Abstract
Omadacycline, a first-in-class aminomethylcycline antibiotic, is approved in the USA as intravenous (IV) and/or oral therapy for treatment of adults with community-acquired bacterial pneumonia (CABP) or acute bacterial skin and skin structure infections (ABSSSI). Phase 1 and 3 studies indicate that omadacycline dose adjustments are not required for any patient group based on age, sex, race, weight, renal impairment, end-stage renal disease, or hepatic impairment. Equivalency of exposure has also been demonstrated for 300 mg oral and 100 mg IV doses. Using an oral loading-dose regimen results in drug exposures exceeding established efficacy targets against the most common CABP and ABSSSI pathogens by Day 2 of treatment, and omadacycline has demonstrated clinical efficacy and is well tolerated. The oral-only dosing regimens provide the potential for treatment of CABP and ABSSSI either within a hospital setting or in the community, which could support earlier hospital discharge and reduced treatment costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical studies of omadacycline indicate that no dose adjustments are needed for any particular group of patients, including those with renal or hepatic impairment. |
By the second day of treatment, levels of omadacycline were above efficacy targets needed for bacterial load reduction or stasis for common bacterial pathogens causing community-acquired bacterial pneumonia (CABP; e.g., Streptococcus pneumoniae) and acute bacterial skin and skin structure infections (ABSSSI; e.g., Staphylococcus aureus). |
The oral-only formulation of omadacycline allows the treatment of CABP and ABSSSI in the community, potentially reducing hospital admissions, hospital stays, and associated costs. |
1 Introduction
Omadacycline is a first-in-class aminomethylcycline antibiotic, approved in the USA for the treatment of adults with community-acquired bacterial pneumonia (CABP) [1] or acute bacterial skin and skin structure infections (ABSSSI) [2, 3]. Studies demonstrate that omadacycline treatment does not require dose adjustment for any patient population [4,5,6]. Omadacycline treatment for CABP and ABSSSI uses different oral loading dose regimens, so there is a need for clarity regarding these different regimens. This short communication aims to provide background on variations in the oral loading dose for omadacycline, expanding on information in the prescribing information [7]. The article also discusses outcomes from pharmacokinetic and Phase 3 registrational studies investigating omadacycline for CABP and ABSSSI.
2 Background on Omadacycline Oral Regimens
Omadacycline is currently approved by the US Food and Drug Administration (FDA) for the treatment of CABP and ABSSSI in adults. Preclinical and clinical data support both indications for intravenous (IV)-to-oral or oral-only dosing regimens [7]. The oral-only dosing regimens include the recent extension to the CABP indication (Table 1). Oral antibiotic options can decrease the need for patients to undergo hospitalization and IV therapy, shorten hospital stays, and therefore decrease the overall economic burden of their infectious disease [8, 9]. Omadacycline loading doses vary by indication, as a result of the study designs used to generate data. The ABSSSI oral loading-dose regimen of 450 mg daily on Days 1 and 2 was FDA approved based on safety and efficacy from a Phase 3 registrational study in patients with ABSSSI, while the CABP loading-dose regimen (300 mg twice on Day 1) was approved based on a pharmacokinetic study demonstrating bioequivalence between IV and oral dosing for patients with CABP [10].
The recently completed oral-only pharmacokinetic study of omadacycline in patients with CABP (ClinicialTrials.gov identifier NCT04160260) supported the FDA’s recent approval of oral-only omadacycline therapy for CABP. This study included 18 participants (in total and in the safety population) who received omadacycline; 14 were included in the pharmacokinetic population after excluding two patients with emesis and two with outlying pharmacokinetic values. All participants received a loading dose of omadacycline (300 mg orally twice on Day 1), followed by maintenance treatment of 300 mg orally once daily (qd), for a total treatment duration of 7–10 days [10]. The loading dose was selected to closely match the reference IV regimen for bioequivalence: 100 mg IV given twice on Day 1, the FDA-approved IV loading dose for both CABP and ABSSSI [1, 2, 7, 10, 11].
