefore important to pay attention to the avoidance of co-administration of known potent ENT inhibitors shortly before and during the few days of cladribine treatment. In addition to DDI, the potential NT-inhibitory effects of food components such as dietary purines, alcohol, and lifestyle drugs such as cannabinoids are also considered below.
3.1 Food Effects
Based on existing knowledge on the ENT/CNT substrate characteristics of cladribine, the intestinal uptake of cladribine can, in principle, be facilitated by intestinal apical uptake transporters such as concentrative NTs CNT2 [17, 28] and CNT3 [17, 29, 30], while efflux from the intestinal enterocytes into the mesenteric blood is, in principle, facilitated by the basolateral located ENTs [24, 31, 32]. Among the ENT family, ENT1 is likely to be the key transporter mediating nucleoside efflux into the mesenteric blood as its expression and activity are higher than that of co-localized ENT2 [17]. CNT2 has been suggested as the jejunal NT of purine nucleosides [33], and CNT3 transports both pyrimidine and purine nucleosides [17].
For the antiviral nucleoside analog ribavirin, which displays similar ENT1/2 and CNT2/3 substrate characteristics as cladribine [22], a study in healthy volunteers examined the effects of the dietary purine content of meals on the pharmacokinetics of orally administered ribavirin. Participants were administered a single 600-mg oral dose of ribavirin either after a high-purine meal (purine content 192.1 mg) or a low-purine meal (purine content 7.56 mg). Maximum concentration and area under the concentration–time curve from zero to 14 h values of ribavirin following a low-purine meal were 136% (90% confidence interval 120–155) and 139% (90% confidence interval 120–159) higher than corresponding data obtained after the high-purine meal, indicating a reduced maximum exposure and extent of absorption of the ENT1/2 and CNT2/3 substrate ribavirin, probably owing to competition of dietary nucleosides with ribavirin for intestinal CNT and ENT transporters [34].
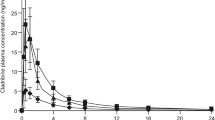
In a cladribine food-interaction study employing a typical FDA-recommended high-fat, high-calorie breakfast [35], the rate of cladribine absorption was delayed in the fed state (median time to maximum concentration 1.5 h; range 1–3 h) as compared with the fasted state (median time to maximum concentration 0.5 h; range 0.5–1.5 h), and the geometric mean maximum concentration (Cmax) was reduced by 29%. In contrast, total cladribine exposure (geometric mean area under the concentration–time curve from zero to infinity) was only marginally affected with 72.8 ng·h/mL for the fed state vs 75.7 ng·h/mL for the fasted state [35]. Based on this, it was concluded that cladribine tablets can be administered without regard to food [3, 6]. It should be noted, however, that the high-fat, high-calorie test meal employed in the study only contained relatively low amounts of dietary purines of approximately 24 mg, which is about eight-fold less than the high-purine meal employed in the ribavirin study. It remains therefore unknown whether purine-rich meals [including certain fish and seafood (such as anchovies, haddock, herring, mussels, sardines, scallops, and trout) and some meats (such as bacon, turkey, veal, venison, and organ meats like liver)] may have the potential to alter the bioavailability of cladribine tablets.
3.2 Effects of Alcohol
Clinicians should be aware of the possible effects that alcohol intake could have on the effectiveness of cladribine, particularly as problem drinking has been reported in patients with MS [36]. A number of studies have identified ethanol as a pharmacological inhibitor of ENT1-mediated adenosine uptake, resulting in increased extracellular adenosine concentrations in experimental in vitro studies using human lymphocytes [37], primary cultures of rat hepatocytes [38], human placental cells [39], human bronchial cells [40], S49 mouse lymphoma cells and rodent neuronal-glial cells (NG108-15) [41,42,43,44], and in the cardiomyocyte cell line, HL-1 [45]. Ethanol is known to selectively inhibit ENT1, but not ENT2 (Table 1).
Ramadan and co-workers showed partial ENT1 inhibition at lower ethanol exposures that are known to occur in vivo by an average consumption of one to two drinks per day (which is equivalent to peak blood alcohol levels of ~ 10 mmol/L ethanol) while about 25-mmol/L ethanol blood concentrations are commonly achieved in social surroundings [45]. This suggests that ethanol-mediated ENT1 inhibition is likely to be relevant in vivo. The same group also showed that gemcitabine cytotoxicity is reduced in the presence of 2-mmol/L ethanol concentrations in the human bladder cancer cell line, HBT2. The authors proposed a direct partial inhibition of ENT1 upon acute ethanol exposure and a long-term down-regulation of ENT1 expression, resulting in less ENT1 protein at the plasma membrane upon chronic alcohol exposure [45].
Ethanol-mediated ENT1 inhibition may alter intestinal absorption of cladribine as well as ENT1-mediated uptake into lymphocytes and tubular secretion in the kidney. A reduced bioavailability together with an altered uptake into lymphocytes may theoretically have potential to result in an attenuated efficacy of cladribine treatment, while safety appears less of a concern. Therefore, it appears advisable that patients refrain from alcohol consumption before taking cladribine tablets.
3.3 Tetrahydrocannabinol and Cannabidiol
Two recent high-quality systematic reviews concluded that the only strong evidence for medical marijuana in neurological disorders was for reducing the symptoms of patient-reported spasticity and central pain in MS and that the only complementary and alternative medicine intervention in MS with strong supportive evidence was cannabinoids [46]. A UK survey conducted in 2014 in patients with MS revealed that one in five patients used cannabis products to alleviate their symptoms, especially muscle spasms or stiffness (spasticity) and pain [47].
The Cannabis sativa components tetrahydrocannabinol (THC) and cannabidiol (CBD) were reported to inhibit adenosine transport with IC50 values in the nanomolar range by acting as competitive inhibitors at the equilibrative transporter ENT1 [48]. In particular, CBD and, less potently, THC decreased uptake of [3H]adenosine to a similar extent as [3H]thymidine in both murine microglia and RAW264.7 macrophages. Binding studies confirmed that CBD binds to ENT1 with a Ki < 250 nmol/L, and the Ki for CBD to inhibit adenosine transport was 120 nmol/L [48] (Table 1).
Marketed medicinal products containing the synthetic THC derivative dronabinol (delta-9-tetrahydrocannabinol) are available in USA and Canada, and include capsules for oral use [49] and an oral solution [50]. Although both are not indicated for the symptomatic treatment of MS symptoms, some off-label use may be assumed. Mean plasma Cmax achieved with the highest approved Marinol® capsule strength, i.e., 10 mg in the fasted condition, are reported with 7.88 ± 4.54 ng/mL [49], corresponding to about 250 nmol/L. Maximum concentration values achieved with the highest recommended dose (4.2 mg/m2 body surface area) of the oral solution product are reported with about 3.3 ng/mL distinctly lower [50]. Considering these exposure data together with the delta-9-THC plasma protein binding of 97%, the maximum unbound Cmax values are unlikely to confer a relevant ENT1 inhibition in vivo, i.e., (Cmax × fu/IC50 is < 0.02; see Table 1).
In addition to the available oral THC mono products, there is a fixed combination medicinal product available in 19 European countries and Switzerland (European Union since 2010, CH since 2013), which is specifically indicated for symptom improvement in adult patients with moderate-to-severe spasticity due to MS. This product contains THC and the non-psychoactive cannabinoid-component CBD, and is presented as an oromucosal spray (USAN: nabiximols; tradename Sativex®; one puff delivers a 100-µL spray containing 2.7 mg of THC and 2.5 mg of CBD) [51]. The highest recommended dose consists of 12 sprays per day separated into five sprays in the morning and seven sprays in the evening. The latter corresponds to maximum recommended total single oromucosal doses of 18.9 mg and 17.5 mg of THC and CBD, respectively. The inter-subject variability of THC and CBD pharmacokinetic parameters is high. Following a single Sativex® administration of four sprays under fasted conditions, the mean maximum plasma THC levels (Cmax) ranged between 0.97 and 9.34 ng/mL, while the observed Cmax for CBD ranged between 0.24 and 2.57 ng/mL, i.e., about ten-fold for both THC and CBD. After 9 consecutive days of dosing Cmax ranged from 0.92 to 6.37 ng/mL for THC and from 0.34 to 3.39 ng/mL for CBD, respectively, indicating an absence of accumulation of THC and CBD plasma concentrations upon repeated dosing [51]. This means also for CBD that with repeat administration of recommended doses of Sativex®, the achieved maximum unbound Cmax values are unlikely to confer a relevant ENT1 inhibition in vivo, i.e., Cmax × fu/IC50 is < 0.02; see Table 1.
