Abstract
Background
Pertuzumab is a humanized monoclonal antibody for the treatment of breast cancer. HLX11 is a biosimilar of pertuzumab developed by Shanghai Henlius Biotech, Inc. We conducted a bioequivalence study for HLX11 and pertuzumab (United States [US]-, European Union [EU]-, and China [CN]-approved products).
Objectives
This study compared the biosimilarity in pharmacokinetics (PK), safety, and immunogenicity between HLX11 and reference pertuzumab (approved in the US, the EU, and CN) in healthy Chinese male participants after a single infusion and further characterized the PK profile of HLX11.
Methods
Eligible individuals were randomized 1:1:1:1 to receive a single dose of 420 mg HLX11, US-, EU-, or CN-pertuzumab via intravenous infusion over 60 min. The primary endpoints were maximum serum drug concentration (Cmax), area under the serum concentration–time curve (AUC) from time 0 to time of the last quantifiable concentration (AUC0–t), and AUC from time 0 to infinity (AUC0–∞). PK bioequivalence was established if the 90% confidence intervals (CIs) of the geometric mean ratios of the primary endpoints were between 80.0 and 125.0%. Secondary endpoints included other PK parameters, safety, and immunogenicity.
Results
A total of 160 participants were enrolled and randomly assigned to each group (n = 40 per group). The 90% CIs of the geometric mean ratios of the primary endpoints were all within the prespecified equivalence margins (HLX11 vs. pertuzumab [US-, EU-, CN-approved products]: Cmax 97.03–115.06%, 91.39–109.80%, 94.53–110.65%; AUC0–t 87.65–99.68%, 87.07–100.79%, 86.29–101.09%; AUC0–∞ 87.66–99.90%, 87.54–101.05%, 89.23–103.20%). The incidence of adverse drug reactions was comparable across the four groups. The presence of anti-drug antibodies or neutralizing antibodies had no obvious effect on PK.
Conclusion
The PK, safety, and immunogenicity of HLX11 were highly similar to those of reference pertuzumab (US-, EU-, CN-approved products). The established bioequivalence supports further clinical trials of HLX11 in cancer treatment.
Trial Registration
This study was registered with ClinicalTrials.gov (NCT04411550) and Chinadrugtrials.org.cn (CTR20200618).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This is the first-in-human clinical study of HLX11, a biosimilar candidate of pertuzumab; HLX11 was found to be pharmacokinetically bioequivalent to the reference pertuzumab (United States [US]-, European Union [EU]-, and China [CN]-approved products). |
The safety profile of HLX11 was similar to that of the originator pertuzumab (US-, EU-, and CN-approved products). |
The overall incidences of anti-drug antibody and neutralizing antibody positivity were low and comparable to the reference pertuzumab (US-, EU-, and CN-approved products). Pharmacokinetic characteristics and the safety profile of HLX11 were not influenced by the presence of anti-drug antibodies. |
1 Introduction
Breast cancer is one of the most common cancers in female patients, and has high morbidity and mortality rates [1]. In recent years, the annual incidence of breast cancer has been increasing, with an estimated 2.3 million new cases (11.7%) occurring in 2020 worldwide [2]. Amplification or overexpression of human epidermal growth factor receptor 2 (HER2) is present in 15–20% of patients with breast cancer, and is known as HER2-positive breast cancer [3]. The amplification of the HER2 gene is an important factor for poor prognosis [4]. The introduction of anti-HER2 therapy has significantly improved clinical outcomes for patients with HER2-positive breast cancer, and HER2 is recognized as one of the most common targets in breast cancer therapy [5].
Currently, several HER2-directed agents are approved for clinical use in various settings. Pertuzumab (Perjeta®) and trastuzumab are monoclonal antibodies used in the treatment of HER2-positive breast cancer [6]. Pertuzumab, a HER dimerization inhibitor, is the first humanized monoclonal antibody in a new class of drugs and is approved for use in combination with trastuzumab as therapy in HER2-positive patients [7]. Pertuzumab (Perjeta®) was approved for marketing in the United States (US), the European Union (EU), and China (CN) in 2012, 2015, and 2018, respectively [7, 8]. Since pertuzumab binds to a different epitope than trastuzumab, combination therapy with pertuzumab and trastuzumab results in a more complete blockade of HER2 signalling than trastuzumab monotherapy. Clinical studies have shown that the combination of these two HER2 inhibitors has a good synergistic effect that significantly improves clinical efficacy and prognosis [8].