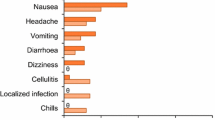
Using the Day 1 plasma concentration profile of 100 mg IV dosing, twice-daily (bid) dosing on Day 1 and qd dosing on Day 2 was simulated using the superposition principle. The analysis showed that oral omadacycline 300 mg provided 100.8% of the total exposure, as measured by area under the concentration-time curve (AUC), achieved with omadacycline 100 mg IV (log geometric mean ratio of AUC0–24: 100.8% [90% confidence interval (CI) 88.0–115.5; Table 2]) [10]. All study participants achieved clinical success for overall clinical response. Furthermore, omadacycline was safe and well tolerated by all participants. Consistent with the established safety profile for omadacycline, the most frequent treatment-emergent adverse events (TEAEs), nausea and vomiting, were mild to moderate in nature, and were not treatment limiting [10]. The study was terminated early because of the COVID-19 pandemic and, therefore, achieved lower enrollment than expected. Results of this study supported the expanded FDA label to include an oral-only regimen for CABP.
3 Pharmacokinetics of Omadacycline
Pharmacokinetics of omadacycline include peak concentrations (Cmax) that increase proportionally to dose administered, over a certain range (Cmax ranges from 548 ng/mL after a single oral dose of 300 mg omadacycline to 1077 ng/mL at steady state [Day 5] of 450 mg qd) [7]. Regardless of the omadacycline dose (300 or 450 mg orally), the median time to maximum plasma concentration (Tmax) is 2.5–3.0 h [11] and the half-life is 15.5–16.8 h [12,13,14]. Omadacycline absorption is rapid, with peak radioactivity between 1 and 4 h in plasma or blood. Steady-state AUC with 300 mg oral omadacycline is 11,156 ng × h/mL. Omadacycline exhibits high clearance (CL/F, 34.6 L/h for a single dose of 300 mg oral omadacycline) and volume of distribution (Vz/F 794 L for a single dose of 300 mg oral omadacycline), with no plasma metabolites [7]. Previous studies have shown that there was no significant interaction of omadacycline with a broad range of membrane transporters, suggesting that drug–drug interactions based on the inhibition or induction of human drug transporter activity are unlikely with omadacycline when given at therapeutic concentrations [7, 14]. The bioavailability of oral omadacycline is 34.5%; omadacycline is not metabolized, and oral omadacycline is primarily eliminated in the feces [4, 7, 11, 15]. Previous Phase 1 and Phase 3 studies of omadacycline showed that no dose adjustments are necessary for any patient group, such as people with hepatic or renal impairment, including end-stage renal disease (ESRD) and those receiving dialysis [4, 6, 13]; dose adjustments are also unnecessary by body mass index [13, 16, 17] or older age [1].
General pharmacokinetic principles suggest that drug concentrations reach steady state within 4–5 half-lives. Given that the half-life for omadacycline is ~ 16 h, one may estimate that, without a loading dose, steady state would be achieved on Days 3–4 [13]. In an effort to achieve therapeutic concentration by Day 2, loading doses of omadacycline were utilized in the clinical development program.
4 Pharmacodynamics of Omadacycline
The pharmacodynamic measurement most associated with the antibacterial effect of omadacycline is total exposure (time × concentration) above the minimum inhibitory concentration (MIC) for the bacteria [7, 13, 18]. Omadacycline oral-only dosing can achieve and exceed the necessary exposure needed for common pathogens in CABP and ABSSSI regardless of the loading-dose regimen used [19,20,21] (Tables 2 and 3). The dose justification for omadacycline is supported by a robust population pharmacokinetic model developed using data obtained throughout the omadacycline clinical development program and incorporates key pathogens' MIC distributions from surveillance studies [22], non-clinical exposure targets for efficacy [23, 24], and clinical outcomes from patients [19, 20]. For example, given MIC90 values of 0.12 and 0.25 mg/L for omadacycline against Streptococcus pneumoniae and Staphylococcus aureus, respectively, including drug-resistant strains, the omadacycline exposure achieved with an approved oral-only regimen (AUC0-24h ~ 11,000 ng × h/mL) would exceed established efficacy targets (S. pneumoniae: median target for 1-log10 reduction = 17.4; S. aureus: median target for stasis = 21.9) [22,23,24]. The favorable pharmacodynamic parameters combined with the low MIC90 values of bacteria that commonly cause CABP and ABSSSI make target concentrations of omadacycline easily achievable when using it to treat patients, whether it is given orally or IV.
