Abstract
Treatment options for chronic hepatitis C virus (HCV) infection have drastically changed since the development and licensing of new potent direct-acting antivirals (DAAs). The majority of DAAs are extensively metabolized by liver enzymes and have the ability to influence cytochrome P450 (CYP) enzymes. Additionally, these DAAs are both substrates and inhibitors of drug transporters, which makes the DAAs both possible victims or perpetrators of drug–drug interactions (DDIs). There is a high prevalence of mental illnesses such as depression or psychosis in HCV-infected patients; therefore, psychoactive medications are frequently co-administered with DAAs. The majority of these psychoactive medications are also metabolized by CYP enzymes but remarkably little information is available on DDIs between psychoactive medications and DAAs. Hence, the aim of this review is to provide an overview of the interaction mechanisms between DAAs and psychoactive agents. In addition, we describe evidenced-based interactions between DAAs and psychoactive drugs and identify safe options for the simultaneous treatment of mental illnesses and chronic HCV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Escitalopram and citalopram have been studied in combination with most direct-acting antivirals (DAAs) and either of these drugs can be safely combined with hepatitis C virus (HCV) treatment. |
No formal interaction studies between psychoactive agents and sofosbuvir or ledipasvir have been performed in humans. However, these DAAs are generally neither victims nor perpetrators of drug interactions and can therefore be safely used in combination with psychoactive drugs. |
Boceprevir, simeprevir, and the combination paritaprevir/ritonavir plus ombitasvir with dasabuvir are most likely to cause drug interactions via the inhibition of cytochrome P450 (CYP) 3A4. Therefore, caution must be exercised when CYP3A4 substrates such as midazolam and/or quetiapine are co-administered with these DAAs. |
1 Introduction
One of the components previously used in the treatment regimen for hepatitis C virus (HCV) is pegylated interferon; however, it has major adverse effects on mental health and depression was a commonly seen adverse event [1]. Since the development of novel direct-acting antivirals (DAAs), pegylated interferon is no longer used in the treatment of HCV infections in resource-rich settings. However, the prevalence of mental disorders remains high among untreated HCV-infected patients [2]. For example, a retrospective study reported that 86 % of HCV-infected patients had at least one psychiatric, drug-, or alcohol use-related disorder recorded in their patient charts. The most common conditions were depressive disorders (50 %), psychosis (50 %), anxiety disorders (41 %), post-traumatic stress disorders (34 %), and bipolar disorders (16 %) [3]. Another study reported a prevalence of 41 % for anxiety and 27 % for depression in HCV-infected individuals (n = 395) [4]. One explanation for this high prevalence was that patients with mental disorders are more likely to have a drug addiction, because intravenous drug use is a major route of HCV transmission [5].
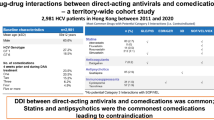
The results from a cross-sectional study were in agreement with the high prevalence of mental disorders. In that study, 16 % of the HCV-infected patients were on antidepressants and 10 % were on antipsychotics (n = 3716) [6]. This corresponds with data from a Dutch nationwide survey in which benzodiazepines, drugs used for treating opioid dependence, and selective serotonin reuptake inhibitors (SSRIs) were among the drugs most frequently used by chronic HCV-infected patients [7].
The use of antipsychotics and antidepressants during DAA therapy increases the risk of drug-drug interactions (DDIs). Both DAAs and psychoactive agents are extensively metabolized in the liver and have the ability to affect the activities of various enzymes (e.g., cytochrome P450 [CYP]) and drug transporters (e.g., P-glycoprotein [P-gp]). This makes DAAs as well as psychoactive agents possible victims (objects of DDIs) and perpetrators (causes of DDIs) of drug interactions, which could negatively affect treatment outcomes as a result of adverse effects (increased plasma concentrations) or treatment failure (decreased plasma concentrations) [8, 9]. In order to interpret the DDIs between DAAs and psychoactive agents, it is important to have sufficient knowledge of their therapeutic ranges. Benzodiazepines, tricyclic antidepressants (TCAs), and antipsychotics have a narrow therapeutic range, while SSRIs have a broad therapeutic range. Generally, drugs with narrow therapeutic ranges are more likely to have clinically relevant DDIs than drugs with large therapeutic ranges [10]. DAAs have a large therapeutic range, which makes them less susceptible to the effects of an increase or decrease in their plasma concentrations caused by, for example, CYP inhibition or induction. However, extremely low plasma concentrations could lead to virologic failure.
Little information is available on interactions between DAAs and psychoactive agents. Therefore, the aim of this review is to provide an overview of the interaction mechanisms of DAAs and psychoactive agents. In addition, we describe evidenced-based interactions between DAAs and psychoactive drugs and identify safe options for treatment of the simultaneous treatment of mental illnesses and HCV infection.
