Abstract
Musculoskeletal pain such as osteoarthritis (OA) and low back pain (LBP) are very common and contribute to enormous burden and societal costs, despite dramatic therapeutic advances over recent decades. Novel approaches and targeted therapies are required to satisfy the urgent unmet medical need of musculoskeletal pain relief in both conditions. Nerve growth factor (NGF) inhibitors have utilized novel mechanisms different from conventional drugs, which have a variety of gastrointestinal, cardiac, or renal adverse effects. Several phase 2/3 studies have been accomplished for these drugs, such as tanezumab, fasinumab, and tyrosine receptor kinase A (TrkA) inhibitors. We searched the literature using the PubMed database and clinical trials using ClinicalTrials.gov to identify original papers, meta-analyses as well as ongoing clinical trials assessing the efficacy and safety profile of these drugs. In this narrative review, we briefly overview the disease burden of musculoskeletal pain, the role of NGF signaling and its receptors in the genesis of pain, and the mechanisms of action of inhibitors of NGF signaling and downstream pathways, and then discuss the efficacy and safety of each investigational drug in OA and LBP. Finally, we briefly review two serious adverse effects of NGF inhibitors, namely rapidly progressive OA and sympathetic system effects, and conclude with possible barriers and potential research directions to overcome these.



Similar content being viewed by others
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59.
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207–13.
Qin J, Barbour KE, Murphy LB, Nelson AE, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic hand osteoarthritis: the johnston county osteoarthritis project. Arthritis Rheumatol. 2017;69(6):1204–12.
Murphy LB, Helmick CG, Schwartz TA, Renner JB, Tudor G, Koch GG, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthr Cartil. 2010;18(11):1372–9.
International ORS. OARSI White Paper- OA as a Serious Disease. 2016.
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37.
Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–17.
Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine. 2008;33(26):2923–8.
Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–48.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333.
Conaghan PG, Peloso PM, Everett SV, Rajagopalan S, Black CM, Mavros P, et al. Inadequate pain relief and large functional loss among patients with knee osteoarthritis: evidence from a prospective multinational longitudinal study of osteoarthritis real-world therapies. Rheumatology (Oxford). 2015;54(2):270–7.
Dziedzic KS, Allen KD. Challenges and controversies of complex interventions in osteoarthritis management: recognizing inappropriate and discordant care. Rheumatology. 2018;57(4):88–98.
Tousignant-Laflamme Y, Martel MO, Joshi AB, Cook CE. Rehabilitation management of low back pain—it’s time to pull it all together! J Pain Res. 2017;10:2373–85.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–89.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. 2020;72(2):149–62.
Chetty L. A critical review of low back pain guidelines. Workplace Health Saf. 2017;65(9):388–94.
Kreiner DS, Matz P, Bono CM, Cho CH, Easa JE, Ghiselli G, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020;20(7):998–1024.
Oo WM, Yu SP, Daniel MS, Hunter DJ. Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics. Expert Opin Emerg Drugs. 2018;23(4):331–47.
Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:1225.
Oo WM, Liu X, Hunter DJ. Pharmacodynamics, efficacy, safety and administration of intra-articular therapies for knee osteoarthritis. Expert Opin Drug Metab Toxicol. 2019;15(12):1021–32.
Lim YZ, Chou L, Au RTM, Seneviwickrama KLMD, Cicuttini FM, Briggs AM, et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65(3):124–35.
de Ferreira MS, Rannou F, Hunter DJ. Osteoarthritis guidelines: barriers to implementation and solutions. Ann Phys Rehabil Med. 2016;59(3):170–3.
Oo WMLC, Duong V, Hunter DJ. The development of disease-modifying therapies for osteoarthritis (DMOADs): the evidence to date. Drug Des Devel Ther. 2021;2021(15):2921–45.
Cowan WM. Viktor hamburger and rita levi-montalcini: the path to the discovery of nerve growth factor. Annu Rev Neurosci. 2001;24(1):551–600.
Levi-Montalcini R. The nerve growth factor 35 years later. Science. 1987;237(4819):1154–62.
Chao MV. Neurotrophins and their receptors: a convergence point for many signalling pathways. Nat Rev Neurosci. 2003;4(4):299–309.
