Abstract
Interleukin (IL)-36 cytokines are members of the IL-1 superfamily of cytokines. IL-36 cytokines are composed of three agonists (IL-36α, IL-36β, and IL-36γ) and two antagonists (IL-36 receptor antagonist [IL36Ra] and IL-38). These work in innate and acquired immunity and are known to contribute to host defense and to the pathogenesis of autoinflammatory diseases, autoimmune diseases, and infectious diseases. In the skin, IL-36α and IL-36γ are mainly expressed by keratinocytes in the epidermis, although they are also produced by dendritic cells, macrophages, endothelial cells, and dermal fibroblasts. IL-36 cytokines participate in the first-line defense of the skin against various exogenous assaults. IL-36 cytokines play significant roles in the host defense system and in the regulation of inflammatory pathways in the skin, collaborating with other cytokines/chemokines and immune-related molecules. Thus, numerous studies have shown IL-36 cytokines to play important roles in the pathogenesis of various skin diseases. In this context, the clinical efficacy and safety profiles of anti-IL-36 agents such as spesolimab and imsidolimab have been evaluated in patients with generalized pustular psoriasis, palmoplantar pustulosis, hidradenitis suppurativa, acne/acneiform eruptions, ichthyoses, and atopic dermatitis. This article comprehensively summarizes the roles played by IL-36 cytokines in the pathogenesis and pathophysiology of various skin diseases and summarizes the current state of research on therapeutic agents that target IL-36 cytokine pathways.

Similar content being viewed by others
References
Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281:8–27. https://doi.org/10.1111/imr.12621.
van de Veerdonk FL, Netea MG. New insights in the immunobiology of IL-1 family members. Front Immunol. 2013;4:167. https://doi.org/10.3389/fimmu.2013.00167.
Xu D, Mu R, Wei X. The roles of IL-1 family cytokines in the pathogenesis of systemic sclerosis. Front Immunol. 2019;10:2025. https://doi.org/10.3389/fimmu.2019.02025.
Tsang MS, Sun X, Wong CK. The role of newe IL-1 family members (IL-36 and IL-38) in atopic dermatitis, allergic asthma, and allergic rhinitis. Curr Allergy Asthma Rep. 2020;20:40. https://doi.org/10.1007/s1182-020-00937-1.
Boutet MA, Nerviani A, Pitzalis C. IL-36, IL-37, and IL-38 cytokines in skin and joint inflammation: a comprehensive review of their therapeutic potential. Int J Mol Sci. 2019;20:1257. https://doi.org/10.3390/ijms20061257.
Madonna S, Girolomoni G, Dinarello CA, Albanesi C. The significance of IL-36 hyperactivation and IL-36R targeting in psoriasis. Int J Mol Sci. 2019;20:3318. https://doi.org/10.3390/ijms20133318.
Towne JE, Renshaw BR, Douangpanya J, Lipsky BP, Shen M, Gabel CA, Sims JE. Interleukin-36 (IL-36) ligands require processing for full agonist (IL-36α, IL-36β, and IL-36γ) or antagonist (IL-36Ra) activity. J Biol Chem. 2011;286:42594–602. https://doi.org/10.1074/jbc.M111.267922.
Henry CM, Sullivan GP, Clancy DM, Afonina IS, Kulms D, Martin SJ. Neutrophil-derived proteases escalate inflammation through activation of IL-36 family cytokines. Cell Rep. 2016;14:708–22. https://doi.org/10.1016/j.celrep.2015.12.072.
Macleod T, Doble R, McGonagle D, Wasson CW, Alase A, Stacey M, Wittmann M. Neutrophil elastase-mediated proteolysis activates the anti-inflammatory cytokine IL-36 receptor antagonist. Sci Rep. 2016;6:24880. https://doi.org/10.1038/srep24880.
Clancy DM, Henry CM, Sullivan GP, Martin SJ. Neutrophil extracellular traps can serve as platforms for processing and activation of IL-1 family cytokines. FEBS J. 2017;284:1712–25. https://doi.org/10.1111/febs.14075.
Clancy DM, Sullivan GP, Moran HBT, Henry CM, Reeves EP, McElvaney NG, et al. Extracellular neutrophil proteases are efficient regulators of IL-1, IL-33, and IL-36 cytokine activity but poor effectors of microbial killing. Cell Rep. 2018;22:2937–50. https://doi.org/10.1016/j.celrep.2018.02.062.