2 Methods
We searched PubMed (1946–January 2016) and EMBASE (1947–January 2016) to identify peer-reviewed studies. The search covered all DAAs recommended in European and US guidelines [11, 12] and licensed by the European Medicines Agency (EMA) and US Food and Drug Administration (FDA). The DAAs included protease inhibitors (PIs) (boceprevir, simeprevir, paritaprevir, and grazoprevir), NS5A inhibitors (daclatasvir, ledipasvir, ombitasvir, and elbasvir), and NS5B polymerase inhibitors (sofosbuvir and dasabuvir). Telaprevir (PI) was excluded from the review because it has limited use in current therapy. We also referred to the work published by Kiser and colleagues [13] for more information about telaprevir and DDIs between DAAs and psychoactive drugs.
The psychoactive agents included were SSRIs, TCAs, typical and atypical antipsychotics, benzodiazepines, monoamine oxidase inhibitors, lithium, and St John’s wort.
The Google and Google Scholar search engines, and ClinicalTrials.gov (http://www.clinicaltrials.gov) website and the Liverpool drug interaction database (http://www.hep-druginteractions.org) were used to identify conference papers and abstracts. All searches were performed in English. The search items contained generic and/or brand names of the drugs and included terms such as antidepressant, antipsychotic, sedative, and tranquilizer.
Information about the pharmacokinetics and metabolism of the DAAs and psychoactive agents were obtained from the Summary of Product Characteristics (SmPC) and FDA prescribing information for each drug as well as from the Lexicomp database (available via http://www.uptodate.com). Enzyme inhibitors and inducers were defined as being strong, moderate, or weak if they changed the area under the plasma concentration–time curve (AUC) of a substrate by 5-fold, >2 to <5-fold, and <2-fold, respectively. Substrates were also grouped as being minor and major substrates of enzymes. These groupings were based on the clinical relevance of the potential interaction described by Lexicomp (http://www.uptodate.com) [14, 15].
3 Drug-Drug Interaction (DDI) Mechanisms: Direct-Acting Antivirals (DAAs)
In this section, we elaborate on the mechanisms by which DAAs can be perpetrators and/or victims of DDIs. We focused on interactions through hepatic drug metabolism and drug transporters because they are the most important pathways underlying interactions between DAAs and psychoactive agents. These mechanisms are illustrated using examples of drug interactions between DAAs and psychoactive agents or non-psychoactive drugs, which were studied in healthy volunteers.
Tables 1 and 2 give an overview of the involvement of enzymes and drug transporters in the metabolism of DAAs and psychoactive agents, respectively. Table 3 shows the results of drug interaction studies performed between DAAs and psychoactive drugs.
3.1 Phase I and II Reactions: DAAs as Perpetrators
Drugs that influence drug-metabolizing enzymes (perpetrators) such as CYP and uridine diphosphate glucuronyltransferase (UGT) have the ability to affect the plasma concentration of substrates of the enzymes (victims). Inhibitors of CYP and UGT generally cause an increased plasma concentration of the victim, while inducers usually lower the plasma concentration of the victim.
Ritonavir is included in the fixed-dose combination with paritaprevir, ombitasvir, and dasabuvir to ‘boost’ the pharmacokinetic characteristics of paritaprevir through the inhibition of CYP3A4; this opens the door for DDIs to occur. For example, the AUC and maximum plasma concentration (C max) of orally administered midazolam, a CYP3A4 substrate, increased ~26-fold and ~4-fold, respectively, when midazolam was co-administered with ritonavir (note: the interaction between ritonavir and midazolam is studied in the absence of paritaprevir, ombitasvir, or dasabuvir) [16]. Increases in the plasma concentration of midazolam have also been observed when the drug was administered with boceprevir, simeprevir, and grazoprevir, which are also CYP3A4 inhibitors. Boceprevir is a strong inhibitor of CYP3A4, while simeprevir and grazoprevir are mild CYP3A4 inhibitors (Table 3) [17–19].
UGTs are inhibited by DAAs such as ombitasvir, dasabuvir, and paritaprevir. Lorazepam (benzodiazepine) is a UGT substrate; however, this interaction has not been studied. Interaction studies between furosemide (UGT1A1 substrate) and combination regimen paritaprevir/ritonavir, ombitasvir, and dasabuvir have indicated the importance of UGT inhibition. Results from these studies showed that the AUC and C max of furosemide were increased by 8 and 42 %, respectively. As a result of this, a reduction in the dose of furosemide of up to 50 % might be required if the drugs have to be co-administered [20].
3.2 Phase I and II Reactions: DAAs as Victims
DAAs, e.g., daclatasvir, simeprevir, grazoprevir, and elbasvir, are predominantly metabolized by CYP3A4/5 in the liver and gastrointestinal tract. Thus, caution is needed when DAAs are administered with strong inducers or inhibitors of CYP3A4. A reduced plasma concentration of DAAs creates a potential risk of resistance of the virus to the administered drug and/or virologic failure, while elevated drug concentrations increase the risk of adverse events. Most psychoactive agents do not strongly inhibit or induce CYP3A4 and, thus, we do not expect DAAs to be victims of psychoactive agents. St John’s wort, which is a psychoactive agent, is the exception; it is a strong CYP3A4 inducer. However, co-administration of boceprevir and St John’s wort showed only a slight decrease in the plasma concentration of boceprevir (9 %) [21].