In addition to approved and well-standardized, THC-containing and CBD-containing pharmaceutical products, medical cannabis is also provided in the form of herbal products derived from dried cannabis flowers (medical cannabis or medical marijuana). In this context, it is worthy to note that plasma concentrations achieved with THC/CBD products for oral or oromucosal administration, THC, and CBD plasma concentrations are much lower compared with concentrations achieved following inhalation (e.g., smoking or vaporisation) of cannabinoids at similar doses. For instance, a dose of 8 mg of vaporised THC extract, administered by inhalation, resulted in a mean Cmax of more than 116.2 ng/mL (corresponding to 0.37 µmol/L) within minutes of administration, which exceeds mean Cmax values upon oral administration of 10 mg delta-9-THC by about 15-fold [52]. This yields a cut-off value for Cmax × fu/IC50 of 0.07, thereby indicating a possible relevant ENT1 inhibition in vivo (Table 1). The same applies to CBD maximum exposure concentrations observed after vaporisation with a mean Cmax value of 76.3 ng/mL (range 2.3–339 ng/mL) achieved with just a CBD 1.5-mg single dose or smoking of cannabis cigarettes containing CBD 1.5 mg, which resulted in a mean Cmax value of 93.3 ng/mL (range 0.65–350 ng/mL) in frequent cannabis smokers [53, 54]. This translates to an approximately 27-fold maximum CBD exposure concentration upon smoking of cannabis cigarettes as compared to the CBD steady-state exposure achieved with recommended doses of the oral mucosal spray (Sativex®). This translates to a cut-off value of 0.09 when Cmax × fu/IC50 is considered, and 0.08 when Cmax × fu/Ki is considered. Both outcomes point to a possible relevant ENT1 inhibition in vivo (Table 1). Taken together, systemic THC/CBD exposure concentrations achieved with inhalation/smoking are deemed sufficiently high to predict that in vivo inhibition of ENT1 by both compounds is likely.
The terminal half-life of THC is reported to be 25–36 h upon oral administration [49], while the half-life of CBD was reported between 1.4 and 10.9 h after an oromucosal spray, 2–5 days after long-term oral administration and 31 h after smoking [53]. In addition, THC and CBD may be retained in the adipose tissue for as long as 4 weeks from which they are slowly re-distributed at sub-therapeutic concentrations into the systemic circulation [51]. Thus, it is recommended that patients with MS refrain from the use of cannabinoid products, in particular from inhaled administration, for at least 1 week before and during treatment with cladribine tablets in order to optimize ENT1-mediated absorption of cladribine and uptake into lymphocytes.
3.4 Adenosine Re-Uptake Inhibitors
Adenosine re-uptake inhibitors such as dipyridamole [55] and dilazep [56] are old drugs developed in the 1950s and 1960s. They were designed to retard the cellular uptake of extracellular adenosine into endothelial cells and red blood cells, thereby potentiating the receptor-mediated physiological effects of adenosine, by potent inhibition of ENTs, in particular ENT1. They were deemed to be clinically useful because of their cerebral and coronary vasodilating action, and inhibition of platelet aggregation through enhancement of adenosine effects.
Dipyridamole was introduced for the treatment of ischemic heart disease in 1959. Its undesired and harmful coronary “steal” phenomenon was observed a few years later [57]. Although its clinical use in cardiac indications such as coronary artery disease and myocardial infarction has been considered obsolete in the scientific community for decades, the drug is still marketed for these indications in some countries (e.g., Japan and India). Dipyridamole is also marketed in the European Union and the USA as an adjunct to oral anti-coagulation in combination with acetylsalicylic acid or coumarin anticoagulants in patients with prosthesis-related thromboembolic events, e.g., in the prevention of postoperative thromboembolic complications of cardiac valve replacement [55].
Dipyridamole and dilazep are known to inhibit ENT1 at nanomolar concentrations, with Ki values of 48 nmol/L and 19 nmol/L, respectively [58, 59]. Considering the dipyridamole exposure data together with the lowest reported plasma protein binding of 96.5%, the maximum unbound Cmax values are likely to confer a relevant ENT1 inhibition in vivo, i.e., Cmax × fu/Ki is calculated with 2.43, which is by far the highest cut-off value for all identified ENT1 inhibitors (Table 1), which is consistent with the established evidence that dipyridamole represents the most potent prototypic ENT1 inhibitor known to date. Dipyridamole also inhibits ENT2 at low micromolar concentrations (Ki = 6.2 µmol/L), which however, is unlikely to exert clinical relevance (Table 1).
Unfortunately, no protein binding data are available in the public domain for dilazep, which prevents calculation of ENT1 and ENT2 inhibition cut-off values. However, when the reported Ki values for ENT1 inhibition in the lower nanomolar range are compared with the Ki values for ENT2 inhibition in the higher micromolar range (Table 1), it can be inferred that dilazep most probably acts as a specific ENT1 inhibitor in vivo. As both dipyridamole and dilazep products are available as oral formulations, they are in principle to be considered perpetrators of the intestinal transporter-mediated absorption of cladribine as well as ENT1-mediated uptake into lymphocytes and red blood cells, and tubular secretion of cladribine in the kidney. However, because of the required 3-h time separation of cladribine dosing from other orally administered drug products, as per the cladribine label, intestinal ENT-mediated absorption interactions are not expected to play a significant role in clinical practice. As the mean (dominant) plasma half-lives of dipyridamole and dilazep are short (about 3 h for both compounds), it is recommended that patients suspend intake of dipyridamole or dilazep at least 1 day before starting treatment with cladribine tablets. If withdrawal is not possible, selection of alternative products with no, or minimal, ENT1 transporter-inhibiting properties should be considered.
3.5 Ticagrelor
Ticagrelor is an oral, direct-acting, selective, and reversibly binding P2Y12 receptor antagonist that prevents ADP-mediated P2Y12-dependent platelet activation and aggregation to inhibit the prothrombotic effects of ADP [60]. In addition to the inhibition of platelet activation and aggregation via P2Y12 receptor antagonism, part of the antiplatelet effect of ticagrelor is due to a drug-induced increase in extracellular adenosine levels via ENT1-mediated adenosine re-uptake inhibition, resulting in adenosine-mediated platelet inhibition via the A2A receptor. Thus, ticagrelor has a unique dual mode of action, with a primary effect mediated by P2Y12 antagonism complemented by adenosine re-uptake inhibition as a secondary mechanism [61].
Ticagrelor inhibited adenosine uptake in MDCK cells expressing ENT1, with an IC50 of 260 nmol/L (Table 1), which is approximately 35-fold less than that of dipyridamole (IC50 = 7.4 nmol/L), a known prototypic inhibitor of ENT1 [62]. These findings are in line with those from another study in human breast carcinoma cells, where the potency of ticagrelor with respect to inhibition of adenosine uptake was approximately ten-fold less than that of dipyridamole [63]. The major ticagrelor metabolites AR-C124910XX and AR-C133913XX also inhibited adenosine uptake with IC50 values of 2.2 µmol/L and 3.5 µmol/L, respectively (Table 1).
The authors further demonstrated that ticagrelor can displace the potent inhibitor [3H]NBTI (nitrobenzylthioinosine) from ENT1 in MDCK cells, confirming that ticagrelor binds with high affinity (Ki = 41 nmol/L) directly to ENT1 to inhibit adenosine uptake [62] (Table 1). In this cell system, the Ki of ticagrelor was about 15-fold less than that of dipyridamole (Ki = 2.6 nmol/L). In turn, no significant inhibitory activity was observed in MDCK cells expressing ENT2 or CNT2/3, characterizing ticagrelor as a specific ENT1 inhibitor.
Both ticagrelor and the active metabolite AR-C124910XX are highly bound to human plasma protein (> 99.8%), i.e., the unbound fraction is ~0.2% [64]. However, despite this high protein binding, the unbound ticagrelor Cmax/IC50 for ENT1 inhibition is calculated with 0.078 (Table 1), thereby exceeding the EMA guideline criteria for the assessment of systemic transporter inhibition of potential clinical relevance (cut-off of ≥ 0.02 applied). The predicted in vivo relevance of ticagrelor-mediated ENT1 inhibition was confirmed by clinical studies in healthy subjects (180-mg single dose) and in patients with non-ST-elevation acute coronary syndrome undergoing percutaneous coronary intervention (90 mg twice daily [bid] over 15 days), both showing that ticagrelor enhanced adenosine-mediated coronary blood flow velocity via an adenosine-mediated mechanism [65, 66]. Finally, a study investigating the impact of ticagrelor on adenosine plasma concentrations in patients with acute coronary syndrome (180-mg loading dose followed by 90 mg bid) compared to a clopidogrel treatment (600-mg loading dose followed by 75 mg bid), showed more than twice as high adenosine plasma concentrations in patients receiving ticagrelor than patients receiving clopidogrel [1.5 µM (interquartile range: 0.98–1.7 µM) vs 0.68 µM (interquartile range: 0.49–0.78 µM; p < 0.01)] [67]. These results confirm that the concentration of ticagrelor attained after oral administration with the recommended clinical dose regimen is sufficient to inhibit cellular uptake of adenosine in vivo, thereby increasing its plasma concentration. These findings are also supported by the adverse event profile of ticagrelor, which includes dyspnea and bradyarrhythmias, symptoms that are attributed to elevated adenosine levels due to ENT1 inhibition [21, 68, 69].