Guo J, Tu J, Hu Y, Song G, Yin Z. Cathepsin G cleaves and activates IL-36γ and promotes the inflammation of psoriasis. Drug Des Devel Ther. 2019;13:581–8. https://doi.org/10.2147/DDDT.S194765.
Johnston A, Xing X, Wolterink L, Barnes DH, Yin Z, Reingold L, et al. IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis. J Allergy Clin Immunol. 2017;140:109–20. https://doi.org/10.1016/j.jaci.2016.08.056.
Gresnigt MS, van de Veerdonk FL. Biology of IL-36 cytokines and their role in disease. Semin Immunol. 2013;25:458–65. https://doi.org/10.1016/j.smim.2013.11.003.
Boutet MA, Bart G, Penhoat M, Amiaud J, Brulin B, Charrier C, et al. Distinct expression of interleukin (IL)-36α, β and γ, their antagonist IL-36Ra and IL-38 in psoriasis, rheumatoid arthritis and Crohn’s disease. Clin Exp Immunol. 2016;184:159–73. https://doi.org/10.1111/cei.12761.
Dyring-Andersen B, Løvendorf MB, Coscia F, Santos A, Møller LBP, Colaço AR, et al. Spatially and cell-type resolved quantitative proteomic atlas of healthy human skin. Nat Commun. 2020;11:5587. https://doi.org/10.1038/s41467-020-19383-8.
Albanesi C, Madonna S, Gisondi P, Girolomoni G. The interplay between keratinocytes and immune cells in the pathogenesis of psoriasis. Front Immunol. 2018;9:1549. https://doi.org/10.3389/fimmu.2018.01549.
Walsh PT, Fallon PG. The emergence of the IL-36 cytokine family as novel targets for inflammatory diseases. Ann N Y Acad Sci. 2018;1417:23–34. https://doi.org/10.1111/nyas.13280.
Murrieta-Coxca JM, Rodríguez-Martínez S, Cancino-Diaz ME, Markert UR, Favaro RR, Morales-Prieto DM. IL-36 cytokines: regulators of inflammatory responses and their emerging role in immunology of reproduction. Int J Mol Sci. 2019;20:1649. https://doi.org/10.3390/ijms20071649.
van de Veerdonk FL, Stoeckman AK, Wu G, Boeckermann AN, Azam T, Netea MG, et al. IL-38 binds to the IL-36 receptor and has biological effects on immune cells similar to IL-36 receptor antagonist. Proc Natl Acad Sci USA. 2012;109:3001–5. https://doi.org/10.1073/pnas.1121534109.
Calabrese L, Fiocco Z, Satoh TK, Peris K, French LE. Therapeutic potential of targeting interleukin-1 family cytokines in chronic inflammatory skin diseases. Br J Dermatol. 2022;186:925–41. https://doi.org/10.1111/bjd.20975.
Foster AM, Baliwag J, Chen CS, Guzman AM, Stoll SW, Gudjonsson JE, et al. IL-36 promotes myeloid cell infiltration, activation, and inflammatory activity in skin. J Immunol. 2014;192:6053–61. https://doi.org/10.4049/jimmunol.1301481.
Vigne S, Palmer G, Lamacchia C, Martin P, Talabot-Ayer D, Rodriguez E, et al. IL-36R ligands are potent regulators of dendritic and T cells. Blood. 2011;118:5813–23. https://doi.org/10.1182/blood-2011-05-356873.
Carrier Y, Ma HL, Ramon HE, Napierata L, Small C, O’Toole M, et al. Inter-regulation of Th-17 cytokines and the IL-36 cytokines in vitro and in vivo: implications in psoriasis pathogenesis. J Invest Dermatol. 2011;131:2428–37. https://doi.org/10.1038/jid.2011.234.
Li N, Yamasaki K, Saito R, Fukushi-Takahashi S, Shimada-Omori R, Asano M, et al. Alarmin function of cathelicidin antimicrobial peptide LL37 through IL-36γ induction in human epidermal keratinocytes. J Immunol. 2014;193:5140–8. https://doi.org/10.4049/jimmunol.1302574.
Gabay C, Towne JE. Regulation and function of interleukin-36 cytokines in homeostasis and pathological conditions. J Leukoc Biol. 2015;97:645–52. https://doi.org/10.1189/jlb.3RI1014-495R.