5 Omadacycline Oral Loading Dose Exposures (AUC) Profiles
As shown in Tables 2 and 3, either loading-dose regimen provides similar exposure to the reference IV loading dose used in the Phase 3 registration trials for CABP and ABSSSI [1,2,3, 7, 10]. The most common TEAEs across Phase 3 clinical trials were nausea and vomiting. These most frequently occurred when patients received 450 mg orally, and resolved or were seen at similar rates to comparators when patients transitioned to a 300 mg maintenance dose [2, 3, 25].
A notable difference between the two oral loading-dose regimens is the need to fast twice on Day 1 when 300 mg bid is utilized, versus fasting once when 450 mg qd is administered (fasting, per label instructions, is defined as no food or drink [except for water] for 4 h before and 2 h after oral dosing).
6 Clinical Relevance
The clinical results from Phase 3 studies of omadacycline bore out the expectations, based on pharmacokinetic and pharmacodynamic data for omadacycline, in treating both CABP and ABSSSI. Clinical efficacy (investigator-assessed clinical response at post-treatment evaluation) was 87.6% for omadacycline versus 85.1% for moxifloxacin in CABP (p = NS) [1], 86.1% for omadacycline versus 83.6% for linezolid in one study of ABSSSI (p = NS) [2], and 84.2% for omadacycline versus 80.8% for linezolid in a second study of ABSSSI (p = NS) [3].
7 Conclusions
The results of several Phase 1 and Phase 3 studies indicate that omadacycline treatment met the expectations in treating both CABP and ABSSSI, with omadacycline demonstrating more than 80% clinical efficacy in all Phase 3 studies. Furthermore, omadacycline does not require any dose adjustments for patients based on age, sex, race, weight, renal impairment, ESRD, or hepatic impairment. In all three Phase 3 studies, adverse events seen with omadacycline were generally tolerable, and similar in frequency and severity to those seen with comparator antibiotics. Additionally, the available oral loading-dose regimens provide drug exposures by Day 2 that exceed established efficacy targets for the most common pathogens for CABP and ABSSSI and are efficacious and well tolerated [25]. The availability of an efficacious oral-only antibiotic for CABP and ABSSSI provides an additional therapeutic option, regardless of whether a patient needs to be treated in a hospital or in the community. This could also facilitate IV-to-oral transition, potentially enabling outpatient therapy or earlier hospital discharge, thus reducing hospitalization and overall costs [8, 26].
References
Stets R, Popescu M, Gonong JR, Mitha I, Nseir W, Madej A, et al. Omadacycline for community-acquired bacterial pneumonia. N Engl J Med. 2019;380(6):517–27. https://doi.org/10.1056/NEJMoa1800201.
O’Riordan W, Green S, Overcash JS, Puljiz I, Metallidis S, Gardovskis J, et al. Omadacycline for acute bacterial skin and skin-structure infections. N Engl J Med. 2019;380(6):528–38. https://doi.org/10.1056/NEJMoa1800170.
O’Riordan W, Cardenas C, Shin E, Sirbu A, Garrity-Ryan L, Das AF, et al. Once-daily oral omadacycline versus twice-daily oral linezolid for acute bacterial skin and skin structure infections (OASIS-2): a phase 3, double-blind, multicentre, randomised, controlled, non-inferiority trial. Lancet Infect Dis. 2019;19(10):1080–90. https://doi.org/10.1016/S1473-3099(19)30275-0.