Taken together, it is concluded that ticagrelor inhibits cellular adenosine uptake selectively via ENT1 inhibition at concentrations of clinical relevance, suggesting that ticagrelor treatment should be suspended for at least 3 days (the mean terminal disposition half-life of ticagrelor ranges between 7.7 and 13.1 h) before initiation of treatment with cladribine tablets, and should only be resumed 1 day after the last dose of cladribine. If withdrawal is not possible, selection of an alternative antiplatelet product with no, or minimal, ENT1 transporter-inhibiting properties should be considered.
3.6 Cilostazol
Cilostazol (Pletal®) is a dual inhibitor of phosphodiesterase III and adenosine re-uptake with antiplatelet activity that is indicated for the improvement of the maximal and pain-free walking distances in patients with intermittent claudication [70]. Cilostazol inhibits adenosine uptake into muscle, endothelial cells, red blood cells, and platelets with an IC50 of ~5–10 µmol/L [71, 72] (Table 1). As with other adenosine re-uptake inhibitors, clinically relevant concentrations of cilostazol (3–5 µmol/L) have been shown to increase rabbit cardiac interstitial and circulatory adenosine levels [72]. It is noteworthy that the 3,4-dehydro metabolite of cilostazol (OPC-13015), one of two major metabolites, is about five times more potent than cilostazol as a phosphodiesterase III inhibitor and three times more potent as an adenosine re-uptake inhibitor [71], and its plasma concentration (as measured by area under the concentration–time curve) is about 41% of the cilostazol parent drug [70]. It was later shown that the adenosine uptake inhibition by cilostazol was actually due to direct inhibition of ENT1 [21]. Thus, it is reasonable to assume that the total ENT1-inhibiting potency in vivo might be the result of a combined effect of the cilostazol parent drug and its major 3,4-dehydro metabolite OPC-13015. Additionally, the adverse event profile of cilostazol includes dyspnea and bronchospasm in patients with pre-existing respiratory diseases, symptoms that are attributed to elevated adenosine levels due to ENT1 inhibition [21]. This suggests that the inhibition of ENT1 by recommended doses of cilostazol (i.e., 100 mg bid) is clinically relevant. It is important to note that the calculated cut-off values of cilostazol of 0.02 for both ENT1 and ENT2 inhibition (Table 1) correctly point to the potential in vivo relevance of cilostazol-mediated dual ENT1/2 inhibition. Therefore, patients should be advised to suspend cilostazol treatment for at least 3 days (the mean terminal disposition half-life of cilostazol is about 10.5 h) before initiation of treatment with cladribine tablets, resuming 1 day after the last dose of cladribine. If withdrawal is not possible, selection of an alternative product with no, or minimal, ENT1 transporter-inhibiting properties should be considered.
3.7 Dihydropyridine CCBs
Calcium channel blockers (CCBs) are among the five major drug classes recommended for the treatment of hypertension [73], and have similar effectiveness as other major drug classes on blood pressure, major cardiovascular events, and mortality outcomes. This is a heterogeneous class of agents including dihydropyridines (DHP-CCBs) and non-dihydropyridines (e.g., verapamil and diltiazem). The two subclasses do not show substantial differences in effectiveness [73].
Nimodipine (Nimotop®) is a DHP-CBB that is not indicated for the treatment of hypertension but approved for the prevention of ischemic neurological deficits and cerebral vasospasm after aneurysmal subarachnoid hemorrhage [74]. The substance is known to inhibit adenosine transport in the brain, heart, and red blood cells with IC50 values in the nanomolar range [27, 75, 76]. A pharmacokinetic study in patients with cerebral ischemia has shown that intravenous (bolus of 0.03 mg/kg) and oral (30, 60, and 90 mg) administration of nimodipine increases the plasma level of adenosine [77]. It has therefore been suggested that the inhibition of adenosine uptake is a relevant mechanism for the clinical effects of nimodipine. Other DHP-CBB such as nitrendipine, nifedipine, and nicardipine inhibit adenosine transport in vitro to different extent [18, 78].
Li et al. investigated the mechanism by which dihydropyridines inhibit adenosine uptake [27]. Among the dihydropyridines tested, nimodipine was identified as a very potent inhibitor of ENT1 (IC50 = 60 ± 31 nmol/L), whereas nicardipine, nitrendipine, felodipine, and nifedipine exhibited at least 100-fold less potent inhibitory activity (nicardipine IC50 = 8.7 ± 8.2 µmol/L; nitrendipine IC50 = 10.1 ± 1.3 µmol/L; felodipine IC50 = 12.4 ± 3.1 µmol/L; nifedipine IC50 = 13.7 ± 3.2 µmol/L) (Table 1). Nifedipine, nitrendipine, and nimodipine also inhibited ENT2 with IC50 values in the lower micromolar range (nifedipine IC50 = 1.3 ± 0.1mol/L; nitrendipine IC50 = 3.7 ± 1.5 µmol/L; nimodipine IC50 = 13.1 ± 4.9 µmol/L) (Table 1), while nicardipine and felodipine did not exert significant effects on ENT2 [27].
Kinetic studies suggested that DHP-CCBs act as non-competitive inhibitors of ENT1 and ENT2. In this respect, DHP-CCBs are distinct from most other nucleoside transport inhibitors, which are usually competitive inhibitors. The interactions of DHP-CCBs with ENT1 and ENT2 are reversible [27].
When EMA DDI guideline criteria for the assessment of systemic transporter inhibition of potential clinical relevance are considered, only nimodipine is expected to act as a clinically relevant inhibitor of ENT1 in vivo, with a cut-off value of 0.26 when Cmax × fu/IC50 for a 90-mg oral dose is considered. In turn, all other DHP-CCBs with reported in vitro ENT-inhibiting properties are unlikely to exert these effects in vivo (Table 1). The dominant half-life for nimodipine ranges between 1.1 and 1.7 h. Accordingly, co-administration of nimodipine does not need to be washed out before initiation of cladribine treatment but should be avoided (if possible) during the 4–5 days of treatment with cladribine tablets. If withdrawal is not possible, selection of an alternative product with no, or minimal, ENT1 transporter-inhibiting properties should be considered. All other DHP-CCBs are unlikely to exert clinically relevant inhibition of ENT1 or ENT2 when used at recommended doses.
3.8 Nonsteroidal Anti-Inflammatory Drugs
Li and co-workers investigated the effects of nonsteroidal anti-inflammatory drugs (NSAIDs) on adenosine uptake in human aortic smooth muscle cells. Aspirin, ibuprofen, and naproxen had no effect on adenosine uptake, while etodolac, indomethacin, ketoprofen, mefenamic acid, and sulindac inhibited adenosine uptake by 13–18%, and piroxicam inhibited adenosine uptake by 30% [79] (Table 1). However, sulindac sulphide (the active metabolite of sulindac) completely inhibited adenosine uptake with an IC50 of 40 µmol/L (Table 1). The action of sulindac sulphide on adenosine uptake is due to the direct blockade of NTs rather than to the inhibition of COX. Kinetic data of adenosine uptake indicated that the inhibition of adenosine transport by sulindac sulphide is competitive, and results also showed that the inhibitory effect on ENT1 was more potent (IC50 of 33 µmol/L) than that on ENT2 (35% inhibition of adenosine uptake at 300 µmol/L) (Table 1). The peak blood concentration of sulindac sulphide in patients who take sulindac (150 mg bid) is about 20 µmol/L, and the authors of the study estimated that such a concentration can weakly (but significantly) inhibit ENT1-mediated adenosine uptake [79]. However, when the most conservative EMA cut-off criterion for potential in vivo relevance of transporter inhibition is applied (i.e., Cmax,u × fu/IC50 is ≥ 0.02), it does not appear that sulindac sulphide may be able to confer a clinically relevant ENT1 inhibition in vivo (Table 1). Taken together, NSAIDs, as a class, are not regarded as clinically relevant NT inhibitors in vivo.