Esposito D, Patel P, Stephens RM, Perez P, Chao MV, Kaplan DR, et al. The cytoplasmic and transmembrane domains of the p75 and Trk A receptors regulate high affinity binding to nerve growth factor. J Biol Chem. 2001;276(35):32687–95.
Bibel M, Hoppe E, Barde YA. Biochemical and functional interactions between the neurotrophin receptors trk and p75NTR. Embo J. 1999;18(3):616–22.
Wehrman T, He X, Raab B, Dukipatti A, Blau H, Garcia KC. Structural and mechanistic insights into nerve growth factor interactions with the TrkA and p75 receptors. Neuron. 2007;53(1):25–38.
Marchetti L, Callegari A, Luin S, Signore G, Viegi A, Beltram F, et al. Ligand signature in the membrane dynamics of single TrkA receptor molecules. J Cell Sci. 2013;126(Pt 19):4445–56.
Marlin MC, Li G. Biogenesis and function of the NGF/TrkA signaling endosome. Int Rev Cell Mol Biol. 2015;314:239–57.
Barker PA, Mantyh P, Arendt-Nielsen L, Viktrup L, Tive L. Nerve growth factor signaling and its contribution to pain. J Pain Res. 2020;13:1223–41.
Obreja O, Rukwied R, Nagler L, Schmidt M, Schmelz M, Namer B. Nerve growth factor locally sensitizes nociceptors in human skin. Pain. 2018;159(3):416–26.
Cheng CF, Cheng JK, Chen CY, Rau RH, Chang YC, Tsaur ML. Nerve growth factor-induced synapse-like structures in contralateral sensory ganglia contribute to chronic mirror-image pain. Pain. 2015;156(11):2295–309.
Denk F, Bennett DL, McMahon SB. Nerve growth factor and pain mechanisms. Annu Rev Neurosci. 2017;40:307–25.
Wise BL, Seidel MF, Lane NE. The evolution of nerve growth factor inhibition in clinical medicine. Nat Rev Rheumatol. 2021;17(1):34–46.
McKelvey L, Shorten GD, O’Keeffe GW. Nerve growth factor-mediated regulation of pain signalling and proposed new intervention strategies in clinical pain management. J Neurochem. 2013;124(3):276–89.
Wu C, Boustany L, Liang H, Brennan TJ. Nerve growth factor expression after plantar incision in the rat. Anesthesiology. 2007;107(1):128–35.
Banik RK, Subieta AR, Wu C, Brennan TJ. Increased nerve growth factor after rat plantar incision contributes to guarding behavior and heat hyperalgesia. Pain. 2005;117(1–2):68–76.
Petty BG, Cornblath DR, Adornato BT, Chaudhry V, Flexner C, Wachsman M, et al. The effect of systemically administered recombinant human nerve growth factor in healthy human subjects. Ann Neurol. 1994;36(2):244–6.
Manni L, Lundeberg T, Fiorito S, Bonini S, Vigneti E, Aloe L. Nerve growth factor release by human synovial fibroblasts prior to and following exposure to tumor necrosis factor-alpha, interleukin-1 beta and cholecystokinin-8: the possible role of NGF in the inflammatory response. Clin Exp Rheumatol. 2003;21(5):617–24.
Aoki Y, Nakajima A, Ohtori S, Takahashi H, Watanabe F, Sonobe M, et al. Increase of nerve growth factor levels in the human herniated intervertebral disc: can annular rupture trigger discogenic back pain? Arthritis Res Ther. 2014;16(4):R159.
Freemont AJ, Watkins A, Le Maitre C, Baird P, Jeziorska M, Knight MT, et al. Nerve growth factor expression and innervation of the painful intervertebral disc. J Pathol. 2002;197(3):286–92.
Schmelz M, Mantyh P, Malfait A-M, Farrar J, Yaksh T, Tive L, et al. Nerve growth factor antibody for the treatment of osteoarthritis pain and chronic low-back pain: mechanism of action in the context of efficacy and safety. Pain. 2019;160(10):2210–20.
