Abstract
Background and Objectives
Palbociclib is a cyclin-dependent kinase 4/6 inhibitor that is approved in the United States for the treatment of hormone receptor‒positive (HR+)/human epidermal growth factor receptor‒2 negative (HER2−) advanced breast cancer (ABC). The objectives of this expanded access trial were to provide palbociclib in combination with letrozole to patients with HR+/HER2− ABC in Argentina, Brazil, Colombia, and Mexico who were candidates for letrozole therapy before commercial availability of palbociclib, and to evaluate the safety and tolerability of palbociclib plus letrozole.
Patients and Methods
Postmenopausal women aged ≥ 18 years with HR+/HER2− ABC were eligible to participate in this study. Patients received palbociclib 125 mg once daily (3/1 schedule) and letrozole 2.5 mg once daily (continuous schedule). Safety, objective response rate (ORR), and duration of treatment were evaluated.
Results
A total of 130 patients were treated with palbociclib plus letrozole (Argentina, n = 33; Brazil, n = 35; Colombia, n = 28; Mexico, n = 34). The most common treatment-emergent adverse events (TEAEs) of any grade were neutropenia (70.0%), leukopenia (34.6%), anemia (33.8%), decreased neutrophil count (27.7%), and thrombocytopenia (24.6%); 22.3% of patients required a palbociclib dose reduction due to adverse events (AEs). Serious AEs were reported in 32 patients (24.6%). The ORR was 24.8% (95% confidence interval 17.6‒33.2), and the median duration of treatment was 10.6 months (range 0.1‒29.3).
Conclusion
Palbociclib in combination with letrozole was generally well tolerated with a clinically manageable safety profile; the observed ORR supported treatment benefit in Latin American women with HR+/HER2− ABC.
Trial Registry
ClinicalTrials.gov, NCT02600923.
Plain Language Summary
This study was done to learn more about the safety of 2 medicines together for women with advanced breast cancer after menopause. All 130 women in the study had the most common kind of breast cancer and were from Argentina, Brazil, Colombia, and Mexico. Everyone took 2 oral medicines called palbociclib and letrozole during the study. The researchers looked for any side effects experienced by the women while taking these medicines together. Another goal of the study was to see how well the treatment worked. Blood tests showed 70.0% of women had a side effect where they had a lower number of a type of white blood cell called a neutrophil. In total, 34.6% of women had low levels of another white blood cell called a leukocyte. These blood test results can mean a person is more likely to get infections. Serious side effects were experienced by 24.6% of the women, which meant these were life-threatening, caused lasting problems, or they needed hospital care. To cope with their side effects, 22.3% of the women switched to a lower palbociclib dose; 24.8% of the women had an overall response, which meant they either had a decrease in their tumor size or all cancer signs disappeared from their body. The most common length of time in the study was 10.6 months and the longest time was 29.3 months. The results of this study support using palbociclib plus letrozole to treat women who live in Latin America with advanced breast cancer after menopause.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Of the 130 women with advanced breast cancer after menopause treated with palbociclib plus letrozole, 70.0% had neutropenia and 24.6% had serious adverse events; the overall safety profile was similar to other studies where participants took these 2 medications together. |
In this study, the overall response rate was 24.8% for women taking palbociclib with letrozole and the median duration of treatment was 10.6 months. |
The results of this study suggest women with advanced breast cancer after menopause in Latin America could be treated with palbociclib and letrozole together. |
1 Introduction
In Latin America, breast cancer is the most common form of cancer in women, with most cases diagnosed at a late stage [1]. Approximately 115,000 women are diagnosed with breast cancer and 37,000 die each year [1]. Compared with patients in the USA, patients in Latin America are twice as likely to die from breast cancer [1]. Access to breast cancer care and treatment varies across Latin America depending on geographic location and patients’ type of insurance [1]. The AMAZONA III study of breast cancer in Brazil, the country with the largest population in Latin America, showed that privately insured patients were more frequently diagnosed at stage I than publicly insured patients (40.6% vs 18.5%) [2].