3.9 Benzodiazepines
Benzodiazepines are widely used for the symptomatic treatment of a variety of MS symptoms including spasticity (stiffness), tremor dizziness/vertigo, and anxiety [80]. There are data to indicate that benzodiazepines show affinity for ENT1. Competition binding assays of five structurally distinct benzodiazepines (midazolam, alprazolam, flurazepam, diazepam and chlordiazepoxide) in membranes from porcine striatum and guinea pig ventricles showed that all benzodiazepines completely displaced the ENT1-specific inhibitor [3H]NBMPR in a concentration-dependent manner [81]. Midazolam was the most potent ENT1 inhibitor with a Ki value of 6 µmol/L (Table 1). The Ki values of all other benzodiazepines tested ranged between 39.8 and 53.7 µmol/L when the guinea pig ventricle data are considered. The authors concluded that benzodiazepines are weak ENT1 inhibitors at concentrations achieved with clinically recommended doses to facilitate their primary mode of action, i.e., GABAergic transmission in vivo. The affinity of benzodiazepines for ENT1 was shown to be about 1000-fold lower than that of the prototypical high-affinity ENT1 inhibitor NBMPR or dipyridamole (Ki = 1.9 nmol/L in human erythrocytes). Apart from that, benzodiazepines are highly bound to plasma proteins, resulting in much lower free concentrations of the drugs in vivo. Finally, midazolam, the most potent ENT1-inhibiting benzodiazepine identified, has a short plasma disposition half-life and is primarily used as an intravenous formulation in perioperative or diagnostics settings (e.g., endoscopic procedures) for anesthesia and sedation, although tablet formulations are also available in some countries for the short-term treatment of insomnia. However, when the most conservative EMA cut-off criterion for potential in vivo relevance of transporter inhibition is applied (i.e. ,Cmax,u × fu/IC50 is ≥ 0.02), it does not appear that recommended intravenous or oral doses of midazolam may be suspected to confer a clinically relevant ENT1 inhibition in vivo (Table 1).Taken together, benzodiazepines as a class are not considered to act as clinically relevant ENT1 inhibitors in vivo, and thus must not be suspended before or during treatment with cladribine tablets.
3.9.1 BCR-ABL TKIs
BCR-ABL TKIs are indicated for the treatment of Philadelphia chromosome-positive chronic myelogenous leukemia and acute lymphoblastic leukemia. The leukemic cells of both hematological malignancies carry a constitutively active BCR-ABL oncogene (BCR: breakpoint cluster region; ABL: Abelson murine leukemia), which is the therapeutic target of inhibition by BCR-ABL TKIs [82].
Damaraju and colleagues examined interactions of the BCR-ABL TKIs bosutinib, dasatinib, imatinib, nilotinib, and ponatinib with recombinant human NTs (ENT1 and ENT2; CNT1, CNT2, and CNT3) produced in yeast Saccharomyces cerevisiae. Nilotinib inhibited ENT1-mediated uridine transport most potently (IC50 0.7 µmol/L) followed by ponatinib > bosutinib > dasatinib > imatinib. Imatinib inhibited CNT2 with an IC50 of 2.3 µmol/L (Table 1). Ponatinib inhibited all five NTs with the greatest effect seen for ENT1 (IC50 9 µmol/L) [83]. Tyrosine kinase inhibitors inhibited [3H]uridine uptake in a competitive manner.
In cultured human CEM lymphoblastoid cells, which possess a single human NT type (ENT1), accumulation of [3H]cytarabine, [3H]cladribine, or [3H]fludarabine was reduced by each of the five TKIs, and also caused a reduction in cell surface expression of the ENT1 protein. The authors concluded that, at concentrations achieved in human plasma, ponatinib and bosutinib may exert their effects on ENT1 by down-regulation of the membrane abundance of ENT1 over prolonged exposure times, whereas imatinib and dasatinib may have less effect on ENT1 activity and levels [83]. When the most conservative EMA cut-off criterion for potential in vivo relevance of transporter inhibition is applied (i.e., Cmax,u × fu/IC50 is ≥ 0.02), only nilotinib exceeded this threshold for possibly relevant ENT1 inhibition in vivo as well as imatinib for CNT2 inhibition (Table 1). However, as all BCR-ABL TKIs are associated with severe myelosuppressive side effects such as grade 3–4 neutropenia and thrombocytopenia, concurrent treatment with cladribine tablets in patients with MS is contraindicated as per prescribing information [3, 6].
3.10 Immunosuppressants
Long-term administration of the immunosuppressive drug cyclosporin A (CsA) was shown in a clinical study in kidney transplant recipients to block ENT-mediated uptake of adenosine to increase its plasma levels. Adenosine plasma levels in CsA-treated kidney transplant recipients were significantly higher (mean 0.76 µmol/L) than in the kidney transplant recipient CsA-untreated control group (mean 0.31 µmol/L). The authors further showed that elevated adenosine plasma levels correlated with CsA blood levels, and that adenosine plasma level increases were due to ENT-mediated adenosine uptake inhibition by CsA [23, 84]. As the initiation of treatment with cladribine tablets is contraindicated in immunocompromised patients, including patients currently receiving immunosuppressive or myelosuppressive therapy, no practical implications of the CsA-mediated ENT1 inhibition are expected for cladribine-treated patients with MS.
4 Discussion and Conclusions
Cladribine has been shown to be a substrate of various NTs. Intestinal absorption and distribution of cladribine throughout the body appear to be exclusively mediated by ENTs and CNTs, specifically by ENT1, ENT2 and ENT4, and CNT2 (low affinity) and CNT3. It is important to note that, owing to the required 3-hour time separation of cladribine dosing from other orally administered drug products, as per the cladribine tablets label, intestinal NT-mediated absorption interactions are not expected to play a significant role in clinical practice. This is because currently available ENT1 inhibitors act in a reversible, competitive, or (rarely) non-competitive manner, and display relatively fast dissociation kinetics with only short-to-moderate residence times between 1 and 44 min at the transporter protein [25, 26]. To the best of our knowledge, there are no irreversible NT inhibitors among currently marketed drugs.
Therefore, this review focusses particularly on NT-based distribution interactions into the primary target cells of cladribine (i.e., lymphocytes), which may go along with a reduced efficacy. The key transporter for the intracellular uptake of cladribine into B and T-lymphocytes is ENT1, with ancillary contributions of ENT2 and CNT2. Thereby, ENT1 and ENT2 work in a bidirectional manner along a transmembrane concentration gradient, i.e., they are also capable of facilitating cladribine efflux from lymphocytes, when plasma concentrations fall below intracellular concentrations.
As the renal clearance of cladribine involves active tubular secretion, and accounts for almost 50% of the total cladribine clearance (22.2 L/h for renal clearance and 23.4 L/h for non-renal clearance), renal transporter inhibition needs in principle also to be considered [16]. All five NTs are expressed in the kidney. It is likely that ENT1 and ENT2 facilitate renal uptake of cladribine through the basolateral membrane (i.e., blood side), while ENT1 may also be involved in the apical urinary excretion of cladribine [11]. Thus, inhibition of renal ENT1/2 may have the potential to alter the renal clearance of cladribine, thereby possibly resulting in higher systemic exposure. Unfortunately, no studies are available to support this mechanistic hypothesis and to quantify possible effects of renal ENT1/2 inhibition on renal cladribine clearance and systemic cladribine exposure. However, effects of ENT1/2 inhibition on the renal clearance of cladribine are expected to be modest as ENT1/2-mediated tubular secretion of cladribine only represents an ancillary renal clearance mechanism on top of glomerular filtration, and may be possibly compensated by other apical renal efflux transporters that have been shown to transport cladribine more (e.g., BCRP) or less (e.g., P-gp) efficiently. Even if systemic cladribine exposure would be increased by renal ENT1/2 inhibition, it is expected that this would not give rise to safety concerns, as cladribine is an inactive prodrug, and at the time of renal ENT1/2 inhibition, ENT1/2 inhibition is also expected to be present at lymphocyte membranes, which means that an increased target-cell uptake and activation of the prodrug cladribine appears unlikely in the presence of a clinically relevant systemic ENT1/2 inhibition despite some systemic cladribine exposure increase.
