Abstract
Background
Schizophrenia is one of the leading causes of disability. Paliperidone palmitate once-monthly injection (PP1M) was developed to provide consistent drug delivery and improve medication adherence for maintenance treatment. It is well known that patients with schizophrenia have higher cardiovascular risks, however little is known about the cardiovascular risks of patients with schizophrenia treated with PP1M in Asia.
Objective
This study aimed to estimate the incidence of cardiovascular events after initiating PP1M treatment and evaluate the cardiovascular risk associations compared with oral second-generation antipsychotics (SGAs).
Methods
Data from Taiwan’s National Health Insurance Research Database were used to identify a cohort of adult patients with schizophrenia who received any SGAs from 1 March 2012 to 31 December 2018. Patients who initiated PP1M treatment were enrolled for descriptive analysis of incidence rates. PP1M patients were propensity matched 1:1 to patients initiating a new oral SGA, for comparative analysis based on demographics, clinical characteristics and treatment history at baseline, in three-step matching procedures, following the prevalent new-user design to enhance comparability. Follow-up ended at the end of the treatment episode of index drug, death, last record available, or end of the study (31 December 2019). Study endpoints included serious cardiovascular events (including severe ventricular arrhythmia and sudden death), expanded serious cardiovascular events (which further included acute myocardial infarction and ischemic stroke), and cardiovascular hospitalizations. Risks of study endpoints between matched cohorts were compared using Cox regression.
Results
Overall, 11,023 patients initiating PP1M treatment were identified (49.5% were females; mean age of 43.2 [12.2] years). Overall incidences for serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations were 3.92, 7.88 and 51.96 per 1000 person-years, respectively. In matched cohort analysis (N = 10,115), the hazard ratios (HRs) between initiating PP1M and a new oral SGA for serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations were 0.86 (95% confidence interval [CI] 0.55–1.36), 0.88 (95% CI 0.63–1.21), and 0.78 (95% CI 0.69–0.89), respectively.
Conclusion
This study reported the population-based incidence of cardiovascular events in schizophrenic patients initiating PP1M treatment. PP1M was not associated with increased risks of serious cardiovascular events but was potentially associated with lower risks of cardiovascular hospitalizations compared with oral SGAs.
Similar content being viewed by others
This study presents the first report on population-based incidence rates of cardiovascular events among patients with schizophrenia initiating paliperidone palmitate once-monthly injection (PP1M) treatment. The overall incidence rates for serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations were 3.92, 7.88, and 51.96 per 1000 person-years, respectively. |
Initiating PP1M treatment was not associated with increased risks of serious cardiovascular events but was associated with 22% decreased risks of cardiovascular hospitalizations compared with initiating a new oral second-generation antipsychotic. |
The results from this study contribute to the growing real-world evidence of safety for long-acting injectable antipsychotics at the population level, and provide additional insights into the cardiovascular risk profile of PP1M. |
1 Introduction
Schizophrenia is one of the top 15 leading causes of disability worldwide [1] and affects an estimated 0.28% of the global population and 0.42% of the population in Asia [2]. It is a chronic disorder necessitating long-term pharmacological treatment with antipsychotics [3]. It is well known that patients with schizophrenia have higher risks of cardiovascular events [4, 5], yet the underlying mechanisms have not been fully understood until now. Potential causal factors include poor diet and lifestyles, substance abuse, cardiometabolic dysfunctions, and metabolic- and cardiac-related adverse effects of antipsychotics [6, 7]. Previous studies have revealed that the use of antipsychotics may be linked to severe ventricular arrhythmia (SVA) through prolongation of the corrected QT interval and torsade de pointes [8, 9], as well as ischemic cardiovascular events such as acute myocardial infarction (AMI) and ischemic stroke (IS), potentially resulting from weight gain, metabolic dysregulation, or cardiac arrhythmia [10,11,12]. Antipsychotic use has been associated with an increased risk of death, including sudden cardiac death [13, 14]. It is important to note that while current evidence remains inconclusive, previous studies suggest the associations may vary across different types of antipsychotics and may potentially be drug-specific [9, 11]. Considering the potential impacts of antipsychotics on the cardiovascular system, it is recommended to implement cardiovascular risk management strategies such as electrocardiogram (ECG) monitoring, particularly when initiating antipsychotic treatment [15] for individuals with established cardiovascular risk factors or those who are at an increased risk of cardiovascular events [16]. As the cardiovascular risks may be different across antipsychotics, it is essential to establish the cardiovascular risk profiles for more precise risk evaluation and management in clinical practice.