The treatment of patients with HER2-positive breast cancer is constantly evolving [9]. While new drugs and treatment strategies are emerging, biological therapies, particularly pertuzumab, are likely to remain a cornerstone of treatment [10]. Although pertuzumab and other biological therapies offer substantial clinical benefits, they are costly, which can limit their availability. Evidence suggests that pertuzumab and trastuzumab are underused worldwide [10]. Biosimilars are biological products that are highly similar to the licenced reference biologic in analytical, preclinical, and clinical properties [11]. Compared to the original drugs, the development of biosimilars provides more cost-effective alternatives to the originator due to lower costs and improved treatment access, thus alleviating unmet clinical needs [12].
HLX11, a recombinant anti-HER2 domain II humanized monoclonal antibody, is a pertuzumab biosimilar candidate that was independently developed by Shanghai Henlius Biotech, Inc. Similar to its branded originator, HLX11 is composed of the variable region of a humanized murine-derived anti-HER2 antibody and the constant region of a human IgG1 antibody, and it is a glycosylated monoclonal antibody containing two 448-amino-acid heavy chains and two 214-amino-acid light chains. Preclinical in vitro, in vivo, and toxicity studies showed that HLX11 and EU-pertuzumab were highly similar in efficacy and safety (data on file).
This phase 1 clinical trial is the first-in-human study of HLX11, and mainly focused on HLX11 to evaluate its pharmacokinetics (PK) profile, safety, and immunogenicity compared to reference pertuzumab (approved in the US, EU, and CN) after a single dose in healthy Chinese male participants.
2 Methods
2.1 Study Design and Treatment
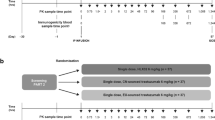
This randomized, double-blind, four-arm, parallel phase 1 study was conducted between September 16, 2020, and February 8, 2021, at the Phase 1 Clinical Trial Unit, the Second Hospital of Anhui Medical University (Hefei, China). The trial was registered at ClinicalTrials.gov (NCT04411550) and Chinadrugtrials.org.cn (CTR20200618).
This single-dose study consisted of a 28-day screening period and a 99-day follow-up period. Upon completion of all screening procedures, eligible participants were randomly assigned in a ratio of 1:1:1:1 to HLX11, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab groups 1 day before infusion. Detailed information on the study drugs is provided in the Electronic Supplementary Material (ESM Table S1). On day 1, participants were given a single dose of 420 mg HLX11, US-pertuzumab, EU-pertuzumab, or CN-pertuzumab via intravenous infusion over 60 min (± 10 min). To prevent infusion-related reactions (IRRs), each participant was given 5 mg of dexamethasone intravenously and 12.5 mg of promethazine hydrochloride intramuscularly 30 min prior to receiving the study drug. Any infusion-related adjustments that occurred during infusion were documented in the original medical records. The administration procedures of the four drugs were identical.
Participants were required to stay at the research centre, and were supervised by the investigators from day 1 (1 day before study drug administration) to day 5 (96 h after study drug administration); during this period of time, the participants were prohibited from taking non-study drugs, excluding the prespecified premedication and any drugs needed for the treatment of an adverse event (AE).
Participants returned to the research centre for follow-up on days 8, 15, 29, 50, 71, and 99 post-dose, mainly for the collection of PK and anti-drug antibody (ADA) blood samples, routine laboratory examinations, including N-terminal pro-brain natriuretic peptide (NT-proBNP), routine blood, routine urine, and blood chemistry tests, and the collection of information on AEs and concomitant medications according to the proposal. The major clinical and laboratory assessments can be found in the Electronic Supplementary Material (see “Clinical and Laboratory Assessments”).
The study was conducted in accordance with the principles of the Declaration of Helsinki, Good Clinical Practice guidelines, and all local applicable regulations. The study protocol and all amendments were approved by the Ethics Committee of the Second Hospital of Anhui Medical University (SL-YW2019-099). All participants provided written informed consent.
2.2 Eligibility Criteria
Healthy Chinese males aged 18–45 years with a body mass index (BMI) of 19–26 kg/m2 were eligible for the study. Left ventricular ejection fraction measured by echocardiography needed to be in the normal range (≥ 55%) within 14 days before randomization. Participants were excluded if they had any serious clinical disease or a history of drug abuse, used any monoclonal antibody within 6 months before receiving the study drug, or donated blood within 3 months before receiving study treatment. Full inclusion and exclusion criteria can be found in the Electronic Supplementary Material (see “Inclusion and Exclusion criteria”).
2.3 Randomization and Blinding
A randomization table was generated by an independent randomization biostatistician using SAS software (v9.2 or higher; SAS Institute Inc., Cary, North Carolina, US); a block randomization method with variable block sizes was applied. The investigator or a qualified designee assigned a random number to each participant in the order of enrolment, and the participant was then assigned to the treatment group by the random number.