Taken together, based on our review, the issue of the potential clinical relevance of NT inhibition regarding the safety or efficacy of cladribine can be summarized as follows. The vast majority of NT-inhibiting lifestyle drugs and approved medical products act as specific or at least fairly specific ENT1 inhibitors (Table 1). There are hardly any CNT inhibitors among marketed products, with the exception of the CNT2 inhibitor imatinib (see Table 1), which is contra-indicated in cladribine-treated patients. Hence, the entire story of clinically relevant NT-based DDIs of cladribine is essentially about ENT1 inhibition, which is predominantly of concern in terms of altered cladribine uptake into lymphocytes, thereby hampering clinical efficacy, resulting in a “silent interaction”, which can hardly be detected clinically. This efficacy concern is based on the observation that ENT1 efficiently transports cladribine in cultured human leukemic cells with a Km of 23 μM and overexpression of ENT1 leads to a significant increase in the cytotoxicity of cladribine (10 μM) compared with control cells [31]. In turn, it can be reasonably inferred that ENT1-mediated uptake-inhibition of cladribine goes along with reduced lymphocyte toxicity, thereby altering the clinical efficacy of cladribine. In order to manage cladribine therapy optimally, i.e., to ensure uncompromised target cell uptake to preserve the full therapeutic potential of cladribine, it is of importance that clinicians are aware of the existence of NT-inhibiting medicinal products, various lifestyle drugs, and food components such as dietary purines, which should be avoided during cladribine treatment.
In turn, there is no conceivable mechanism to suggest that NT inhibition may confer any safety risk, as cladribine is an inactive prodrug, requiring target-cell uptake and metabolic activation to exert its pharmacological action. Therefore, it can be reasonably inferred that increased systemic exposure concentrations of the prodrug cladribine, which cannot be excluded to occur because of renal NT inhibition, are unlikely to confer clinically significant adverse reactions. This consideration is supported by the established adverse event profile of cladribine, showing that clinically significant adverse events (e.g., lymphopenia, other white blood cell alterations, and infections and infestations) are altogether closely related to the primary pharmacology of cladribine, which renders the hypothetical possibility of any off-target toxicities mediated by the prodrug cladribine unlikely.
Although the strength of the available evidence on the in vivo relevance of NT inhibition varies, and predictions on the net effects in terms of potential cladribine distribution and exposure alterations are difficult to make, it appears prudent to avoid concomitant treatments and lifestyle drugs with in vitro evidence of a high degree of ENT1/2 inhibition, i.e., for which significant inhibiting activities were shown (i.e., Cmax × fu/Ki or IC50 ≥ 0.02) or for which clinically relevant ENT1 inhibition is suggested by typical adenosine-related adverse effects (e.g., dyspnea, bronchospasm, and bradyarrhythmias) as is the case for ticagrelor and cilostazol or the clinical relevance of ENT1 inhibition is evidenced by increased adenosine plasma levels (e.g., ticagrelor and CsA).
Cardiovascular drugs with significant ENT-inhibiting potential include legacy products such as dipyridamole, dilazep, and cilostazol, which are no longer widely used but are still available in a few countries. These should not be co-administered with cladribine tablets.
Only a few prescription drugs with relevant NT-inhibiting properties have been identified.
The DHP-CBB nimodipine, which is indicated for the prevention of ischemic neurological deficits and cerebral vasospasm after aneurysmal subarachnoid hemorrhage, is another very potent and fairly selective ENT1 inhibitor in vitro, which has been shown to increase plasma adenosine levels upon oral single dosing [77], and it does exceed the regulatory cut-off threshold for possible in vivo relevance (i.e., Cmax × fu/Ki or IC50 ≥ 0.02), and thus is expected to confer a clinically meaningful ENT1 inhibition. Nimodipine should therefore not be co-administered with cladribine tablets. All other DHP-CBBs are unlikely to confer significant ENT1/2 inhibition in vivo.
The P2Y12 receptor antagonist ticagrelor and its major metabolites are potent specific ENT1 inhibitors. Despite their high protein binding, significant ENT1 inhibition has been shown to increase systemic adenosine levels and to elicit prototypical adenosine-related adverse events such as dyspnea and bradyarrhythmias. Therefore, ticagrelor treatment should be suspended for at least 3 days (the mean terminal disposition half-life of ticagrelor ranges between 7.7 and 13.1 h) before initiation of treatment with cladribine tablets, and should only be resumed 1 day after the last dose of cladribine. Alternatively, patients can be switched to other anti-platelet drug products.
Among the class of NSAIDs, only sulindac has been shown to elicit dual competitive ENT1/2 inhibition to a degree that may be relevant in vivo, mainly owing to the effects of its major active metabolite sulindac sulphide. However, even sulindac sulphide does not exceed the regulatory cut-off threshold for possible in vivo relevance (Table 1), and thus is not expected to confer a clinically meaningful ENT1 inhibition. Thus, NSAIDs reported to act as dual competitive ENT1/2 in vitro are not regarded as clinically relevant NT inhibitors, and must not be avoided before or during cladribine treatment.
Some benzodiazepines have also been shown to inhibit ENT1 in vitro, the most potent being midazolam with a Ki of 6 µmol/L, which however does not exceed the regulatory cut-off threshold for possible in vivo relevance (Table 1), and thus is not expected to confer a clinically meaningful ENT1 inhibition. Among the class of TKI inhibitors, nilotinib and ponatinib have been shown to be potent ENT1 inhibitors with potential in vivo relevance, while imatinib was shown to be a fairly selective and potent CNT2 inhibitor.
Among the class of immunosuppressants, CsA was shown to elevate plasma adenosine levels upon long-term administration in kidney transplant patients by about two-fold, presumably by selective ENT1 inhibition. However, as the initiation of treatment with cladribine tablets is contraindicated in immunocompromised patients, including patients currently receiving immunosuppressive or myelosuppressive oncological therapies, no practical implications of the TKI-mediated or CsA-mediated ENT1 inhibition are expected for cladribine-treated patients with MS.
Frequently used lifestyle drugs such as alcohol and cannabis, and in particular inhaled or smoked THC/CBD-containing products, should be avoided before and during treatment with cladribine tablets because of their potent ENT1-inhibiting properties. In addition to ENT1 inhibition, long-term use of alcohol has been shown to result in down-regulation of ENT1 expression. For inhaled/smoked THC/CBD-containing products, it is recommended that patients with MS refrain from the use for at least 1 week before and during treatment with cladribine tablets in order to optimize ENT1-mediated uptake of cladribine into lymphocytes. In turn, oral or oral-mucosal medical THC/CBD products are unlikely to confer a clinically relevant ENT1 inhibition in vivo (Table 1).
Last but not least, although direct evidence is lacking, cladribine tablets should not be taken together with purine-rich meals, as dietary purines have been shown to compete for CNT2/3-mediated intestinal uptake of nucleosidic drugs as shown for ribavirin. However, it has been shown that cladribine tablets can be taken with high-fat high-calorie meals with a low purine content (e.g., the FDA-recommended standard high-fat breakfast).
A principle limitation of our review regarding the assessment of the possible in vivo relevance based on in vitro ENT inhibitor data together with human pharmacokinetic and protein binding data is the lack of specific regulatory (EMA/FDA/PMDA) or scientific (e.g., International Transporter Consortium) guidance for bidirectional equilibrative transporters. We therefore applied to our assessments the most conservative cut-off criterion provided in the EMA DDI guideline, which is the use of inhibitor concentrations of 50-fold Cmax,u divided by IC50 or Ki, which results in a cut-off value of 0.02. Although this cut-off value is conservative, it is acknowledged that it is arbitrary and was not specifically developed for ENTs. However, our review showed that all ENT1-inhibiting substances for which it was shown that they are capable of increasing plasma adenosine concentrations to a significant extent exceed the chosen cut-off value of 0.02, which is a first confirmation of the practical applicability and usefulness of this cut-off for the assessment of possible in vivo relevance of in vitro identified ENT inhibitors. Although this review aimed to optimize the clinical efficacy of cladribine treatment by identification of potent NT inhibitors that should be avoided during treatment with cladribine tablets, the results of this review are considered to some extent generalizable for other treatments with nucleosidic compounds, which may have similar or comparable NT substrate characteristics.
References
The Multiple Sclerosis International Federation. Atlas of MS. 3rd ed. 2020.
Giovannoni G, Butzkueven H, Dhib-Jalbut S, Hobart J, Kobelt G, Pepper G, et al. Brain health: time matters in multiple sclerosis. Mult Scler Relat Disord. 2016;9(Suppl. 1):S5-48.
Mavenclad 10 mg tablets. Summary of product characteristics (SmPC). 2021. https://www.ema.europa.eu/en/documents/product-information/mavenclad-epar-product-information_en.pdf. Accessed 8 Jun 2021.
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372(9648):1502–17.