Endocrine therapy has been well established as a first-line treatment for postmenopausal women with hormone receptor–positive (HR+)/human epidermal growth factor receptor‒2 negative (HER2−) advanced breast cancer (ABC) [3, 4]. The recent development of cyclin-dependent kinase 4/6 (CDK4/6) inhibitors led the European Society for Medical Oncology guidelines to recommend the addition of a CDK4/6 inhibitor to endocrine therapy as a preferred treatment for patients with HR+/HER2− ABC [3]. Although practice is changing due to multiple available treatment guidelines, many physicians in Latin America still treat these patients with first-line chemotherapy instead of endocrine therapy, potentially due to lack of access to newer drugs, culture, and burden of disease [5, 6]. In patients with HR+ breast cancer, a real-world study showed that only 47% of patients in Brazil received endocrine therapy as first-line therapy, with 53% of patients receiving first-line chemotherapy [6]. Endocrine therapy was initiated as first-line treatment for 60% of patients with HR+/HER2− ABC in the USA and 69% of patients in Europe [5, 7]. Additionally, without earlier access to CDK4/6 inhibitors, patients in Latin America are now receiving CDK4/6 inhibitors in later lines after they have received ≥ 3 lines of therapy up to a maximum of 9 lines [6]. Therefore, an unmet need exists in Latin America for better breast cancer screening, earlier diagnosis, improved survival and quality of life for patients with metastatic disease, and improved accessibility to treatments [8].
Palbociclib, the first-in-class CDK4/6 inhibitor, was initially approved in the USA in February 2015 for the treatment of estrogen receptor–positive (ER+)/HER2− ABC in postmenopausal women who had not received prior endocrine therapy for their advanced disease [9]. Palbociclib in combination with letrozole was approved in Argentina in December 2015 [10], Brazil in February 2018, Colombia in October 2018, and Mexico in June 2016. In this expanded access protocol, the primary objective was to provide palbociclib in combination with letrozole to patients with HR+/HER2− ABC in Argentina, Brazil, Colombia, and Mexico who were deemed appropriate candidates for letrozole therapy by their physician before commercial availability of palbociclib. Secondary objectives were to evaluate safety and tolerability of palbociclib plus letrozole, as well as to assess antitumor activity per local clinical practice, but detailed efficacy data were not collected.
2 Patients and Methods
2.1 Study Design
This was a multicenter, single-arm, open-label, prospective clinical study conducted in Argentina, Brazil, Colombia, and Mexico between April 15, 2016 and May 28, 2019. The protocol was approved by independent ethics committees or institutional review boards at each of the sites participating in the study (supplementary material). The study was conducted in compliance with the ethical principles derived from the Declaration of Helsinki. All patients provided written informed consent at screening before study procedures were performed. The end of the trial was defined by the time of regulatory approval and commercial availability of palbociclib for the treatment of ABC. At that time, patients enrolled in the study were moved to commercial supply. A patient assistance program was designed to cover all patients to ensure that every patient could continue receiving the combination therapy at no cost to them via commercial access.
2.2 Patients and Treatment
At screening (28–30 days before treatment start) patients were evaluated for their eligibility, medical and oncological history, and their Eastern Cooperative Oncology Group (ECOG) performance status. Postmenopausal women aged ≥ 18 years with HR+/HER2− ABC with an ECOG performance status of 0‒2 who, according to their physician, could benefit from letrozole therapy were eligible to participate in this study. Postmenopausal was defined as being in a state of non-childbearing potential by meeting at least 1 of the following: (1) documented hysterectomy and/or bilateral oophorectomy, (2) medically confirmed ovarian failure, and/or (3) had ceased all regular menses for at least 12 consecutive months with no alternative pathological or physiological cause with a serum follicle-stimulating hormone level confirming postmenopausal state. Patients also had to have adequate bone marrow, liver, and renal function. Patients were excluded from the study if they received prior treatment with any CDK inhibitor, had previously participated in a palbociclib clinical study, had a high cardiovascular risk, or had active uncontrolled or symptomatic brain metastases. Patients received palbociclib (Ibrance®, supplied by Pfizer Inc, New York, NY, USA) capsules 125 mg orally once daily for 21 days, followed by 7 days off treatment for each 28-day cycle (3/1 schedule). Patients received letrozole 2.5 mg orally once daily as a continuous daily dose schedule. Dose reduction for palbociclib and treatment interruption for letrozole were allowed in the event of significant treatment-related toxicity. If only 1 study treatment required dose adjustment or interruption, treatment with the other medication could continue as clinically indicated and at the treating physician’s discretion. Treatment continued until palbociclib was permanently discontinued for any reason.
