Abstract
Background and Objectives
Entospletinib is a selective, reversible, adenosine triphosphate-competitive small-molecule spleen tyrosine kinase (SYK) inhibitor that blocks B cell receptor-mediated signaling and proliferation in B lymphocytes. This study evaluated the safety, pharmacokinetics, and pharmacodynamics of entospletinib in a double-blind, single/multiple ascending dose study in healthy volunteers.
Methods
In sequential cohorts, 120 subjects received entospletinib (25–1200 mg; fasted) as single or twice-daily oral doses for 7 days. Along with pharmacokinetics, the study assessed functional inhibition of ex vivo anti-immunoglobulin E-stimulated CD63 expression on basophils and pervanadate-evoked phosphorylated SYK (pSYK) Y525. Safety and tolerability were assessed throughout the study.
Results
Entospletinib was generally well-tolerated over a 48-fold dose range. Adverse events (AEs) were generally mild to moderate, with no AE-driven study drug discontinuations noted. Entospletinib displayed a median plasma half-life of 9–15 h; entospletinib exposures reached a plateau at ≥600 mg twice daily (likely due to solubility-limited absorption) and provided >90% CD63 inhibition at peak concentrations and >60% inhibition at trough concentrations (corresponding pSYK inhibition of >70 and >50%).
Conclusion
The overall safety, pharmacokinetics, and pharmacodynamics profiles of entospletinib support further clinical evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Entospletinib is a selective oral inhibitor of spleen tyrosine kinase (SYK) that has been linked to the pathogenesis of a variety of B cell malignancies, including chronic lymphocytic leukemia and various subtypes of non-Hodgkin’s lymphoma. |
When administered in single or multiple oral doses in healthy adults, entospletinib monotherapy is generally well-tolerated. |
Entospletinib displays a median plasma half-life of 9–15 h; exposures plateau at ≥600 mg twice-daily doses, which provides >50% coverage at trough concentrations (based on CD63/phosphorylated SYK biomarker assessment). |
1 Introduction
Spleen tyrosine kinase (SYK) is a non-receptor, cytoplasmic protein tyrosine kinase that is predominantly expressed in cells of hematopoietic lineage. It is an important mediator of immunoreceptor signaling in macrophages, neutrophils, mast cells, and B cells.
In B lymphocytes, antigen-mediated stimulation of the B cell receptor (BCR) results in the recruitment and phosphorylation of various kinases, including SYK. Phosphorylation of SYK (pSYK) leads to the activation and amplification of downstream receptor signaling and likely plays a role in chemokine signaling and cellular responses such as proliferation, survival, differentiation, and apoptosis [1, 2].
Uncontrolled BCR signaling via SYK has been implicated in the pathogenesis of several common B cell malignancies, including chronic lymphocytic leukemia (CLL), diffuse large B cell lymphoma (DLBCL), follicular lymphoma (FL), mantle cell lymphoma (MCL), marginal zone lymphoma, and B-lineage acute lymphoblastic leukemia. Given the vital role of SYK in BCR signaling, inhibitors of SYK activity are an attractive therapeutic option for hematopoietic B cell lymphomas and other non-Hodgkin’s lymphoma histologies, where SYK inhibition would prevent BCR-mediated signaling and therefore prevent the uncontrolled growth of lymphoma cells [3, 4].
A number of molecules targeting the SYK pathway for allergic, autoimmune, and neoplastic disorders are currently in various stages of development. These include adenosine triphosphate (ATP)-binding site inhibitors (fostamatinib, CG14979, and P505-15), P-site inhibitors (C-61), antisense oligonucleotides, and small-interfering RNAs [5].
