Abstract
Subcutaneous MYL1501D insulin glargine 100 U/mL (hereafter referred to as MYL1501D insulin glargine) [Semglee®] is a long-acting human insulin analogue approved as a biosimilar of insulin glargine 100 U/mL (hereafter referred to as reference insulin glargine 100 U/mL) [Lantus®] in various countries, including those of the EU for the treatment of diabetes mellitus in patients aged ≥ 2 years, as well as Japan for diabetes where insulin therapy is indicated. MYL1501D insulin glargine has similar physicochemical characteristics and biological properties to those of EU- and US-sourced reference insulin glargine 100 U/mL, with the bioequivalence of pharmacodynamic and pharmacokinetic parameters between these agents shown in adults with type 1 diabetes. Once-daily MYL1501D insulin glargine demonstrated noninferior glycaemic efficacy to that of once-daily reference insulin glargine 100 U/mL in adults with type 1 or 2 diabetes, with its glycated haemoglobin-lowering benefits maintained over the longer-term (52 weeks) and unaffected by previous insulin exposure. Switching between MYL1501D insulin glargine and reference insulin glargine 100 U/mL did not appear to impact glycaemic efficacy in adults with type 1 diabetes. MYL1501D insulin glargine was well tolerated, demonstrating a safety and immunogenicity profile similar to that of reference insulin glargine 100 U/mL in patients with type 1 and 2 diabetes, and in those with type 1 diabetes switching between the two agents. As expected, hypoglycaemia was the most frequently reported treatment-emergent adverse event. Thus, MYL1501D insulin glargine provides an effective biosimilar alternative for patients requiring insulin glargine therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Biosimilar to reference insulin glargine 100 U/mL |
Similar pharmacodynamic and pharmacokinetic parameters to EU- and US-sourced reference insulin glargine 100 U/mL in adults with type 1 diabetes |
Noninferior glycaemic efficacy and a similar safety and immunogenicity profile to reference insulin glargine 100 U/mL in adults with type 1 or 2 diabetes |
Switching between MYL1501D insulin glargine and reference insulin glargine 100 U/mL did not appear to impact glycaemic efficacy in adults with type 1 diabetes |
1 Introduction
Diabetes poses a considerable public health challenge [1]. When uncontrolled, the resultant hyperglycaemia gradually damages blood vessels, nerves and other tissues, with diabetes ranked among the leading causes of blindness, cardiovascular disease, kidney failure and lower limb amputation [1].
The most effective and consistent way of controlling blood glucose levels in patients with diabetes is insulin therapy [2], with the development of long-acting insulin analogues (e.g. insulin glargine) overcoming some of the limitations (e.g. variable absorption, hypoglycaemia) associated with the use of older (shorter-acting) insulins (e.g. NPH insulin) [3]. While the introduction of long-acting insulin analogues has influenced the management of diabetes, these agents tend to be associated with substantial costs [3, 4]. Biosimilar or follow-on biological insulins are insulins with demonstrated similarity (in purity, potency and safety) to an approved insulin analogue (i.e. the reference product) [4].
Subcutaneous MYL1501D insulin glargine 100 U/mL (hereafter referred to as MYL1501D insulin glargine) [Semglee®] is a long-acting human insulin analogue approved as a biosimilar of insulin glargine 100 U/mL (hereafter referred to as reference insulin glargine 100 U/mL) [Lantus®] in various countries, including those of the EU for the treatment of diabetes mellitus in patients aged ≥ 2 years [5], as well as Japan for diabetes where insulin therapy is indicated [6] (Sect. 5). This article summarizes the key pharmacological properties of MYL1501D insulin glargine and reviews therapeutic efficacy and tolerability data relevant to its use in the treatment of this patient population.
