Abstract
Background and Objectives
Data on the effect of food on the pharmacokinetics of senaparib (previously IMP4297), an oral poly (adenosine diphosphate-ribose) polymerase inhibitor, are limited. This study was conducted to evaluate the effect of food on the pharmacokinetics of senaparib in healthy Chinese subjects.
Methods
This is a phase I, open-label, randomized, single-dose, two-way crossover study. Healthy Chinese male subjects were randomized 1:1 to receive a single dose of senaparib 100 mg in two prandial states: fasted or after a high-fat meal; subjects were given a second dose after switching prandial states and a washout period of at least 7 days. Pharmacokinetics were assessed at pre-dose and up to 72 h post-dose. Safety was assessed throughout the study.
Results
Sixteen subjects were randomized and included in the pharmacokinetic analysis; 15 completed the study. The presence of food slowed the rate of senaparib absorption (time to maximum concentration) by ~ 3 h and reduced the maximum concentration of senaparib by ~ 24%. Total exposure to senaparib was higher in the fed than fasted state; senaparib area under the plasma concentration–time curve from time zero to the last measurable concentration and area under the plasma concentration–time curve from time zero to infinity were increased by ~ 24 and ~28%, respectively. Safety profiles were similar in both prandial states. All treatment-emergent adverse events were grade 1 in severity; no serious adverse events or deaths were reported.
Conclusions
Food slightly decreased the rate and increased the extent of senaparib absorption following oral administration. However, the effect of food on various exposure parameters was not considered clinically meaningful. Safety data were consistent with the known profile of senaparib and senaparib was well tolerated in the fed and fasted states in healthy subjects. These results indicated that senaparib could be administered orally with or without food.
Clinical Trial Registration
ClinicalTrials.gov NCT04057729.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Results of this study showed that senaparib was absorbed faster without food; however, its exposure and bioavailability were slightly higher with food intake in healthy Chinese subjects. |
The effect of food on oral senaparib pharmacokinetics was not considered to be clinically relevant because of its wide therapeutic range. |
1 Introduction
Tumor cells that have defects in homologous recombination repair, such as those with mutations in breast cancer susceptibility genes 1 or 2 (BRCA1/2), are sensitive to poly (adenosine diphosphate-ribose) polymerase (PARP) inhibition [1]. The selective vulnerability of these tumor cells to PARP inhibitors can be explained by synthetic lethality: PARP inhibition causes the accumulation of DNA damage that is otherwise repaired by a functional homologous recombination repair pathway, leading to cell death [1]. In addition, PARP trapping occurs at sites of DNA damage under PARP inhibition, another key mechanism leading to cell death. To date, a number of PARP inhibitors have been developed, with several approved worldwide [2,3,4,5].
Senaparib (previously IMP4297) is a novel PARP inhibitor that demonstrates potent enzymatic inhibition against both PARP-1 and PARP-2 and a higher potency to induce PARP-1 trapping than olaparib [6]. In pre-clinical studies using various in vitro and ex vivo models, senaparib demonstrated greater anti-tumor activity than olaparib without increasing toxicity [6]. Pre-clinical pharmacokinetic studies showed dose proportionality (dose levels increased proportionally from 0.1 to 1 mg/kg in rats and from 0.2 to 0.8 mg/kg in dogs), good oral bioavailability (68.5% in dogs, with an elimination half-life [t½] of ~ 4.50 ± 0.15 h), and wide tissue distribution of senaparib, and indicated that this drug is mainly metabolized by cytochrome P450 (CYP) 3A4 in the liver and excreted via the feces (unpublished data). Its low activity against five CYPs (half maximal inhibitory concentration > 30 μM against CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4) also suggests low risk of drug–drug interactions [6]. In two phase I studies of senaparib in Australian and Chinese patients with advanced tumors, the exposure to senaparib reflected by maximum concentration (Cmax) and area under the plasma concentration–time curve (AUC) demonstrated an increasing trend from 2 to 80 mg, but appeared to plateau above 80 mg [7, 8]. In Australian patients, the median time to reach Cmax (Tmax) ranged from 2.0 to 2.3 h across the different dosages from 2 to 120 mg, when given in the fasted state. Similarly, in Chinese patients, Tmax following a single dose of 2–150 mg ranged between 2.0 and 2.7 h. It should be noted that these pharmacokinetic parameters were reported for day 15 of cycle 1, with 21 days as a cycle.