In recent decades, there has been a notable worldwide shift in the treatment of schizophrenia from first-generation antipsychotics (FGAs) to second-generation antipsychotics (SGAs) [17, 18], mainly due to a more favorable safety profile of SGAs [19]. Alongside orally administered antipsychotics, long-acting injectable (LAI) antipsychotics have been developed to improve medication adherence for long-term maintenance treatment and minimize the risk of relapse compared with existing oral counterparts [20, 21]. Meanwhile, there is an upward trend in the use of LAI antipsychotics (including LAI SGAs) globally and in Asia [22, 23]. Moreover, the use of LAI SGAs has been recommended for patients experiencing a first episode, in several clinical practice guidelines globally in the recent 10-year period [24]. Specifically for Taiwan, the consensus statements by the Taiwan Society of Biological Psychiatry and Neuropsychopharmacology (TSBPN) suggests that LAI antipsychotics can be a treatment option for all patients with schizophrenia, including first-episode patients [25]. Paliperidone palmitate once-monthly injection (PP1M), which is a commonly used LAI SGA in clinical practice [26], has been associated with significant improvements in symptoms of schizophrenia, enhanced persistence and adherence to treatment [27], and reduction of hospitalizations and relapse [28,29,30]. Despite the established safety and tolerability profile of PP1M treatment in patients with schizophrenia in controlled clinical trial settings [28,29,30,31,32], its increased use in clinical practice highlights the need for further population-level evidence regarding any potential association with serious cardiovascular events (SVA and sudden death, AMI and IS) or more general cardiovascular risks. This is particularly crucial for the Asian population for whom such evidence is currently greatly limited. Obtaining such evidence will contribute to a better understanding of the appropriate use of PP1M in clinical practice.
In the present study, we aimed to evaluate the risk associations between the use of PP1M and cardiovascular events: (1) estimate the incidence rates of cardiovascular events among adult patients with schizophrenia or schizoaffective disorder who initiated PP1M treatment in Taiwan, and (2) assess the risk associations of cardiovascular events between the use of PP1M versus oral SGAs.
2 Methods
2.1 Data Sources
Taiwan’s National Health Insurance Research Database (NHIRD) is a population-based claims database and covers more than 99% of the population in Taiwan [33]. The database offers comprehensive clinical information, including demographics, dispensed prescription drugs, and medical services provided, with diagnoses coded in International Classification of Diseases (ICD), Ninth Revision, Clinical Modification (ICD-9-CM) until 2016, and by the ICD 10th Revision (ICD-10) thereafter. Death information was obtained through linkage to the National Death Registry with a unique and anonymous identifier at patient level.
2.2 Study Design and Population
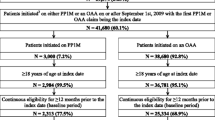
This was a retrospective, longitudinal cohort study among adult patients with a confirmed diagnosis of schizophrenia (ICD-9: 295.x, except 295.7; ICD-10: F20.x) or schizoaffective disorder (ICD-9: 295.7; ICD-10: F25.x), of any sex (non-missing), who were treated with at least one SGA in the NHIRD from 1 March 2012 to 31 December 2018 in Taiwan (see Online Resource Fig. S1). Patients who received at least one prescription of PP1M were identified as the primary study group. The cohort entry was defined as the date of PP1M initiation, and baseline period was defined as 2 years prior to the date of cohort entry. The study’s follow-up ended at the end of the treatment episode of PP1M, death, last record available, or end of the study period (31 December 2019), whichever came first. In the primary study group, treatment episode was defined as a period of continuous treatment that ended when a prescription gap of ≥ 60 days (grace period, follow-up ended at the start of the gap period) was observed for PP1M. The group of all PP1M ever users was used to estimate the incidence rates of cardiovascular events for descriptive analysis.
For comparative analysis, to facilitate a comparative assessment of the risk associations of cardiovascular events between PP1M and oral SGAs, we utilized a prevalent new-user design [34, 35] to identify a comparator group (initiating a new oral SGA). This design allowed for the identification and matching of the patients who initiated a new oral SGA and shared a similar treatment history of antipsychotics, clinical and demographic characteristics at baseline, and index date with PP1M users in the primary study group. The cohort entry for oral SGA comparators was defined as the date of initiation of the new oral SGA to establish meaningful comparisons between the two treatment groups while appropriately accounting for prior treatment exposures and baseline characteristics (Fig. 1). Following a three-step procedure [34, 35], each patient initiating PP1M treatment was first matched with other patients who initiated a new oral SGA based on calendar time of cohort entry (± 180 days), treatment duration of the most recent treatment episode of an SGA before cohort entry (± 90 days), visit type at cohort entry (inpatient or outpatient), and history of cardiovascular hospitalizations at baseline. Next, conditional logistic regression was performed to obtain the propensity score (PS) of initiating treatment of PP1M or a new oral SGA, stratified by stratums consisting of each patient initiating PP1M treatment and their respective set of potential oral comparators, based on selected baseline characteristics, including age at cohort entry, Charlson Comorbidity Index (CCI) [36, 37] score, psychiatric comorbidity and hospitalization, number of cardiovascular hospitalizations, cumulative exposures to SGAs or FGAs, and other important co-medications (Online Resource Table S3). Finally, each patient who initiated PP1M treatment was 1:1 matched with an oral SGA comparator within their respective set of potential oral comparators, using nearest-neighbor matching with a caliper of 0.2 standard deviation (SD) of logit PS [38] without replacement. Matching performance was assessed using standardized mean differences (SMDs) [39] between the primary study group and the oral comparator group. The follow-up ended at the end of the treatment episode of index oral SGAs (defined as a treatment gap of ≥ 45 days without any prescriptions of index oral SGAs, sensitivity analysis was conducted using an alternative definition of ‘grace period’ of 30 days for both groups), and otherwise similar to the primary study group.