In the study, a randomized, double-blind design was used to ensure that the investigator, relevant study personnel, and participants were blinded to the study grouping. Since the investigational drug and the control drug could not be similar in terms of internal packaging, double-blinding was achieved by dividing the researcher into unblinded and blinded groups. The unblinded group was primarily responsible for the management of the investigational drug and dispensing the investigational drug based on the randomization results. The other group, the blinded group, was primarily responsible for infusing the prepared study drug infusion solution and performing safety monitoring and blood sample collection. The unblinded group was not to disclose any information regarding treatment assignment to participants, their families, or others, including study physicians and related study researchers.
2.4 Pharmacokinetic Assessments
All randomized participants who received the designated study drug and had no major protocol deviation affecting the calculation of major PK parameters were included in the PK analysis set (PKS). Blood samples for PK assessment were collected before infusion, immediately after the end of infusion (0 h), and at 1.5 h, 3 h, 24 h (day 2), 48 h (day 3), 96 h (day 5), 168 h (day 8), 336 h (day 15), 672 h (day 29), 1176 h (day 50), 1680 h (day 71), and 2352 h (day 99) post-infusion. A 3.5-mL sample of whole blood was collected at each time point above. The serum concentrations of the study drugs were measured by a validated enzyme-linked immunosorbent assay (ELISA) at WuXi AppTec Co., Ltd. (Shanghai, China). The lower limit of quantification (LLOQ) was 200 ng/mL, and concentrations less than the LLOQ were set to zero. PK analyses were performed using WinNonlin v8.3.1 software (Certara, Princeton, New Jersey, US) with a noncompartmental analysis model.
The primary endpoints of this study were maximum serum drug concentration (Cmax), area under the serum concentration–time curve from time 0 to time of the last quantifiable concentration (AUC0–t), and area under the serum concentration–time curve from time 0 to infinity (AUC0–∞). Secondary PK endpoints included time to reach maximum serum drug concentration (Tmax), elimination half-life (t½), terminal elimination rate constant (λz), total clearance (CL), apparent volume of distribution during terminal phase (Vz), and mean residence time (MRT).
2.5 Safety Assessment
All randomized participants who received the designated study drug were included in the safety set (SS). All AEs that occurred between the time of signing the informed consent form and the end of the follow-up period were recorded. AEs were coded according to Medical Dictionary for Regulatory Activities (MedDRA) Version 23.0 or above. The severity of AEs was graded per the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE) Version 5.0. In causality assessments, all AEs were categorized as adverse drug reactions (ADRs; AEs related to the study drug) except for those definitely unrelated or unlikely related to the study drug. AEs of special interest (AESIs) in this study included cardiotoxicity (for frequency and time points of ECGs, NT-proBNP measurements, and echocardiograms see the Electronic Supplementary Material, “Clinical and Laboratory Assessments”), IRRs, and hypersensitivity or immediate hypersensitivity.
2.6 Immunogenicity Assessment
Blood samples for immunogenicity assessments were collected from all participants before infusion and at 336 h (day 15), 1176 h (day 50), and 2352 h (day 99) post-infusion. ADAs and neutralizing antibodies (NAbs) were detected by validated electrochemiluminescence immunoassays at WuXi AppTec Co., Ltd. Samples with ADA positivity were further tested for the presence or absence of NAbs using validated assays. The titre of positive ADA samples was also evaluated. Methodological validation was strictly implemented in accordance with guidelines [13]. The detailed methodological validation results can be found in the Electronic Supplementary Material (ESM Table S2).
2.7 Administration Dosages and Sample Size
According to the biosimilar guidelines, after high similarity between the investigational drug and the reference products has been confirmed through preclinical trials, the therapeutic dose of the reference products can be used for biosimilarity studies without the necessity of determining the therapeutic dose of the investigational drug through a maximum toxicity dose assessment study [14]. The 420 mg dose is the current clinical dose of the original drug, pertuzumab, and has been reported to have a manageable safety profile in healthy participants, with no serious or unintended toxicity observed [15, 16].
Regarding the variation coefficient of the main PK parameters of pertuzumab in healthy participants, which was approximately 20.0% [16], using Bonferroni adjustment, the true mean ratio was 0.95, and the combined power was 80.0% (the power of the comparison between groups was 97.0%). The equivalent interval for the primary endpoint was 80.0–125.0%, and α = 0.05 (two one-sided, t test). Thirty-four valuable participants were needed in each group. Considering the possible withdrawal rate was approximately 20%, the number of samples in each group was set to 40, and a total of 160 participants were enrolled.
2.8 Statistical Analysis
Statistical analysis was conducted using SAS v9.4 for Windows. PK equivalence was established if 90% confidence intervals (CIs) for the ratios of the geometric means for Cmax, AUC0–t, and AUC0–∞ were within the range 80.0–125.0%.