In the same dose-escalation, phase I clinical trials, no dose-limiting toxicities were observed when the dose of senaparib was escalated up to 150 mg once daily (QD), and anti-tumor activity was demonstrated across the dose range of 20 mg to 150 mg QD, and 50 mg twice daily (in the fasted state), while absorption seemed to saturate at around 80 mg QD and above following oral administration [7, 8]. In addition, the median dose used in 12 patients who achieved a partial response was 80 mg QD (unpublished data). Considering the high inter-subject variability in senaparib exposure, 100 mg QD was selected to minimize the potential risk of having lower exposure in patients for subsequent phase II/III studies. Moreover, no dose-limiting toxicities were observed at 80, 100, and 120 mg, and a pre-clinical study showed that 100 mg QD was sufficient to cover the half maximal inhibitory concentration in vitro (unpublished data). Based on the efficacy, safety, and pharmacokinetic results, the recommended dose for the phase II study was 100 mg QD.
Food may change the bioavailability of an oral drug by affecting its absorption through the gastrointestinal tract, its metabolism, or by interacting with the drug substance [9]. In this phase I study, we evaluated the effect of food on the pharmacokinetics of senaparib in healthy Chinese male subjects.
2 Subjects and Methods
2.1 Study Design
This was a phase I, open-label, randomized, single-dose, two-way crossover study to evaluate the effect of food on the pharmacokinetics of senaparib. The study was conducted at the Shanghai Public Health Clinical Center, China. Subjects were randomized to two sequence groups (1:1), in which subjects received a single oral dose of senaparib under fasted states in period 1 and under fed conditions in period 2 (sequence group 1), or vice versa (sequence group 2). Eight subjects were planned to be included in each sequence. A washout phase of at least 7 days separated the two treatment periods.
This study was designed and conducted in accordance with the Declaration of Helsinki, Good Clinical Practice guidelines, and applicable Chinese National Medical Products Administration regulations (e.g., the Drug Registration Regulation [10], Good Clinical Practice [11], and the Technical Guidelines for Clinical Pharmacokinetics Study of Chemical Medicine [12]). Informed consent was obtained from all subjects before any study-related procedures were performed. The study protocol and informed consent information were approved by the Ethics Committee at the Shanghai Public Health Clinical Center. This trial was registered with ClinicalTrials.gov, number NCT04057729.
2.2 Subjects
Eligible subjects were healthy Chinese male adults aged 18–55 years with a body mass index of 19.0–26.0 kg/m2 and body weight of ≥ 50.0 kg. Enrolled subjects needed to have no plans for conception or sperm donation and be willing to use effective contraception from the start of the study to 90 days after the last dose of the investigational drug. Key exclusion criteria included: lactose intolerance; a history of diseases/conditions or use of medications that may interfere with the trial results or pose a risk to the subjects; vaccination; surgery; drug abuse; and excessive consumption of alcohol, tobacco, tea, coffee, and/or caffeine-rich beverages. Concomitant medications were not allowed during the study, except those for adverse event management.
2.3 Interventions
Subjects took a single oral dose of senaparib 100 mg with 240 mL of warm water. Food effect was tested with a high-fat meal, which was high calorie (800–1000 kcal) and high fat (approximately 50% of total calories of the meal were derived from fat) with 150, 250, and 500–600 kcal calories derived from proteins, carbohydrates, and fats, respectively, designed in accordance with the Technical Guidelines for Clinical Pharmacokinetics Study of Chemical Medicine [12]. Subjects were instructed to finish the meal within 30 min.
In the fasted state, subjects were fasted overnight for at least 10 h before taking senaparib, with meals allowed 4 h post-dose. In the fed state, subjects were fasted overnight for at least 10 h and received a high-fat meal 30 mins before taking senaparib, with another meal allowed 4 h post-dose. Drinking water was not allowed 1 h pre-dose and post-dose except during the administration of senaparib.