2 Pharmacological Properties of MYL1501D Insulin Glargine
MYL1501D insulin glargine is a long-acting human insulin analogue manufactured by recombinant DNA technology in Pichia pastoris (a yeast) [5]. It has similar physicochemical characteristics and biological properties to those of EU- and US-sourced reference insulin glargine 100 U/mL [7], with a dose of 0.4 U/kg demonstrating pharmacodynamic and pharmacokinetic bioequivalence to 0.4 U/kg of EU- and US-sourced reference insulin glargine 100 U/mL in a randomized, double-blind, phase I, crossover study in 113 adults with type 1 diabetes [8] (Table 1). The three-way crossover design of this study permitted the demonstration of pharmacodynamic and pharmacokinetic bioequivalence between EU- and US-sourced reference insulin glargine 100 U/mL, establishing a three-way bridge between MYL1501D insulin glargine, EU-sourced reference insulin glargine 100 U/mL and US-sourced reference insulin glargine 100 U/mL (data from an abstract) [9].
3 Therapeutic Efficacy of MYL1501D Insulin Glargine
Two open-label, multinational, phase III, noninferiority studies in adults with diabetes evaluated the glycaemic efficacy of subcutaneous MYL1501D insulin glargine compared with subcutaneous reference insulin glargine 100 U/mL [10, 11]. INSTRIDE 1 was conducted in patients with type 1 diabetes who had a glycated haemoglobin (HbA1c) level of ≤ 9.5% [10], while INSTRIDE 2 was conducted in patients with type 2 diabetes who had an HbA1c level of 7.5–10.5% (insulin-naïve patients) or < 10.5% (insulin-experienced patients) and had received a stable oral antidiabetic drug (OAD) dosage for the previous ≥ 3 months [11]. Patients in INSTRIDE 1, and those in INSTRIDE 2 who were not insulin-naïve had received reference insulin glargine 100 U/mL once daily for the previous ≥ 3 months [10, 11]. At baseline, patient characteristics were generally similar between the treatment groups. The change from baseline at week 24 in HbA1c levels was the primary endpoint. Analyses were conducted in the intent-to-treat population [10, 11].
3.1 In Type 1 Diabetes
Patients initially underwent a 6-week run-in period during which they received reference insulin glargine 100 U/mL once daily [titrated weekly to achieve a fasting plasma glucose (FPG) level of 3.9–7.2 mmol/L] and subcutaneous insulin lispro three times daily (titrated weekly to achieve a 2-h postprandial blood glucose level of 10.0 mmol/L), after which they were randomized to receive MYL1501D insulin glargine (n = 280) or reference insulin glargine 100 U/mL once daily (n = 278) in combination with insulin lispro (at a dose equivalent to that of the pre-study mealtime insulin) three times daily for 52 weeks [10]. Doses were titrated weekly for the first 4 weeks of therapy, and then (unless required for patient safety) every 4 weeks thereafter [10].
MYL1501D insulin glargine provided noninferior glycaemic efficacy to reference insulin glargine 100 U/mL in terms of the change from baseline in HbA1c levels at week 24 (primary endpoint), with no significant between-group difference in this endpoint seen at week 52 [10] (Table 2). Moreover, the two groups did not significantly differ with respect to the proportion of patients achieving an HbA1c level of < 7% at weeks 24 and 52 (Table 2) and actual HbA1c levels over the 52-week treatment period (with values decreasing during the run-in period, after which they increased in a small but non-significant manner to study end) [10].
With regard to other endpoints, there were no statistically significant differences between patients receiving MYL1501D insulin glargine and those receiving reference insulin glargine 100 U/mL in the changes from baseline in FPG levels, SMBG levels and the daily basal insulin dose at all of the timepoints assessed [weeks 12 (FPG levels), 24, 36 (FPG levels) and 52], apart from statistically significant between-group differences in the change from baseline in both FPG levels and the daily basal insulin dose at week 24 [10] (Table 2). Of note, the reduction from baseline in FPG levels at week 24 was not considered to be clinically relevant [7]. The changes from baseline in the daily total insulin dose and the daily mealtime insulin dose did not significantly differ between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups at any post-baseline visit, except for the daily total insulin dose at week 20 (+ 0.0245 vs + 0.0071 U/kg; p = 0.04), although this difference was not considered to be clinically relevant [10]. Moreover, while a statistically significant (p < 0.001) change from baseline at week 52 in mean bodyweight was seen in both the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups (+ 1.04 vs + 0.88 kg), the between-group difference in this endpoint was not statistically significant [10].