Giovannoni G, Comi G, Cook S, Rammohan K, Rieckmann P, Soelberg Sørensen P, et al. A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis. N Engl J Med. 2010;362(5):416–26.
Mavenclad prescribing information. 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/022561s000lbl.pdf. Accessed 8 Jul 2021.
Baker D, Herrod SS, Alvarez-Gonzalez C, Zalewski L, Albor C, Schmierer K. Both cladribine and alemtuzumab may effect MS via B-cell depletion. Neurol Neuroimmunol Neuroinflamm. 2017;4(4):e360.
Stuve O, Soelberg Soerensen P, Leist T, Giovannoni G, Hyvert Y, Damian D, et al. Effects of cladribine tablets on lymphocyte subsets in patients with multiple sclerosis: an extended analysis of surface markers. Ther Adv Neurol Disord. 2019;12:1756286419854986.
Ceronie B, Jacobs BM, Baker D, Dubuisson N, Mao Z, Ammoscato F, et al. Cladribine treatment of multiple sclerosis is associated with depletion of memory B cells. J Neurol. 2018;265(5):1199–209.
Carlini F, Ivaldi F, Gualandi F, Boschert U, Centonze D, Matarese G, et al. Different susceptibility of T and B cells to cladribine depends on their levels of deoxycytidine kinase activity linked to activation status. J Neuroimmune Pharmacol. 2021. https://doi.org/10.1007/s11481-021-09994-3.
Hermann R, Krajcsi P, Fluck M, Seithel-Keuth A, Bytyqi A, Galazka A, et al. Review of transporter substrate, inhibitor and inducer characteristics of cladribine. Clin Pharmacokinet. 2021. https://doi.org/10.1007/s40262-021-01065-3.
Comi G, Hartung HP, Kurukulasuriya NC, Greenberg SJ, Scaramozza M. Cladribine tablets for the treatment of relapsing-remitting multiple sclerosis. Expert Opin Pharmacother. 2013;14(1):123–36.
Salvat C, Curchod M-L, Guedj E, Peixoto H, Guerrier M, Wojcik J, et al. Cellular expression profiling of genes involved in the cladribine metabolic pathway: insights into mechanism of action in multiple sclerosis. Mult Scler. 2009;15:5–150.
Soelberg-Sorensen P, Dangond F, Hicking C, Giovannoni G. P1141: innate immune cell counts in patients with relapsing-remitting multiple sclerosis (RRMS) treated with cladribine tablets 3.5 mg/kg in CLARITY and CLARITY Extension. Presented at: 4th Congress of the European Academy of Neurology; 16–19 June 2018;23(s3):598.
Comi G, Cook S, Giovannoni G, Rieckmann P, Sørensen PS, Vermersch P, et al. Effect of cladribine tablets on lymphocyte reduction and repopulation dynamics in patients with relapsing multiple sclerosis. Mult Scler Relat Disord. 2019;29:168–74.
Hermann R, Karlsson MO, Novakovic AM, Terranova N, Fluck M, Munafo A. The clinical pharmacology of cladribine tablets for the treatment of relapsing multiple sclerosis. Clin Pharmacokinet. 2019;58(3):283–97.
Young JD, Yao SY, Baldwin JM, Cass CE, Baldwin SA. The human concentrative and equilibrative nucleoside transporter families, SLC28 and SLC29. Mol Aspects Med. 2013;34(2–3):529–47.
Boswell-Casteel RC, Hays FA. Equilibrative nucleoside transporters: a review. Nucleos Nucleot Nucl. 2017;36(1):7–30.
Cheung KWK, van Groen BD, Spaans E, van Borselen MD, de Bruijn A, Simons-Oosterhuis Y, et al. A comprehensive analysis of ontogeny of renal drug transporters: mRNA analyses, quantitative proteomics, and localization. Clin Pharmacol Ther. 2019;106(5):1083–92.
Oswald S, Müller J, Neugebauer U, Schröter R, Herrmann E, Pavenstädt H, et al. Protein abundance of clinically relevant drug transporters in the human kidneys. Int J Mol Sci. 2019;20(21):5303.
Rosenbrier Ribeiro L, Ian SR. A semi-quantitative translational pharmacology analysis to understand the relationship between in vitro ENT1 inhibition and the clinical incidence of dyspnoea and bronchospasm. Toxicol Appl Pharmacol. 2017;15(317):41–50.
Pastor-Anglada M, Pérez-Torras S. Nucleoside transporter proteins as biomarkers of drug responsiveness and drug targets. Front Pharmacol. 2015;6:13.
Jacobson KA, Reitman ML. Adenosine-related mechanisms in non-adenosine receptor drugs. Cells. 2020;9(4):956.
Pastor-Anglada M, Pérez-Torras S. Emerging roles of nucleoside transporters. Front Pharmacol. 2018;9:606.
Damaraju VL, Elwi AN, Hunter C, Carpenter P, Santos C, Barron GM, et al. Localization of broadly selective equilibrative and concentrative nucleoside transporters, hENT1 and hCNT3, in human kidney. Am J Physiol Renal Physiol. 2007;293(1):F200–11.
Vlachodimou A, Konstantinopoulou K, AP IJ, Heitman LH. Affinity, binding kinetics and functional characterization of draflazine analogues for human equilibrative nucleoside transporter 1 (SLC29A1). Biochem Pharmacol. 2020;172:113747.
Li RW, Tse CM, Man RY, Vanhoutte PM, Leung GP. Inhibition of human equilibrative nucleoside transporters by dihydropyridine-type calcium channel antagonists. Eur J Pharmacol. 2007;568(1–3):75–82.
Owen RP, Badagnani I, Giacomini KM. Molecular determinants of specificity for synthetic nucleoside analogs in the concentrative nucleoside transporter, CNT2. J Biol Chem. 2006;281(36):26675–82.
Ritzel MW, Ng AM, Yao SY, Graham K, Loewen SK, Smith KM, et al. Molecular identification and characterization of novel human and mouse concentrative Na+-nucleoside cotransporter proteins (hCNT3 and mCNT3) broadly selective for purine and pyrimidine nucleosides (system cib). J Biol Chem. 2001;276(4):2914–27.
Badagnani I, Chan W, Castro RA, Brett CM, Huang CC, Stryke D, et al. Functional analysis of genetic variants in the human concentrative nucleoside transporter 3 (CNT3; SLC28A3). Pharmacogenomics J. 2005;5(3):157–65.
King KM, Damaraju VL, Vickers MF, Yao SY, Lang T, Tackaberry TE, et al. A comparison of the transportability, and its role in cytotoxicity, of clofarabine, cladribine, and fludarabine by recombinant human nucleoside transporters produced in three model expression systems. Mol Pharmacol. 2006;69(1):346–53.
Pastor-Anglada M, Molina-Arcas M, Casado FJ, Bellosillo B, Colomer D, Gil J. Nucleoside transporters in chronic lymphocytic leukaemia. Leukemia. 2004;18(3):385–93.
Hiratochi M, Tatani K, Shimizu K, Kuramochi Y, Kikuchi N, Kamada N, et al. Hypouricemic effects of novel concentrative nucleoside transporter 2 inhibitors through suppressing intestinal absorption of purine nucleosides. Eur J Pharmacol. 2012;690(1–3):183–91.
Li L, Koo SH, Limenta LMG, Han L, Lee EJD, Hashim KB, et al. Effect of dietary purines on the pharmacokinetics of orally administered ribavirin. J Clin Pharmacol. 2009;49(6):661–7.
U.S. Department of Health and Human Services. Food and Drug Administration. Center for Drug Evaluation and Research (CDER). Guidance for Industry. Assessing the effects of food on drugs in INDs and NDAs: clinical pharmacology considerations. 2019. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/assessing-effects-food-drugs-inds-and-ndas-clinical-pharmacology-considerations.
Quesnel S, Feinstein A. Multiple sclerosis and alcohol: a study of problem drinking. Mult Scler. 2004;10(2):197–201.
Krauss SW, Ghirnikar RB, Diamond I, Gordon AS. Inhibition of adenosine uptake by ethanol is specific for one class of nucleoside transporters. Mol Pharmacol. 1993;44(5):1021–6.
Nagy LE. Ethanol metabolism and inhibition of nucleoside uptake lead to increased extracellular adenosine in hepatocytes. Am J Physiol. 1992;262(5 Pt 1):C1175–80.
Acevedo CG, Huambachano A, Perez E, Rojas S, Bravo I, Contreras E. Effect of ethanol on human placental transport and metabolism of adenosine. Placenta. 1997;18(5–6):387–92.