Berg JK, Tzanis E, Garrity-Ryan L, Bai S, Chitra S, Manley A, et al. Pharmacokinetics and safety of omadacycline in subjects with impaired renal function. Antimicrob Agents Chemother. 2018;62(2):e02057-e2117. https://doi.org/10.1128/AAC.02057-17.
Gallagher JC. Omadacycline: a modernized tetracycline. Clin Infect Dis. 2019;69(suppl 1):S1-5. https://doi.org/10.1093/cid/ciz394.
Kovacs SJ, Ting L, Praestgaard J, Sunkara G, Sun H, Stein DS, et al. An open-label study of the impact of hepatic impairment on the pharmacokinetics and safety of single oral and intravenous doses of omadacycline. Antimicrob Agents Chemother. 2020;64(1):e01650-e1720. https://doi.org/10.1128/AAC.01650-20.
NUZYRA [prescribing information]. King of Prussia, PA: Paratek Pharmaceuticals, Inc. May 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/209816s011,209817s010lbl.pdf. Accessed 5 Aug 2021.
Lodise T, LaPensee K. Cost-saving opportunities with an oral and intravenous once-daily aminomethylcycline antibiotic for community-acquired bacterial pneumonia: Findings from decision-analytic models. Am Health Drug Benefits. 2019;12(4):168–76.
Lodise TP, Van Le H, LaPensee K. Hospital admission patterns in adult patients with community-acquired pneumonia who received ceftriaxone and a macrolide by disease severity across United States hospitals. Antibiotics (Basel). 2020;9(9):577. https://doi.org/10.3390/antibiotics9090577.
ClinicalTrials.gov. Study to Evaluate the PK of PO Omadacycline in Adults With Community-Acquired Bacterial Pneumonia. NCT 04160260. https://www.clinicaltrials.gov/ct2/show/results/NCT04160260. Updated 3 November 2021. Accessed 1 Dec 2021.
Lakota EA, Van Wart SA, Trang M, Tzanis E, Bhavnani SM, Safir MC, et al. Population pharmacokinetic analyses for omadacycline using Phase 1 and 3 data. Antimicrob Agents Chemother. 2020;64(7):e02263-e2319. https://doi.org/10.1128/AAC.02263-19.
Bundrant LA, Tzanis E, Garrity-Ryan L, Bai S, Chitra S, Manley A, et al. Safety and pharmacokinetics of the aminomethylcycline antibiotic omadacycline administered to healthy subjects in oral multiple-dose regimens. Antimicrob Agents Chemother. 2018;62(2):e01487-e1517. https://doi.org/10.1128/AAC.01487-17.
Rodvold KA, Pai MP. Pharmacokinetics and pharmacodynamics of oral and intravenous omadacycline. Clin Infect Dis. 2019;69(suppl 1):S16-22. https://doi.org/10.1093/cid/ciz309.
Flarakos J, Du Y, Gu H, Wang L, Einolf HJ, Chun DY, et al. Clinical disposition, metabolism and in vitro drug–drug interaction properties of omadacycline. Xenobiotica. 2016;47(8):682–96. https://doi.org/10.1080/00498254.2016.1213465.
Sun H, Ting L, Machineni S, Praestgaard J, Kuemmell A, Stein DS, et al. Randomized, open-label study of the pharmacokinetics and safety of oral and intravenous administration of omadacycline to healthy subjects. Antimicrob Agents Chemother. 2016;60(12):7432–5. https://doi.org/10.1128/AAC.01393-16.
Pai MP, Wilcox MH, Chitra S, McGovern PC. Safety and efficacy of omadacycline by BMI categories and diabetes history in two Phase III randomized studies of patients with acute bacterial skin and skin structure infections. J Antimicrob Chemother. 2021;76(5):1315–22. https://doi.org/10.1093/jac/dkaa558.