3.1.1 Switching to MYL1501D Insulin Glargine
Patients who completed 52 weeks’ therapy with reference insulin glargine 100 U/mL in INSTRIDE 1 were eligible to enter an open-label, multinational, phase III switching study (INSTRIDE 3) [12]. In this study, patients were randomized to two treatment sequence groups:
MYL1501D insulin glargine for 12 weeks, followed by reference insulin glargine 100 U/mL for 12 weeks and then MYL1501D insulin glargine for 12 weeks (n = 64)
Reference insulin glargine 100 U/mL for 36 weeks (n = 63)
The initial doses of both MYL1501D insulin glargine and reference insulin glargine 100 U/mL were adapted to the actual blood glucose levels of the patient. Patients in both groups also received insulin lispro three times daily. At baseline, patient and disease characteristics were generally similar between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups; mean HbA1c levels were 7.6% and 7.9%. The primary endpoint was the change from baseline to week 36 in HbA1c levels. Analyses were conducted in the intent-to-treat population [12].
Switching between MYL1501D insulin glargine and reference insulin glargine 100 U/mL resulted in equivalent glycaemic efficacy, with the least-squares mean (LSM) difference between the treatment sequence groups in the LSM change from baseline to week 36 in HbA1c levels having 95% CIs that were within the prespecified equivalence margin of ± 0.4% [− 0.05% vs − 0.06%; 0.01% (95% CI − 0.085 to + 0.101)] [12]. HbA1c, FPG and SMBG levels and the daily total insulin dose in both treatment sequence groups remained comparatively stable throughout the study, with no statistically significant (HbA1c levels and the daily total insulin dose) or clinically relevant (FPG and SMBG levels) changes from baseline and/or between the treatment sequence groups seen at any timepoint. Moreover, no clinically relevant changes from baseline and/or between the treatment sequence groups in the daily basal insulin dose and the daily mealtime insulin dose were seen at any timepoint [12].
3.2 In Type 2 Diabetes
In INSTRIDE 2, patients were randomized to receive MYL1501D insulin glargine (n = 274) or reference insulin glargine 100 U/mL (n = 278) [titrated weekly for the first 12 weeks of therapy to achieve a fasting pre-prandial SMBG level of 3.9–7.2 mmol/L] in combination with OAD therapy for 24 weeks, with 0.2 U/kg once daily the recommended starting dosage in patients not currently receiving insulin therapy [11].
MYL1501D insulin glargine was noninferior to reference insulin glargine 100 U/mL in improving glycaemic control (as assessed by the change from baseline in HbA1c levels at week 24) [11] (Table 2). Of note, improvements in this endpoint were seen early (mean change from baseline at week 12 of − 0.57% and − 0.59%), with the two groups not significantly differing in actual HbA1c levels over time [11].
In terms of other endpoints, there were no significant differences between MYL1501D insulin glargine and reference insulin glargine 100 U/mL in the change from baseline to week 24 in FPG levels, SMBG levels and the daily basal insulin dose (Table 2), although statistically significant reductions from baseline in SMBG levels were seen at all assessed timepoints [11]. Moreover, while mean bodyweight increased from baseline to week 24 by a statistically significant (p < 0.05) extent in both the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups (0.67 vs 0.42 kg), the between-group difference in this endpoint was not significant at either week 12 or week 24 [11].