Study design. a Overall study design indicating primary study group and oral comparator group, and matched key characteristics between groups. b Time windows for assessment of exposures, outcomes, and covariates. PP1M paliperidone palmitate once-monthly injection, SGA second-generation antipsychotic
2.3 Study Endpoints
Serious cardiovascular events potentially leading to death and overall cardiovascular risks were the primary focus for the current study. Previous studies suggested that paliperidone causes a modest increase in corrected QT interval, which is a risk factor to SVA and sudden death. The first study endpoint of serious cardiovascular events was the composite outcome of the following: SVA, including paroxysmal ventricular tachycardia, ventricular fibrillation, ventricular flutter, or cardiac arrest; and sudden death, which was defined as records filed with codes for instantaneous death, death occurring in < 24 h from onset of symptoms, or death attributed to SVA following validated definitions in previous studies [40,41,42]. Furthermore, to assess the effects of PP1M on more expanded definitions of serious cardiovascular events in accordance with major adverse cardiovascular events, an endpoint of expanded serious cardiovascular events to include AMI and IS in addition to the first study endpoint was used. Finally, to assess the more general cardiovascular risks of the study drug in addition to serious cardiovascular events, the endpoint of cardiovascular hospitalizations was used. We identified patients with the above‐mentioned outcomes during the study period through the medical records from emergency department visits or hospitalization claims data in the NHIRD and the death records from the National Death Registry. A complete list of ICD codes is listed in Online Resource Table S2.
The overall incidence rate of serious cardiovascular events and cardiovascular hospitalizations during follow-up was estimated as the number of serious cardiovascular events or cardiovascular hospitalizations divided by the total number of person-years of the follow-up.
2.4 Statistical Analysis
To assess risk associations of serious cardiovascular events and cardiovascular hospitalizations between PP1M and oral SGAs, a Cox regression [43] model was used. Risk associations are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). Both unadjusted HRs and adjusted HRs after matching were generated, with double-adjustment of baseline characteristics including age, baseline CCI score, psychiatric comorbidity and hospitalization, number of cardiovascular hospitalizations, and co-medications, as previous studies suggested additional benefit of double-adjustment considering residual imbalance of covariates after PS matching [44].
In the secondary analysis to investigate the risks of cardiovascular events of interest for paliperidone palmitate LAIs, follow-up was extended in the primary study group to the end of the paliperidone palmitate every 3-month injection (PP3M) treatment episode for patients who switched to PP3M from PP1M (180 days as the grace period), and the follow-up in the oral comparator group was extended to the end of the treatment episode of any oral SGAs accordingly.
In sensitivity analysis, the potential effects of ‘grace period’ on the length of follow-up were explored by repeating the primary analysis using an alternative definition of ‘grace period’ of 30 days for both PP1M users and the oral SGA comparators.
P values < 0.05 were considered statistically significant. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
3 Results
We identified 11,023 patients (5567 [50.5%] were men and 5456 [49.5%] were women, with a mean [SD] age of 43.2 [12.2] years) who initiated use of PP1M between 2012 and 2018 (see Online Resource Fig. S1).
The baseline characteristics of the primary study group before matching are shown in Table 1. More than 37% of patients had a prior psychiatric comorbidity and nearly 60% of patients had any psychiatric hospitalization at baseline. Overall, the mean duration of follow-up in the study population was 1.04 (SD 1.22) years. During follow-up, any serious cardiovascular events (SVA/sudden death) occurred in 45 of PP1M ever users, with an overall incidence rate of 3.92 (95% CI 2.86–5.25) per 1000 person-years. Any expanded serious cardiovascular events (SVA/sudden death/AMI/IS) occurred in 90 PP1M ever users, with an overall incidence rate of 7.88 (95% CI 6.33–9.68) per 1000 person-years. Lastly, cardiovascular hospitalizations occurred in 571 PP1M users, with an overall incidence rate of 51.96 (95% CI 47.78–56.40) per 1000 person-years.