DAAs are not metabolized by UGT or other phase II enzymes; therefore, phase II-mediated DDIs with DAAs as victims are not usually expected.
3.3 Drug Transporters: DAAs as Perpetrators
DAAs inhibit various drug transporters such as the efflux transporters P-gp and breast cancer resistance protein (BCRP) (Table 1), which are, among other located at the blood–brain barrier (BBB). Little information is available on DDIs between psychoactive agents and drug transporters. However, it is known that amitriptyline and risperidone are P-gp substrates (Table 2). Accordingly, inhibition of these transporters increases substrate concentrations in the cerebrospinal fluid [22]. Since the pharmacological action of psychoactive drugs takes place in the brain, inhibition of P-gp can result in an increased pharmacological effect.
No formal interaction studies have been conducted between the P-gp substrates and DAAs. The effect of P-gp inhibition by DAAs has been studied using digoxin, which is a known P-gp substrate. Boceprevir had a minor influence on plasma digoxin concentrations (an increase in AUC and C max by 19 and 18 %, respectively) [17]. Daclatasvir and simeprevir also affected digoxin plasma concentrations; the AUC of digoxin was increased by 27 and 39 %, and C max was increased by 65 and 31 %, respectively [18, 23]. It should be noted that these interactions between the P-gp inhibitors and digoxin were driven by the concentration of digoxin in the intestinal lumen, which is high after oral intake. For psychoactive drugs, interactions with P-gp inhibitors take place at the BBB. This is affected by the systemic concentration of the P-gp substrate instead of the concentration in the lumen. Therefore, it is difficult to predict possible interactions between DAAs and psychoactive drugs from these results. Additionally, the clinical relevance of P-gp inhibition by DAAs depends on the inhibitory potential of the perpetrator and the therapeutic range of the victim (see Sect. 4).
Many DAAs are inhibitors of organic anion-transporting polypeptide (OATP) 1B1 and OATP1B3, which are uptake transporters. No psychoactive drug is a substrate of OATPs; hence, these transporters are not discussed in this review.
3.4 Drug Transporters: DAAs as Victims
Most DAAs are substrates of P-gp and OATPs; therefore, DAAs are possible victims when psychoactive agents inhibit or induce these transporters. However, there are limited data available on psychoactive agents and transporters. An example demonstrating the importance of a transporter-mediated interaction is the contraindication of the co-administration of grazoprevir with OATP1B1/3 inhibitors.
4 DDI Mechanisms: Psychoactive Agents
Table 2 provides an overview of the enzymes and transporters involved in the metabolism of psychoactive agents. In this section, we describe the mechanisms by which psychoactive agents can be victims and perpetrators of DDIs.
4.1 Psychoactive Agents as Perpetrators
In general, psychoactive agents are more often victims of DDIs than perpetrators. For example, benzodiazepines have limited influence on drug-metabolizing enzymes and transporters (Table 2).
Various antipsychotics, SSRIs, and TCAs have the potential to inhibit CYP2D6, which makes these drugs perpetrators of drug interactions. However, the currently available DAAs are not metabolized by CYP2D6 and therefore DDIs via this pathway are not expected (Tables 2, 3).
4.2 Psychoactive Agents as Victims
Most benzodiazepines are substrates of various CYP enzymes, such as CYP3A4, CYP2B6, CYP2C19, and CYP1A2; therefore, benzodiazepines are potential victims of DDIs. Benzodiazepines have a narrow therapeutic range and a strong concentration–effect relationship [24]; thus, increased plasma concentrations are likely to cause increased toxicity.
Midazolam is a model substrate of CYP3A4; therefore, interactions between midazolam and DAAs have been extensively studied. For example, oral co-administration of midazolam and boceprevir resulted in an increase in the midazolam AUC of 430 % and an increase in its C max of 177 %. As a result, co-administration of midazolam and boceprevir is contraindicated [17]. Similarly, an increase in the plasma concentration of midazolam is expected when it is administered with paritaprevir/ritonavir, ombitasvir, and dasabuvir; therefore, this co-administration is also contraindicated [20]. Interactions between midazolam and simeprevir or grazoprevir have both been studied and increased midazolam AUC and C max values were observed; thus, caution is needed with co-administration [18, 19]. On the other hand, daclatasvir has been shown to have little effect on midazolam exposure [23].
SSRIs are hepatically metabolized by various CYP enzymes (e.g., CYP3A4, CYP2D6, CYP2C9, and CYP2C19), particularly CYP3A4. Theoretically, this puts patients at risk when they are also taking DAAs. However, SSRIs have a broad therapeutic range; therefore, increased plasma concentrations of SSRIs are not likely to result in significant toxicities [10]. For instance, the co-administration of escitalopram (CYP3A4 substrate) and DAAs such as boceprevir, simeprevir, or the combination of paritaprevir/ritonavir, ombitasvir, and dasabuvir did not result in a clinically relevant increase in the escitalopram plasma concentration [17, 18, 20].
