Abstract
Background
The acceptability of switching between reference drugs and their biosimilars is often disputed. It is unclear whether this concern is specific to the use of biosimilars or is relevant to the practice of switching between any biological drugs.
Objective
The objective of this study was to quantify the occurrence of switching between different erythropoiesis-stimulating agents.
Methods
A retrospective drug utilization study was conducted in the Umbria region (Italy). The study population included all residents who received their first epoetin prescription between 1 July 2011 and 31 December 2014. The Umbria drug prescription database and the regional archive of residents were used to gather information. Switching was defined as any transition between different epoetins (different substances and/or different products of the same substance) in a series of two prescriptions. The probability of switching was described in relationship to the duration of treatment in a survival analysis.
Results
Overall, 3258 subjects received prescriptions of epoetins. Among the 2896 patients with at least two prescriptions, 354 (12.2 %) experienced one or more switches. The probability of switching depended on the duration of treatment: approximately 15 % of users switched within 12 months of observation and 25 % switched within 2 years. Switching was not limited to reference and biosimilar epoetins and it affected patent and off-patent epoetins equally.
Conclusions
Switching between different epoetins was related to the duration of use and most episodes of switching involved epoetins that have never been contrasted in a comparability exercise. The present level of switching may provide reassurance to physicians when taken together with other sources of comparative evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The probability of switching between different epoetins was associated with the duration of treatment: about 15 % of users switched within 12 months and almost 25 % within 2 years of observation. |
When switched from the reference epoetin, the majority of subjects (61.8 %) received another patented epoetin and 38.2 % received a biosimilar epoetin. Initial users of other patented epoetins were mainly shifted to a different product within the same category (67.1 %). |
The phenomenon of switching was not restricted to the replacement of reference epoetins with biosimilar epoetins, but also extended to products that have not been directly compared in clinical studies. |
1 Introduction
Marketing of biosimilars represents an opportunity for significant savings in pharmaceutical expenditure. However, despite the approval of biosimilars being preceded by tests that document their equivalence to the reference products, their use is the subject of ongoing debate in clinical practice, mainly concerning the acceptability of switching between a reference drug and its biosimilars (in patients already treated with a reference product).
In order to be commercialized, a biosimilar must be proven equivalent to the reference product in terms of quality, safety, and effectiveness. This comparability exercise, which is the basis of the marketing authorization, should be considered sufficiently reassuring. For erythropoietin-stimulating agents (hereafter referred to as epoetins), clinical trials include two study phases: the correction and the maintenance phases. To be included in the maintenance phase, patients should be optimally titrated with the reference epoetin (stable hemoglobin in the target range with a stable epoetin dose) for a suitable duration of time. Thereafter, study subjects are randomized to either the biosimilar or the reference epoetin [1]. Thus, pre-registration trials establish not only the therapeutic equivalence of the two products, but also that switching from reference to a biosimilar product is not associated with an increased risk of adverse events [2, 3].
Nevertheless, some documents, as well as numerous debates, on the use of biosimilars reiterate that biosimilars may represent a more efficient (less costly) option for the treatment of ‘naïve’ subjects [4], whereas it is preferable that therapeutic continuity be guaranteed for every treated patient [5] because the safety of the substitution between originators and their biosimilars is not considered to be supported by robust studies [6]. This position does not take into account that switching between different products of the same therapeutic category, not only between reference and biosimilar drugs, may be relatively common in clinical practice. If this were the case, it would provide an indirect justification for the option of switching between reference and biosimilar epoetins.
To date, few studies have investigated the frequency with which biological products of the same therapeutic category are substituted in clinical practice. The aim of the present study was to quantify the occurrence of switching between different epoetins.
2 Methods
2.1 Study Population
The study was conducted in the Umbria region (about 900,000 inhabitants) of Italy in the period between 1 July 2011 and 31 December 2014. All residents (without age restriction) who received a first prescription of an epoetin during the study period and without prescriptions in the previous 6 months (incident users) were included in the analysis.