For assessment of the risk associations of cardiovascular events between initiating treatment of PP1M and a new oral SGA, the study cohort finally included 10,115 (92%) patients initiating PP1M use, who were matched 1:1 to 10,115 patients initiating use of a new oral SGA. Patients initiating PP1M use had a similar baseline profile to those initiating a new oral SGA, with SMDs of all baseline covariates < 0.1 (Table 1). Overall, the mean duration of follow-up in the primary study group was 1.05 (SD 1.24) years, and the mean duration of follow-up in the oral comparator group was 0.74 (SD 1.10) years. During follow-up, serious cardiovascular events (SVA/sudden death) occurred in 40 patients in the primary study group and 35 patients in the oral comparator group, with an overall incidence rate of 3.76 (95% CI 2.68–5.12) per 1000 person-years in the primary study group versus 4.70 (95% CI 3.28–6.54) per 1000 person-years in the matched oral comparator group. Expanded serious cardiovascular events (SVA/sudden death/AMI/IS) occurred in 81 patients in the primary study group and 69 patients in the oral comparator group, with an overall incidence rate of 7.64 (95% CI 6.07–9.49) per 1000 person-years in the primary study group versus 9.31 (95% CI 7.24–11.78) per 1000 person-years in the matched oral comparator group. Cardiovascular hospitalizations occurred in 488 patients in the primary study group and 483 patients in the oral comparator group, with an overall incidence rate of 47.73 (95% CI 43.59–52.16) per 1000 person-years in the primary study group versus 68.43 (95% CI 62.46–74.81) per 1000 person years in the matched oral comparator group. There were non-significant reduced risks of serious cardiovascular events (HR 0.86, 95% CI 0.55–1.36) or expanded serious cardiovascular events (HR 0.88, 95% CI 0.63–1.21), and 22% decreased risk of cardiovascular hospitalizations (HR 0.78, 95% CI 0.69–0.89; p = 0.0002) associated with initiating PP1M use compared with initiating a new oral SGA use (Table 2).
In secondary analysis, the observations were extended in the primary study group to the end of the PP3M treatment episode for those who switched to PP3M from PP1M. For the matched cohort, the overall incidence rates of serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations were 3.89 (95% CI 2.85–5.18), 7.89 (95% CI 6.37–9.66) and 45.42 (95% CI 41.58–49.51) per 1000 person-years, respectively, for the primary study group, versus 4.72 (95% CI 3.76–5.84), 8.58 (95% CI 7.27–10.05), and 57.47 (95% CI 53.86–61.26) per 1000 person-years, respectively, for the matched oral comparator group. The HRs between the primary study and oral comparator groups for serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations were 0.84 (95% CI 0.59–1.22), 0.90 (95% CI 0.69–1.17), and 0.78 (95% CI 0.70–0.87), respectively, which were at similar levels as the primary analysis (Table 3). Furthermore, consistent results of comparative risks of cardiovascular events of interest as primary analysis were observed in sensitivity analysis when an alternative definition of ‘grace period’ was applied (Table 4).
4 Discussion
This study estimated the incidence of cardiovascular events after initiating PP1M treatment, and further evaluated the comparative cardiovascular risk associations. Compared with oral SGAs, we found that use of PP1M was not associated with increased risk of serious cardiovascular events but was potentially associated with lower risk of cardiovascular hospitalizations. To our knowledge, this is the first study to report population-based incidence rates of serious cardiovascular events and cardiovascular hospitalizations among patients with schizophrenia treated with PP1M, and to evaluate the associations between use of PP1M and risk of cardiovascular events in clinical practice among Asian populations.
The incidence rate of serious cardiovascular events, including SVA and sudden death, after initiating treatment of PP1M was 3.92 per 1000 person-years. The majority of previous studies investigating the cardiovascular effects of antipsychotics exposure have primarily focused on outcomes such as sudden cardiac death, myocardial infarction, or stroke in the past decades [12, 45]. Only a few studies reported the incidence rates of serious cardiovascular events, including SVAs as defined in this study. Assessing the effects of antipsychotics on life-threatening arrhythmias such as SVAs is crucial for a comprehensive understanding of the cardiovascular impact of these medications. In a cohort study using three US Medicaid administrative datasets, the incidence rates of SVA and sudden death, as defined in the present study, were reported for patients treated with four commonly used oral antipsychotics (haloperidol, thioridazine, clozapine, and risperidone), and the incidence rates ranged from 2.2 to 5.0 per 1000 person-years [46]. Another retrospective cohort study using Medicaid data from five states reported an overall incidence rate of sudden death/SVA of 3.4 per 1000 person-years for incident antipsychotic users [47]. The incidence rates of serious cardiovascular events for oral antipsychotics documented in those two previous studies in the US were similar to the findings for PP1M in the present study, in which the incidence rates of serious cardiovascular events of an injectable antipsychotic were estimated for the first time and the limited evidence was further supplemented for Asian populations.