Giannoudaki E, Stefanska AM, Lawler H, Leon G, Hernandez Santana YE, Hassan N, et al. SIGIRR negatively regulates IL-36-driven psoriasiform inflammation and neutrophil infiltration in the skin. J Immunol. 2021;207:651–60. https://doi.org/10.4049/jimmunol.2100237.
Bou-Dargham MJ, Khamis ZI, Cognetta AB, Sang QA. The role of interleukin-1 in inflammatory and malignant human skin diseases and the rationale for targeting interleukin-1 alpha. Med Res Rev. 2017;37:180–216. https://doi.org/10.1002/med.21406.
Bridgewood C, Fearnley GW, Berekmeri A, Laws P, Macleod T, Ponnambalam S, et al. IL-36γ is a strong inducer of IL-23 in psoriatic cells and activates angiogenesis. Front Immunol. 2018;9:200. https://doi.org/10.3389/fimmu.2018.00200.
Buhl AL, Wenzel J. Interleukin-36 in infectious and inflammatory skin diseases. Front Immunol. 2019;10:1162. https://doi.org/10.3389/fimmu.2019.01162.
Akiyama M, Takeichi T, McGrath JA, Sugiura K. Autoinflammatory keratinization diseases. J Allergy Clin Immunol. 2017;140:1545–7. https://doi.org/10.1016/j.jaci.2017.05.019.
Akiyama M, Takeichi T, McGrath JA, Sugiura K. Autoinflammatory keratinization diseases: an emerging concept encompassing various inflammatory keratinization disorders of the skin. J Dermatol Sci. 2018;90:105–11. https://doi.org/10.1016/j.jdermsci.2018.01.012.
Akiyama M. Pustular psoriasis as an autoinflammatory keratinization disease (AiKD): genetic predisposing factors and promising therapeutic targets. J Dermatol Sci. 2022;105:11–7. https://doi.org/10.1016/j.jdermsci.2021.11.009.
Marrakchi S, Guigue P, Renshaw BR, Puel A, Pei XY, Fraitag S, et al. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N Engl J Med. 2011;365:620–8. https://doi.org/10.1056/NEJMoa1013068.
Sugiura K, Muto M, Akiyama M. CARD14 c.526G>C (p.Asp176His) is a significant risk factor for generalized pustular psoriasis with psoriasis vulgaris in the Japanese cohort. J Invest Dermatol. 2014;134:1755–7. https://doi.org/10.1038/jid.2014.46.
Takeichi T, Kobayashi A, Ogawa E, Okuno Y, Kataoka S, Kono M, et al. Autosomal dominant familial generalized pustular psoriasis caused by a CARD14 mutation. Br J Dermatol. 2017;177:e133–5. https://doi.org/10.1111/bjd.15442.
Setta-Kaffetzi N, Simpson MA, Navarini AA, Patel VM, Lu HC, Allen MH, et al. AP1S3 mutations are associated with pustular psoriasis and impaired toll-like receptor 3 trafficking. Am J Hum Genet. 2014;94:790–7. https://doi.org/10.1111/bjd.15442.
Haskamp S, Bruns H, Hahn M, Hoffmann M, Gregor A, Löhr S, et al. Myeloperoxidase modulates inflammation in generalized pustular psoriasis and additional rare pustular skin diseases. Am J Hum Genet. 2020;107:527–38. https://doi.org/10.1016/j.ajhg.2020.07.001.
Frey S, Sticht H, Wilsmann-Theis D, Gerschütz A, Wolf K, Löhr S, et al. Rare loss-of-function mutation in SERPINA3 in generalized pustular psoriasis. J Invest Dermatol. 2020;140:1451-5.e13. https://doi.org/10.1016/j.jid.2019.11.024.
Mössner R, Wilsmann-Theis D, Oji V, Gkogkolou P, Löhr S, Schulz P, et al. The genetic basis for most patients with pustular skin disease remains elusive. Br J Dermatol. 2018;178:740–8. https://doi.org/10.1111/bjd.15867.
Twelves S, Mostafa A, Dand N, Burri E, Farkas K, Wilson R, et al. Clinical and genetic differences between pustular psoriasis subtypes. J Allergy Clin Immunol. 2019;143:1021–6. https://doi.org/10.1016/j.jaci.2018.06.038.
Sugiura K, Takemoto A, Yamaguchi M, Takahashi H, Shoda Y, Mitsuma T, et al. The majority of generalized pustular psoriasis without psoriasis vulgaris is caused by deficiency of interleukin-36 receptor antagonist. J Invest Dermatol. 2013;133:2514–21. https://doi.org/10.1038/jid.2013.230.