2.2 Data Source
In Italy, epoetins are covered free of charge by the National Health Service on the basis of a prescription issued by the general practitioner upon presentation of a treatment plan filled in by a specialist. The medication can be dispensed through local health units or community pharmacies. To activate the reimbursement procedure, the dispensing pharmacies are required to create a dispensing record in the appropriate regional database. For each dispensing record, the patient identifier, number of dispensed packages, drug authorization code, and date of dispensation were retrieved. Information on substances and on the expected duration of the prescription on the basis of the defined daily doses contained in each package were identified. Patients’ demographic information was acquired through the archive of residents in the Umbria region. No information was available on the indication (e.g., chronic kidney disease or cancer) for the epoetin prescription or on drug use during hospitalization.
2.3 Study Drugs
The following epoetins were prescribed in the Umbria region during the study period: epoetin alfa (Eprex® and Binocrit®), epoetin beta (Neorecormon®), epoetin zeta (Retacrit®), darbepoetin alfa (Aranesp® and Nespo®), and methoxypolyethyleneglycol–epoetin beta (Mircera®). The analysis was performed by grouping the different substances as “reference epoetin” (Eprex®), “biosimilar epoetins” (Binocrit® and Retacrit®), and “other patented epoetins” (Aranesp®, Nespo®, Mircera®, and NeoRecormon®).
2.4 Definition of Switching
On the basis of the first prescription, subjects were classified as users of reference epoetin, of biosimilar epoetins, and of other patented epoetins. Patients were followed from the first prescription until the first of the following events: switching, last prescription, or end of the study period. Switching was defined as any transition between (substitution of) different products in a series of two prescriptions; switching might concern different substances (e.g., epoetin alfa vs. epoetin beta) as well as different products of the same substance (e.g., Binocrit® vs. Retacrit®; reference vs. biosimilar epoetins). Switches could occur at any time during the study period, up to a maximum observation time of 42 months.
2.5 Data Analysis
Descriptive analyses by age and sex of the study population were conducted. The probability distribution of switching was related to the months of treatment in a survival analysis (Kaplan–Meier). This analysis was performed including users with at least two prescriptions and distinguishing between users of reference epoetin, biosimilar epoetins, and other patented epoetins. Two sensitivity analyses were conducted: by year of the first prescription; and, in patients who had more than one epoetin dispensed, after the first switch during the study period (to describe the characteristics of the second switch). The age and sex of the study subjects were tested as possible determinants of switching and the association was assessed using a Chi-squared (χ 2) test. P values <0.05 were considered statistically significant. The statistical analysis was performed using STATA® software (version 11.2; StataCorp LP, College Station, TX, USA).
3 Results
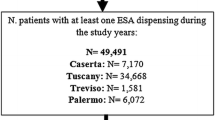
During the study period 3258 subjects received at least one epoetin prescription (3.6 per 1000 inhabitants). Users had a median age of 79 years, with similar sex distribution. Each user received an average of 14 prescriptions and only 11.1 % were sporadic users (one prescription in the study period) (Table 1). Most epoetin users were prescribed products categorized as other patented epoetins (n = 2545; 78.1 %) and a relatively small proportion of patients received either reference (n = 446; 13.7 %) or biosimilar epoetins (n = 267; 8.2 %). The three cohorts were quite similar in terms of demographic characteristics, although users of other patented epoetins had a median age (80 years) slightly higher than that of other users (73 and 77 years, respectively, for users of reference and biosimilar epoetins) (Table 1). The use of biosimilar epoetins was very low in 2011 (0.7 %) and 2012 (1.8 %) and increased to 9 and 18.3 % in 2013 and 2014, respectively (Fig. 1).
Distribution of epoetin prescribing in the Umbria region between 2011 and 2014. Reference epoetin: epoetin alfa (Eprex®); other patented epoetins: darbepoetin alfa (Aranesp®, Nespo®), methoxypolyethyleneglycol–epoetin beta (Mircera®), and epoetin beta (NeoRecormon®); biosimilar epoetins: epoetin alfa (Binocrit®) and epoetin zeta (Retacrit®). DDD defined daily dose
3.1 Analysis of Switching
Among the 2896 patients with at least two prescriptions of epoetins, 354 (12.2 %) experienced at least one switch in the study period. When switched from the reference epoetin (n = 68), the majority of subjects (n = 42; 61.8 %) received one of the other patented epoetins and 38.2 % (n = 26) received one biosimilar epoetin (Table 2). Users of other patented epoetins (n = 246) were mainly shifted to a different product within the same category (n = 165; 67.1 %).