Clinical investigation of fostamatinib, the prodrug of SYK inhibitor R406, in B cell malignancies demonstrated responses in CLL/small lymphocyte leukemia (overall response rate [ORR] 55%), DLBCL (ORR 22%), MCL (ORR 11%), and FL (ORR 10%) following doses of 200 or 250 mg twice daily. Reported toxicities included diarrhea, nausea, hypertension, cytopenias, and fatigue, which limited dosing and have been partially attributed to off-target effects, including the inhibition of multiple kinases in addition to SYK [6].
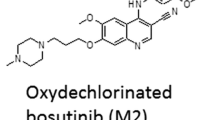
Entospletinib (GS-9973) is a highly selective and oral SYK inhibitor and is currently undergoing clinical evaluation for autoimmune and oncology indications. Entospletinib is an ATP-competitive inhibitor of SYK that disrupts kinase activity with a half-maximal inhibitory concentration (IC50) of 7.6 nmol/L. A phase II study involving entospletinib 800 mg twice-daily oral administration in subjects with relapsed or refractory CLL (n = 41) showed a progression-free survival (PFS) rate of 70.1% (at 24 weeks), median PFS of 13.8 months, and an ORR of 61.0%. The most common treatment-emergent serious adverse events (AEs) included dyspnea, pneumonia, febrile neutropenia, dehydration, and pyrexia. Common Grade 3/4 laboratory abnormalities included neutropenia and reversible alanine aminotransferase/aspartate aminotransferase elevations. Overall, entospletinib demonstrated clinical activity in subjects with relapsed or refractory CLL with acceptable toxicity [7].
This paper reports the results of the first-in-human (FIH) study conducted to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of entospletinib in healthy volunteers following single- and multiple-dose oral administration. The data from this study provided the basis for subsequent testing of the safety and efficacy of entospletinib in cancer patients.
Further, this paper describes entospletinib pharmacokinetics following multiple-dose administration (doses of 100–1200 mg twice daily) under fed conditions across additional healthy volunteer studies.
2 Methods
2.1 Ethics
All study protocols were reviewed and approved by the local institutional review boards (all studies were conducted at Algorithme Pharma, Inc., Laval, QC, Canada). The studies were conducted in accordance with recognized international scientific and ethical standards, including but not limited to the International Conference on Harmonization guideline for Good Clinical Practice and the original principles embodied in the Declaration of Helsinki. These standards are consistent with the requirements of the US Code of Federal Regulations Title 21, Part 312 (21CFR312) and the European Community Directive 2001/20/EC. Written informed consent was obtained from all participants.
2.2 Study Design
The FIH study was a phase I, randomized, double-blind, placebo-controlled, single and multiple dose-escalation study, involving an oral tablet formulation of the mono-mesylate salt of entospletinib. Subjects received either single or multiple doses of entospletinib (or placebo) under fasted conditions (Table 1). The study cohorts were enrolled in a staggered fashion; single-dose cohorts were escalated after review of the safety/pharmacokinetic data, allowing at least 1 week between cohorts, and multiple-dose cohorts were initiated/escalated after review of safety/pharmacokinetics from the single-dose cohorts (up to 200 mg) (Electronic Supplementary Material Fig. S1).
Additionally, open-label, multiple-cohort, multiple-dose studies were conducted that evaluated the pharmacokinetics of entospletinib under fed conditions, i.e., co-administration with a standard meal of ~400–500 calories with ~10–13 g of fat (Table 1).
2.3 Subjects
Healthy male and non-pregnant, non-lactating female subjects aged 18–45 years (inclusive) who were ≥45 kg in weight and had a body mass index between 19 and 30 kg/m2 were eligible to participate in the FIH study. Similar inclusion criteria were used for the fed studies, except that the eligible enrollment age was increased to 60 years.