Antipsychotics are metabolized in the liver by a variety of CYP enzymes, as shown in Table 2. CYP3A4 and CYP2D6 are involved in this metabolism; however, they can be inhibited by DAAs. Most antipsychotics have a narrow therapeutic range. Therefore, DDIs involving antipsychotics can result in clinically relevant outcomes, especially with strong CYP3A4 inhibitors such as boceprevir and ritonavir. However, no interaction studies have been conducted so far. Theoretically, interactions might occur with, for example, strong CYP3A4 inhibitors such as boceprevir and ritonavir.
5 Clinical Guidance
In this section, we provide guidance for clinical decision making regarding the use of a combined treatment of DAAs and psychoactive drugs. Most potential drug interactions have not been subjected to rigid pharmacokinetic testing in humans, and recommendations are often based on theoretical interpretations of the pharmacokinetics characteristics of drugs.
We believe that a relevant interaction only occurs when a drug (victim) is metabolized to a ‘major’ or ‘moderate’ extent. Major or moderate substrate status is based on the potential clinically relevant drug interaction as described by Lexicomp [15]. A major status indicates that the regimen should be modified, whereas a moderate status implies that the therapy should be monitored. Consequently, a drug should have strong (>5-fold increase in substrate AUC) or moderate (2- to 5-fold increase in substrate AUC) influence on an enzyme/transporter (perpetrator) in order to cause an interaction (Tables 4, 5, 6, 7, 8, 9, 10).
5.1 Protease Inhibitors
5.1.1 Boceprevir
Table 4 shows benzodiazepines, antidepressants, and antipsychotics that are safe to combine with boceprevir. Of the currently available DAAs, boceprevir is one of the most potent CYP3A4 inhibitors. Therefore, we do not recommend combining boceprevir and drugs primarily metabolized by CYP3A4, especially if they have a narrow therapeutic range (a contraindication).
Co-administration of midazolam and boceprevir (both oral and parenteral) is contraindicated since the midazolam AUC and C max are both significantly increased [17]. This exceptional increase was not observed with other DAAs, which emphasizes the strong inhibitory potential of boceprevir on CYP3A4.
On the other hand, no dose adjustment is required when escitalopram is administered with boceprevir. This is unexpected as escitalopram is a CYP3A4 substrate. It is possible that there is involvement of other unknown enzymes or transporters; hence, the underlying mechanism cannot be explained [17].
Boceprevir is also a P-gp inhibitor. Theoretically, this inhibition could have an impact on P-gp substrates; however, it seems to have minimal clinical relevance due to the mild inhibition of P-gp by boceprevir [17, 22]. Boceprevir may not be a victim of any DDIs with benzodiazepines, SSRIs, TCAs, or antipsychotics, as studies with midazolam and escitalopram have shown [17]. Additionally, interaction studies between St John’s wort and boceprevir showed no alterations in the plasma concentration of boceprevir; hence, this combination is safe to use [17, 21].
Finally, physicians should take care when prescribing boceprevir in combination with drugs that might prolong the QT interval and are metabolized by CYP3A4 [17]. For instance, SSRIs and TCAs may influence the QT interval and serious pharmacodynamic interactions may occur when they are administered with boceprevir (Table 4).
5.1.2 Simeprevir
Table 4 shows psychoactive medications that can be safely combined with simeprevir. Simeprevir inhibits intestinal CYP3A4 and therefore only interactions with orally administered medications are relevant. Thus, intravenous midazolam can be used safely with simeprevir but oral midazolam should be used with caution, as the AUC and C max of midazolam are increased by 45 and 31 %, respectively, when the two are co-administered [18].
Studies have been conducted of escitalopram and it can be safely used in combination with simeprevir [18].
Simeprevir inhibits P-gp and OATP1B1. Simeprevir has a higher impact than boceprevir on the transport activity of P-gp, as indicated in Sect. 3.3. Therefore, inhibition of P-gp by simeprevir may lead to a small increase in concentrations of P-gp substrates (e.g., risperidone and nortriptyline) in the brain. However, the clinical relevance seems limited [18].
Simeprevir is a possible victim of DDIs as it is primarily metabolized by CYP3A4 [18]. St John’s wort may therefore cause a decrease in the plasma concentration of simeprevir as it is a CYP3A4 inducer. Nevertheless, this change might not be clinically relevance since simeprevir exhibits high inter-individual variability in its plasma concentrations [25].
5.2 NS5A Inhibitor
5.2.1 Daclatasvir
Daclatasvir has a negligible influence on the activities of CYP3A4 and other CYP enzymes and no dose adjustments were required when it was studied with midazolam [23]. Based on this information, it is expected that most benzodiazepines, antidepressants, and antipsychotics can be used safely in combination with daclatasvir, as shown in Table 6. Daclatasvir is metabolized by CYP3A4 and thus inducers and inhibitors of CYP3A4 have the ability to affect the plasma concentrations of daclatasvir [23]. Most psychoactive drugs do not influence CYP3A4, with the exception of St John’s wort; therefore, co-administration of St John’s wort and daclatasvir is contraindicated [23].