We further found that in the present study, PP1M treatment was not associated with a higher risk of serious and life-threatening cardiovascular events (HR 0.86) compared with oral SGAs. Few studies have previously examined the risk associations between LAI antipsychotic treatment and serious cardiovascular events, although meta-analyses and real-world studies suggested that use of LAIs was not associated with elevated risks of all-cause death, sudden death or cardiovascular death, or was associated with lower mortality compared with oral antipsychotics [42, 48, 49]. Furthermore, the null risk associations for expanded serious cardiovascular events (HR 0.88) reflected no elevated risks for a larger set of serious cardiovascular events associated with PP1M treatment, and such evidence can be used to enrich cardiovascular risk profiles for PP1M. Moreover, regarding more general cardiovascular risks of antipsychotics, the current study found that patients treated with PP1M were associated with lower risks of cardiovascular hospitalizations (HR 0.78). This finding is consistent with a recent study which reported that full treatment with LAIs was associated with a 12% decrease in hospitalizations for cardiovascular diseases (incidence rate ratio 0.88, 95% CI 0.81–0.96), compared with full treatment with oral antipsychotics [50]. In comparison with the present study, the use of a self-controlled design and inclusion of both FGAs and SGAs for oral and LAI formulations in the analysis may influence the point estimate of the HRs (0.78 vs. 0.88). On the basis of analyses for all three cardiovascular endpoints, PP1M showed comparable risks as oral SGAs or even more benefits. One possible explanation is that schizophrenia has been associated with increased cardiovascular risks, although the mechanisms remain unclear [4, 5]. If the relapse of schizophrenia symptoms directly contributes to elevated risks of cardiovascular events, improving treatment adherence and preventing relapse through the use of LAIs may decrease the incidence of cardiovascular diseases among patients with schizophrenia. To validate these findings, a meta-analysis of randomized controlled trials is needed, and potential underlying mechanisms should be examined in future studies if such associations are proved to be causal.
In a secondary analysis, the present study observed comparable or lower risks of cardiovascular events of interest when comparing the exposure to PP3M alongside PP1M with the exposure to any oral SGAs within a treatment episode. These findings suggest that there were no additional serious cardiovascular risks or potentially lower risks of more general cardiovascular risks associated with PP1M and PP3M use compared with oral SGAs, as measured by serious cardiovascular events, expanded serious cardiovascular events, and cardiovascular hospitalizations. However, it is important to note that these findings are exploratory in nature. Patients who further switched from PP1M to PP3M may show good tolerance to PP1M and the medication delivery change prior to clinical decisions of switching by clinicians, and those selected patients may naturally have lower risks of cardiovascular events after exposure to paliperidone LAIs. Future studies are needed to confirm and validate our findings. Additionally, as the definition of ‘grace period’ for study drug or oral comparators may influence duration of follow-up and estimates of incidence rate for outcomes, a sensitivity analysis with different definitions of ‘grace period’ was conducted to address potential inaccuracy in exposure assessment. The consistent results across these analyses indicated the robustness of our findings.
Most psychiatrists, especially in Asia, adopt a cautious approach when prescribing LAIs [51,52,53]. Concerns regarding potential adverse effects (including cardiovascular complications) expressed by both psychiatrists and patients contribute to this conservative attitude [54]. However, accumulating scientific evidence consistently demonstrates the overall benefits or comparable risks of LAIs compared with oral antipsychotics across various outcomes related to effectiveness, efficacy, safety, and quality of life [55]. Accordingly, the consensus statements by the TSBPN indicated that LAIs can be an available treatment for all patients with schizophrenia, including patients experiencing a first episode [25]. Specifically for PP1M, a review summarized its overall safety profile [56], including its potential cardiovascular adverse effects, however no quantitative incidence rates of cardiovascular events were documented, possibly due to the limited number of studies and/or small sample size of previous clinical trials. In the context of our current analysis, which supplements existing evidence by assessing population-based incidence rates and risk associations for cardiovascular events, if the advantages for LAIs in prompting medication adherence are taken into account, particularly for non-compliant individuals, the active consideration of PP1M to achieve better long-term outcomes should be encouraged in clinical practice.
This study has several strengths. One of the major strengths is the population-based analysis and the completeness and accuracy of data in terms of antipsychotic treatments, cardiovascular events of interest, and recognized important covariates. The ability to include nearly 100% of national health insurance-covered patients enables accurate estimate of population-based incidence rates. Second, the study design maximized the inclusion of PP1M users in real-world settings and enabled direct comparisons by identifying oral comparators in three-step matching procedures to ensure comparable demographic characteristics, recent and long-term exposure to antipsychotics, and disease conditions at baseline between groups. Using the calendar time for matching reduced the effects of time-related bias (e.g., immortal bias). Furthermore, comparing PP1M with oral SGAs used by patients with similar psychiatric clinical characteristics and treatment history at baseline could minimize confounding by indication. While alternative matching strategies could be explored in different settings, we believe our results are meaningful for general clinical practice and can be reasonably interpreted. Third, we minimized misclassification bias of outcomes in the present study, particularly for identification of sudden death. The validity of the ICD codes used was confirmed in prior studies, ensuring the accuracy of outcome definition.