Shang X, Wang Z, Tao H. Mechanism and therapeutic effectiveness of nerve growth factor in osteoarthritis pain. Ther Clin Risk Manag. 2017;13:951–6.
Bothwell M. Recent advances in understanding neurotrophin signaling. F1000Res. 2016;5:2.
Abdiche YN, Malashock DS, Pons J. Probing the binding mechanism and affinity of tanezumab, a recombinant humanized anti-NGF monoclonal antibody, using a repertoire of biosensors. Protein Sci. 2008;17(8):1326–35.
Tiseo PJ, Ren H, Mellis S. Fasinumab (REGN475), an antinerve growth factor monoclonal antibody, for the treatment of acute sciatic pain: results of a proof-of-concept study. J Pain Res. 2014;7:523–30.
Owolabi JB, Rizkalla G, Tehim A, Ross GM, Riopelle RJ, Kamboj R, et al. Characterization of antiallodynic actions of ALE-0540, a novel nerve growth factor receptor antagonist, in the rat. J Pharmacol Exp Ther. 1999;289(3):1271–6.
Colquhoun A, Lawrance GM, Shamovsky IL, Riopelle RJ, Ross GM. Differential activity of the nerve growth factor (NGF) antagonist PD90780 [7-(Benzolylamino)-4,9-dihydro-4-methyl-9-oxo-pyrazolo[5,1-bquinazoline-2-carboxylic Acid] suggests altered NGF-p75NTR interactions in the presence of TrkA. J Pharmacol Exp Ther. 2004;310(2):505–11.
Niederhauser O, Mangold M, Schubenel R, Kusznir EA, Schmidt D, Hertel C. NGF ligand alters NGF signaling via p75NTR and TrkA. J Neurosci Res. 2000;61(3):263–72.
Eibl JK, Chapelsky SA, Ross GM. Multipotent neurotrophin antagonist targets brain-derived neurotrophic factor and nerve growth factor. J Pharmacol Exp Ther. 2010;332(2):446–54.
Eibl JK, Strasser BC, Ross GM. Identification of novel pyrazoloquinazolinecarboxilate analogues to inhibit nerve growth factor in vitro. Eur J Pharmacol. 2013;708(1):30–7.
Ugolini G, Marinelli S, Covaceuszach S, Cattaneo A, Pavone F. The function neutralizing anti-TrkA antibody MNAC13 reduces inflammatory and neuropathic pain. Proc Natl Acad Sci U S A. 2007;104(8):2985–90.
Nwosu LN, Mapp PI, Chapman V, Walsh DA. Blocking the tropomyosin receptor kinase A (TrkA) receptor inhibits pain behaviour in two rat models of osteoarthritis. Ann Rheum Dis. 2016;75(6):1246–54.
Watt FE, Blauwet MB, Fakhoury A, Jacobs H, Smulders R, Lane NE. Tropomyosin-related kinase A (TrkA) inhibition for the treatment of painful knee osteoarthritis: results from a randomized controlled phase 2a trial. Osteoarthr Cartil. 2019;27(11):1590–8.
Levicept Starts First-in-Human Phase I Trial of LEVI-04, A Novel Fusion Protein Therapy for Chronic Pain [press release]. b3cnewswire2017.
Janssen Announces Discontinuation of Fulranumab Phase 3 Development Program in Osteoarthritis Pain [press release]. March 31, 2016 2016.
Lane NE, Schnitzer TJ, Birbara CA, Mokhtarani M, Shelton DL, Smith MD, et al. Tanezumab for the treatment of pain from osteoarthritis of the knee. N Engl J Med. 2010;363(16):1521–31.
Katz N, Borenstein DG, Birbara C, Bramson C, Nemeth MA, Smith MD, et al. Efficacy and safety of tanezumab in the treatment of chronic low back pain. Pain. 2011;152(10):2248–58.
Mullard A. Drug developers reboot anti-NGF pain programmes. Nat Rev Drug Discov. 2015;14(5):297–8.
Hochberg MC, Tive LA, Abramson SB, Vignon E, Verburg KM, West CR, et al. When is osteonecrosis not osteonecrosis?: Adjudication of reported serious adverse joint events in the tanezumab clinical development program. Arthritis Rheumatol. 2016;68(2):382–91.