HbA1c-lowering benefits did not significantly differ between MYL1501D insulin glargine and reference insulin glargine 100 U/mL regardless of previous insulin exposure, with LSM changes from baseline in HbA1c levels at week 24 of − 1.01% and − 1.09% (95% CI for the between-group difference of − 0.19 and 0.37) in insulin-naïve patients (n = 112 and 115) and − 0.15% and − 0.21% in insulin-experienced patients (n = 162 and 163). Moreover, in insulin-naïve patients, there was no significant between-group difference in the mean increase from baseline to week 24 in the daily basal insulin dose (0.24 vs 0.24 U/kg) [11].
4 Tolerability of MYL1501D Insulin Glargine
MYL1501D insulin glargine was well tolerated, with a safety profile similar to that of reference insulin glargine 100 U/mL, when administered in combination with insulin lispro in patients with type 1 diabetes (INSTRIDE 1) [10] or OADs in patients with type 2 diabetes (INSTRIDE 2) [11]. Of note, the safety profile of reference insulin glargine 100 U/mL in children and adolescents (i.e. patients aged ≤ 18 years) is generally similar to that in adults [5].
Treatment-emergent adverse events (TEAEs) were reported in 80.4% of 280 MYL1501D insulin glargine recipients and 86.0% of 278 reference insulin glargine 100 U/mL recipients in INSTRIDE 1 [7, 10] and in 64.1% of 276 and 58.2% of 282 patients in INSTRIDE 2 [11]; the difference between the groups was not significant in either study. Of note, previous insulin exposure did not appear to affect the TEAE profile of MYL1501D insulin glargine in patients with type 2 diabetes [11]. Most TEAEs reported in INSTRIDE 1 and 2 were mild or moderate in severity, with the incidence of grade ≥ 3 (i.e. severe [10]) TEAEs not significantly differing between the respective treatment groups in both studies (INSTRIDE 1: 8.2% vs 8.3% of patients [7, 10]; INSTRIDE 2: 2.9% vs 4.6% [11]). Treatment discontinuation because of TEAEs occurred in ≤ 1.1% of patients in each treatment group of both studies (with the between-group differences not statistically significant) [7, 10, 11].
Hypoglycaemia is generally the most common adverse reaction associated with insulin therapy [5]. Indeed, it was the most frequently reported TEAE in both studies (where it was defined as a SMBG level of ≤ 3.9 mmol/L), occurring in 55.0% and 61.2% of patients receiving MYL1501D insulin glargine or reference insulin glargine 100 U/mL in INSTRIDE 1 [10] and in 27.2% and 23.4% of patients in INSTRIDE 2 [11]. Notably, both the incidences and rates (episodes/30 days) of overall and nocturnal hypoglycaemia did not significantly differ between the treatment groups at any assessed timepoint throughout INSTRIDE 1 and 2 [10, 11]. Where reported [11], 22.5% of MYL1501D insulin glargine recipients and 19.9% of reference insulin glargine 100 U/mL recipients experienced treatment-related hypoglycaemia. At least one severe hypoglycaemic event occurred in 3.9% of MYL1501D insulin glargine recipients and 4.7% of reference insulin glargine 100 U/mL recipients in INSTRIDE 1, with ≥ 1 severe nocturnal hypoglycaemic event reported in 2.9% and 2.5% of patients [10]. In INSTRIDE 2, one patient (receiving reference insulin glargine 100 U/mL) experienced a severe nocturnal hypoglycaemic episode during the first week of therapy [11].
The other most frequently reported (incidence > 5% in either treatment group of both studies) TEAE in the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups was upper respiratory tract infection [9.6% vs 11.9% (statistical significance not reported) of patients in INSTRIDE 1 [10] and 6.2% vs 5.3% (with the between-group difference not statistically significant) in INSTRIDE 2 [11]]. Of note, the proportion of patients with ≥ 1 local and systemic reaction during the treatment period was low and did not significantly differ between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups in both INSTRIDE 1 (1.8% vs 2.2%) [10] and INSTRIDE 2 (1.4% vs 0.7%) [11].