This study also has several limitations. First, observational studies are at risk for residual confounding. Efforts have been made to minimize this potential bias by propensity matching procedures and further adjustments in the models. Moreover, a 2-year baseline was used to acquire more information of psychological, cardiovascular, comorbidities, and treatment history, which further assures the comparability of those key baseline characteristics. As measurement of some traditional cardiovascular risk factors, such as obesity and cigarette smoking, was not available in the NHIRD, it might be a source of residual confounding. Current clinical guidelines do not explicitly specify which SGA should be used based on existing cardiovascular risks [21]. Thus, the current levels of cardiovascular risk factors for patients may not be directly associated with assignment of PP1M or oral comparator groups in clinical practice, indicating the limited effects from these confounding variables. Second, we did not take into account the concomitant use of antipsychotics during follow-up, which might be a source of confounding variables if the concomitant use occurred unequally between two groups. However, as concomitant drug use is common [57,58,59,60] in clinical practice for patients taking LAI antipsychotics, our results reflect the comprehensive cardiovascular risks after initiating and continuing treatment of PP1M in the real world, and offered insights from clinical practice. Future studies should focus on improving the assessments of exposure and potential confounding variables, examining real-world associations among other large populations, and exploring the potential underlying mechanisms of the associations between LAIs and cardiovascular risks.
5 Conclusion
In summary, this study presents the first report on population-based incidence rates of cardiovascular events among schizophrenic patients initiating treatment with PP1M. The findings indicate that PP1M treatment is not associated with increased risks of serious cardiovascular events when compared with oral SGAs. Additionally, there is a potential association suggesting lower risks of cardiovascular hospitalizations compared with oral SGAs. These results contribute to the growing real-world evidence at the population level, providing additional insights into the pharmacologic profile of PP1M in relation to its cardiovascular risk. Moreover, considering the advantage of improved treatment adherence associated with PP1M, these findings hold significant implications for its appropriate use in clinical practice.
References
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2018;44(6):1195–203.
Correll CU, Rubio JM, Kane JM. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry. 2018;17(2):149–60.
Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150(6):1115–21.
Veeneman RR, Vermeulen JM, Abdellaoui A, Sanderson E, Wootton RE, Tadros R, et al. Exploring the relationship between schizophrenia and cardiovascular disease: a genetic correlation and multivariable mendelian randomization study. Schizophr Bull. 2021;48(2):463–73.
Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease—a non-systematic review of epidemiology, possible causes, and interventions. Front Psych. 2014;5:137.
Henderson DC, Vincenzi B, Andrea NV, Ulloa M, Copeland PM. Pathophysiological mechanisms of increased cardiometabolic risk in people with schizophrenia and other severe mental illnesses. Lancet Psychiatry. 2015;2(5):452–64.
Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart (British Cardiac Society). 2003;89(11):1363–72.
Wu CS, Tsai YT, Tsai HJ. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Assoc. 2015;4(2).
De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol. 2011;8(2):114–26.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23.
Rotella F, Cassioli E, Calderani E, Lazzeretti L, Ragghianti B, Ricca V, et al. Long-term metabolic and cardiovascular effects of antipsychotic drugs. A meta-analysis of randomized controlled trials. Eur Neuropsychopharmacol. 2020;32:56–65.
Tenback D, Pijl B, Smeets H, Os J, Harten P. All-cause mortality and medication risk factors in schizophrenia: a prospective cohort study. J Clin Psychopharmacol. 2012;32(1):31–5.
Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360(3):225–35.
Bischoff E, Jakobs KM, Assendelft WJJ. Cardiovascular risk management in patients using antipsychotics: it is time to take action. BMC Med. 2020;18(1):339.
Shah AA, Aftab A, Coverdale J. QTc prolongation with antipsychotics: is routine ECG monitoring recommended? J Psychiatr Pract. 2014;20(3):196–206.
Meyer JM, Stahl SM. Important concepts about second-generation antipsychotics. In: Meyer JM, Stahl SM, editors. The clinical use of antipsychotic plasma levels: stahl’s handbooks. Cambridge: Cambridge University Press; 2021. p. 241–8.
Kane JM, Correll CU. Past and present progress in the pharmacologic treatment of schizophrenia. J Clin Psychiatry. 2010;71(9):1115–24.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Kissling W, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38(1):167–77.
Zipursky RB, Menezes NM, Streiner DL. Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res. 2014;152(2–3):408–14.
Keepers GA, Fochtmann LJ, Anzia JM, Benjamin S, Lyness JM, Mojtabai R, et al. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2020;177(9):868–72.
Manchanda R, Chue P, Malla A, Tibbo P, Roy MA, Williams R, et al. Long-acting injectable antipsychotics: evidence of effectiveness and use. Can J Psychiatry Revue Can Psychiatr. 2013;58(5 Suppl 1):5s–13s.
Sim K, Su A, Ungvari GS, Fujii S, Yang SY, Chong MY, et al. Depot antipsychotic use in schizophrenia: an East Asian perspective. Hum Psychopharmacol. 2004;19(2):103–9.
Correll CU, Martin A, Patel C, Benson C, Goulding R, Kern-Sliwa J, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia (Heidelberg, Germany). 2022;8(1):5.
Yang KC, Liao YT, Yang YK, Lin SK, Liang CS, Bai YM. Evidence-based expert consensus regarding long-acting injectable antipsychotics for schizophrenia from the Taiwanese Society of Biological Psychiatry and Neuropsychopharmacology (TSBPN). CNS Drugs. 2021;35(8):893–905.