Roos EM, Klässbo M, Lohmander LS. WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol. 1999;28(4):210–5.
Verburg K. Tanezumab monoclonal antibody against nerve growth factor. 2021.
Berenbaum F, Schnitzer TJ, Kivitz AJ, Viktrup L, Hickman A, Pixton G, et al. General safety and tolerability of subcutaneous tanezumab for osteoarthritis: a pooled analysis of 3 randomized, placebo-controlled trials. Arthritis Care Res (Hoboken). 2021.
Schnitzer TJ, Lane NE, Birbara C, Smith MD, Simpson SL, Brown MT. Long-term open-label study of tanezumab for moderate to severe osteoarthritic knee pain. Osteoarthr Cartil. 2011;19(6):639–46.
Brown MT, Murphy FT, Radin DM, Davignon I, Smith MD, West CR. Tanezumab reduces osteoarthritic knee pain: results of a randomized, double-blind, placebo-controlled phase III trial. J Pain. 2012;13(8):790–8.
Brown MT, Murphy FT, Radin DM, Davignon I, Smith MD, West CR. Tanezumab reduces osteoarthritic hip pain: results of a randomized, double-blind, placebo-controlled phase III trial. Arthritis Rheum. 2013;65(7):1795–803.
Ekman EF, Gimbel JS, Bello AE, Smith MD, Keller DS, Annis KM, et al. Efficacy and safety of intravenous tanezumab for the symptomatic treatment of osteoarthritis: 2 randomized controlled trials versus naproxen. J Rheumatol. 2014;41(11):2249–59.
Balanescu AR, Feist E, Wolfram G, Davignon I, Smith MD, Brown MT, et al. Efficacy and safety of tanezumab added on to diclofenac sustained release in patients with knee or hip osteoarthritis: a double-blind, placebo-controlled, parallel-group, multicentre phase III randomised clinical trial. Ann Rheum Dis. 2014;73(9):1665–72.
Schnitzer TJ, Ekman EF, Spierings EL, Greenberg HS, Smith MD, Brown MT, et al. Efficacy and safety of tanezumab monotherapy or combined with non-steroidal anti-inflammatory drugs in the treatment of knee or hip osteoarthritis pain. Ann Rheum Dis. 2015;74(6):1202–11.
Spierings ELH, Fidelholtz J, Wolfram G, Smith MD, Brown MT, West CR. A phase III placebo- and oxycodone-controlled study of tanezumab in adults with osteoarthritis pain of the hip or knee. Pain. 2013;154(9):1603–12.
Lalovic B XR, Marshall S, Arends R. Population PK analysis of tanezumab administered to healthy volunteers subcutaneously or intravenously. Poster presented at: American Society for Clinical Pharmacology and Therapeutics (ASCPT). Atlanta, GAMarch 17–20, 2010.
Xie R AR, Olson S, Marshall S. Preliminary pharmacokinetic/ pharmacodynamic (PK/PD) analysis for the effect of tanezumab on overall daily pain score data in adults with moderate-to-severe pain due to osteoarthritis of the knee. Poster presented at: Population Approach Group in Europe (PAGE). St Petersburg, RussiaJune 23–26, 2009.
Birbara C, Dabezies EJ Jr, Burr AM, Fountaine RJ, Smith MD, Brown MT, et al. Safety and efficacy of subcutaneous tanezumab in patients with knee or hip osteoarthritis. J Pain Res. 2018;11:151–64.
Schnitzer TJ, Easton R, Pang S, Levinson DJ, Pixton G, Viktrup L, et al. Effect of tanezumab on joint pain, physical function, and patient global assessment of osteoarthritis among patients with osteoarthritis of the hip or knee: a randomized clinical trial. JAMA. 2019;322(1):37–48.
Schnitzer TJ, Khan A, Bessette L, Davignon I, Brown MT, Pixton G, et al. Onset and maintenance of efficacy of subcutaneous tanezumab in patients with moderate to severe osteoarthritis of the knee or hip: A 16-week dose-titration study. Semin Arthritis Rheum. 2020;50(3):387–93.