Of the three deaths (two MYL1501D insulin glargine recipients and one reference insulin glargine 100 U/mL recipient) in INSTRIDE 1, one (believed to result from hypoglycaemia) in a patient receiving MYL1501D insulin glargine and insulin lispro was considered to be probably related to the treatment regimen and possibly related to insulin lispro [10]. No patients in INSTRIDE 2 died [11].
MYL1501D insulin glargine was also well tolerated, with a safety profile similar to that of reference insulin glargine 100 U/mL, in patients with type 1 diabetes switching between the two drugs in INSTRIDE 3 [12]. Indeed, the incidence of TEAEs, overall hypoglycaemic events and nocturnal hypoglycaemic events did not significantly differ between the treatment sequences, with the incidence (64.1% and 66.7% of patients) and severity (most were mild or moderate) of TEAEs between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL treatment sequences in keeping with those reported in INSTRIDE 1 and 2 [12].
4.1 Immunogenicity
The immunogenicity profile of MYL1501D insulin glargine was similar to that of reference insulin glargine 100 U/mL in patients with type 1 [10] and 2 [11] diabetes, and in those switching between the two agents [12].
In INSTRIDE 1, there was no statistically significant difference between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups in any insulin antibody type at any assessed timepoints during the treatment period [10]. For instance, in the respective treatment groups, a total anti-drug antibody (ADA) response was demonstrated in 69.3% and 70.9% of patients at week 24 and in 67.1% and 66.5% at week 52 (data from an abstract) [13]. In INSTRIDE 2, the proportions of patients who were total ADA-negative (63.4% vs 61.3%), insulin cross-reactive antibody-negative (62.7% vs 62.8%), total ADA-positive (25.4% vs 27.0%) and insulin cross-reactive antibody-positive (26.1% vs 25.5%) did not significantly differ between the MYL1501D insulin glargine and reference insulin glargine 100 U/mL groups [11]. In the switching study, there was no significant difference between the MYL1501D insulin glargine treatment sequence and the reference insulin glargine 100 U/mL treatment sequence in the treatment-emergent antibody response rate (14.1% vs 14.3%) [12].
5 Dosage and Administration of MYL1501D Insulin Glargine
MYL1501D insulin glargine, available as a 100 U/mL solution for subcutaneous injection, is approved in the EU for the treatment of diabetes mellitus in patients aged ≥ 2 years [5, 14] and in Japan for the treatment of diabetes where insulin therapy is indicated [6]. It can be administered concomitantly with OADs in patients with type 2 diabetes [5] or with other insulin preparations [6].
MYL1501D insulin glargine should be administered once daily (at the same time each day) into the abdomen, deltoid or thigh, with both the dose and the timing of administration individually adjusted [5, 6]. It is not the insulin of choice for treating diabetic ketoacidosis, and patients receiving it concomitantly with pioglitazone should be monitored for the signs and symptoms of heart failure, oedema and weight gain (as cardiac failure cases have been reported with the combined use of pioglitazone and insulin) [5].
Local prescribing information should be consulted for detailed information regarding switching patients from other insulins (including insulin glargine 300 U/mL) to MYL1501D insulin glargine, contraindications, potential drug interactions, use in special patient populations (as insulin requirements may be reduced), and warning and precautions.
6 Current Status of MYL1501D Insulin Glargine in Diabetes Mellitus
The 2015 expiration of the patent for reference insulin glargine 100 U/mL opened up the market to biosimilars/follow-on biologicals [15, 16]. LY2963016 insulin glargine was the first of these, being approved in the EU as a biosimilar and in the USA as a follow-on biological to reference insulin glargine 100 U/mL [17]. More recently, MYL1501D insulin glargine was approved in the EU as a biosimilar of reference insulin glargine 100 U/mL for the treatment of diabetes mellitus in patients aged ≥ 2 years [5].