5.3 NS5B Polymerase Inhibitor
5.3.1 Sofosbuvir
Sofosbuvir is an NS5B inhibitor and not a perpetrator of DDIs as it has no influence on CYP enzymes or drug transporters; therefore, it has no impact on the plasma concentrations of psychoactive drugs [26]. However, an unexpected interaction has occurred involving sofosbuvir and the antiarrhythmic agent amiodarone. This indicates that not every DDI can be predicted based on the activities of CYP, UGT, or drug transporters. The mechanism and the specific role of sofosbuvir in the interaction was uncertain because other DAAs (daclatasvir, simeprevir, and ledipasvir) were simultaneously administered and could have been involved in causing the interaction [27, 28]. Additionally, it could also be caused by a pharmacodynamic interaction.
Sofosbuvir is metabolized in the liver and intestine; the drug is not a victim of enzymatic DDIs because it is not metabolized by, for example, CYPs or UGTs [26]. Sofosbuvir is a substrate for P-gp and BCRP; hence, interactions may occur with inducers and inhibitors of P-gp. P-gp inducers, e.g., St John’s wort, could potentially decrease plasma concentrations of sofosbuvir and result in a decrease in the pharmacological effects of sofosbuvir. Therefore, co-administration of the two drugs is contraindicated. Trazodone is also a possible P-gp inducer and may affect the plasma concentration of sofosbuvir (Table 8). Inhibition of P-gp could increase the plasma concentration of sofosbuvir; however, the interaction studies have not been performed in humans [26]. Lastly, the main (inactive) metabolite of sofosbuvir (GS-331007) is not a P-gp substrate [26].
5.4 Fixed-Dose Combinations
5.4.1 Ledipasvir and Sofosbuvir
Ledipasvir inhibits P-gp and BCRP and may cause interactions with P-gp and BCRP substrates (e.g., risperidone, and nortriptyline) [29]. P-gp inhibition at the BBB could potentially increase the exposure of these P-gp substrates in the brain. No interaction studies have been performed between ledipasvir and psychoactive agents. Table 7 shows the psychoactive agents that can be safely used with or potentially interact with ledipasvir.
The metabolism of ledipasvir is unknown but it is mainly excreted unchanged through bile. Thus, ledipasvir is not expected to be a victim of DDIs [29].
Sofosbuvir is discussed in Sect. 5.3.1.
5.4.2 Paritaprevir/Ritonavir, Ombitasvir, and Dasabuvir
Ritonavir is a strong CYP3A4 inhibitor but it also influences other CYP enzymes and drug transporters. Consequently, caution is needed if combining drugs metabolized by CYP3A4 with this fixed-dose regimen (paritaprevir/ritonavir, ombitasvir, and dasabuvir). Psychoactive agents such as duloxetine, escitalopram, zolpidem, alprazolam, and diazepam can be safely administered with this regimen as previous studies have not shown any clinically relevant interactions (Table 9) [20, 30–32].
The plasma concentrations of duloxetine did not alter when it was co-administered with the combination regimen [20]. Duloxetine is a substrate for CYP2D6 and CYP1A2, and ritonavir inhibits CYP2D6 and induces CYP1A2. As no effect was observed when combined with paritaprevir/ritonavir, ombitasvir, and dasabuvir, it was suggested that the inhibition of CYP2D6 and induction of CYP1A2 occurred to similar extents. We recommend that this combination regimen be used with care in patients receiving medications that are metabolized by CYP2D6 and/or CYP1A2, especially as a previous interaction study on the co-administration of olanzapine (CYP1A2 and CYP2D6 substrate) and ritonavir resulted in decreased olanzapine concentrations [33].
It is important to note that CYP2D6 inhibition by ritonavir is dose dependent [34]. Low-dose ritonavir (100 mg twice daily) had only a mild effect on CYP2D6, as shown with the CYP2D6 substrate desipramine (26 % AUC increase), but the therapeutic dose of ritonavir (600 mg twice daily) had a stronger effect (desipramine AUC increase of 145 %) [34–36]. However, this fixed-dose HCV regimen contains only 100 mg of ritonavir. Therefore, we expect DDIs only with co-administered drugs that are primarily metabolized by CYP2D6 and that have a narrow therapeutic range. Such drugs are not contraindicated with this combination regimen; however, plasma drug concentrations and adverse events should be monitored after co-administration [34].
Ritonavir also inhibits P-gp; therefore, ritonavir may modify plasma concentrations of P-gp substrates such as risperidone and amitriptyline.
Paritaprevir, ombitasvir, and dasabuvir are inhibitors of UGT and thus benzodiazepines (e.g., lorazepam, lormetazepam, and oxazepam) conjugated by UGT could be victims of interactions (Table 6) [20].