Druais S, Doutriaux A, Cognet M, Godet A, Lancon C, Levy P, et al. Cost effectiveness of paliperidone long-acting injectable versus other antipsychotics for the maintenance treatment of schizophrenia in France. Pharmacoeconomics. 2016;34(4):363–91.
Wang H, Zhang Y, Liu J, Chi R, Wu T, Zhang T, et al. Persistence with and adherence to paliperidone palmitate once-monthly injection for schizophrenia treatment in China and Japan. J Clin Psychiatry. 2021;83(1).
Kramer M, Litman R, Hough D, Lane R, Lim P, Liu Y, et al. Paliperidone palmitate, a potential long-acting treatment for patients with schizophrenia. Results of a randomized, double-blind, placebo-controlled efficacy and safety study. Int J Neuropsychopharmacol. 2010;13(5):635–47.
Pandina GJ, Lindenmayer JP, Lull J, Lim P, Gopal S, Herben V, et al. A randomized, placebo-controlled study to assess the efficacy and safety of 3 doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharmacol. 2010;30(3):235–44.
Bossie CA, Sliwa JK, Ma YW, Fu DJ, Alphs L. Onset of efficacy and tolerability following the initiation dosing of long-acting paliperidone palmitate: post-hoc analyses of a randomized, double-blind clinical trial. BMC Psychiatry. 2011;11:79.
Morris MT, Tarpada SP. Long-acting injectable paliperidone palmitate: a review of efficacy and safety. Psychopharmacol Bull. 2017;47(2):42–52.
Fernández-Miranda JJ, Díaz-Fernández S, De Berardis D, López-Muñoz F. Paliperidone palmitate every three months (PP3M) 2-year treatment compliance, effectiveness and satisfaction compared with paliperidone palmitate-monthly (PP1M) in people with severe schizophrenia. J Clin Med. 2021;10(7):1408.
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, et al. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349–58.
Suissa S, Moodie EE, Dell’Aniello S. Prevalent new-user cohort designs for comparative drug effect studies by time-conditional propensity scores. Pharmacoepidemiol Drug Saf. 2017;26(4):459–68.
Yang CY, Kuo S, Lai EC, Ou HT. Three-step matching algorithm to enhance between-group comparability and minimize confounding in comparative effectiveness studies. Sci Rep. 2022;12(1):214.
Lin CY, Ma T, Lin CC, Kao CH. The impact of global budgeting on health service utilization, health care expenditures, and quality of care among patients with pneumonia in Taiwan. Eur J Clin Microbiol Infect Dis. 2016;35(2):219–25.
Fernández-Ruiz M, Guerra-Vales JM, Colina-Ruizdelgado F. Comorbidity negatively influences prognosis in patients with extrahepatic cholangiocarcinoma. World J Gastroenterol. 2009;15(42):5279–86.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmaceut Stat. 2011;10(2):150–61.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Hennessy S, Leonard CE, Freeman CP, Deo R, Newcomb C, Kimmel SE, et al. Validation of diagnostic codes for outpatient-originating sudden cardiac death and ventricular arrhythmia in Medicaid and Medicare claims data. Pharmacoepidemiol Drug Saf. 2010;19(6):555–62.
Tamariz L, Harkins T, Nair V. A systematic review of validated methods for identifying ventricular arrhythmias using administrative and claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):148–53.
Tang CH, Ramcharran D, Yang CW, Chang CC, Chuang PY, Qiu H, et al. A nationwide study of the risk of all-cause, sudden death, and cardiovascular mortality among antipsychotic-treated patients with schizophrenia in Taiwan. Schizophr Res. 2021;237:9–19.
Fox J. Cox proportional-hazards regression for survival data: appendix to an R and S-PLUS companion to applied regression. 2002 [cited 24 Aug 2022]. https://socialsciences.mcmaster.ca/jfox/Books/Companion-1E/appendix-cox-regression.pdf
Nguyen TL, Collins GS, Spence J, Daurès JP, Devereaux PJ, Landais P, et al. Double-adjustment in propensity score matching analysis: choosing a threshold for considering residual imbalance. BMC Med Res Methodol. 2017;17(1):78.
Papola D, Ostuzzi G, Gastaldon C, Morgano GP, Dragioti E, Carvalho AF, et al. Antipsychotic use and risk of life-threatening medical events: umbrella review of observational studies. Acta Psychiatr Scand. 2019;140(3):227–43.
Hennessy S, Bilker WB, Knauss JS, Margolis DJ, Kimmel SE, Reynolds RF, et al. Cardiac arrest and ventricular arrhythmia in patients taking antipsychotic drugs: cohort study using administrative data. BMJ (Clinical research ed). 2002;325(7372):1070.
Leonard CE, Freeman CP, Newcomb CW, Bilker WB, Kimmel SE, Strom BL, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in medicaid and dually-eligible medicaid-medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;10(6):1–9.
Tang CH, Shen SP, Huang MW, Qiu H, Watanabe S, Goh CH, et al. Risks of all-cause death and completed suicide in patients with schizophrenia/schizoaffective disorder treated with long-acting injectable or oral antipsychotics: a population-based retrospective cohort study in Taiwan. Eur Psychiatry. 2021;65(1): e5.