2.4 Endpoints and Assessments
The primary endpoint was the pharmacokinetics parameters of senaparib. This included Cmax, Tmax, AUC from time zero to the last measurable concentration (AUC0–last), AUC from zero to infinity (AUC0–inf), t½, apparent clearance, and apparent volume of distribution.
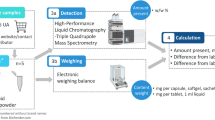
Blood samples (approximately 3 mL) for the pharmacokinetic analysis were collected at 0 (within 1 h pre-dose), 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 10, 12, 24, 48, and 72 h post-dose. Senaparib concentration in human ethylene diamine tetraacetic acid dipotassium plasma was measured using a pre-validated, liquid chromatography-tandem mass spectrometry method (Q Squared Solutions, Beijing, China). Blood samples were immediately inverted gently at least five times to mix the blood with ethylene diamine tetraacetic acid dipotassium, and centrifuged at approximately 3000 rpm for 10–15 min at 4 °C within 60 min from the collection. The plasma was then transferred into storage tubes and stored at − 20 °C or below before transfer to Q Squared Solutions (Beijing) Co., Ltd, a laboratory for bioanalysis of senaparib.
Safety was assessed by reviewing treatment-emergent adverse events (TEAEs), clinical laboratory tests, vital signs, and 12-lead electrocardiograms. Electrocardiograms were performed at prespecified timepoints (matched with pharmacokinetic sampling times) pre-dose and post-dose. Adverse events were monitored up to 1 month after the last dose. Treatment-emergent adverse events were coded using the Medical Dictionary for Regulatory Activities, version 22.0 and graded according to Common Terminology Criteria for Adverse Events, version 4.03. Treatment-emergent adverse events of special interest included drug-induced liver injury; pregnancy; drug-related neutropenia of grade 3 or worse; drug-related thrombocytopenia of grade 3 or worse; drug-related hypochromia of grade 3 or worse; and medication error, overdose, abuse, or misuse.
2.5 Statistical Analysis
It was planned that 16 subjects would be enrolled in this trial. Assuming a dropout rate of 25%, it was estimated that 12 subjects would complete the study. This would provide the trial with 11 and 15% accuracy (width of 90% confidence interval [CI]) to show a difference in AUC and Cmax in the fed state relative to the fasted state, respectively (at a geometric mean ratio [GMR] of 50%) under a small intra-subject variability (assuming the standard deviation of loge AUC and loge Cmax is 0.15 and 0.20, respectively), and provide corresponding 22 and 29% accuracy under a large intra-subject variability (assuming the standard deviation of loge AUC and loge Cmax is 0.30 and 0.40, respectively).
Pharmacokinetics parameters were calculated in subjects who received at least one dose of study drug and had at least one evaluable pharmacokinetics parameter for senaparib. Safety was assessed in all subjects who received at least one dose of the study drug and had evaluable data for post-dose safety evaluation.
Pharmacokinetic parameters were calculated by a non-compartmental analysis using WinNonlin™ software version 8.2 (Certara USA Inc., Princeton, NJ, USA). Log-transformed AUC0–last, AUC0–inf, and Cmax were determined using a mixed-effects model, with the sequence, period, and treatment as the fixed effect, and subjects within the sequence as the random effect. Geometric mean ratios and corresponding 90% CIs of log-transformed AUC0–last, AUC0–inf, and Cmax in the fed state relative to the fasted state were calculated. An absence of food effect would be concluded if the 90% CI of the GMR fell within 80.00–125.00% for AUC0–last, AUC0–inf, and Cmax. Descriptive statistics were used to summarize the pharmacokinetic parameters (Cmax, Tmax, AUC0–last, AUC0–inf, t½, apparent clearance, and apparent volume of distribution) in the fasted and fed states. Using linear and semi-log scales, the plasma concentration–time profiles (mean ± standard deviation curves) were plotted.
2.6 Bioanalytical Assay
Analytical procedures and conduct of biological sample analysis according to the Good Laboratory Practice issued by the National Medical Products Administration in China and laboratory standard operating procedures were carried out by Q Squared Solution (Beijing) Co., Ltd. During the bioanalytical process, the quality assurance personnel of the bioanalytic unit reviewed the sample analysis scheme according to the study protocol and reviewed sample receipt records, sample management, standard substance management, verified sample analysis on-site, and audited the data and report. There were 11 analytical runs for sample analysis, including two solution comparison runs, two pre-study measurement and evaluation runs, and seven sample analysis runs. The first sample and last sample were analyzed within 45 days.