5.4.3 Grazoprevir and Elbasvir
Table 10 shows safe options for psychoactive drugs that can be administered with grazoprevir and elbasvir. Grazoprevir is a mild CYP3A inhibitor as it was observed to increase the plasma concentration of midazolam by only 30 % [19]. Therefore, CYP3A4 substrates are not contraindicated for co-administration with grazoprevir. However, we recommend that prescribers be aware of possible interactions with drugs that are primarily metabolized by CYP3A4 and have a narrow therapeutic range. There are no reported studies on drug interactions between the grazoprevir/elbasvir combination and psychoactive agents [19]. Grazoprevir and elbasvir are mainly metabolized by CYP3A4; thus, they should not be administered with St John’s wort and other CYP3A4 inducers or inhibitors [19] (Table 10).
6 Conclusion
In this review we have shown that there is a paucity of experimental data on drug interactions between psychoactive agents and DAAs. Many mechanisms are involved in the metabolism and transport of both classes of drugs, making it difficult to predict which drugs can be safely co-administered to patients.
In our opinion, safe options for concomitant administration should be combinations that have actually been studied in humans, or combinations that are not based on theoretical pharmacokinetic interactions. In addition, all medications used at the start of and during HCV treatment should be inventoried, so that possible DDIs can be evaluated before clinically relevant effects arise. Physicians should also be aware of possible interactions and their consequences. These may include adverse effects caused by increased plasma drug concentrations or reduced efficacy due to decreases in drug exposure. These are of great importance as such issues may also affect adherence to both DAAs and psychoactive agents. Our final recommendation is that physicians contact pharmacists or clinical pharmacologists for support in managing these interactions.
This review provides an overview of the mechanisms of interactions between DAAs and psychoactive agents. Based on interaction studies, we give recommendations for the co-administration of DAAs and psychoactive agents. The administration of various combinations of drugs results in different potential interactions. It is therefore necessary that theoretical predictions of DDIs be backed with actual drug interaction studies, in order to obtain more conclusive and useful data for clinical applications.
References
Udina M, Castellvi P, Moreno-Espana J, Navines R, Valdes M, Forns X, et al. Interferon-induced depression in chronic hepatitis C: a systematic review and meta-analysis. J Clin Psychiatry. 2012;73(8):1128–38. doi:10.4088/JCP.12r07694.
Schaefer M, Capuron L, Friebe A, Diez-Quevedo C, Robaeys G, Neri S, et al. Hepatitis C infection, antiviral treatment and mental health: a European expert consensus statement. J Hepatol. 2012;57(6):1379–90. doi:10.1016/j.jhep.2012.07.037.
El–Serag HB, Kunik M, Richardson P, Rabeneck L. Psychiatric disorders among veterans with hepatitis C infection. Gastroenterology. 2002;123(2):476–82. doi:10.1053/gast.2002.34750.
Stewart B, Mikocka-Walus A, Morgan J, Colman A, Phelps M, Harley H, et al. Anxiety and depression in Australian chronic hepatitis C outpatients: prevalence and predictors. Australas Psychiatry. 2012;20(6):496–500. doi:10.1177/1039856212460597.
Buckingham E, Schrage E, Cournos F. Why the treatment of mental disorders is an important component of HIV prevention among people who inject drugs. Adv Prev Med. 2013;2013:690386. doi:10.1155/2013/690386.
Patel N, Nasiri M, Koroglu A, Bliss S, Davis M, McNutt LA, et al. A cross-sectional study comparing the frequency of drug interactions after adding simeprevir- or sofosbuvir-containing therapy to medication profiles of hepatitis C monoinfected patients. Infect Dis Ther. 2015;4(1):67–78.
Radboud university medical center. Data on file. 2015
Burger D, Back D, Buggisch P, Buti M, Craxi A, Foster G, et al. Clinical management of drug-drug interactions in HCV therapy: challenges and solutions. J Hepatol. 2013;58(4):792–800. doi:10.1016/j.jhep.2012.10.027.
Back D, Else L. The importance of drug-drug interactions in the DAA era. Digest Liver Dis. 2013;45(S5):S343–8.
Hiemke C, Baumann P, Bergemann N, Conca A, Dietmaier O, Egberts K, et al. AGNP consensus guidelines for therapeutic drug monitoring in psychiatry: update 2011. Pharmacopsychiatry. 2011;44(6):195–235. doi:10.1055/s-0031-1286287.
European Association for Study of the Liver. EASL recommendations on treatment of hepatitis C 2015. 2015. http://www.easl.eu/research/our-contributions/clinical-practice-guidelines/detail/recommendations-on-treatment-of-hepatitis-c-2015/report/1. Accessed 8 June 2015.
American Association for the Study of Liver Diseases. Recommendations for testing, managing, and treating hepatitis C. 2015. http://www.hcvguidelines.org. Accessed 15 Feb 2016.
Kiser JJ, Burton JR, Everson GT. Drug-drug interactions during antiviral therapy for chronic hepatitis C. Nat Rev Gastroenterol Hepatol. 2013;10(10):596–606.
FDA. Drug development and drug interactions: table of substrates, inhibitors and inducers. 2014. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/DrugInteractionsLabeling/ucm093664.htm#classSub. Accessed 30 Mar 2016.