In all studies, subjects were required to be free of clinically significant disease or any condition that could jeopardize subject safety or study validity as determined through the subjects’ medical history, physical examination, 12-lead electrocardiogram (ECG), and results from clinical laboratory tests that were performed within 2 weeks prior to the baseline visit (day 0). Prior to enrollment in the study, all subjects provided informed written consent. Subjects were ineligible for the studies if they had used any investigational drug and/or participated in any clinical trial within 1 month of the first entospletinib administration. Use of medications, including over-the-counter medications or herbal products, was not allowed within 1 week of commencing study drug dosing. Vitamins, acetaminophen, hormone replacement therapy, and/or oral contraceptives were allowed.
2.4 Safety Assessments
Safety was evaluated by assessment of clinical laboratory tests (hematology profile, chemistry profile, and urinalysis), physical examinations, vital signs, serum pregnancy tests (for female subjects), 12-lead safety ECGs, and review of concomitant medications performed at screening, at baseline (the day before the first study dose), on days before pharmacokinetic blood sampling, and at various times during the study. Subjects were monitored for AEs from baseline to the follow-up visit. AEs were rated as Grade 1 = mild, Grade 2 = moderate, Grade 3 = severe, and Grade 4 = life-threatening, according to the Gilead Sciences’ Modified National Institute of Allergy and Infectious Diseases (NIAID) Common Toxicity Grading Scale. Clinical and laboratory AEs were coded (system organ class, high-level group term, high-level term, preferred term, and lower-level term) using the Medical Dictionary for Regulatory Activities (MedDRA®) Version 15.0.
2.5 Pharmacokinetic Sampling
Serial blood samples were collected pre-dose and over a 12-, 24-, or 48-h period following single or multiple dosing for assessing the pharmacokinetics of entospletinib across all studies (Table 1).
2.6 Pharmacodynamic Sampling
Serial blood samples for pharmacodynamics assessment were collected pre-dose and over a 48-h period following single or multiple dosing in the FIH study. Whole-blood samples were utilized for the analysis. The samples were refrigerated (2–8 °C) immediately post collection and stored for up to 24 h. Samples were analyzed within 12 h of blood collection.
2.7 Bioanalytical Procedures
Entospletinib plasma concentrations were determined with a validated high-performance liquid chromatography/tandem mass spectrometry (MS/MS) bioanalytical assay (Covance®, Madison, WI, USA) [8]. A 50 µL aliquot of plasma sample was mixed with internal standard and reconstituted with water/acetonitrile at 50:50 (v:v) followed by a liquid/liquid extraction procedure using methyl tert-butyl ether. Chromatography was performed using a Synergi™ Polar-RP column (Phenomenex, Torrance, CA, USA), with mobile phases consisting of formic acid in water and formic acid in acetonitrile at a flow rate of 0.6 mL/min. The MS/MS precursor ion → product ion transition was m/z 412.2 → m/z 105.1 for entospletinib. The assay calibration curves were linear, from 1 to 1000 ng/mL (R 2 = 0.9070, intercept = 0.000038). Samples were diluted and re-analyzed if the concentrations exceeded the curve range.
Dilution quality control (QC) samples were included, at least in duplicate, for each analytical batch containing samples requiring dilution. These QC samples were diluted with blank matrix to the same extent as the most highly diluted sample. At least one-half of the dilution QC samples had to be within the range of 85.0–115.0% of theoretical for the results of diluted samples to be accepted. The inter-assay precision range (% relative standard deviation) was 2.5–5.6, and the inter-assay accuracy range (% relative error) was −3.2 to 4.3. The stability in frozen matrix was 91 days at −10 to −30 °C and 343 days at −60 to −80 °C.