Takeichi T, Togawa Y, Okuno Y, Taniguchi R, Kono M, Matsue H, et al. A newly revealed IL36RN mutation in sibling cases complements our IL36RN mutation statistics for generalized pustular psoriasis. J Dermatol Sci. 2017;85:58–60. https://doi.org/10.1016/j.jdermsci.2016.10.009.
Akiyama M. Early-onset generalized pustular psoriasis is representative of autoinflammatory keratinization diseases. J Allergy Clin Immunol. 2019;143:809–10. https://doi.org/10.1016/j.jaci.2018.11.009.
Hussain S, Berki DM, Choon SE, Burden AD, Allen MH, Arostegui JI, et al. IL36RN mutations define a severe autoinflammatory phenotype of generalized pustular psoriasis. J Allergy Clin Immunol. 2015;135:1067–70. https://doi.org/10.1016/j.jaci.2014.09.043.
Mahil SK, Twelves S, Farkas K, Setta-Kaffetzi N, Burden AD, Gach JE, et al. AP1S3 mutations cause skin autoinflammation by disrupting keratinocyte autophagy and up-regulating IL-36 production. J Invest Dermatol. 2016;136:2251–9. https://doi.org/10.1016/j.jid.2016.06.618.
Akiyama M. Autoinflammatory keratinization diseases (AiKDs): Expansion of disorders to be included. Front Immunol. 2020;11:280. https://doi.org/10.3389/fimmu.2020.00280.
Zhou L, Todorovic V. Interleukin-36: structure, signaling and function. Adv Exp Med Biol. 2021;21:191–210. https://doi.org/10.1007/5584_2020_488.
Mercurio L, Morelli M, Scarponi C, Eisenmesser EZ, Doti N, Pagnanelli G, et al. IL-38 has an anti-inflammatory action in psoriasis and its expression correlates with disease severity and therapeutic response to anti-IL-17A treatment. Cell Death Dis. 2018;9:1104. https://doi.org/10.1038/s41419-018-1143-3.
Catapano M, Vergnano M, Romano M, Mahil SK, Choon SE, Burden AD, et al. IL-36 promotes systemic IFN-I responses in severe forms of psoriasis. J Invest Dermatol. 2020;140:816-26.e3. https://doi.org/10.1016/j.jid.2019.08.444.
Wang WM, Jin HZ. Role of neutrophils in psoriasis. J Immunol Res. 2020;2020:3709749. https://doi.org/10.1155/2020/3709749.
Watanabe S, Iwata Y, Fukushima H, Saito K, Tanaka Y, Hasegawa Y, et al. Neutrophil extracellular traps are induced in a psoriasis model of interleukin-36 receptor antagonist-deficient mice. Sci Rep. 2020;10:20149. https://doi.org/10.1038/s41598-020-76864-y.
Murakami M, Terui T. Palmoplantar pustulosis: Current understanding of disease definition and pathomechanism. J Dermatol Sci. 2020;98:13–9. https://doi.org/10.1016/j.jdermsci.2020.03.003.
Xiaoling Y, Chao W, Wenming W, Feng L, Hongzhong J. Interleukin (IL)-8 and IL-36γ but not IL-36Ra are related to acrosyringia in pustule formation associated with palmoplantar pustulosis. Clin Exp Dermatol. 2019;44:52–7. https://doi.org/10.1111/ced.13689.
Sidoroff A, Halevy S, Bavinck JN, Vaillant L, Roujeau JC. Acute generalized exanthematous pustulosis (AGEP): a clinical reaction pattern. J Cutan Pathol. 2001;28:113–9. https://doi.org/10.1034/j.1600-0560.2001.028003113.x.
Feldmeyer L, Heidemeyer K, Yawalkar N. Acute generalized exanthematous pustulosis: pathogenesis, genetic background, clinical variants and therapy. Int J Mol Sci. 2016;17:1214. https://doi.org/10.3390/ijms17081214.
Meier-Schiesser B, Feldmeyer L, Jankovic D, Mellett M, Satoh TK, Yerly D, et al. Culprit drugs induce specific IL-36 overexpression in acute generalized exanthematous pustulosis. J Invest Dermatol. 2019;139:848–58. https://doi.org/10.1016/j.jid.2018.10.023.