2.3 Outcomes
The safety outcomes were adverse events (AEs), serious AEs, and death from any cause and were monitored at each clinical visit from the time informed consent was obtained until 28 days after palbociclib discontinuation (end of treatment) or until all palbociclib-related toxicities were resolved, whichever was later. Adverse events were characterized by type, frequency, and severity (as graded by National Cancer Institute Common Terminology Criteria for Adverse Events version 4.03), and seriousness. Platelet count, absolute neutrophil count (ANC), white blood cell count, and hemoglobin were assessed at screening, every 2 weeks of the first 2 treatment cycles, monthly on each subsequent cycle, and at end of treatment. Patients who developed grade 3 (ANC < 1000/mm3) or grade 4 (ANC < 500/mm3) neutropenia were managed with temporary dose interruptions and/or dose reductions in accordance with the US palbociclib package insert [11].
The efficacy outcomes assessed included objective response rate (ORR) and duration of treatment. Tumor assessments were performed at screening per local practice and according to the patient’s clinical status thereafter until the end of treatment. Tumor response was determined based on the response reported by the investigator per local practice. No response confirmation assessments were performed. Objective response rate was defined as the proportion of patients with complete response or partial response relative to the as-treated population. Best response was the best outcome the patient achieved out of all the tumor assessments during the study as assessed by the investigator. The duration of treatment was defined as the length of time patients remained on palbociclib from the first day of treatment until the last day of treatment during the study. Because of the nature of the study, no inferential analyses were planned and no hypotheses were tested. Results were presented using descriptive statistics. Confidence intervals (CIs) for ORR were calculated using exact methods based on the binomial distribution. The statistical analyses were performed using version 9.4 of the Statistical Analysis Software (SAS® 9.4).
3 Results
3.1 Patients
A total of 130 patients were treated with palbociclib plus letrozole at 18 sites in Latin America (Argentina, n = 33; Brazil, n = 35; Colombia, n = 28; Mexico, n = 34) between April 2016 and May 2019. All treated patients discontinued from the study (Supplementary Fig. 1). Most discontinuations were not related to the study drug; 40.8% of patients discontinued from the study because the study was terminated by the sponsor (i.e., when palbociclib became commercially available in the patient’s country of residence), and 38.5% discontinued because of objective progression or relapse.
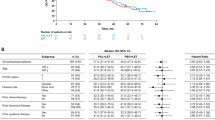
At baseline, mean age was 59.3 years (range 28‒83), and 72.3% of patients were White (Table 1). One hundred seventeen patients (90.0%) had received prior systemic therapies in both the adjuvant and metastatic setting, and 54.6% of patients had received ≥ 2 prior systemic therapies before receiving palbociclib treatment.
3.2 Safety
The median duration of palbociclib treatment was 11 cycles (range 1‒31), with a median relative dose intensity of 90.9%. All-causality AEs were reported in 129 patients (99.2%), and serious AEs were reported in 32 patients (24.6%; Table 2). The most common treatment-emergent adverse events (TEAEs) of any grade were neutropenia (70.0%), leukopenia (34.6%), anemia (33.8%), decreased neutrophil count (27.7%), and thrombocytopenia (24.6%; Table 3). A total of 16 patients (12.3%) experienced TEAEs that resulted in palbociclib discontinuation (the most common AEs were hematologic AEs [n = 3], disease progression [n = 2], and tuberculosis [n = 2]), and 14 patients (10.8%) experienced TEAEs that resulted in letrozole discontinuation. Twenty-nine patients (22.3%) required dose reduction of palbociclib due to AEs, with hematologic AEs being the most common reason patients required dose reduction. Eight patients (6.2%) experienced TEAEs that resulted in discontinuation from the study, most commonly due to disease progression. The most common serious AE experienced by patients was related to neoplasm disease progression (7 patients [5.4%]). From study initiation through 28 days after the last administration of palbociclib, 5 patients died; 7 patients died after Day 28 following the last dose. No patients died due to study treatment toxicities. The most common cause of death was disease progression (8 patients). One patient died due to respiratory insufficiency, 1 patient died due to hypoglycemia, and 2 patients died of unknown causes.