3 Results
3.1 Participant Disposition and Characteristics
A total of 394 participants were selected for this phase 1 clinical trial, and 234 participants were excluded due to screen failure. The 160 eligible participants were randomized 1:1:1:1 to the HLX11, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab groups (n = 40 per group). All eligible participants received the designated study treatment and were included in the PKS and the SS. One participant from the CN-pertuzumab group discontinued the study due to poor compliance (Fig. 1). Among 160 adults who received an injection, all were aged 18–45 years and weighed no less than 50 kg, and their BMIs were within the range of 19–26. The baseline characteristics were well balanced among the four groups, and the detailed demographics and baseline characteristics are shown in Table 1.
3.2 Pharmacokinetics Results
Serum drug concentration was detected by ELISA, which was fitted to form the average plasma drug concentration curve of HLX11 and the other three reference products (Fig. 2A). The logarithmic transformation of the curve is shown in Fig. 2B. At the same time, the plasma drug concentration of each participant in the four groups was fitted (see Electronic Supplementary Material ESM Figures S1A–D). It can be seen from the mean serum concentration–time profiles that after a single intravenous infusion of HLX11 and the three reference products, the profiles of each treatment group basically coincided, the mean serum concentration–time profiles of the study drugs basically coincided, and the serum concentrations were similar over time. There was no significant difference in blood concentration between the four groups after administration, which showed the high similarity of the time course of drug concentrations.
The mean serum concentration (mean ± SD)–time profiles by treatment (linear and semilogarithmic scale) (PKS). A The mean serum concentration–time profiles (linear scale), mean (± SD). B The mean serum concentration–time profiles (semilogarithmic scale). CN China, EU European Union, PK pharmacokinetic, PKS PK analysis set, SD standard deviation, US United States
A summary of serum PK parameters is shown in Table 2. After a single intravenous infusion of the four study drugs, the exposure level of the study drugs was comparable. Statistics show that for the primary evaluation parameters, the arithmetic means of the Cmax of HLX11, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab were 189.39, 178.28, 189.63, and 182.45 μg/mL, respectively; the arithmetic means of AUC0–t were 49925.9, 52876.8, 53220.2, and 53824.1 h μg/mL, respectively; and the arithmetic means of AUC0–∞ were 51259.2, 54308.4, 54390.0, and 53299.9 h μg/mL, respectively. The main PK parameters above were similar among the four groups.
The results of the PK similarity for each pairwise comparison of the primary PK endpoint (Cmax, AUC0–t, AUC0–∞) between HLX11 and the three reference pertuzumab products are summarized in Table 3. From the results, it can be seen that after a single intravenous infusion of 420 mg HLX11 and pertuzumab (US-, EU-, and CN-approved products), the 90% CIs of the geometric mean ratios (GMRs) of the primary PK parameters (Cmax, AUC0–t, AUC0–∞) ranged from 86.29 to 115.06%, all within the range of 80.0–125.00%, and analysis of variance indicated that treatment had no statistically significant effect on the primary PK parameters (Table 3).
For the secondary PK parameters, the statistical results showed that the t½ of each treatment group was very close, at 316.089, 330.392, 310.725, and 307.217 h. The CL of the four groups was 0.0085, 0.0079, 0.0080, and 0.0081 L/h, respectively, and the λz were 0.0023, 0.0022, 0.0023, and 0.0024 1/h, respectively. Other PK parameters, such as Vz and MRT, were all comparable across the four treatment groups (Table 2). For the secondary PK endpoint (Tmax), the results showed that the median values of the secondary PK parameter (Tmax) between each pair of groups were all 4.150 h, and there was no significant difference between each pairwise comparison group (Table 4).
3.3 Safety Results
The AEs occurring during the study were all treatment-emergent adverse events (TEAEs) during the treatment period, and no AEs occurred at screening. The incidence and severity of TEAEs were essentially comparable among HLX11 and the three reference products. TEAEs were reported in a total of 153 participants (95.6%), including 39 participants (97.5%) in the HLX11 group, 39 participants (97.5%) in the US-pertuzumab group, 39 (97.5%) participants in the EU-pertuzumab group, and 36 participants (90.0%) in the CN-pertuzumab group. Most of the TEAEs were grade 1 or 2 (Table 5). A total of four participants (2.5%) had grade 3 TEAEs, of which two participants had transient blood triglycerides increased, one in the HLX11 group and one in the EU-pertuzumab group each, which may not be related to the study drugs, and the other two participants experienced drug-related AEs, with one participant experiencing duodenal ulcer in the US-pertuzumab group and one participant experiencing transient proteinuria in the CN-pertuzumab group. No participants had grade 4 or grade 5 TEAEs. In all eligible participants, the most frequently reported TEAEs by preferred term (PT) were leucocytosis (54.4%), proteinuria (36.9%), hypertriglyceridaemia (30.6%), urinary tract infection (28.1%), diarrhoea (26.3%), mouth ulceration (18.8%), and hyperuricaemia (15.6%) (Table 6).