Kishi T, Matsunaga S, Iwata N. Mortality risk associated with long-acting injectable antipsychotics: a systematic review and meta-analyses of randomized controlled trials. Schizophr Bull. 2016;42(6):1438–45.
Wei Y, Yan VKC, Kang W, Wong ICK, Castle DJ, Gao L, et al. Association of long-acting injectable antipsychotics and oral antipsychotics with disease relapse, health care use, and adverse events among people with schizophrenia. JAMA Netw Open. 2022;5(7): e2224163.
Jaeger M, Rossler W. Attitudes towards long-acting depot antipsychotics: a survey of patients, relatives and psychiatrists. Psychiatry Res. 2010;175(1–2):58–62.
Heres S, Hamann J, Kissling W, Leucht S. Attitudes of psychiatrists toward antipsychotic depot medication. J Clin Psychiatry. 2006;67(12):1948–53.
Huang CY, Fang SC, Shao YJ. Comparison of long-acting injectable antipsychotics with oral antipsychotics and suicide and all-cause mortality in patients with newly diagnosed schizophrenia. JAMA Netw Open. 2021;4(5): e218810.
Heres S, Reichhart T, Hamann J, Mendel R, Leucht S, Kissling W. Psychiatrists’ attitude to antipsychotic depot treatment in patients with first-episode schizophrenia. Eur Psychiatry. 2011;26(5):297–301.
Kishimoto T, Hagi K, Kurokawa S, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry. 2021;8(5):387–404.
Mauri MC, Reggiori A, Paletta S, Di Pace C, Altamura AC. Paliperidone for the treatment of schizophrenia and schizoaffective disorders—a drug safety evaluation. Expert Opin Drug Saf. 2017;16(3):365–79.
Aggarwal NK, Sernyak MJ, Rosenheck RA. Prevalence of concomitant oral antipsychotic drug use among patients treated with long-acting, intramuscular, antipsychotic medications. J Clin Psychopharmacol. 2012;32(3):323–8.
Doshi JA, Pettit AR, Stoddard JJ, Zummo J, Marcus SC. Concurrent oral antipsychotic drug use among schizophrenia patients initiated on long-acting injectable antipsychotics post-hospital discharge. J Clin Psychopharmacol. 2015;35(4):442–6.
Cordiner M, Shajahan P, McAvoy S, Bashir M, Taylor M. Effectiveness of long-acting antipsychotics in clinical practice: 2. Effects of antipsychotic polypharmacy on risperidone long-acting injection and zuclopenthixol decanoate. Ther Adv Psychopharmacol. 2016;6(2):66–76.
Dimitropoulos E, Drogemuller L, Wong K. Evaluation of concurrent oral and long-acting injectable antipsychotic prescribing at the Minneapolis veterans affairs health care system. J Clin Psychopharmacol. 2017;37(5):605–8.
Acknowledgements
This study used data obtained from linked databases maintained by the HWDC, Ministry of Health and Welfare, Executive Yuan, Taiwan.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by Janssen Research & Development LLC (Titusville, NJ, USA).
Conflicts of interests
The authors declare the following conflicts of interest. Li Yan, Tao Wu, Kuan-Chih Huang, Hong Qiu, and Yongjing Zhang are employees of Global Epidemiology, Office of Chief Medical Officer, Johnson & Johnson. Hong Qiu and Yongjing Zhang report stock ownership in Johnson & Johnson. Shih-Pei Shen, Min-Wei Huang, and Chao-Hsiun Tang declare no conflicts of interest.
Availability of data and material
The data underlying this study are from the National Health Insurance Research Database, which has been transferred to the Health and Welfare Data Science Center (HWDC). The Taiwan government prohibits the release of the NHI claims dataset to the public domain. Interested researchers can obtain the data through formal application to the HWDC, Department of Statistics, Ministry of Health and Welfare, Taiwan (http://dep.mohw.gov.tw/DOS/np-2497-113.html).
Ethics approval
De-identified aggregated patient data were used for the analysis. This study was granted an exemption from ethical review by the Taipei Medical University-Joint Institutional Review Board and an exemption from the need for patient consent. The study was conducted according to all applicable guidelines and regulations.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
Data curation: CHT and SPS. Formal analysis: CHT and SPS. Data interpretation: MWH. Manuscript review and editing: All authors. Methodology: LY, TW, HQ, YZ and CHT. Project administration: LY, TW, and KCH. Protocol writing: LY and TW. Study conceptualization: HQ, YZ and CHT. Supervision: HQ, YZ and CHT. All authors have reviewed and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shen, SP., Yan, L., Wu, T. et al. Risk of Cardiovascular Events in Schizophrenic Patients Treated with Paliperidone Palmitate Once-Monthly Injection (PP1M): A Population-Based Retrospective Cohort Study in Taiwan. Clin Drug Investig (2024). https://doi.org/10.1007/s40261-024-01358-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s40261-024-01358-y