Berenbaum F, Blanco FJ, Guermazi A, Miki K, Yamabe T, Viktrup L, et al. Subcutaneous tanezumab for osteoarthritis of the hip or knee: efficacy and safety results from a 24-week randomised phase III study with a 24-week follow-up period. Ann Rheum Dis. 2020;79(6):800–10.
Hochberg MC, Carrino JA, Schnitzer TJ, Guermazi A, Walsh DA, White A, et al. Long-Term Safety and Efficacy of Subcutaneous Tanezumab Versus Nonsteroidal Antiinflammatory Drugs for Hip or Knee Osteoarthritis: A Randomized Trial. Arthritis Rheumatol. 2021.
David Hunter TN, Melvin Churchill, Ivan Shirinsky, Masanari Omata, Alexander White, Ali Guermazi, Robert Fountaine, Glenn Pixton, Lars Viktrup, Mark Brown, Christine West and Kenneth Verburg. Clinically Important Improvements in Patients with Osteoarthritis Treated with Subcutaneous Tanezumab: Results from a 56-Week Randomized NSAID-Controlled Study [abstract]. Arthritis Rheumatol. 2020;2020; 72 (suppl 10).
Marc C. Hochberg JC, Thomas Schnitzer, Ali Guermazi, David Walsh, Alexander White, Satoru Nakajo, Robert Fountaine, Anne Hickman, Glenn Pixton, Lars Viktrup, Mark T. Brown, Christine R. West and Kenneth M. Verburg Subcutaneous Tanezumab versus NSAID for the Treatment of Osteoarthritis: Joint Safety Events in a Randomized, Double-Blind, Active-Controlled, 80-Week, Phase-3 Study [Abstract]. Arthritis Rheumatol 2019;2019; 71 (suppl 10).
Schnitzer TJ, Marks JA. A systematic review of the efficacy and general safety of antibodies to NGF in the treatment of OA of the hip or knee. Osteoarthr Cartil. 2015;23(Suppl 1):S8-17.
Kan SL, Li Y, Ning GZ, Yuan ZF, Chen LX, Bi MC, et al. Tanezumab for patients with osteoarthritis of the knee: a meta-analysis. PLoS ONE. 2016;11(6):e0157105.
Chen J, Li J, Li R, Wang H, Yang J, Xu J, et al. Efficacy and safety of tanezumab on osteoarthritis knee and hip pains: a meta-analysis of randomized controlled trials. Pain Med. 2017;18(2):374–85.
Tive L, Bello AE, Radin D, Schnitzer TJ, Nguyen H, Brown MT, et al. Pooled analysis of tanezumab efficacy and safety with subgroup analyses of phase III clinical trials in patients with osteoarthritis pain of the knee or hip. J Pain Res. 2019;12:975–95.
Yang S, Huang Y, Ye Z, Li L, Zhang Y. The efficacy of nerve growth factor antibody for the treatment of osteoarthritis pain and chronic low-back pain: a meta-analysis. Front Pharmacol. 2020;11:817.
Song GG, Lee YH. Relative efficacy and tolerability of 2.5, 5, and 10 mg tanezumab for the treatment of osteoarthritis: A Bayesian network meta-analysis of randomized controlled trials based on patient withdrawal. Int J Clin Pharmacol Ther. 2021;59(2):147–55.
Fan ZR, Ma JX, Wang Y, Chen HT, Lang S, Ma XL. Efficacy and safety of tanezumab administered as a fixed dosing regimen in patients with knee or hip osteoarthritis: a meta-analysis of randomized controlled phase III trials. Clin Rheumatol. 2021;40(6):2155–65.
Cao Z, Zhou J, Long Z, Li Y, Sun J, Luo Y, et al. Targeting nerve growth factor, a new option for treatment of osteoarthritis: a network meta-analysis of comparative efficacy and safety with traditional drugs. Aging (Albany NY). 2020;13(1):1051–70.
Yu Y, Lu ST, Sun JP, Zhou W. Safety of low-dose tanezumab in the treatment of hip or knee osteoarthritis: a systemic review and meta-analysis of randomized phase III clinical trials. Pain Med. 2021;22(3):585–95.