Allen-Gipson DS, Jarrell JC, Bailey KL, Robinson JE, Kharbanda KK, Sisson JH, et al. Ethanol blocks adenosine uptake via inhibiting the nucleoside transport system in bronchial epithelial cells. Alcohol Clin Exp Res. 2009;33(5):791–8.
Coe IR, Dohrman DP, Constantinescu A, Diamond I, Gordon AS. Activation of cyclic AMP-dependent protein kinase reverses tolerance of a nucleoside transporter to ethanol. J Pharmacol Exp Ther. 1996;276(2):365–9.
Coe IR, Yao L, Diamond I, Gordon AS. The role of protein kinase C in cellular tolerance to ethanol. J Biol Chem. 1996;271(46):29468–72.
Nagy LE, Diamond I, Collier K, Lopez L, Ullman B, Gordon AS. Adenosine is required for ethanol-induced heterologous desensitization. Mol Pharmacol. 1989;36(5):744–8.
Nagy LE, Diamond I, Casso DJ, Franklin C, Gordon AS. Ethanol increases extracellular adenosine by inhibiting adenosine uptake via the nucleoside transporter. J Biol Chem. 1990;265(4):1946–51.
Ramadan A, Naydenova Z, Stevanovic K, Rose JB, Coe IR. The adenosine transporter, ENT1, in cardiomyocytes is sensitive to inhibition by ethanol in a kinase-dependent manner: implications for ethanol-dependent cardioprotection and nucleoside analog drug cytotoxicity. Purinergic Signal. 2014;10(2):305–12.
Rice J, Cameron M. Cannabinoids for treatment of MS symptoms: state of the evidence. Curr Neurol Neurosci Rep. 2018;18(8):50.
Multiple Sclerosis Society UK. Cannabis. 2014. https://www.mssociety.org.uk/about-ms/treatments-and-therapies/cannabis#:~:text=One%20in%20five%20people%20with,up%20of%20compounds%20called%20cannabinoids. Accessed 20 Apr 2021.
Carrier EJ, Auchampach JA, Hillard CJ. Inhibition of an equilibrative nucleoside transporter by cannabidiol: a mechanism of cannabinoid immunosuppression. Proc Natl Acad Sci USA. 2006;103(20):7895–900.
Marinol (dronabiol) capsules. Summary of product characteristics. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018651s029lbl.pdf. Accessed 20 Apr 2021.
Syndros (dronabinol) oral solution. Summary of product characteristics. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/205525s003lbl.pdf. Accessed 20 Apr 2021.
Sativex product monograph. 2019. https://omr.bayer.ca/omr/online/sativex-pm-en.pdf. Accessed 20 Apr 2021.
Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol. 1992;16(5):276–82.
Millar SA, Stone NL, Yates AS, O’Sullivan SE. A systematic review on the pharmacokinetics of cannabidiol in humans. Front Pharmacol. 2018;9:1365.
Swortwood MJ, Newmeyer MN, Andersson M, Abulseoud OA, Scheidweiler KB, Huestis MA. Cannabinoid disposition in oral fluid after controlled smoked, vaporized, and oral cannabis administration. Drug Test Anal. 2017;9(6):905–15.
Persantine tablets. US summary of product characteristics. 2019. https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Persantine%20Tabs/PersTab.pdf. Accessed 20 Apr 2021.
Dilazep hydrochloride tablets 100mg "SAWAI". Summary of product characteristics. 2014. Available from: https://www.rad-ar.or.jp/siori/english/kekka.cgi?n=39136. Accessed 27 Oct 2020.
Haustein K-O. Dipyridamol: sein heutiger Stellenwert. Dtsch Arztebl Int. 1998;95(14):A-817.
Visser F, Vickers MF, Ng AM, Baldwin SA, Young JD, Cass CE. Mutation of residue 33 of human equilibrative nucleoside transporters 1 and 2 alters sensitivity to inhibition of transport by dilazep and dipyridamole. J Biol Chem. 2002;277(1):395–401.
Rehan S, Shahid S, Salminen TA, Jaakola VP, Paavilainen VO. Current progress on equilibrative nucleoside transporter function and inhibitor design. SLAS Discov. 2019;24(10):953–68.
Patil SB, Norman K, Robins S, Crosdale D, Nylander S, Francis S, et al. Inhibition of thrombosis by AZD6140 via selective blockade of the P2Y12 receptor in a murine laser-injury model. J Thromb Haemost. 2007. https://doi.org/10.1111/J.1538-7836.2007.TB03189.X.
Nylander S, Femia EA, Scavone M, Berntsson P, Asztély AK, Nelander K, et al. Ticagrelor inhibits human platelet aggregation via adenosine in addition to P2Y12 antagonism. J Thromb Haemost. 2013;11(10):1867–76.
Armstrong D, Summers C, Ewart L, Nylander S, Sidaway JE, van Giezen JJ. Characterization of the adenosine pharmacology of ticagrelor reveals therapeutically relevant inhibition of equilibrative nucleoside transporter 1. J Cardiovasc Pharmacol Ther. 2014;19(2):209–19.
van Giezen JJ, Sidaway J, Glaves P, Kirk I, Björkman JA. Ticagrelor inhibits adenosine uptake in vitro and enhances adenosine-mediated hyperemia responses in a canine model. J Cardiovasc Pharmacol Ther. 2012;17(2):164–72.
Sillén H, Cook M, Davis P. Determination of unbound ticagrelor and its active metabolite (AR-C124910XX) in human plasma by equilibrium dialysis and LC-MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci. 2011;879(23):2315–22.
Alexopoulos D, Moulias A, Koutsogiannis N, Xanthopoulou I, Kakkavas A, Mavronasiou E, et al. Differential effect of ticagrelor versus prasugrel on coronary blood flow velocity in patients with non-ST-elevation acute coronary syndrome undergoing percutaneous coronary intervention: an exploratory study. Circ Cardiovasc Interv. 2013;6(3):277–83.
Wittfeldt A, Emanuelsson H, Brandrup-Wognsen G, van Giezen JJ, Jonasson J, Nylander S, et al. Ticagrelor enhances adenosine-induced coronary vasodilatory responses in humans. J Am Coll Cardiol. 2013;61(7):723–7.
Bonello L, Laine M, Kipson N, Mancini J, Helal O, Fromonot J, et al. Ticagrelor increases adenosine plasma concentration in patients with an acute coronary syndrome. J Am Coll Cardiol. 2014;63(9):872–7.
Cannon CP, Husted S, Harrington RA, Scirica BM, Emanuelsson H, Peters G, et al. Safety, tolerability, and initial efficacy of AZD6140, the first reversible oral adenosine diphosphate receptor antagonist, compared with clopidogrel, in patients with non-ST-segment elevation acute coronary syndrome: primary results of the DISPERSE-2 trial. J Am Coll Cardiol. 2007;50(19):1844–51.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Pletal 50 mg tablets. Summary of product characteristics. 2016. https://www.medicines.org.uk/emc/product/164/smpc#gref. Accessed 20 Apr 2021.
Liu Y, Shakur Y, Yoshitake M, Kambayashi Ji J. Cilostazol (pletal): a dual inhibitor of cyclic nucleotide phosphodiesterase type 3 and adenosine uptake. Cardiovasc Drug Rev. 2001;19(4):369–86.
Wang YJ, Li R, Yan JW, Wan YN, Tao JH, Chen B, et al. The epidemiology of alcohol consumption and multiple sclerosis: a review. Neurol Sci. 2015;36(2):189–96.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Nimotop 30mg tablets. Summary of product characteristics, 2017. https://www.medicines.org.uk/emc/medicine/8086/SPC#gref. Accessed 20 Apr 2021.
Deckert J, Bereznai B, Hennemann A, Gsell W, Götz M, Fritze J, et al. Nimodipine inhibits [3H]nitrobenzylthioinosine binding to the adenosine transporter in human brain. Eur J Pharmacol. 1993;238(1):131–3.
Kirsten R, Nelson K, Kirsten D, Heintz B. Clinical pharmacokinetics of vasodilators. Part I. Clin Pharmacokinet. 1998;34(6):457–82.
Blardi P, Urso R, De Lalla A, Volpi L, Perri TD, Auteri A. Nimodipine: drug pharmacokinetics and plasma adenosine levels in patients affected by cerebral ischemia. Clin Pharmacol Ther. 2002;72(5):556–61.
Li RW, Yang C, Sit AS, Lin SY, Ho EY, Leung GP. Physiological and pharmacological roles of vascular nucleoside transporters. J Cardiovasc Pharmacol. 2012;59(1):10–5.
Li RW, Seto SW, Au AL, Kwan YW, Chan SW, Lee SM, et al. Inhibitory effect of nonsteroidal anti-inflammatory drugs on adenosine transport in vascular smooth muscle cells. Eur J Pharmacol. 2009;612(1–3):15–20.