Pai MP, Wilcox M, Chitra S, McGovern P. Safety and efficacy of omadacycline by body mass index in patients with community-acquired bacterial pneumonia: subanalysis from a randomized controlled trial. Respir Med. 2021;184: 106442. https://doi.org/10.1016/j.rmed.2021.106442.
Ambrose PG, Bhavnani SM, Rubino CM, Louie A, Gumbo T, Forrest A, et al. Pharmacokinetics–pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis. 2007;44(1):79–86. https://doi.org/10.1086/510079.
Bhavnani SM, Hammel JP, Lakota EA, Bader JC, Bulik CC, VanScoy BD, et al. Pharmacokinetic-pharmacodynamic target attainment analyses evaluating omadacycline dosing regimens for the treatment of patients with community-acquired bacterial pneumonia for Streptococcus pneumoniae and Haemophilus influenzae. In: Presented at the American Society for Microbiology Annual Microbe Meeting. Atlanta, GA; June 7–11, 2018: Poster Sa625.
Bhavnani SM, Hammel JP, Lakota EA, Liolios K, Rubino CM, Steenbergen JN, et al. Assessment of pharmacokinetics-pharmacodynamics to support omadacycline dosing regimens for the treatment of patients with acute bacterial skin and skin structure infections. In: Presented at the 29th European Congress of Clinical Microbiology and Infectious Diseases. Amsterdam, Netherlands; April 13–16, 2019: Poster P1944.
Friedrich L, Curran M, Chitra S, Manley A, Bai S, Noble B, et al. Modeling the pharmacokinetics and pharmacodynamics of intravenous and oral omadacycline with and without a loading dose. In: Presented at IDWeek 2019. Washington, DC; October 2–6, 2019: Poster 734.
Pfaller MA, Huband MD, Shortridge D, Flamm RK. Surveillance of omadacycline activity tested against clinical isolates from the United States and Europe: report from the SENTRY Antimicrobial Surveillance Program, 2016 to 2018. Antimicrob Agents Chemother. 2020;64(5):e02488-e2519. https://doi.org/10.1128/AAC.02488-19.
Lepak AJ, Zhao M, Marchillo K, VanHecker J, Andes DR. In vivo pharmacodynamic evaluation of omadacycline (PTK 0796) against Streptococcus pneumoniae in the murine pneumonia model. Antimicrob Agents Chemother. 2017;61(5):e02368-e2416. https://doi.org/10.1128/AAC.02368-16.
Lepak AJ, Zhao M, Marchillo K, VanHecker J, Andes DR. In vivo pharmacodynamics of omadacycline against staphylococcus aureus in the neutropenic murine thigh infection model. Antimicrob Agents Chemother. 2019;63(7):e00624-e719.
Opal S, File TM Jr, van der Poll T, Tzanis E, Chitra S, McGovern PC. An integrated safety summary of omadacycline, a novel aminomethylcycline. Clin Infect Dis. 2019;69(suppl 1):S40-47. https://doi.org/10.1093/cid/ciz398.
Zhanel GG, Esquivel J, Zelenitsky S, Lawrence CK, Adam HJ, Golden A, et al. Omadacycline: a novel oral and intravenous aminomethylcycline antibiotic agent. Drugs. 2020;80(3):285–313. https://doi.org/10.1007/s40265-020-01257-4.
Acknowledgments
Medical editorial assistance, funded by Paratek Pharmaceuticals, Inc., was provided by Megan Breuer, PhD, CMPP and Jenny Engelmoer, PhD of Innovative Strategic Communications (Milford, PA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This article was funded by Paratek Pharmaceuticals, Inc.
Conflict of interest
IL has no financial disclosures. MA-G is an employee and shareholder of Paratek Pharmaceuticals, Inc.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
Both authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leviton, I.M., Amodio-Groton, M. Omadacycline Oral Dosing and Pharmacokinetics in Community-Acquired Bacterial Pneumonia and Acute Bacterial Skin and Skin Structure Infection. Clin Drug Investig 42, 193–197 (2022). https://doi.org/10.1007/s40261-022-01119-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-022-01119-9