3 Results
3.1 Subject Disposition and Baseline Characteristics
Between 22 July, 2019 and 30 August, 2019, 64 subjects were screened, among whom 16 subjects were enrolled and randomized (eight subjects in each sequence; Fig. 1). Of them, 15 subjects completed the study; one subject in sequence 1 withdrew from the trial because of anemia without receiving the dose in the fed state in period 2. All randomized subjects (n = 16) were included in the pharmacokinetic analysis and safety assessment. Overall, 16 and 15 subjects in the fasted and fed state were evaluable, respectively.
Baseline characteristics are shown in Table 1. The mean age of subjects was 28.20 ± 6.24 years, with a mean weight of 62.76 kg (range 57.20–76.20) and mean body mass index of 21.40 kg/m2 (range 19.40–24.60).
3.2 Pharmacokinetics
As shown in the plasma concentration–time profiles for senaparib after oral administration, senaparib was absorbed faster in the fasted state compared with the fed state (median Tmax, 2.0 h [range 0.5–4.0] vs. 5.0 h [range 3.0–12.0], respectively; Fig. 2), while being eliminated at a similar rate (mean t½, 8.66 ± 3.67 h vs 7.92 ± 4.53 h, respectively; Table 2). In the fed state, senaparib reached a slightly lower Cmax compared with that in the fasted state (mean Cmax, 1680 vs 1300 ng/mL). The total exposure to senaparib was higher in the fed state versus the fasted state (mean AUC0–last, 13400 vs 10500 hng/mL; mean AUC0–inf, 13900 vs 10700 hng/mL).
In addition, there was lower inter-subject variability in exposure to senaparib after oral administration in the fasted state compared with the fed stated, as indicated by the smaller coefficients of variation for Cmax (16 vs 25%), AUC0–last (24 vs 37%), and AUC0–inf (24 vs 38%). Similarly, other pharmacokinetic parameters related to distribution, clearance, and elimination of senaparib also demonstrated lower inter-subject variability in the fasted state.
The GMRs of Cmax, AUC0–last, and AUC0–inf were 0.76, 1.24, and 1.28, respectively. The lower limit of 90% CI (0.6637) for the GMR of Cmax was below the 80.0–125.0% bioequivalence range, while the upper limits of 90% CIs of the GMRs of AUC0–last (1.4192) and AUC0–inf (1.4914) were above the bioequivalence range. These results indicate that food had a slight effect on the absorption of senaparib; however, the slight changes in Cmax (decreased by 24%), AUC0–last (increased by 24%), and AUC0–inf (increased by 28%) are not considered clinically significant.
3.3 Safety
Treatment-emergent adverse events were reported in five (31.25%) subjects who received senaparib in the fasted state, and four (26.67%) subjects who received senaparib in the fed state. All TEAEs were grade 1 in severity. No serious adverse events or deaths occurred. One subject in the fasted group experienced anemia and withdrew from the study on the investigator’s decision; there were no TEAEs leading to treatment discontinuation. All TEAEs were abnormalities in laboratory tests or electrocardiograms (Table 3). No TEAEs of special interest were reported. All TEAEs resolved without medical intervention except for one laboratory finding of hematuria, for which the outcome was unknown because the subject rejected a follow-up re-examination. One TEAE was considered related to the study drug, which was the aforementioned event of anemia in one subject in the fasted group. The pattern of TEAEs did not reveal any notable differences between the fasted state and the fed state. No clinically significant corrected QT interval by Fridericia interval prolongation (defined as absolute corrected QT interval by Fridericia ≥ 500 ms) or change from baseline (defined as a corrected QT interval by Fridericia interval increased by ≥ 45 ms from baseline) was detected in this study.