Meador W, Salter AR, Rinker 2nd JR. Symptomatic management of multiple sclerosis-associated tremor among participants in the NARCOMS Registry. Int J MS Care. 2016;18(3):147–53
Seubert CN, Morey TE, Martynyuk AE, Cucchiara RF, Dennis DM. Midazolam selectively potentiates the A(2A) - but not A1-receptor-mediated effects of adenosine: role of nucleoside transport inhibition and clinical implications. Anesthesiology. 2000;92(2):567–77.
An X, Tiwari AK, Sun Y, Ding PR, Ashby CR Jr, Chen ZS. BCR-ABL tyrosine kinase inhibitors in the treatment of Philadelphia chromosome positive chronic myeloid leukemia: a review. Leuk Res. 2010;34(10):1255–68.
Damaraju VL, Weber D, Kuzma M, Cass CE, Sawyer MB. Selective inhibition of human equilibrative and concentrative nucleoside transporters by BCR-ABL kinase inhibitors: identification of key hENT1 amino acid residues for interaction with BCR-ABL kinase inhibitors. J Biol Chem. 2016;291(36):18809–17.
Guieu R, Dussol B, Devaux C, Sampol J, Brunet P, Rochat H, et al. Interactions between cyclosporine A and adenosine in kidney transplant recipients. Kidney Int. 1998;53(1):200–4.
Dresse A, Chevolet C, Delapierre D, Masset H, Weisenberger H, Bozler G, et al. Pharmacokinetics of oral dipyridamole (Persantine) and its effect on platelet adenosine uptake in man. Eur J Clin Pharmacol. 1982;23(3):229–34.
Wang C, Lin W, Playa H, Sun S, Cameron K, Buolamwini JK. Dipyridamole analogs as pharmacological inhibitors of equilibrative nucleoside transporters: identification of novel potent and selective inhibitors of the adenosine transporter function of human equilibrative nucleoside transporter 4 (hENT4). Biochem Pharmacol. 2013;86(11):1531–40.
Lenz T, Wilson A. Clinical pharmacokinetics of antiplatelet agents used in the secondary prevention of stroke. Clin Pharmacokinet. 2003;42(10):909–20.
Sambhi MP, Kannan R, Thananopavarn C, Ookhtens M, Gudenzi M. Therapeutic tolerance, hemodynamic effects, and oral dose kinetics of dilazep dihydrochloride in hypertensive patients. J Pharm Sci. 1989;78(4):281–4.
Brilique 60 mg film-coated tablets. Summary of product characteristics. 2015. https://www.ema.europa.eu/en/documents/product-information/brilique-epar-product-information_en.pdf. Accessed 18 Oct 2021.
Eschenhagen T. Treatment of hypertension. In: Brunton LL, Hilal-Dandan R, Knollmann BC, editors. Goodman & Gilman's: the pharmacological basis of therapeutics, 13th edn. New York: McGraw-Hill Education; 2017.
Dow RJ, Graham DJM. A review of the human metabolism and pharmacokinetics of nicardipine hydrochloride. Br J Clin Pharmacol. 1986;22(Suppl. 3):195s–202s.
Kirch W, Hutt HJ, Heidemann H, Rämsch K, Janisch HD, Ohnhaus EE. Drug interactions with nitrendipine. J Cardiovasc Pharmacol. 1984;6(Suppl. 7):S982–5.
Lasseter KC, Shamblen EC, Murdoch AA, Burkholder DE, Krol GJ, Taylor RJ Jr, et al. Steady-state pharmacokinetics of nitrendipine in hepatic insufficiency. J Cardiovasc Pharmacol. 1984;6(Suppl. 7):S977–81.
Kann J, Krol GJ, Raemsch KD, Burkholder DE, Levitt MJ. Bioequivalence and metabolism of nitrendipine administered orally to healthy volunteers. J Cardiovasc Pharmacol Ther. 1984;6(Suppl. 7):S968–73.
Goa KL, Sorkin EM. Nitrendipine. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in the treatment of hypertension. Drugs. 1987;33(2):123–55.
Perini JA, Suarez-Kurtz G. Impact of CYP2C9*3/*3 genotype on the pharmacokinetics and pharmacodynamics of piroxicam. Clin Pharmacol Ther. 2006;80(5):549–51.
Link B, Haschke M, Grignaschi N, Bodmer M, Aschmann YZ, Wenk M, et al. Pharmacokinetics of intravenous and oral midazolam in plasma and saliva in humans: usefulness of saliva as matrix for CYP3A phenotyping. Br J Clin Pharmacol. 2008;66(4):473–84.
Midazolam 5mg/ml, solution for injection/infusion. Summary of product characteristics. 2020. Available from: https://www.medicines.org.uk/emc/product/6420/smpc#gref. Accessed 18 Oct 2021.
Tian X, Zhang H, Heimbach T, He H, Buchbinder A, Aghoghovbia M, et al. Clinical pharmacokinetic and pharmacodynamic overview of nilotinib, a selective tyrosine kinase inhibitor. J Clin Pharmacol. 2018;58(12):1533–40.
Iclusig® 15/30/45 mg film-coated tablets. Summary of product characteristics. 2018. https://www.ema.europa.eu/en/documents/product-information/iclusig-epar-product-information_en.pdf. Accessed 18 Oct 2021.
Bosulif® 100/400/500 mg film-coated tablets. Summary of product characteristics. 2021. https://www.ema.europa.eu/en/documents/product-information/bosulif-epar-product-information_en.pdf. Accessed 18 Oct 2021.
Christopher LJ, Cui D, Wu C, Luo R, Manning JA, Bonacorsi SJ, et al. Metabolism and disposition of dasatinib after oral administration to humans. Drug Metabol Dispos. 2008;36(7):1357–64.
Sprycel® 20/50/70/ 80/100/140 mg film-coated tablets. Summary of product characteristics. 2016. https://www.ema.europa.eu/en/documents/product-information/sprycel-epar-product-information_en.pdf. Accessed 18 Oct 2021.
Glivec® 100 mg hard capsules. Summary of product characteristics. 2006. https://www.ema.europa.eu/en/documents/product-information/glivec-epar-product-information_en.pdf. Accessed 18 Oct 2021.
Acknowledgements
The authors thank the patients, investigators, and co-investigators involved in the cladribine tablets clinical trial program, as well as study teams at the participating centers, at Merck KGaA, Darmstadt, Germany (CrossRef Funder ID: https://doi.org/10.13039/100009945). The authors acknowledge Ella Palmer and Steve Winter of inScience Communications, Springer Healthcare Ltd, UK, for medical writing support, funded by Merck KGaA Darmstadt, Germany.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
RH served as an external clinical pharmacology expert advisor for various aspects in the clinical development of cladribine, and received financial support for research, consulting, and training services from Merck Healthcare KGaA, Darmstadt, Germany. PK served as an external pharmacology expert advisor for in vitro transporter studies. He is a co-founder of Habilitas Kft, which received financial support for generation of an Internal Transporter Report from Merck Healthcare KGaA Darmstadt, Germany. He was also an employee of Solvo Biotechnology, Budapest, Hungary, outside this advisory work. ASK, MF, and AB are employees of Merck Healthcare KGaA Darmstadt, Germany. AG was an employee of Ares Trading SA, Eysins, Switzerland, an affiliate of Merck KGaA at the time of the study, and is currently a consultant to Merck Healthcare KGaA, Darmstadt, Germany. AM was at the time of preparation of this manuscript, an employee of the Merck Institute of Pharmacometrics, Lausanne, Switzerland, an affiliate of Merck KGaA.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Any requests for data by qualified scientific and medical researchers for legitimate research purposes will be subject to Merck KGaA’s Data Sharing Policy. All requests should be submitted in writing to Merck KGaA’s data sharing portal: https://www.merckgroup.com/en/research/our-approach-to-research-and-development/healthcare/clinical-trials/commitment-responsible-data-sharing.html. When Merck KGaA has a co-research, co-development, or co-marketing or co-promotion agreement, or when the product has been out-licensed, the responsibility for disclosure might be dependent on the agreement between parties. Under these circumstances, Merck KGaA will endeavor to gain agreement to share data in response to requests.
Code Availability
Not applicable.
Author Contributions
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hermann, R., Krajcsi, P., Fluck, M. et al. Cladribine as a Potential Object of Nucleoside Transporter-Based Drug Interactions. Clin Pharmacokinet 61, 167–187 (2022). https://doi.org/10.1007/s40262-021-01089-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-021-01089-9