2.8 Pharmacodynamic Procedures
2.8.1 CD63 Assay
CD63 surface expression on human whole-blood basophils was measured using a BasoTest™ Kit (Orpegen Pharma, Heidelberg, Germany). Briefly, heparinized blood was incubated at 37 °C. Following the incubation, 20 μL of potentiation buffer B from the BasoTest™ Kit was added to each well and incubated for an additional 10 min at 37 °C. Subsequently, the Fcɛ receptor (FcɛR) was crosslinked by the addition of 100 μL of anti-immunoglobulin E (anti-IgE) to a final concentration of 10 μg/mL and incubated for 20 min at 37 °C. Degranulation was arrested by placing the plate on ice for 5 min. Cells were stained with 20 μL of a staining cocktail, containing CD123-PE/CD63-FITC/HLA-DR-PerCP and incubated for 20 min on ice. A total of 2 mL of red cell lysis buffer (Buffer G from the BasoTest™ Kit) was added to each well, mixed thoroughly, and incubated at room temperature for 10 min. The plate was centrifuged and the supernatant discarded. The cell pellet was washed with 2 mL of washing solution (Buffer A from the BasoTest™ Kit), and the centrifugation was repeated. The cells were re-suspended in buffer A and kept on ice in a 250 μL 96-well U-bottom plate until read by multicolor flow cytometry on a BD™ FACS LSR II (Becton, Dickinson and Company, Franklin Lakes, NJ, USA).
Fluorescence-activated cell sorter (FACS) sampling of 100,000 total events was collected using a high-throughput screen autosampler. FACS data were collected and CD123+/human leukocyte antigen–antigen D related negative (HLA-DR−) basophils were gated. The percentages of CD63+ cells in this population were recorded for each well. Electronic Supplementary Material Fig. S2 provides a representative scatter plot of the CD63+ assay and gate strategy.
2.8.2 Phosphorylated Spleen Tyrosine Kinase (Y525) Assay
Heparinized blood was incubated in a 96-deep well V-bottom plate for 1 h at 37 °C. Following the incubation, 10 μL of 6 mmol/L pervanadate was added to each well and incubated for an additional hour at 37 °C. Subsequently, 750 μL of phosphate-buffered saline was added to each well and immediately centrifuged at 3300 rpm for 3 min at room temperature. The supernatant was removed with a 96-well block aspirator (V&P Scientific, Inc., San Diego, CA, USA). The wash step was repeated and supernatant was discarded. The cell pellet was placed on ice and 75 μL of ice-cold 2X cell lysis buffer was added, mixed immediately, and kept on ice for 30 min prior to being transferred to 96-well polymerase chain reaction plates and stored frozen until use. Mesoscale (MSD) chemiluminescent capture plates were prepared by adding 5 μL of 2 ng/μL N-19 total SYK antibody diluted in Tris-buffered saline (TBS) to a 96-well goat anti-rabbit small spot plate. The plate was incubated for 1 h at room temperature. Each well was blocked with 25 μL of blocker buffer containing 5% rabbit serum for 1 h with shaking on an orbital shaker. Prior to use, the blocker buffer was decanted and the wells were washed with 200 μL of TBS + 0.2% Tween-20 (TBST). The wash was decanted, and 25 μL of the whole-blood lysate was added to each well. The plate was placed on an orbital shaker for 1 h at room temperature; the supernatant was then decanted into a 10% bleach solution and the plate was washed twice with 200 μL TBST. An antibody cocktail was prepared with anti-pSYK (Y525) biotinylated antibody (1:1000) plus streptavidin sulfo-tagged reagent (1:1000) in blocker buffer containing 5% rabbit serum. A total of 25 µL was added to each well and incubated on an orbital shaker for 1 h at room temperature. The wells were decanted and washed once with 200 μL TBST. Again, the wells were decanted, and 150 μL of read buffer was added and read immediately on the MSD instrument. MSD data were collected, and electrochemiluminescence readings were recorded for each well.