ADRs were reported in 145 participants (90.6%). Of these, ADRs were reported in 35 participants (87.5%) in the HLX11 group, 37 participants (92.5%) in the US-pertuzumab group, 37 participants (92.5%) in the EU-pertuzumab group, and 36 participants (90.0%) in the CN-pertuzumab group. The incidence of ADRs was essentially similar between HLX11 and pertuzumab (US-, EU-, and CN-approved products). By PT, the most common ADRs included leucocytosis (54.4%), proteinuria (36.9%), urinary tract infection (28.1%), diarrhoea (26.3%), mouth ulceration (18.8%), increased neutrophil count (13.1%), and rash (11.3%) (Table 7). For the common ADRs, the incidence was similar in the HLX11 group and the three reference groups.
Most of the ADRs were grade 1–2 in severity, except for the following cases: in one participant in the US-Pertuzumab group, the duodenal ulcer was grade 3, and in one participant in the CN-Pertuzumab group, the proteinuria was grade 3 (Table 8). Overall ADR severity assessments were generally similar between HLX11 and the other three reference products. No AESIs or TEAEs led to the discontinuation of study drugs, and no deaths were reported in any treatment group due to TEAEs. At the end of the study, most of the adverse reactions were recovered or improved. Thus, the safety of HLX11 and the other three reference products is similar, and all have good safety.
3.4 Immunogenicity Results
On day 15 and day 50, no participants tested positive for ADAs, and the occurrence time for ADA positivity was 1680 h (day 70) to 2352 h (day 99) in all four groups. On day 99, the incidence of ADA positivity for the HLX11, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab treatment groups was 62.50% (25/40), 37.50% (15/40), 37.50% (15/40), and 37.50% (15/40), respectively. The overall incidences of NAb positivity after infusion of HLX11, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab were low and comparable across groups, which were 0, 2.50% (1/40), 7.50% (3/40), and 2.50% (1/40), respectively (Table 9). One participant in the EU-pertuzumab group tested positive for ADA at baseline prior to study drug administration and negative for remaining visits, which was categorized as negative for overall ADA status. Because this participant did not test positive at any time after receiving the study drug, no test for NAbs was performed.
To detect the effect of immunogenicity on serum concentration, the mean drug serum concentration–time profiles on the linear and semilogarithmic scale were plotted according to the ADA/NAb (Fig. 3A–D). It can be seen that immunogenicity had no effect on the plasma concentration in the different treatment groups.
The effect of immunogenicity on serum concentration (mean ± SD) (linear and semilogarithmic scales). A Serum concentration–time profiles stratified by ADA results (linear scale) (PKS), mean (± SD). B Serum concentration–time profiles stratified by ADA results (semilogarithmic scale) (PKS), mean (± SD). C Serum concentration–time profiles stratified by NAb results (linear scale) (PKS), mean (± SD). D Serum concentration–time profiles stratified by NAb results (semilogarithmic scale) (PKS), mean (± SD). ADA anti-drug antibody, CN China, EU European Union, NAb neutralizing antibody, PK pharmacokinetic, PKS PK analysis set, SD standard deviation, US United States
To detect the effect of immunogenicity on PK parameters, PK parameters were summarized according to ADA results (Table 10). As shown from the results, after a single intravenous infusion of HLX11, US-pertuzumab, EU-pertuzumab, or CN-pertuzumab, the difference in mean values of AUC0–∞, AUC0–t, and Cmax were all less than 10% between ADA-positive participants and ADA-negative participants, and other PK parameters were comparable. The PK characteristics and the safety profile of the study drugs were not influenced by the ADA (Table 10).
4 Discussion
HLX11, a biosimilar candidate for pertuzumab, displayed comparable PK, safety, and immunogenicity profiles to US-pertuzumab in preclinical findings (data on file), which supported its clinical application potential. This trial is the first-in-human study of HLX11 and mainly focused on HLX11 to evaluate the PK profile, safety, and immunogenicity compared to the originator pertuzumab (US-, EU-, and CN-approved products) in healthy Chinese adult males. Referring to guidelines and other study documents, healthy male participants should be able to provide the most homogenous population for sensitive comparisons of the PKs of HLX11 and pertuzumab, and at the same time, to reduce the occurrence of ADA in women as much as possible, we chose males as participants in this study [17]. We found that the four drugs were bioequivalent and had similar immunogenicity and safety profiles.