Lexicomp. Lexi-Interact Data Fields. Wolters Kluwer. http://webstore.lexi.com/Information/Product-Information/Lexi-Interact-Fields. Accessed 30 Mar 2016.
Greenblatt DJ, Peters DE, Oleson LE, Harmatz JS, MacNab MW, Berkowitz N, et al. Inhibition of oral midazolam clearance by boosting doses of ritonavir, and by 4,4-dimethyl-benziso-(2H)-selenazine (ALT-2074), an experimental catalytic mimic of glutathione oxidase. Br J Clin Pharmacol. 2009;68(6):920–7. doi:10.1111/j.1365-2125.2009.03545.x.
EMA. Victrelis summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002332/WC500109786.pdf. Accessed 29 Sept 2015.
EMA. Olysio summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002777/WC500167867.pdf. Accessed 29 Sept 2015.
FDA. Zepatier prescribing information. 2016. http://www.merck.com/product/usa/pi_circulars/z/zepatier/zepatier_pi.pdf. Accessed 15 Feb 2016.
EMA. Viekirax summary of product characteristics. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003839/WC500183997.pdf. Accessed 29 Sept 2015.
Jackson A, D’Avolio A, Moyle G, Bonora S, Di Perri G, Else L, et al. Pharmacokinetics of the co-administration of boceprevir and St John’s wort to male and female healthy volunteers. J Antimicrob Chemother. 2014;69(7):1911–5. doi:10.1093/jac/dku060.
Nigam SK. What do drug transporters really do? Nat Rev Drug Discov. 2015;14(1):29–44. doi:10.1038/nrd4461.
EMA. Daklinza summary of product characteristics. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003768/WC500172848.pdf. Accessed 29 Sept 2015.
Bramness JG, Skurtveit S, Mørland J. Clinical impairment of benzodiazepines—relation between benzodiazepine concentrations and impairment in apprehended drivers. Drug Alcohol Depend. 2002;68(2):131–41
FDA. Briefing document: simeprevir (TMC435). 2013. http://www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/drugs/antiviraldrugsadvisorycommittee/ucm371624.pdf. Accessed 15 Feb 2016.
EMA. Sovaldi summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002798/WC500160597.pdf. Accessed 29 Sept 2015.
FDA. Drug safety communication: FDA warns of serious slowing of the heart rate when antiarrhythmic drug amiodarone is used with hepatitis C treatments containing sofosbuvir (Harvoni) or Sovaldi in combination with another direct acting antiviral drug. 2015 Mar 24. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM439492.pdf. Accessed 23 Oct 2015.
Back DJ, Burger DM. Interaction between amiodarone and sofosbuvir-based treatment for hepatitis C virus infection: potential mechanisms and lessons to be learned. Gastroenterology. 2015;149(6):1315–7. doi:10.1053/j.gastro.2015.09.031.
EMA. Harvoni summary of product characteristics. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003850/WC500177995.pdf. Accessed Sept 29 2015.
Badri PS, Dutta S, Wang H, Podsadecki TJ, Polepally AR, Coakley EP, et al. Drug interactions with direct acting antiviral combination of paritaprevir/ritonavir + ombitasvir [abstract #55]. In: 16th International workshop on clinical pharmacology of HIV and hepatitis therapy; 26–28 May 2015; Washington, DC.
Menon RM, Badri PS, Wang T, Polepally AR, Zha J, Khatri A, et al. Drug-drug interaction profile of the all-oral anti-hepatitis C virus regimen of paritaprevir/ritonavir, ombitasvir, and dasabuvir. J Hepatol. 2015;63(1):20–9. doi:10.1016/j.jhep.2015.01.026.
Polepally AR, King JR, Shuster DL, Dumas EO, Khatri J, Wu J, et al. Drug-drug interactions of commonly used medications with direct acting antiviral HCV combination therapy of paritaprevir/r, ombitasvir and dasabuvir [abstract #16]. In: 16th International workshop on clinical pharmacology of HIV and hepatitis therapy; 26–28 May 2015; Washington, DC.
Jacobs BS, Colbers AP, Velthoven-Graafland K, Schouwenberg BJ, Burger DM. Effect of fosamprenavir/ritonavir on the pharmacokinetics of single-dose olanzapine in healthy volunteers. Int J Antimicrob Agents. 2014;44(2):173–7. doi:10.1016/j.ijantimicag.2014.03.014.
Aarnoutse RE, Kleinnijenhuis J, Koopmans PP, Touw DJ, Wieling J, Hekster YA, et al. Effect of low-dose ritonavir (100 mg twice daily) on the activity of cytochrome P450 2D6 in healthy volunteers. Clin Pharmacol Ther. 2005;78(6):664–74. doi:10.1016/j.clpt.2005.09.001.
Bertz RJ, Cao G, Cavanaugh JH, Hsu A, Granneman GR, Leonard JM. Effect of ritonavir on the phamacokinetics of desipramine [abstract no. MoB1201]. AIDS Conference; 7-12 July 1996; Vancouver.