2.9 Pharmacokinetic Analysis
The pharmacokinetic parameters of entospletinib were assessed by non-compartmental methods using a non-linear curve-fitting software package (Phoenix® WinNonlin® Professional, Pharsight® Corporation, Mountain View, CA, USA). The following pharmacokinetic parameters were evaluated for entospletinib: C max (the maximum observed concentration of the drug), t max (the time [observed timepoint] of C max), t ½ (the estimate of the terminal elimination half-life of the drug; calculated by dividing the natural log of 2 by the terminal elimination rate constant [λz; which is estimated by linear regression of the terminal elimination phase of the concentration of drug versus time curve]), AUClast (area under the plasma concentration–time curve [AUC] from time zero to the time of the last quantifiable concentration), AUC∞ (AUC extrapolated to infinity; calculated as AUClast + C last/λz [the last observed quantifiable concentration of the drug in plasma divided by λz]) (single dose), AUCτ (AUC over the dosing interval [τ]), and C trough (concentration at the end of the dosing interval) (multiple dose).
2.10 Pharmacodynamic Analysis
The blood pharmacodynamic measurements conducted for entospletinib in the FIH study included the number of CD63+ basophils and pSYK (Y525). The changes in CD63+ and pSYK (Y525) expression versus time profiles were assessed by calculating the following pharmacodynamic parameters: percentage CD63+ basophils and percentage pSYK (Y525), reported as normalized to baseline/pre-dose values.
2.11 Statistical Methods
An evaluable pharmacokinetics population (subjects who completed at least one pharmacokinetics sampling session and for whom pharmacokinetic parameters could be calculated), safety population (subjects who received at least one dose of entospletinib), and pharmacodynamics population (subjects who received at least one dose of entospletinib and had specific laboratory data available for calculating estimates of pharmacodynamic parameters) were identified for this study. Pharmacokinetics, pharmacodynamics, and safety analyses were conducted based on the corresponding evaluable population.
3 Results
3.1 Subject Demographics
A total of 184 healthy subjects were enrolled and analyzed for this report. The majority of healthy subjects were male, white, and of non-Hispanic/Latino ethnicity. The demographics and other baseline characteristics are shown in Table 1.
3.2 Safety and Tolerability
Safety results are presented for both the FIH and fed studies (Table 2). Overall, entospletinib monotherapy was generally well-tolerated when administered as a single dose or in multiple doses. No discontinuations due to treatment-related AEs were reported for the FIH study, but two subjects in the fed studies (Grade 3 urticaria and moderate urinary tract infection) discontinued. The majority of AEs were mild or moderate in severity, with no Grade 4 severity events. No apparent dose response was observed with any AE in either the single- or multiple-dose cohorts. The majority of graded laboratory abnormalities were Grade 1 severity. No subjects experienced serious AEs attributed to the study drug. No deaths were reported.
3.3 Pharmacokinetics of Entospletinib
3.3.1 Single Dose
The plasma concentration–time profiles of single oral doses of entospletinib 25, 75, 200, 600, 900, and 1200 mg under fasted conditions are illustrated in Fig. 1. A summary of the pharmacokinetic parameters following single-dose administration is presented in Table 3. Entospletinib was rapidly absorbed, generally achieving C max within 2–3 h after administration for all doses. After attaining C max, entospletinib plasma concentrations declined with a t ½ of approximately 9 h at doses ≥200 mg. The exposures following entospletinib 200 mg increased in a greater-than-dose-proportional manner compared with those following 75 mg. The exposure increase from 600 to 1200 mg was less than dose proportional.
3.3.2 Multiple Doses
The plasma concentration–time profiles of entospletinib following administration of multiple (twice-daily) oral doses of 25, 75, 200, 600, 900, and 1200 mg in healthy volunteers under fasted conditions are presented in Fig. 2. A summary of the corresponding steady-state (day 7) pharmacokinetic parameters is presented in Table 4. Following 7 days of multiple dosing, there was an approximate 2- to 4-fold increase in entospletinib exposure (C max and AUC) on day 7 compared with day 1 (Table 4). Following C max (~2–3 h post-dose), plasma concentrations declined with a t ½ of approximately 9 h at doses ≤200 mg twice daily and approximately 14 h at doses >200 mg twice daily. Steady-state concentrations were achieved after 3–4 days with twice-daily dosing, which is consistent with the estimated t ½. Entospletinib steady-state exposures increased with increasing doses, ranging from 25 to 600 mg twice daily. Similar to single-dose data, at doses greater than 600 mg the entospletinib exposure increases were less than dose proportional, suggesting that exposure was approaching a plateau.