3.3 Efficacy
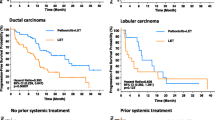
Of the 130 treated patients, 129 had data available for efficacy analyses. The ORR was 24.8% (95% CI 17.6−33.2); 2.3% of patients achieved a best overall response of complete response and 22.5% of patients achieved partial response. Stable disease and objective progression were the best responses in 58.9% and 10.9% of patients, respectively. The median duration of treatment was 10.6 months (range 0.1−29.3).
4 Discussion
In this expanded access trial of 130 postmenopausal women with HR+/HER2− ABC, palbociclib plus letrozole treatment was generally well tolerated; the reported AEs were consistent with the known safety profile of palbociclib plus letrozole, with neutropenia, leukopenia, and anemia most commonly reported. The median duration of palbociclib treatment was 11 cycles, with a median relative dose intensity of 90.9%. Approximately 34% of patients received palbociclib as a ≥ third-line regimen. The observed ORR was 24.8% (95% CI 17.6‒33.2). Because this study was an expanded access protocol that provided eligible patients with access to palbociclib until it became commercially available, no inferential analyses were planned and no hypotheses were tested. Moreover, efficacy outcomes should be cautiously interpreted and interpretation limited to the study treatment period.
Previous clinical trials have shown the benefit of palbociclib in combination with letrozole or fulvestrant [12,13,14,15]. In the PALOMA-1 and PALOMA-2 studies, postmenopausal women with ER+/HER2− ABC were randomized to treatment with palbociclib plus letrozole or letrozole with or without placebo. The palbociclib plus letrozole treatment group had a confirmed ORR of 43% (95% CI 32–54) in PALOMA-1 and 42.1% (95% CI 37.5‒46.9) in PALOMA-2 [13, 14]. Dose adjustments (interruptions, reductions) in the palbociclib plus letrozole treatment group were reported for 33%–40% of patients in the PALOMA-1 study [14] and 36%–67% in the PALOMA-2 study [13]. In the PALOMA-3 study, women with HR+/HER2− metastatic breast cancer of any menopausal status were randomized to treatment with palbociclib plus fulvestrant or fulvestrant plus placebo [15]. The rate of confirmed objective response for the palbociclib plus fulvestrant group was 19% (95% CI 15.0–23.6). Black and Hispanic patients may be underrepresented in clinical trials; however, a post hoc pooled analysis of these patients in the PALOMA-1, 2, and 3 trials found similar rates of grade 3 and 4 AEs as the overall patient population [16]. The safety outcomes reported in this study are consistent with findings from the PALOMA clinical trial program, with neutropenia, leukopenia, fatigue, and nausea being the most common all-causality AEs reported with palbociclib plus letrozole [12,13,14,15].
Real-world studies, which generally include more heterogeneous patient populations than clinical trials and are more representative of patients treated in clinical practice, are important to identify AEs that may not have been reported in the clinical trial setting and to evaluate real-world clinical outcomes [17]. Recent findings from real-world studies support the efficacy and safety of palbociclib [10, 18]. A retrospective medical chart review (IRIS study) evaluated patients with ABC or metastatic breast cancer who received palbociclib combination therapies in clinical practice across various countries. An analysis of 88 patients in Argentina who received palbociclib plus letrozole reported an 85.4% PFS rate at 12 months and 80.4% PFS rate at 18 months. The overall survival rate was 93.4% at 12 months and 88.5% at 18 months. Based on physicians’ assessments, objective responses were achieved in 65% of patients. Most patients (95%) experienced only 1 palbociclib dose adjustment, and among patients who discontinued treatment, nearly half were due to disease progression after initial response. Additionally, a retrospective analysis of electronic health records from the Flatiron Health Analytic database showed a real-world best ORR of 58.6% with palbociclib plus letrozole versus 39.1% with letrozole alone in the first-line setting after propensity score matching adjustment in patients with HR+/HER2− metastatic breast cancer [18]. These real-world data complement the results from clinical studies of palbociclib and support the findings from the present study.