Nakai N, Sugiura K, Akiyama M, Katoh N. Acute generalized exanthematous pustulosis caused by dihydrocodeine phosphate in a patient with psoriasis vulgaris and a heterozygous IL36RN mutation. JAMA Dermatol. 2015;151:311–5. https://doi.org/10.1001/jamadermatol.2014.3002.
Vergnano M, Mockenhaupt M, Benzian-Olsson N, Paulmann M, Grys K, Mahil SK, et al. Loss-of-function myeloperoxidase mutations are associated with increased neutrophil counts and pustular skin disease. Am J Hum Genet. 2020;107:539–43. https://doi.org/10.1016/j.ajhg.2020.06.020.
von Laffert M, Helmbold P, Wohlrab J, Fiedler E, Stadie V, Marsch WC. Hidradenitis suppurativa (acne inversa): early inflammatory events at terminal follicles and at interfollicular epidermis. Exp Dermatol. 2010;19:533–7. https://doi.org/10.1111/j.1600-0625.2009.00915.x.
Ainscough JS, Macleod T, McGonagle D, Brakefield R, Baron JM, Alase A, et al. Cathepsin S is the major activator of the psoriasis-associated proinflammatory cytokine IL-36gamma. Proc Natl Acad Sci USA. 2017;114:E2748–57. https://doi.org/10.1073/pnas.1620954114.
Hessam S, Sand M, Gambichler T, Skrygan M, Rüddel I, Bechara FG. Interleukin-36 in hidradenitis suppurativa: evidence for a distinctive proinflammatory role and a key factor in the development of an inflammatory loop. Br J Dermatol. 2018;178:761–7. https://doi.org/10.1111/bjd.16019.
Thomi R, Kakeda M, Yawalkar N, Schlapbach C, Hunger RE. Increased expression of the interleukin-36 cytokines in lesions of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2017;31:2091–6. https://doi.org/10.1111/jdv.14389.
Di Caprio R, Balato A, Caiazzo G, Lembo S, Raimondo A, Fabbrocini G, et al. IL-36 cytokines are increased in acne and hidradenitis suppurativa. Arch Dermatol Res. 2017;309:673–8. https://doi.org/10.1007/s00403-017-1769-5.
Sims JE, Smith DE. The IL-1 family: regulators of immunity. Nat Rev Immunol. 2010;10:89–102. https://doi.org/10.1038/nri2691.
Wolk K, Brembach TC, Šimaitė D, Bartnik E, Cucinotta S, Pokrywka A, et al. Activity and components of the granulocyte colony-stimulating factor pathway in hidradenitis suppurativa. Br J Dermatol. 2021;185:164–76. https://doi.org/10.1111/bjd.19795.
Yang J, Wang L, Huang Y, Liu K, Lu C, Si N, et al. Keratin 5-Cre-driven deletion of Ncstn in an acne inversa-like mouse model leads to a markedly increased IL-36a and Sprr2 expression. Front Med. 2019;14:305–17. https://doi.org/10.1007/s11684-019-0722-8.
Paller AS, Renert-Yuval Y, Suprun M, Esaki H, Oliva M, Huynh TN, et al. An IL-17-dominant immune profile is shared across the major orphan forms of ichthyosis. J Allergy Clin Immunol. 2017;139:152–65. https://doi.org/10.1016/j.jaci.2016.07.019.
Akiyama M. Understanding immune profiles in ichthyosis may lead to novel therapeutic targets. J Allergy Clin Immunol. 2022;149:1210–2. https://doi.org/10.1016/j.jaci.2022.02.010.
Malik K, He H, Huynh TN, Tran G, Mueller K, Doytcheva K, et al. Ichthyosis molecular fingerprinting shows profound TH-17 skewing and a unique barrier genomic signature. J Allergy Clin Immunol. 2019;143:604–18. https://doi.org/10.1016/j.jaci.2018.03.021.
Fontao L, Laffitte E, Briot A, Kaya G, Roux-Lombard P, Fraitag S, et al. Infliximab infusions for Netherton syndrome: sustained clinical improvement correlates with a reduction of thymic stromal lymphopoietin levels in the skin. J Invest Dermatol. 2011;131:1947–50. https://doi.org/10.1038/jid.2011.124.
Akagi A, Kitoh A, Moniaga CS, Fujimoto A, Fujikawa H, Shimomura Y, et al. Case of Netherton syndrome with an elevated serum thymus and activation-regulated chemokine level. J Dermatol. 2013;40:752–3. https://doi.org/10.1111/1346-8138.12209.