3.4 Effect of Food
Entospletinib pharmacokinetics were also evaluated following multiple (twice-daily) dosing of entospletinib 100, 200, 600, 900, and 1200 mg under fed conditions. A summary of the corresponding steady-state pharmacokinetic parameters under fed conditions is presented in Table 5. Absorption of entospletinib under fed conditions was slower than in the fasted state, with C max attained within 4 h after administration (vs. 2 h under fasted conditions). Entospletinib exposures increased with increasing doses without any apparent exposure plateau, unlike exposures in fasted conditions. At a given dose level, entospletinib exposure was generally lower following fed versus fasted administration.
3.5 Pharmacodynamics of Entospletinib
The effect of entospletinib on inhibition of ex vivo anti-IgE-stimulated cell-surface CD63 expression in basophils after single dosing is illustrated in Electronic Supplementary Material Fig. S3 and multiple dosing (fasted) is illustrated in Fig. 3. Overall, inhibition of cell surface CD63 expression (expressed as percentage of baseline) increased with doses of entospletinib from 25 to 600 mg following single- or multiple-dose administration. For doses ≥600 mg twice daily, the maximal mean inhibition of CD63 expression peaked at 2–4 h post-dose at ≥86% inhibition, with ≥63% inhibition being maintained at C trough (i.e., 12 h post-dose). The maximal mean inhibition of CD63 expression was comparable between entospletinib 600, 900, and 1200 mg twice daily.
Electronic Supplementary Material Fig. S4 illustrates the effect of entospletinib on inhibition of pervanadate-evoked pSYK-Y525 after single dosing and Fig. 4 illustrates multiple dosing (fasted). The baseline levels of pSYK are shown in Electronic Supplementary Material Fig. S5. Overall, there was increasing inhibition of pSYK expression (expressed as percentage of baseline) with entospletinib doses of 25–600 mg following single- or multiple-day (twice-daily) administration. For doses ≥600 mg twice daily, the maximal mean inhibition of pSYK expression peaked at 4–5 h post-dose at ≥72% inhibition, with ≥54% inhibition being maintained at C trough (i.e., 12 h post-dose). The maximal mean inhibition of pSYK expression was comparable between entospletinib 600, 900, and 1200 mg twice daily.
Mean (±standard deviation) inhibition of phosphorylated spleen tyrosine kinase pharmacodynamics on day 7 (pharmacokinetic steady state) following multiple oral doses of entospletinib under fasted conditions. Pre-dose phosphorylated spleen tyrosine kinase pharmacodynamic values are considered as baseline. pSYK phosphorylated spleen tyrosine kinase
Figure 5 illustrates the exposure–response relationship between entospletinib concentrations and inhibition of CD63 expression and pSYK (represented as percentage of baseline). Entospletinib inhibited both of these parameters in a concentration-dependent manner with a median effective concentration (EC50) of 429 and 110 ng/mL for inhibition of CD63 and pSYK, respectively.
4 Discussion
Entospletinib is a potent, highly selective, oral, small-molecule inhibitor of SYK that is being developed for the treatment of hematological malignancies. Entospletinib has greater than 14-fold selectivity for SYK versus other kinase targets [8], and hence has the potential for an improved efficacy and safety profile in patients versus other SYK inhibitors [5]. This paper reports the results of the FIH study conducted to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of entospletinib in healthy volunteers following single- and multiple-dose oral administration under fasted conditions. Additionally, safety, tolerability, and pharmacokinetics following entospletinib co-administration with food are presented.