Kepplinger EE. FDA’s expedited approval mechanisms for new drug products. Biotechnol Law Rep. 2015;34(1):15–37.
Pfizer. Pfizer and lilly receive FDA fast track designation for tanezumab. 2017.
Pfizer. Joint FDA advisory committee votes on application for tanezumab for the treatment of osteoarthritis Pain. 2021.
Tiseo PJ, Kivitz AJ, Ervin JE, Ren H, Mellis SJ. Fasinumab (REGN475), an antibody against nerve growth factor for the treatment of pain: results from a double-blind, placebo-controlled exploratory study in osteoarthritis of the knee. Pain. 2014;155(7):1245–52.
Ghilardi JR, Freeman KT, Jimenez-Andrade JM, Mantyh WG, Bloom AP, Kuskowski MA, et al. Administration of a tropomyosin receptor kinase inhibitor attenuates sarcoma-induced nerve sprouting, neuroma formation and bone cancer pain. Mol Pain. 2010;6:87.
Flannery CR, Moran N, Blasioli D, Donahue K, Kane J, Gladysheva T, et al. Efficacy of a novel, locally delivered TrkA inhibitor in preclinical models of OA and joint pain. Osteoarthr Cartil. 2015;23:A45–6.
Krupka E, Jiang GL, Jan C. Efficacy and safety of intra-articular injection of tropomyosin receptor kinase A inhibitor in painful knee osteoarthritis: a randomized, double-blind and placebo-controlled study. Osteoarthr Cartil. 2019;27(11):1599–607.
Walsh DA, Neogi T. A tale of two TrkA inhibitor trials: same target, divergent results. Osteoarthr Cartil. 2019;27(11):1575–7.
Doshi TL, Tesarz J, Cohen SP. Nerve growth factor inhibitors for low back pain: balancing the risks and benefits. Pain. 2020;161(9):1941–2.
Kivitz AJ, Gimbel JS, Bramson C, Nemeth MA, Keller DS, Brown MT, et al. Efficacy and safety of tanezumab versus naproxen in the treatment of chronic low back pain. Pain. 2013;154(7):1009–21.
Gimbel JS, Kivitz AJ, Bramson C, Nemeth MA, Keller DS, Brown MT, et al. Long-term safety and effectiveness of tanezumab as treatment for chronic low back pain. Pain. 2014;155(9):1793–801.
Leite VF, Buehler AM, El Abd O, Benyamin RM, Pimentel DC, Chen J, et al. Anti-nerve growth factor in the treatment of low back pain and radiculopathy: a systematic review and a meta-analysis. Pain Physician. 2014;17(1):E45-60.
Markman JD, Bolash RB, McAlindon TE, Kivitz AJ, Pombo-Suarez M, Ohtori S, et al. Tanezumab for chronic low back pain: a randomized, double-blind, placebo- and active-controlled, phase 3 study of efficacy and safety. Pain. 2020;161(9):2068–78.
Ashworth J, Green DJ, Dunn KM, Jordan KP. Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up? Pain. 2013;154(7):1038–44.
Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350:6380.
Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev. 2016;2(2):012087.
Dakin P, Kivitz AJ, Gimbel JS, Skrepnik N, DiMartino SJ, Emeremni CA, et al. Efficacy and safety of fasinumab in patients with chronic low back pain: a phase II/III randomised clinical trial. Ann Rheum Dis. 2020;80(4):509–17.
Miller CG, Guermazi A, Roemer F. The current status of imaging in anti-NGF clinical trials. Osteoarthr Cartil. 2015;23(Suppl 1):S3-7.
Chisholm KA, Gilchrist JM. The Charcot joint: a modern neurologic perspective. J Clin Neuromuscul Dis. 2011;13(1):1–13.
Huskisson EC, Berry H, Gishen P, Jubb RW, Whitehead J. Effects of antiinflammatory drugs on the progression of osteoarthritis of the knee. LINK Study Group. Longitudinal Investigation of Nonsteroidal Antiinflammatory Drugs in Knee Osteoarthritis. J Rheumatol. 1995;22(10):1941–6.