Yalcin AD. A case of Netherton syndrome: successful treatment with omalizumab and pulse prednisolone and its effects on cytokines and immunoglobulin levels. Immunopharmacol Immunotoxicol. 2016;38:162–6. https://doi.org/10.3109/08923973.2015.1115518.
Murase Y, Takeichi T, Kawamoto A, Tanahashi K, Okuno Y, Takama H, et al. Reduced stratum corneum acylceramides in autosomal recessive congenital ichthyosis with a NIPAL4 mutation. J Dermatol Sci. 2020;97:50–6. https://doi.org/10.1016/j.jdermsci.2019.12.001.
Barbieux C, Bonnet des Claustres M, Fahrner M, Petrova E, Tsoi LC, Gouin O, et al. Netherton syndrome subtypes share IL-17/IL-36 signature with distinct IFN-α and allergic responses. J Allergy Clin Immunol. 2022;149:1358–72. https://doi.org/10.1016/j.jaci.2021.08.024.
Quaranta M, Knapp B, Garzorz N, Mattii M, Pullabhatla V, Pennino D, et al. Intraindividual genome expression analysis reveals a specific molecular signature of psoriasis and eczema. Sci Transl Med. 2014;6:244ra90. https://doi.org/10.1126/scitranslmed.3008946.
Suárez-Fariñas M, Ungar B, Correa da Rosa J, Ewald DA, Rozenblit M, Gonzalez J, et al. RNA sequencing atopic dermatitis transcriptome profiling provides insights into novel disease mechanisms with potential therapeutic implications. J Allergy Clin Immunol. 2015;135:1218–27. https://doi.org/10.1016/j.jaci.2015.03.003.
Tsoi LC, Rodriguez E, Stölzl D, Wehkamp U, Sun J, Gerdes S, et al. Progression of acute-to-chronic atopic dermatitis is associated with quantitative rather than qualitative changes in cytokine responses. J Allergy Clin Immunol. 2020;145:1406–15. https://doi.org/10.1016/j.jaci.2019.11.047.
Geoghegan JA, Irvine AD, Foster TJ. Staphylococcus aureus and atopic dermatitis: a complex and evolving relationship. Trends Microbiol. 2018;26:484–97. https://doi.org/10.1016/j.tim.2017.11.008.
Liu H, Archer NK, Dillen CA, Wang Y, Ashbaugh AG, Ortines RV, et al. Staphylococcus aureus epicutaneous exposure drives skin inflammation via IL-36-mediated T cell responses. Cell Host Microbe. 2017;22:653-66.e5. https://doi.org/10.1016/j.chom.2017.10.006.
Nakagawa S, Matsumoto M, Katayama Y, Oguma R, Wakabayashi S, Nygaard T, et al. Staphylococcus aureus virulent PSMα peptides induce keratinocyte alarmin release to orchestrate IL-17-dependent skin inflammation. Cell Host Microbe. 2017;22:667-77.e5. https://doi.org/10.1016/j.chom.2017.10.008.
Patrick GJ, Liu H, Alphonse MP, Dikeman DA, Youn C, Otterson JC, et al. Epicutaneous Staphylococcus aureus induces IL-36 to enhance IgE production and ensuing allergic disease. J Clin Invest. 2021;131: e143334. https://doi.org/10.1172/JCI143334.
Mohamed El Esawy F, Ali Mohammed S, Nasar Zargon Nasar E, Hemdan Mostafa S, Elhabak DM. Environmental, inflammatory, and anti-inflammatory squad in acne vulgaris pathogenesis: AhR, IL-36, and IL-38. J Cosmet Dermatol. 2022;21:3038–45. https://doi.org/10.1111/jocd.14542.
Satoh TK, Mellett M, Meier-Schiesser B, Fenini G, Otsuka A, Beer HD, et al. IL-36γ drives skin toxicity induced by EGFR/MEK inhibition and commensal Cutibacterium acnes. J Clin Invest. 2020;130:1417–30. https://doi.org/10.1172/JCI128678.
Ly K, Smith MP, Thibodeaux Q, Reddy V, Liao W, Bhutani T. Anti IL-17 in psoriasis. Expert Rev Clin Immunol. 2019;15(11):1185–94. https://doi.org/10.1080/1744666X.2020.1679625.