HLX11 and pertuzumab (US-, EU-, and CN-approved products) had similar serum drug concentrations versus time profiles. According to the bioequivalence evaluation trial of pertuzumab biosimilars, the PK profile of HLX11 obtained in this study was similar to that of other pertuzumab biosimilars reported in healthy adults [18]. A study on pertuzumab injection (a biosimilar of pertuzumab produced by Chia Tai Tianqing Pharmaceutical Group Co., Ltd) showed that under the 90% CIs, the GMRs of the primary PK parameters of AUC0–t, Cmax, and AUC0–∞ for pertuzumab and the originator of pertuzumab (produced by Roche Pharma AG) were 100.42%, 96.71%, and 101.47%, respectively, and the 90% CIs were all within 80–125%, meeting the bioequivalence standards [19]. In this study, the results demonstrated that the four study drugs had similar mean Cmax, AUC0–t, and AUC0–∞ values. The GMRs of the primary PK parameters (Cmax, AUC0–t, AUC0–∞) for HLX11 and pertuzumab (US-, EU-, and CN-approved products) ranged from 93.40% to 105.66%, and the upper and lower bounds of the 90% CIs of Cmax, AUC0–t, and AUC0–∞ ranged from 115.06 to 87.66%, all within the range of 80.00–125.00%, indicating that HLX11 is bioequivalent to US-pertuzumab, EU-pertuzumab, and CN-pertuzumab in the PK profile. In this study, we not only compared HLX11 to the originator of pertuzumab from three different origins (US, EU, and CN), we also compared the bioequivalence between the three originator products. Results showed that under the 90% CIs, the GMRs of the primary PK parameters between the three reference products were all within the range of 80–125%. These results further indicate that HLX11 has a higher PK similarity with the reference preparations compared to other biosimilars.
The secondary objectives of this study were to assess the safety and immunogenicity of HLX11 with respect to US-pertuzumab, EU-pertuzumab, and CN-pertuzumab. Studies have shown that the administration of pertuzumab may develop immunogenicity [20]. Another study, on SHR1309, a biosimilar of pertuzumab (80 participants), showed that after administration, 12 cases (30.0%) in the pertuzumab group and 13 cases (32.5%) in the SHR-1309 group were ADA positive, and the occurrence time for ADA positivity was 1680 h (70 days) in both groups [16]. In this study, no positive ADA result was observed in any treatment group in the first 50 days, and the overall incidences of ADA and NAb positivity after infusion of the four study drugs were low and comparable across groups, which is consistent with previous reports [15, 19]. In addition, we examined the effect of immunogenicity on serum concentration, and results showed that the drug concentrations between ADA-positive and ADA-negative participants in each treatment group were similar, and the differences in the mean values of the primary PK parameters were all less than 10%; no obvious effect on PK was observed (Fig. 2A–D, Table 10). Above all, we can conclude that HLX11 and pertuzumab (US-, EU-, and CN-approved products) have similar immunogenicity.
There were no serious adverse reactions after intravenous administration of HLX11. The incidence of ADRs was essentially similar between HLX11 and the three reference products. A majority of AEs were mild, grade 1–2 in severity, except for one participant in the US-pertuzumab group, for whom the duodenal ulcer was grade 3, and in one participant in the CN-pertuzumab group, where the proteinuria was grade 3. The occurrence of these adverse reactions mentioned above is actually related to the inhibition of HER2, as previously reported [21]. There were no notable differences between the four treatment groups in clinical laboratory evaluations, electrocardiograms, echocardiograms, or vital signs. Overall ADR severity assessments were generally similar between the HLX11 and the other three reference products.
Pertuzumab has been associated with cardiotoxic events, such as heart failure [22]. To reduce this risk, we excluded participants with a history of or current cardiac disease or left ventricular ejection fraction of ≥ 55% from the study and regularly performed echocardiography and measured blood NT-proBNP concentrations (a biomarker of heart failure) after administration of the study drugs. We observed no echocardiographic or NT-proBNP abnormalities during the follow-up period in any group (Electronic Supplementary Material, ESM Table S3–5). Compared to pertuzumab (US-, EU-, and CN-approved products), HLX11 exhibits similar safety.
Comparing with the previous studies reported, the strength of this study is that it simultaneously compares the bioequivalence of HLX11 with three different sources of pertuzumab, whereas previous studies only compared to a single original drug. So, based on the PK parameter, immunogenicity, and the safety data in this phase 1 study, HLX11 may be one of the recommended candidates for pertuzumab. However, this study has limitations. First, compared to real-world clinical practice, only a limited patient population was included, which may affect its generalizability. Additionally, this study satisfactorily demonstrated the equivalence between HLX11 and the three reference products of pertuzumab, but the similarity of HLX11 and pertuzumab in clinical patients, including safety and efficacy, requires further investigation. Therefore, to further validate the equivalence between HLX11 and the reference pertuzumab, long-term observations in real-world settings are needed.