Tomlinson RE, Li Z, Li Z, Minichiello L, Riddle RC, Venkatesan A, et al. NGF-TrkA signaling in sensory nerves is required for skeletal adaptation to mechanical loads in mice. Proc Natl Acad Sci U S A. 2017;114(18):E3632–41.
LaBranche TP, Bendele AM, Omura BC, Gropp KE, Hurst SI, Bagi CM, et al. Nerve growth factor inhibition with tanezumab influences weight-bearing and subsequent cartilage damage in the rat medial meniscal tear model. Ann Rheum Dis. 2017;76(1):295–302.
Xu L, Nwosu LN, Burston JJ, Millns PJ, Sagar DR, Mapp PI, et al. The anti-NGF antibody muMab 911 both prevents and reverses pain behaviour and subchondral osteoclast numbers in a rat model of osteoarthritis pain. Osteoarthr Cartil. 2016;24(9):1587–95.
Karsdal MA, Verburg KM, West CR, Bay-Jensen AC, Keller DS, Arends R. Serological biomarker profiles of rapidly progressive osteoarthritis in tanezumab-treated patients. Osteoarthr Cartil. 2019;27(3):484–92.
Roemer FW, Miller CG, West CR, Brown MT, Sherlock SP, Kompel AJ, et al. Development of an imaging mitigation strategy for patient enrolment in the tanezumab nerve growth factor inhibitor (NGF-ab) program with a focus on eligibility assessment. Semin Arthritis Rheum. 2017;47(3):323–30.
Losina E, Michl G, Collins JE, Hunter DJ, Jordan JM, Yelin E, et al. Model-based evaluation of cost-effectiveness of nerve growth factor inhibitors in knee osteoarthritis: impact of drug cost, toxicity, and means of administration. Osteoarthr Cartil. 2016;24(5):776–85.
FDA panel rejects Pfizer's tanezumab for osteoarthritis pain over risk-benefit doubts [press release]. Healio Rheumatology, March 25, 2021 2021.
Belanger P, Butler P, Butt M, Bhatt S, Foote S, Shelton D, et al. From the cover: Evaluation of the effects of tanezumab, a monoclonal antibody against nerve growth factor, on the sympathetic nervous system in adult cynomolgus monkeys (Macaca fascicularis): a stereologic, histomorphologic, and cardiofunctional assessment. Toxicol Sci. 2017;158(2):319–33.
Brown M, Koltzenburg M, Nguyen H, West C, Verburg K. Tanezumab does not cause sympathetic nervous system dysfunction in clinical osteoarthritis studies (P3.303). Neurology. 2015;84(14):P3303.
Malfait A-M, Miller RE, Block JA. Targeting neurotrophic factors: Novel approaches to musculoskeletal pain. Pharmacol Therap. 2020;211:107553.
Block JA. OA guidelines: improving care or merely codifying practice? Nat Rev Rheumatol. 2014;10(6):324–6.
Oo WM, Yu SP-C, Daniel MS, Hunter DJ. Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics. Exp Opin Emerg Drugs. 2018;23(4):331–47.
Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Rheum Dis Clin North Am. 2008;34(3):623–43.
Acknowledgements
WMO is supported by the Presidential Scholarship of Myanmar for his PhD course. DJH is supported by an NHMRC Investigator Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was acquired for this work.
Conflicts of interest
WMO has no conflicts of interest. DJH provides consulting advice on scientific advisory boards for Pfizer, Lilly, TLCBio, Novartis, Tissuegene, and Biobone.
Author contributions
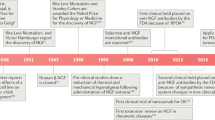
WMO and DJH contributed to the study concept and design. WMO conducted the data search, constructed the illustrations, and drafted the first version of the manuscript. DJH and WMO critically revised the manuscript for important intellectual content.
Ethics approval
Not applicable.
Consent to participate/publish
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Rights and permissions
About this article
Cite this article
Oo, W.M., Hunter, D.J. Nerve Growth Factor (NGF) Inhibitors and Related Agents for Chronic Musculoskeletal Pain: A Comprehensive Review. BioDrugs 35, 611–641 (2021). https://doi.org/10.1007/s40259-021-00504-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-021-00504-8