Following single and multiple oral administration of entospletinib under fasted conditions, entospletinib concentrations showed a bi-exponential decline. Based on a terminal t ½ of ~9 h, entospletinib is suitable for a twice-daily dosing regimen. Entospletinib exposures increased in a less-than-dose-proportional manner at doses >200 mg, with exposures reaching a plateau at >600 mg twice daily. The solubility of entospletinib administered as a mono-mesylate salt is highly pH-dependent: its aqueous solubility is 3 mg/mL in pH 2 buffer but <0.001 mg/mL at pH ≥3.0. As such, the absorption of entospletinib may be limited, particularly at high-dose levels, due to the pH-dependent solubility as it transits through the intestine during absorption and thus may explain the plateau in entospletinib exposures.
Further, there was an approximate 3- to 4-fold increase in entospletinib exposures following multiple doses that was greater than expected (~2-fold), given an average 9-h t ½. Given a slight increase in t ½ between single and multiple doses, the accumulation may not be completely attributed to a non-linear systemic clearance mechanism (e.g., hepatic auto-inhibition), but is also likely due to increased extent of entospletinib absorption (e.g., auto-inhibition of intestinal metabolism/transport). Similar non-linear accumulation following multiple doses has been reported for other molecules (e.g., nefazodone; non-linear accumulation attributed to auto-inhibition of pre-systemic metabolism) [9]. Additional studies to characterize the disposition of entospletinib via metabolic/transporter-mediated pathways, and non-linear mixed-effects modeling-based population pharmacokinetic analyses are ongoing to elucidate the mechanism.
Food and food type can affect the pharmacokinetics of a drug [10]; therefore, entospletinib pharmacokinetics were evaluated following co-administration with a high-fat meal. A dose-dependent reduction in both the absorption rate (20–70% reduction in C max and t max prolongation by ~2 h) and extent (20–80% reduction in AUC) of entospletinib exposures was observed under fed conditions with comparable terminal t ½, suggesting a decrease in the total bioavailability of entospletinib without significant effect on total body clearance. The results may be explained by the pH-dependent solubility of the mono-mesylate salt, since food intake can increase pH in the gastrointestinal tract [10] (which appears to take precedence over the solubilizing effect of food on entospletinib).
The potency of entospletinib to inhibit SYK downstream of the FcɛR was determined in basophils. Crosslinking of the FcɛR by anti-IgE induces a phosphorylation of the immunoreceptor tyrosine-based activation motif (ITAM) repeat in the FcɛR, thereby engaging and activating SYK. The resultant intracellular signaling can be monitored by an increase in the cell-surface expression of the activation marker CD63 in basophils [11]. In addition, direct inhibition of pervanadate-induced SYK phosphorylation (at the Y525/526 autophosphorylation site) by entospletinib was evaluated in whole blood.
A good correlation existed between plasma entospletinib concentrations and the pharmacodynamic measurements; increasing entospletinib plasma concentrations resulted in greater suppression of CD63 expression/pSYK, with maximal inhibition observed at C max. Furthermore, pharmacodynamic inhibition increased with doses of entospletinib up to 600 mg with comparable maximal inhibition at higher doses.
The estimated EC50 values for inhibition of CD63 and pSYK were 429 and 110 ng/mL, respectively. Therefore, at entospletinib doses of 600 mg twice daily or higher, the steady-state C trough levels (approximately >1200 ng/mL) achieved would provide complete coverage of the pharmacodynamics EC50 values throughout the 12-h dosing interval.
Based on the results shown previously, and considering the inter-individual variability, entospletinib 800 mg twice daily (fasted) was selected as the phase II dose to provide maximum drug exposure for subjects with malignant disease.