MYL1501D insulin glargine is a recombinant human insulin analogue (Sect. 2). It has similar physicochemical characteristics and biological properties to those of EU- and US-sourced reference insulin glargine 100 U/mL, and the pharmacodynamic and pharmacokinetic bioequivalence of these agents has been shown in adults with type 1 diabetes (Sect. 2). In adults with type 1 diabetes (INSTRIDE 1) or type 2 diabetes (INSTRIDE 2), MYL1501D insulin glargine demonstrated noninferior efficacy to that of reference insulin glargine 100 U/mL in the change from baseline in HbA1c levels at week 24 (primary endpoint) [Sect. 3]. Moreover, HbA1c-lowering benefits were maintained over the longer-term (52 weeks) in INSTRIDE 1 (Sect. 3.1) and were unaffected by previous insulin exposure in INSTRIDE 2 (Sect. 3.2). For the most part, the change from baseline in other efficacy endpoints (including FBG levels, SMBG levels, the daily basal insulin dose and bodyweight) did not significantly differ between patients receiving MYL1501D insulin glargine and those receiving reference insulin glargine 100 U/mL at all timepoints (Sect. 3). Switching between MYL1501D insulin glargine and reference insulin glargine 100 U/mL did not appear to impact glycaemic efficacy in adults with type 1 diabetes (INSTRIDE 3), with the change from baseline to week 36 in HbA1c levels considered equivalent, and HbA1c, FPG and SMBG levels and the daily total insulin dose remaining comparatively stable over the study (Sect. 3.1.1).
MYL1501D insulin glargine was well tolerated in the INSTRIDE studies, demonstrating a safety and immunogenicity profile similar to that of reference insulin glargine 100 U/mL in patients with type 1 and 2 diabetes, and in those with type 1 diabetes switching between the two agents (Sect. 4). As expected, hypoglycaemia was the most frequently reported TEAE (Sect. 4); of note, owing to its more sustained basal insulin supply, less nocturnal, but more early morning hypoglycaemia can be expected with MYL1501D insulin glargine therapy [5].
Given the growing prevalence of diabetes and the ever increasing cost of healthcare, it is hoped that the introduction of biosimilar or follow-on biological insulins will increase market competition and thus lower costs [1, 15, 16]. Well-designed cost-effectiveness analyses of the use of biosimilar or follow-on biological insulin glargine would be of interest.
In conclusion, MYL1501D insulin glargine has similar physicochemical characteristics, biological properties, pharmacodynamic and pharmacokinetic parameters, efficacy and safety to reference insulin glargine 100 U/mL in adults with type 1 or 2 diabetes, proving an effective biosimilar alternative for patients requiring insulin glargine therapy.
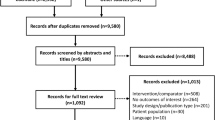
Data Selection MYL1501D Insulin Glargine: 57 records identified
Duplicates removed | 12 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 19 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 9 |
Cited efficacy/tolerability articles | 4 |
Cited articles not efficacy/tolerability | 13 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Insulin glargine MYL-1501D, Semglee, Type 1 diabetes, Type 2 diabetes. Records were limited to those in English language. Searches last updated 16 March 2020 | |
Change history
12 May 2020
The article MYL1501D Insulin Glargine: A Review in Diabetes Mellitus, written by Sheridan M.
References
European Coalition for Diabetes. Diabetes in Europe: policy puzzle. 2014. https://d-net.idf.org/en/library/281-diabetes-in-europe-policy-puzzle-the-state-we-are-in.html. Accessed 9 Mar 2020.
Owens DR, Matfin G, Monnier L. Basal insulin analogues in the management of diabetes mellitus: what progress have we made? Diabetes Metab Res Rev. 2014;30(2):104–19.