Hsu A, Granneman GR, Bertz RJ. Ritonavir: clinical pharmacokinetics and interactions with other anti-HIV agents. Clin Pharmacokinet. 1998;35(4):275–91. doi:10.2165/00003088-199835040-00002.
EMA. Exviera summary of product characteristics. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003837/WC500182233.pdf. Accessed 29 Sept 2015.
FDA. Xanax® prescribing information. 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018276s045lbl.pdf. Accessed 11 Feb 2016.
FDA. Limbitrol® prescribing information. 2007. http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/016949s038lbl.pdf. Accessed 1 July 2015.
FDA. Onfi® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/202067s003,203993s003lbl.pdf. Accessed 1 July 2015.
FDA. Tranxene T-Tab® tablets prescribing information. 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/017105s076lbl.pdf. Accessed 11 Feb 2016.
FDA. Valium® prescribing information. 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/013263s092lbl.pdf. Accessed 1 July 2015.
FDA. Dalmane® prescribing information. 2007. http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/016721s076lbl.pdf. Accessed 23 Apr 2016.
EMA. Buccolam summary of product characteristics. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002267/WC500112310.pdf. Accessed 1 July 2015.
FDA. Restoril™ prescribing information. 2010. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/018163s054lbl.pdf. Accessed 11 Feb 2016.
FDA. Ambien® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/019908s035,021774s016lbl.pdf. Accessed 1 July 2015.
FDA. Celexa® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020822Orig1s046lbl.pdf. Accessed 1 July 2015.
EMA. Cymbalta summary of product characteristics. 2009. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000572/WC500036781.pdf. Accessed 1 July 2015.
FDA. Lexapro® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021323s044,021365s032lbl.pdf. Accessed 1 July 2015.
FDA. Prozac prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/018936s105,021235s024lbl.pdf. Accessed 1 July 2015.
FDA. Fluvoxamine maleate prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021519Orig1s008lbl.pdf. Accessed 1 July 2015.
FDA. Paxil® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020031s071,020710s035lbl.pdf. Accessed 1 July 2015.
FDA. Zoloft® prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/019839s084,020990s043lbl.pdf. Accessed 1 July 2015.
FDA. Effexor® prescribing information. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020151s031s055s058s060lbl.pdf. Accessed 1 July 2015.
EMA. Brintellix summary of product characteristics. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002717/WC500159449.pdf. Accessed 1 July 2015.
FDA. Anafranil™ prescribing information. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/019906s039lbl.pdf. Accessed 1 July 2015.
EMA. Abilify summary of product characteristics. 2009. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000471/WC500020170.pdf. Accessed 1 July 2015.
EMA. Latuda summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002713/WC500164683.pdf. Accessed 1 July 2015.
EMA. Zyprexa summary of product characteristics. 2006. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000115/WC500055207.pdf. Accessed 1 July 2015.
EMA. Invega summary of product characteristics. 2012. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000746/WC500034925.pdf. Accessed 1 July 2015.
Hulskotte EGJ, Gupta S, Xuan F, van Zutven MGJA, O’Mara E, Galitz L, et al. Coadministration of the HCV protease inhibitor boceprevir has no clinically meaningful effect on the pharmacokinetics of the selective serotonin reuptake inhibitor escitalopram in healthy volunteers [abstract]. HEP DART; 4–8 Dec 2011; Hawaii.
Kasserra C, Hughes E, Treitel M, Gupta S, O’Mara E. Clinical pharmacology of boceprevir (BOC): metabolism, excretion, and drug-drug interactions [abstract #18]. Conference on Retroviruses and Opportunistic Infections; 27 Feb–2 Mar 2011; Boston.
Beumont M. The pharmacokinetic interaction between the investigational HCV NS3/4A protease inhibitor TMC435 and escitalopram [abstract]. Annual Meeting of the American Association for the Study of Liver Diseases; 4 Nov 2011; San Fransisco.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was used in the preparation of this review.
Conflict of interest
E.J. Smolders and C.T.M.M. de Kanter declare that they have no conflicts of interest that are directly relevant to the content of this review. R.J. de Knegt received sponsorship/research grants from BMS and Janssen; is a consultant for AbbVie, BMS, Gilead, Roche, and Janssen; and has delivered lectures for AbbVie, Janssen, Gilead, and Roche. J.P.H. Drenth is on the advisory boards for AbbVie, BMS, Gilead, Janssen, and Merck and received sponsorship/research grants from AbbVie and Janssen. D.M. Burger is on the advisory boards for AbbVie, BMS, Gilead, Janssen, and Merck and received sponsorship/research grants from BMS, Janssen, Merck, and Viiv. However, these conflicts of interests did not influence the preparation of this review.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Smolders, E.J., de Kanter, C.T.M.M., de Knegt, R.J. et al. Drug–Drug Interactions Between Direct-Acting Antivirals and Psychoactive Medications. Clin Pharmacokinet 55, 1471–1494 (2016). https://doi.org/10.1007/s40262-016-0407-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-016-0407-2