In conclusion, this study showed that HLX11 was comparable to three reference products, US-pertuzumab, EU-pertuzumab, and CN-pertuzumab, in terms of PK and safety profiles after a single intravenous infusion in healthy adult males. These data support phase 3 clinical study development of HLX11 as a pertuzumab biosimilar in the patient population. All these promising results necessitate further development of this pertuzumab biosimilar and may increase the possibility of effective treatment for patients with HER2-positive malignancies.
References
Trapani D, Ginsburg O, Fadelu T, Lin NU, Hassett M, Ilbawi AM, et al. Global challenges and policy solutions in breast cancer control. Cancer Treat Rev. 2022;104: 102339. https://doi.org/10.1016/j.ctrv.2022.102339.
Ellington T, Miller J, Henley S, Wilson R, Wu M, Richardson L. Trends in breast cancer incidence, by race, ethnicity, and age among women aged ≥20 years—United States, 1999–2018. MMWR Morb Mortal Wkly Rep. 2022;71(2):43–7. https://doi.org/10.15585/mmwr.mm7102a2.
McAndrew N. Updates on targeting human epidermal growth factor receptor 2-positive breast cancer: what’s to know in 2021. Curr Opin Obstet Gynecol. 2022;34(1):41–5. https://doi.org/10.1097/gco.0000000000000762.
Pusztai L, Yau C, Wolf D, Han H, Du L, Wallace A, et al. Durvalumab with olaparib and paclitaxel for high-risk HER2-negative stage II/III breast cancer: results from the adaptively randomized I-SPY2 trial. Cancer Cell. 2021;39(7):989-98.e5. https://doi.org/10.1016/j.ccell.2021.05.009.
Lu Y, Im S, Colleoni M, Franke F, Bardia A, Cardoso F, et al. Updated overall survival of ribociclib plus endocrine therapy vs endocrine therapy alone in pre- and perimenopausal patients with HR+/HER2− advanced breast cancer in MONALEESA-7: a phase III randomized clinical trial. Clin Cancer Res. 2021. https://doi.org/10.1158/1078-0432.Ccr-21-3032.
Beddok A, Cottu P, Fourquet A, Kirova Y. Combination of modern radiotherapy and new targeted treatments for breast cancer management. Cancers. 2021. https://doi.org/10.3390/cancers13246358.
O’Shaughnessy J, Sousa S, Cruz J, Fallowfield L, Auvinen P, Pulido C, et al. Preference for the fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection in patients with HER2-positive early breast cancer (PHranceSCa): a randomised, open-label phase II study. Eur J Cancer. 2021;152:223–32. https://doi.org/10.1016/j.ejca.2021.03.047.
Aboudaram A, Loap P, Loirat D, Dhia S, Cao K, Fourquet A, et al. Pertuzumab and trastuzumab combination with concomitant locoregional radiotherapy for the treatment of breast cancers with HER2 receptor overexpression. Cancers. 2021. https://doi.org/10.3390/cancers13194790.
Loibl S, Poortmans P, Morrow M, Denkert C, Curigliano G. Breast cancer. Lancet. 2021;397(10286):1750–69. https://doi.org/10.1016/s0140-6736(20)32381-3.
Jackisch C, Lammers P, Jacobs I. Evolving landscape of human epidermal growth factor receptor 2-positive breast cancer treatment and the future of biosimilars. Breast. 2017;32:199–216. https://doi.org/10.1016/j.breast.2017.01.010.
Paek K, Kim G, Ahn S, Lim J, Jung D, Kim S, et al. Assessment of the molecular mechanism of action of SB3, a trastuzumab biosimilar. BioDrugs. 2019;33(6):661–71. https://doi.org/10.1007/s40259-019-00381-2.
Huizinga TWJ, Torii Y, Muniz R. Adalimumab biosimilars in the treatment of rheumatoid arthritis: a systematic review of the evidence for biosimilarity. Rheumatol Ther. 2021;8(1):41–61. https://doi.org/10.1007/s40744-020-00259-8.
Partridge M, Purushothama S, Elango C, Lu Y. Emerging technologies and generic assays for the detection of anti-drug antibodies. J Immunol Res. 2016;2016:6262383. https://doi.org/10.1155/2016/6262383.