In the current study, the median duration of palbociclib treatment was only 11 cycles and ranged widely from 1 to 31 cycles. Many patients participated in the study for only a short duration because palbociclib became commercially available during the course of this study, resulting in preplanned study termination (40.8% of patients discontinued from the study), and potentially precluded response rates from being reported. In contrast, in the PALOMA-1 study, 23% of patients were still receiving palbociclib and letrozole treatment at a median follow-up duration of 29.6 months, and in the PALOMA-2 study, 44.8% of patients were still receiving palbociclib and letrozole treatment at a median follow-up duration of 23 months [13, 14]. The high discontinuation rate in this study after palbociclib became commercially available may underscore the problem of accessibility in low- and middle-income countries to affordable cancer therapies; in parallel to the growing disease burden in these countries is the widening disparity to access to effective therapies [19].
Potential limitations of this study include nonuniform assessment of tumor response and limited availability of data on long-term responders. In the present study, tumor response assessments were evaluated based on investigator assessment, whereas Response Evaluation Criteria in Solid Tumors were applied in the PALOMA studies [13,14,15]. Additionally, early termination of the study due to the commercial availability of palbociclib limited data collection from responders over longer follow-up durations. Despite these limitations, this study supports the existing literature on the safety and efficacy of palbociclib.
5 Conclusion
This expanded access trial provided postmenopausal women with HR+/HER2− ABC in Argentina, Brazil, Colombia, and Mexico who were deemed appropriate candidates for letrozole treatment with palbociclib plus letrozole. Palbociclib plus letrozole was generally well tolerated with manageable AEs, and the observed ORR supported the treatment benefit.
Change history
11 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40261-023-01305-3
References
Cazap E. Breast cancer in Latin America: a map of the disease in the region. Am Soc Clin Oncol Educ Book. 2018;23(38):451–6.
Rosa DD, Bines J, Werutsky G, Barrios CH, Cronemberger E, Queiroz GS, et al. The impact of sociodemographic factors and health insurance coverage in the diagnosis and clinicopathological characteristics of breast cancer in Brazil: AMAZONA III study (GBECAM 0115). Breast Cancer Res Treat. 2020;183(3):749–57.
Cardoso F, Senkus E, Costa A, Papadopoulos E, Aapro M, André F, et al. 4th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 4). Ann Oncol. 2018;29(8):1634–57.
Gradishar WJ, Anderson BO, Abraham J, Aft R, Agnese D, Allison KH, et al. Breast cancer, version 3.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18(4):452–78.
Swallow E, Zhang J, Thomason D, Tan RD, Kageleiry A, Signorovitch J. Real-world patterns of endocrine therapy for metastatic hormone-receptor-positive (HR+)/human epidermal growth factor receptor-2-negative (HER2-) breast cancer patients in the United States: 2002–2012. Curr Med Res Opin. 2014;30(8):1537–45.
Barrios C, Uema D, Cronenberger E, Lima V, Bines J, de Sant’ana R, et al. Real world data and patterns of care of metastatic breast cancer (MBC) in Brazil: first results of LACOG 0312 retrospective study. Cancer Res. 2017;77(4 suppl):P6-16–04.
Andre F, Neven P, Marinsek N, Zhang J, Baladi JF, Degun R, et al. Disease management patterns for postmenopausal women in Europe with hormone-receptor-positive, human epidermal growth factor receptor-2 negative advanced breast cancer. Curr Med Res Opin. 2014;30(6):1007–16.
Justo N, Wilking N, Jonsson B, Luciani S, Cazap E. A review of breast cancer care and outcomes in Latin America. Oncologist. 2013;18(3):248–56.
Beaver JA, Amiri-Kordestani L, Charlab R, Chen W, Palmby T, Tilley A, et al. FDA approval: palbociclib for the treatment of postmenopausal patients with estrogen receptor-positive, HER2-negative metastatic breast cancer. Clin Cancer Res. 2015;21(21):4760–6.