4 Discussion
Understanding whether food has a clinically relevant interaction with oral anti-cancer drugs is important in order to provide patients with the necessary food intake guidelines to ensure that exposure to the drug does not result in reduced efficacy or higher toxicity in the fed state. The 100-mg dose used in this food effect study of senaparib was selected based on a projected optimal risk–benefit ratio. Healthy subjects revealed a modest change in the absorption/bioavailability of senaparib when taken after a high-fat meal compared with under fasted states (Cmax decreased by 24%, AUC0–last increased by 24%, and AUC0–inf increased by 28%). We postulate that the intake of a high-fat meal would decrease the gastrointestinal motility. When gastrointestinal motility slows down, there is a possibility that the rate of oral absorption of senaparib would also decrease, which was reflected as altered pharmacokinetics such as delayed Tmax and decreased Cmax.
Previously, a preliminary exposure-safety analysis of senaparib in 96 patients with advanced solid tumors (unpublished data). Senaparib was effective at a dose level of 20 mg QD to 120 mg QD. Although patients with higher grade treatment-related adverse events tended to have higher treatment exposure, there were substantial overlaps in the exposure distribution across different treatment-related adverse event grades (< grade 3 vs ≥ grade 3). Additionally, in the ongoing phase II/III clinical studies, any treatment-related toxicity observed during the study could be managed by dose interruption or modification (40 to 100 mg dose range), minimizing the safety risk. Therefore, given the flexible dosing schedule, the difference in the total exposure to senaparib due to food intake was not considered clinically meaningful, indicating that senaparib can be taken with or without food. Similarly, the approved PARP inhibitors olaparib, rucaparib, niraparib, and talazoparib also showed an absence of clinically relevant food effect, and the dosage information in their product package inserts recommends oral intake either with or without food [2,3,4,5, 13,14,15].
Two separate phase I dose-escalation studies in Chinese and Australian patients with solid tumors demonstrated similar absorption and elimination rates, and higher exposure to senaparib after a single oral dose at 100 mg (mean Cmax was 3195.00 ± 1020.62 and 2401.67 ± 896.33 ng/mL, and mean AUC0–inf was 39337.70 ± 17047.57 and 29541.63 ± 12133.28 h⋅ng/mL, in Chinese and Australian patients, respectively) than in healthy subjects [7, 8]. Both studies further characterized the safety, efficacy, and pharmacokinetic profile of senaparib 100 mg, which was consistent in both populations, providing support for dosing recommendations for phase II studies and for this food effect study.
The TEAEs reported in healthy subjects in this study were restricted to abnormal findings in laboratory tests or electrocardiogram results, and all were grade 1 in severity. Adding to these encouraging preliminary safety data, phase I clinical studies in Chinese (n = 57) and Australian patients (n = 39) with solid tumors showed that most TEAEs were grade 1 or 2, and no dose-limiting toxicities occurred at doses of 2–120 mg. The most common TEAEs were hematological abnormalities in Chinese patients, while the most common TEAEs were fatigue, nausea, constipation, and back pain in Australian patients [7, 8]. The findings of laboratory abnormalities in Chinese subjects receiving senaparib are in line with the established adverse event profile of PARP inhibitors [2,3,4,5]. There was no clinically relevant difference in terms of the safety profile when senaparib was administered with or without food. The existing safety data provide evidence for favorable tolerance and an acceptable safety profile for senaparib, which will continue to be monitored in future studies with larger sample sizes and longer treatment durations.
Only male healthy subjects were enrolled in this study, which was one limitation of the study. However, clinical studies in patients with solid tumors suggested that no sex difference exists in the pharmacokinetics of senaparib (data on file). The lack of a clinically meaningful effect of food on the absorption/bioavailability of senaparib in male subjects is likely to be generalizable to female subjects.
5 Conclusions
A high-fat meal slightly increased the absorption of senaparib upon oral administration but the change in total exposure was not considered to be clinically significant. Therefore, senaparib can be taken orally either with or without food.
References
Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434(7035):917–21. https://doi.org/10.1038/nature03445.
US FDA. Lynparza® (olaparib) product insert. 2014. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/208558s014lbl.pdf. Accessed 11 May 2021.
US FDA. Rubraca® (rucaparib) product insert. 2016. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/209115s003lbl.pdf. Accessed 11 May 2021.
US FDA. Zejulatm (niraparib) product insert. 2017. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208447lbl.pdf. Accessed 11 May 2021.