Kang H, Thorpe R, Knezevic I, Casas Levano M, Chilufya M, Chirachanakul P, et al. Regulatory challenges with biosimilars: an update from 20 countries. Ann N Y Acad Sci. 2021;1491(1):42–59. https://doi.org/10.1111/nyas.14522.
Hanes V, Chow V, Stewart T, Puri A. A randomized, double-blind, single-dose study (LAVENDER) to assess the safety, tolerability, pharmacokinetics, and immunogenicity of a combined infusion of ABP 980 and pertuzumab in healthy subjects. Cancer Chemother Pharmacol. 2021;88(5):879–86. https://doi.org/10.1007/s00280-021-04334-x.
Cui Y, Cui D, Ren X, Chen X, Liu G, Liu Z, et al. Pharmacokinetics, Immunogenicity and Safety Study for SHR-1309 Injection and Perjeta® in Healthy Chinese Male Volunteers. Front Pharmacol. 2021;12: 660541. https://doi.org/10.3389/fphar.2021.660541.
Zhang H, Liu T, Wu M, Wei H, Li C, Li X, et al. Safety and pharmacokinetics of a new biosimilar trastuzumab (HL02): a Phase I bioequivalence study in healthy Chinese men. Expert Opin Biol Ther. 2022;22(2):179–86. https://doi.org/10.1080/14712598.2021.1894121.
Zhang J, Ji D, Cai L, Yao H, Yan M, Wang X, et al. First-in-human HER2-targeted bispecific antibody KN026 for the treatment of patients with HER2-positive metastatic breast cancer: results from a phase I study. Clin Cancer Res. 2021. https://doi.org/10.1158/1078-0432.Ccr-21-2827.
Liu G, Xu Z, Yang W, Xue J, Wang Y, Liu Z, et al. A randomized, double-blind, single-dose, single-center, parallel phase I clinical study comparing the pharmacokinetics, immunogenicity, safety and tolerance of pertuzumab injection and Perjeta® in healthy Chinese male subjects. Expert Opin Biol Ther. 2021. https://doi.org/10.1080/14712598.2021.1988567.
Bekaii-Saab T, Wesolowski R, Ahn D, Wu C, Mortazavi A, Lustberg M, et al. Phase I immunotherapy trial with two chimeric HER-2 B-cell peptide vaccines emulsified in montanide ISA 720VG and Nor-MDP adjuvant in patients with advanced solid tumors. Clin Cancer Res. 2019;25(12):3495–507. https://doi.org/10.1158/1078-0432.Ccr-18-3997.
Inoue K, Takahashi M, Mukai H, Yamanaka T, Egawa C, Sakata Y, et al. Effectiveness and safety of eribulin in Japanese patients with HER2-negative, advanced breast cancer: a 2-year post-marketing observational study in a real-world setting. Investig New Drugs. 2020;38(5):1540–9. https://doi.org/10.1007/s10637-019-00890-5.
Alhussein M, Mokbel A, Cosman T, Aghel N, Yang E, Mukherjee S, et al. Pertuzumab cardiotoxicity in patients with HER2-positive cancer: a systematic review and meta-analysis. CJC Open. 2021;3(11):1372–82. https://doi.org/10.1016/j.cjco.2021.06.019.
Acknowledgements
We would like to express our gratitude to the study participants, their families, and the staff at the study site. We thank the clinical study team from Shanghai Henlius Biotech, Inc. (Ni Zhang, Guiyu Yang, Jing Li; Xiao Qi, Wenting Qiu, Jiancheng Cheng, Xue Wei, Wenying Kang; Qiyu Luo, Shiqi Zhong, Chen Hu, and Wenjie Zhang) for their support in study execution, study design, data acquisition, statistical analyses, and manuscript revisions.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was funded by Shanghai Henlius Biotech, Inc.
Conflict of interest
Guilan Sun, Liang Zhou, Qingyu Wang, and Jun Zhu are employees of Shanghai Henlius Biotech, Inc. All other authors declare that there are no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Anhui Medical University (Hefei, China) and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent
All participants provided informed consent before undergoing any study-specific procedures.
Availability of data and materials
Data are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
The manuscript was developed under the primary guidance of WH and FL. Material preparation, data collection, and analysis were performed by JY, LL, QL, QZ, GS, LZ, QW, and JZ. All authors reviewed and provided comments on the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, J., Lin, L., Long, Q. et al. HLX11, a Proposed Pertuzumab Biosimilar: Pharmacokinetics, Immunogenicity, and Safety Profiles Compared to Three Reference Biologic Products (US-, EU-, and CN-Approved Pertuzumab) Administered to Healthy Male Subjects. BioDrugs 36, 393–409 (2022). https://doi.org/10.1007/s40259-022-00534-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-022-00534-w