Hilgenfeld R, Seipke G, Berchtold H, et al. The evolution of insulin glargine and its continuing contribution to diabetes care. Drugs. 2014;74(8):911–27.
Triplitt C, Hinnen D, Valentine V. How similar are biosimilars? What do clinicians need to know about biosimilar and follow-on insulins? Clinical Diabetes. 2017;35(4):209–16.
Mylan S.A.S. Semglee 100 units/ml solution for injection in pre-filled pen: EU summary of product characteristics 2019. http://www.ema.europa.eu/. Accessed 9 Mar 2020.
Pharmaceuticals and Medical Devices Agency. Insulin glargine BS injection kit “FFP”: Japanese prescribing information. 2019. http://www.pmda.go.jp/. Accessed 11 Feb 2020.
European Medicines Agency. Semglee: EU assessment report. 2018. http://www.ema.europa.eu/. Accessed 9 Mar 2020.
Heise T, Donnelly C, Barve A, et al. Pharmacokinetic and pharmacodynamic bioequivalence of proposed biosimilar MYL-1501D with US and EU insulin glargine formulations in patients with type 1 diabetes mellitus. Diabetes Obes Metab. 2019:1-9.
Heise T, Tagore R, Donnelly C, et al. Comparative pharmacokinetics (PK) and pharmacodynamics (PD) of a proposed biosimilar insulin glargine and Lantus® in patients with type 1 diabetes (T1D) [abstract no. 1019-P]. Diabetes. 2017;66(Suppl 1):A268.
Blevins TC, Barve A, Sun B, et al. Efficacy and safety of MYL-1501D vs insulin glargine in patients with type 1 diabetes after 52 weeks: results of the INSTRIDE 1 phase III study. Diabetes Obes Metab. 2018;20(8):1944–50.
Blevins TC, Barve A, Sun B, et al. Efficacy and safety of MYL-1501D versus insulin glargine in patients with type 2 diabetes after 24 weeks: results of the phase III INSTRIDE 2 study. Diabetes Obes Metab. 2019;21(1):129–35.
Blevins TC, Barve A, Raiter Y, et al. Efficacy and safety of MYL-1501D versus insulin glargine in patients with type 1 diabetes mellitus: results of the INSTRIDE 3 phase 3 switch study. Diabetes Obes Metab. 2019:1–8.
Sun B, Sengupta N, Rao A, et al. Comparable immunogenicity between proposed biosimilar MYL-1501D and insulin glargine in the INSTRIDE 1 study [abstract no. P-0255]. In: Congress of the International Diabetes Federation. 2017.
European Medicines Agency. Semglee (insulin glargine): summary of opinion. 2018. http://www.ema.europa.eu/en/. Accessed 9 Mar 2020.
Kim AP, Bindler RJ. The future of biosimilar insulins. Diabetes Spectrum. 2016;29(3):161–6.
White J, Goldman J. Biosimilar and follow-on insulin: the ins, outs, and interchangeability. J Pharm Technol. 2019;35(1):25–35.
Lamb YN, Syed YY. LY2963016 insulin glargine: a review in type 1 and 2 diabetes. BioDrugs. 2018;32(1):91–8.
Acknowledgements
During the peer review process, the manufacturer of MYL1501D insulin glargine was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Sheridan Hoy is a salaried employee of Adis International Ltd/SpringerNature, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
Additional information for this Adis Drug Evaluation can be found at https://doi.org/10.6084/m9.figshare.11955207.
The manuscript was reviewed by:R. Dolinar, Arizona Endocrinology Center, Phoenix, AZ, USA; N. Papanas, Diabetes Centre, Second Department of Internal Medicine, Democritus University of Thrace, Alexandroupolis, Greece.
The original version of this article was revised due to a retrospective Open Access request.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hoy, S.M. MYL1501D Insulin Glargine: A Review in Diabetes Mellitus. BioDrugs 34, 245–251 (2020). https://doi.org/10.1007/s40259-020-00418-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-020-00418-x