Pfaff CM, Marquardt Y, Fietkau K, Baron JM, Lüscher B. The psoriasis-associated IL-17A induces and cooperates with IL-36 cytokines to control keratinocyte differentiation and function. Sci Rep. 2017;7(1):15631. https://doi.org/10.1038/s41598-017-15892-7.
Elias M, Zhao S, Le HT, Wang J, Neurath MF, Neufert C, Fiocchi C, Rieder F. IL-36 in chronic inflammation and fibrosis—bridging the gap? J Clin Invest. 2021;131(2): e144336. https://doi.org/10.1172/JCI144336.
Mahil SK, Catapano M, Di Meglio P, Dand N, Ahlfors H, Carr IM, et al. An analysis of IL-36 signature genes and individuals with IL1RL2 knockout mutations validates IL-36 as a psoriasis therapeutic target. Sci Transl Med. 2017;9:2514. https://doi.org/10.1126/scitranslmed.aan2514.
Novel Drug Approvals for 2022. US FDA; 2023. https://www.fda.gov/drugs/new-drugs-fda-cders-new-molecular-entities-and-new-therapeutic-biological-products/novel-drug-approvals-2022. Accessed 2 Feb 2023.
Blair HA. Spesolimab: first approval. Drugs. 2022;82(17):1681–6.
Baum P, Visvanathan S, Garcet S, Roy J, Schmid R, Bossert S, Lang B, Bachelez H, Bissonnette R, Thoma C, Krueger JG. Pustular psoriasis: molecular pathways and effects of spesolimab in generalized pustular psoriasis. J Allergy Clin Immunol. 2022;149(4):1402–12. https://doi.org/10.1016/j.jaci.2021.09.035.
Bachelez H, Choon SE, Marrakchi S, Burden AD, Tsai TF, Morita A, et al. Inhibition of the interleukin-36 pathway for the treatment of generalized pustular psoriasis. N Engl J Med. 2019;380:981–3. https://doi.org/10.1056/NEJMc1811317.
Bachelez H, Choon SE, Marrakchi S, Burden AD, Tsai TF, Morita A, et al. Effisayil 1 trial investigators. Trial of spesolimab for generalized pustular psoriasis. N Engl J Med. 2021;385:2431–40. https://doi.org/10.1056/NEJMoa2111563.
Choon SE, Lebwohl MG, Marrakchi S, Burden AD, Tsai TF, Morita A, et al. Study protocol of the global Effisayil 1 Phase II, multicentre, randomised, double-blind, placebo-controlled trial of spesolimab in patients with generalized pustular psoriasis presenting with an acute flare. BMJ Open. 2021;11: e043666. https://doi.org/10.1136/bmjopen-2020-043666.
Morita A, Choon SE, Bachelez H, Anadkat MJ, Marrakchi S, Zheng M, et al. Design of Effisayil™ 2: a randomized, double-blind, placebo-controlled study of spesolimab in preventing flares in patients with generalized pustular psoriasis. Dermatol Ther (Heidelb). 2023;13(1):347–59.
Mrowietz U, Burden AD, Pinter A, Reich K, Schäkel K, Baum P, et al. Spesolimab, an anti-interleukin-36 receptor antibody, in patients with palmoplantar pustulosis: results of a phase IIa, multicenter, double-blind, randomized, placebo-controlled pilot study. Dermatol Ther (Heidelb). 2021;11:571–85. https://doi.org/10.1007/s13555-021-00504-0.
Burden A, Bissonnette R, Navarini A, Murakami M, Morita A, Mozzicato S, et al. 32923 A multicenter, double-blind, randomized, placebo-controlled, phase IIb dose-finding study to evaluate efficacy and safety of spesolimab in patients with moderate-to-severe palmoplantar pustulosis. J Am Acad Dermatol. 2022;87(3 Suppl):AB131.
Misiak-Galazka M, Zozula J, Rudnicka L. Palmoplantar pustulosis: Recent advances in etiopathogenesis and emerging treatments. Am J Clin Dermatol. 2020;21:355–70. https://doi.org/10.1007/s40257-020-00503-5.
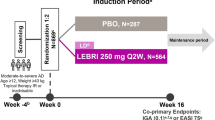
Bissonnette R, Abramovits W, Saint-Cyr Proulx É, Lee P, Guttman-Yassky E, Zovko E, et al. Spesolimab, an anti-interleukin-36 receptor antibody, in patients with moderate-to-severe atopic dermatitis: Results from a multicentre, randomized, double-blind, placebo-controlled, phase IIa study. J Eur Acad Dermatol Venereol. 2023;37(3):549–57. https://doi.org/10.1111/jdv.18727.