Waller J, Mitra D, Mycock K, Taylor-Stokes G, Milligan G, Zhan L, et al. Real-world treatment patterns and clinical outcomes in patients receiving palbociclib for hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced or metastatic breast cancer in Argentina: the IRIS study. J Glob Oncol. 2019;5:JGO1800239.
IBRANCE® capsules. palbociclib. New York: Pfizer Inc; 2019.
Rugo HS, Finn RS, Dieras V, Ettl J, Lipatov O, Joy AA, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Res Treat. 2019;174(3):719–29.
Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–36.
Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16(1):25–35.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–39.
Isaacs C, Mahtani R, Lynce F, Sleckman B, Castrellon A, Kalmadi S, et al. Abstract P1-18-13: Efficacy and safety of palbociclib plus endocrine therapy in Black and Hispanic patients with hormone receptor positive/human epidermal growth factor receptor 2-negative advanced breast cancer (HR+/HER2− ABC) participating in the PALOMA trials. Cancer Res. 2022;82(4):P1-18–13.
Webster J, Smith BD. The case for real-world evidence in the future of clinical research on chronic myeloid leukemia. Clin Ther. 2019;41(2):336–49.
Brufsky A, Liu X, Li B, McRoy L, Layman RM. Real-world tumor response of palbociclib plus letrozole vs letrozole for metstatic breast cancer in US clinical practice. In: European Society for Medical Oncology Breast Cancer Virtual Meeting; 2020 May 23-24; 2020.
Bharadwaj M, Vallurupalli M, Huang FW. Global precision oncology: a call to action on expanding access to targeted cancer therapies. Oncologist. 2021;26(5):353–5.
Acknowledgments
All authors provided analysis and interpretation of the data, drafted, or revised the manuscript critically for important intellectual content, and provided the final decision to submit the manuscript for publication. The authors thank Dr. Cesar Blajman and Dr. Gustavo Adolfo Rojas Uribe for their contributions to this study. Editorial support was provided by Anny Wu, PharmD, of ICON plc, North Wales, PA, USA, and Oxford PharmaGenesis Inc., Newtown PA, USA, and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Pfizer Inc. The sponsor was involved in study design and data collection.
Conflicts of Interest
LF, NL, FD, SF, and YLC have no conflicts of interest. JRGRB has served as an investigator in sponsored trials for Pfizer, Bristol Myers Squibb, and MSD and as a sponsored speaker for Pfizer, AstraZeneca, and Novartis. MSM has been compensated for lectures and educational support from Pfizer Brazil. JL has served as a speaker and on a scientific advisory board for Roche, MSD, AstraZeneca, Pfizer, and Novartis. EK has received fees from Pfizer for participating in the clinical trial. DRL and SJP are employees of and own stock in Pfizer Inc. AM is an employee of and owns stock in Pfizer S.r.l.
Ethics Approval
The protocol was approved by the independent ethics committees or institutional review boards at each of the sites participating in the study (see supplementary material). The study was conducted in compliance with the ethical principles derived from the Declaration of Helsinki.
Consent to Participate
All patients provided written informed consent at screening before study procedures were performed.
Consent for Publication
Not applicable.
Availability of Data and Material
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Code Availability
Not applicable.
Author Contributions
LF, NL, YLC, JRGRB, MSM, JL, EK, FD, and SF contributed to the collection and assembly of data, and manuscript writing. DRL performed the data analysis and interpretation, and contributed to the manuscript writing. AM and SJP contributed to the concept and design, and the manuscript writing. All authors read and approved the final manuscript, and agree to be accountable for all aspects.
Additional information
The original online version of this article was revised due to a retrospective Open Access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fein, L., Lazaretti, N., Chuken, Y.L. et al. Expanded Access Study of Palbociclib Plus Letrozole for Postmenopausal Women with HR+/HER2− Advanced Breast Cancer in Latin America for Whom Letrozole Therapy is Deemed Appropriate. Clin Drug Investig 43, 699–706 (2023). https://doi.org/10.1007/s40261-023-01294-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01294-3