US FDA. Talzenna™ (talazoparib) product insert. 2018. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/211651s000lbl.pdf. Accessed 11 May 2021.
Cai SX, Ma N, Wang X, Jiang Y, Guo M, Hsieh C-Y, et al. Discovery and development of PARP inhibitor senaparib [abstract no. 1399]. Cancer Res. 2022;82(12_Suppl.):1399. https://doi.org/10.1158/1538-7445.Am2022-1399.
Xu B, Cao J, Guo H, Zhang P, Yang S, Zhou Y, et al. Updated analysis of phase 1 dose-escalation and dose cohort expansion studies of senaparib (IMP4297) in Chinese patients with advanced solid tumors [abstract no. 1317]. In: Presented at the ESMO Virtual Congress; 19-21 September 2020.
De Souza P, Gao B, Voskoboynik M, Wilkinson K, Cooper A, Hoon S-N, et al. Updated results of phase 1 study of senaparib (IMP4297) in Australian patients with advanced solid tumors [abstract no. 1338]. In: Presented at the ESMO Virtual Congress; 19-21 September 2020.
Scripture CD, Figg WD. Drug interactions in cancer therapy. Nat Rev Cancer. 2006;6(7):546–58. https://doi.org/10.1038/nrc1887.
China National Medical Products Administration. Drug registration regulation. 2020. Available from: https://www.nmpa.gov.cn/directory/web/nmpa/xxgk/fgwj/bmgzh/20200330180501220.html. Accessed 11 May 2021.
China National Medical Products Administration. Good clinical practice. 2020. Available from: https://www.nmpa.gov.cn/yaopin/ypggtg/20200426162401243.html. Accessed 11 May 2021.
China National Medical Products Administration. Technical guidelines for clinical pharmacokinetics study of chemical medicine. 2005. Available from: https://www.nmpa.gov.cn/xxgk/fgwj/gzwj/gzwjyp/20050318010101201.html. Accessed 11 May 2021.
Shapiro GI, Kristeleit RS, Burris HA, LoRusso P, Patel MR, Drew Y, et al. Pharmacokinetic study of rucaparib in patients with advanced solid tumors. Clin Pharmacol Drug Dev. 2019;8(1):107–18. https://doi.org/10.1002/cpdd.575.
Moore K, Zhang ZY, Agarwal S, Burris H, Patel MR, Kansra V. The effect of food on the pharmacokinetics of niraparib, a poly(ADP-ribose) polymerase (PARP) inhibitor, in patients with recurrent ovarian cancer. Cancer Chemother Pharmacol. 2018;81(3):497–503. https://doi.org/10.1007/s00280-017-3512-5.
Plummer R, Swaisland H, Leunen K, van Herpen CM, Jerusalem G, De Greve J, et al. Olaparib tablet formulation: effect of food on the pharmacokinetics after oral dosing in patients with advanced solid tumours. Cancer Chemother Pharmacol. 2015;76(4):723–9. https://doi.org/10.1007/s00280-015-2836-2.
Acknowledgements
The authors thank the participants who took part in the study, and Molly Yu, PhD and Lawrence Law, MPH from Parexel who provided medical writing assistance funded by IMPACT Therapeutics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by IMPACT Therapeutics and the sponsor was involved in the study design, analysis, and interpretation of the data.
Conflict of interest
Xianmin Meng, Xiaoyan Lin, Rongrong Jiang, Yan Lu, Liyan Zeng, Ming Cao, and Jianliang Zhang have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
The informed consent form and other information available for subjects have been reviewed by the Medical Ethics Committee of Shanghai Public Health Clinical Center. All the modifications of the protocol had been approved by the ethics committee. The design, conduct, and reporting of the study adhered to Good Clinical Practice, Declaration of Helsinki, and current National Medical Products Administration regulations.
Consent to participate
Informed consent was obtained from all the subjects prior to study enrollment.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
XM wrote the manuscript. All authors took part in the collection of data and contributed to the review of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Meng, X., Lin, X., Jiang, R. et al. Effect of Food on the Pharmacokinetics of Senaparib (IMP4297) in Healthy Chinese Subjects. Clin Drug Investig 42, 1009–1016 (2022). https://doi.org/10.1007/s40261-022-01198-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01198-8