Khanskaya I, Pinkstaff J, Marino MH, Savall T, Li J, Londei M. A phase 1 study of ANB019, an anti-IL-36 receptor monoclonal antibody, in healthy volunteers. AnaptysBio; 2018. https://www2.anaptysbio.com/wp-content/uploads/ANB019-Phase-1-Study-Poster-EAACI-2018.pdf. Accessed 2 Feb 2023.
Gudjonsson J, Randazzo B, Zhou J. 34617 Imsidolimab in the treatment of adult subjects with generalized pustular psoriasis: design of a pivotal phase 3 clinical trial and a long-term extension study. J Am Acad Dermatol. 2022;87(3 Suppl):AB70.
About 008. INMAGENE; 2022. https://www.inmagenebio.com/zokibep.html?id=fc074bee-425d-4f55-ab6a-6064f67bf751. Accessed 2 Feb 2023.
Iznardo H, Puig L. Exploring the role of IL-36 cytokines as a new target in psoriatic disease. Int J Mol Sci. 2021;22:4344. https://doi.org/10.3390/ijms22094344.
Ågerstam H, Hansen N, von Palffy S, Sandén C, Reckzeh K, Karlsson C, et al. IL1RAP antibodies block IL-1-induced expansion of candidate CML stem cells and mediate cell killing in xenograft models. Blood. 2016;128:2683–93. https://doi.org/10.1182/blood-2015-11-679985.
Chackerian AA, Oldham ER, Murphy EE, Schmitz J, Pflanz S, Kastelein RA. IL-1 receptor accessory protein and ST2 comprise the IL-33 receptor complex. J Immunol. 2007;179(4):2551–5. https://doi.org/10.4049/jimmunol.179.4.2551.
Ganesan R, Raymond EL, Mennerich D, Woska JR Jr, Caviness G, Grimaldi C, et al. Generation and functional characterization of anti-human and anti-mouse IL-36R antagonist monoclonal antibodies. MAbs. 2017;9:1143–54. https://doi.org/10.1080/19420862.2017.1353853.
Grönberg C, Rattik S, Kunz M, Trinh-Minh T, Tran-Manh C, Zhou X, et al. Blocking IL-1, IL-33 and IL-36 signaling with the anti-IL1RAP antibody mCAN10 ameliorates inflammation and fibrosis in preclinical models of systemic sclerosis [abstract]. Arthritis Rheumatol. 2022;74(Suppl):9.
Almirall’s Full-Year 2021 Results. Almirall; 2022. https://www.almirall.com/newsroom/news/almirall-full-year-2021-results. Accessed 2 Feb 2023.
Todorović V, Su Z, Putman CB, Kakavas SJ, Salte KM, McDonald HA, et al. Small molecule IL-36γ antagonist as a novel therapeutic approach for plaque psoriasis. Sci Rep. 2019;9:9089. https://doi.org/10.1038/s41598-019-45626-w.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Masashi Akiyama is supported by Grant-in-Aid for Scientific Research (B) 21H02941 from the Japan Society for the Promotion of Science (JSPS) and by a grant from the Ministry of Health, Labor and Welfare of Japan (Health and Labor Sciences Research Grant for Research on Intractable Diseases: 20FC1052).
Conflicts of interest/competing interests
Masashi Akiyama has received a research grant from Boehringer Ingelheim, Novartis Japan and Maruho, and payment for lectures from Maruho and Sanofi. Ryo Fukaura reports no potential conflicts of interest or financial disclosures that are pertinent to this article.
Ethics approval
Ethics approval is not applicable to this article as no human or animal subjects were analyzed in this review.
Consent to participate
Consent to participate is not applicable to this article as no human or animal subjects were analyzed in this review.
Consent for publication
Consent for publication is not applicable to this article as no human or animal subjects were analyzed in this review.
Availability of data and material
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Code availability
Not applicable to this article as no new data were created or analyzed with code in this study.
Author contributions
All authors contributed to the literature review, writing, and editing of this article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fukaura, R., Akiyama, M. Targeting IL-36 in Inflammatory Skin Diseases. BioDrugs 37, 279–293 (2023). https://doi.org/10.1007/s40259-023-00587-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-023-00587-5