Overall, entospletinib was generally well-tolerated when administered as a single dose or in multiple doses. At higher doses, some subjects developed modest increases in indirect bilirubin, consistent with uridine 5′-diphospho-glucuronosyltransferase (UGT) 1A1 inhibition (in vitro IC50 ~ 2.5 µmol/L) [8]. Increases in bilirubin were not associated with other liver function test abnormalities. Increased transaminases were noted in six subjects, including two placebo subjects, and tended to be observed approximately 2 weeks after completion of the study drug. All elevated total bilirubin and transaminase levels returned to normal during follow-up.
5 Conclusions
Entospletinib exposures reached a plateau at 600 mg twice daily under fasted conditions, and provided >50% CD63/pSYK inhibition at C trough. Overall, entospletinib displayed an acceptable safety profile, supporting further clinical evaluation in cancer patients.
References
Geahlen RL. SYK and pTyr’d: signaling through the B cell antigen receptor. Biochim Biophys Acta. 2009;1793:1115–27.
Wong BR, Grossbard EB, Payan DG, Masuda ES. Targeting SYK as a treatment for allergic and autoimmune disorders. Expert Opin Invest Drugs. 2004;13:743–62.
Efremov DG, Laurenti L. The SYK kinase as a therapeutic target in leukemia and lymphoma. Expert Opin Invest Drugs. 2011;20:623–36.
Woyach JA, Johnson AJ, Byrd JC. The B-cell receptor signaling pathway as a therapeutic target in CLL. Blood. 2012;120:1175–84.
D’Cruz OJ, Uckun FM. Targeting spleen tyrosine kinase (SYK) for treatment of human disease. J Pharm Drug Deliv Res. 2012;1:1–14.
Friedberg JW, Sharman J, Sweetenham J, Johnston PB, Vose JM, Lacasce A, et al. Inhibition of Syk with fostamatinib disodium has significant clinical activity in non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood. 2010;115:2578–85.
Sharman J, Hawkins M, Kolibaba K, Boxer M, Klein L, Wu M, et al. An open-label phase 2 trial of entospletinib (GS-9937), a selective spleen tyrosine kinase inhibitor, in chronic lymphocytic leukemia. Blood. 2015;125:2336–43.
Data on file, Gilead Sciences, Inc. (2012)
Greene DS, Barbhaiya RH. Clinical pharmacokinetics of nefazodone. Clin Pharmacokinet. 1997;33:260–75.
Singh BN. Effects of food on clinical pharmacokinetics. Clin Pharmacokinet. 1999;37:213–55.
Braselmann S, Taylor V, Zhao H, Wang S, Sylvain C, Baluom M, et al. R406, an orally available spleen tyrosine kinase inhibitor blocks fc receptor signaling and reduces immune complex-mediated inflammation [erratum in J Pharmacol Exp Ther. 2013;345:326]. J Pharmacol Exp Ther. 2006;319:998–1008.
Acknowledgements
The authors thank Impact Communication Partners, Inc., for editorial assistance in preparing the manuscript. The results of this study were presented in part at the 2013 Annual Meeting of American Conference of Cancer Research (AACR) (6–10 April 2013, Washington, DC, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
This study was performed in compliance with current Good Clinical Practice (GCP) and was conducted under the review of the affiliated Institutional Review Board (IRB), whose operations were in compliance with Section 56 of Title 21 of the Code of Federal Regulations (CFR). This study was sponsored by Gilead Sciences, Inc.
Informed Consent
Informed consent was obtained from all subjects.
Funding
Financial support for this study was provided by Gilead Sciences, Inc.
Conflict of Interest
SR, JAD, FJ, LS, SS, MR, and BPK are employees of Gilead Sciences, Inc. and may own stock or hold stock options in the company.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ramanathan, S., Di Paolo, J.A., Jin, F. et al. Pharmacokinetics, Pharmacodynamics, and Safety of Entospletinib, a Novel pSYK Inhibitor, Following Single and Multiple Oral Dosing in Healthy Volunteers. Clin Drug Investig 37, 195–205 (2017). https://doi.org/10.1007/s40261-016-0476-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-016-0476-x