The probability of switching was associated with the duration of treatment: approximately 15 % of users switched within 12 months and almost 25 % switched within 2 years of observation (Fig. 2). A similar picture was observed when the three cohorts (users of other epoetins, reference epoetin, and biosimilar epoetins) were analyzed separately. The probability of switching did not differ between men and women or by different age classes (Table 3). Moreover, no difference was observed when the analysis was stratified by year of first prescription (see the Electronic Supplementary Material).
Kaplan–Meier estimate for time to first switch among patients dispensed at least two epoetin prescriptions between 2011 and 2014 in the Umbria region of Italy. The inset graph shows the time to switch in the cohorts of users of other patented epoetins (O, red line), reference epoetin (R, green line), and biosimilar products (B, blue line). The corresponding 95 % confidence interval is represented by shaded regions
The analysis of the second switch involved 38.9 % (n = 130) of the 334 patients who received at least one prescription after their first switch. The same prescriptive pattern already observed after the first switch could be seen at the second switch (Table 4).
4 Discussion
We were able to trace all prescriptions of epoetins in a 4-year period for the entire population of the Umbria region. The analysis showed that the probability of switching increased with the duration of therapy, reaching 25 % in subjects who were treated for up to 24 months. Switching equally affected all users and was not restricted to reference and biosimilar epoetins, suggesting that the likelihood of switching is unrelated to the evidence provided by comparability exercises.
In a study conducted in Southern Italy, Loiacono et al. [7] found a higher prevalence of users (5.5 per 1000 inhabitants) than observed in Umbria (3.6 per 1000 inhabitants). Moreover, they also estimated a larger proportion of patients would switch between different products (21.8 %) in the 1.5 years of follow-up [7] versus 12.2 % over 2 years in the present study. The large variability in the prescribing pattern of epoetins reported in the Italian regions [8] might explain the differences observed in the estimates of switching. A recent population-based study analyzing the patterns of epoetin use in a large cohort of Italian outpatients found a high degree of heterogeneity of epoetin use across different Italian regions ranging from 1.5 per 1000 inhabitants in the Veneto region to more than 3.0 per 1000 inhabitants in the Sicily region in 2013 [9].
No other observational studies are currently available regarding the frequency of switching between epoetins in relation to the duration of therapy. What is well-documented, however, is that substituting different epoetins was not associated with the occurrence of adverse events. Data supporting the safety of switching mostly derive from crossover studies in which the therapeutic regimen of all patients admitted to a hospital or a hemodialysis unit was modified. Ebbers et al. [2] identified 35 crossover studies that evaluated the safety of switching between different epoetins (regardless of whether reference, biosimilar, or other patented epoetins) in a total of 11,249 patients. Although these studies were generally too short to exclude the occurrence of long-term adverse events, no safety problems were reported in association with switching [2]. An analysis by Więcek et al. [3] evaluated the impact of switching from epoetin alfa to epoetin zeta, or vice versa, in patients with chronic kidney disease. The study showed that treatment with epoetin alfa or epoetin zeta could be exchanged without any clinically relevant effects (in terms of efficacy, safety, or dosing) [3].
Among the obstacles to the use of biosimilars in clinical practice, there are two main uncertainties often referred to by physicians: (1) the safety of long-term use of these products; and (2) the safety of switching between reference and biosimilar products. The first concern will probably lessen with time, with the increasing number of patients being treated with biosimilars. In our opinion, the issue of switching might be more difficult to overcome because the evidence derived from the comparability exercise that precedes biosimilar marketing should already be sufficient to convince physicians.
The European Medicines Agency entrusted physicians with the responsibility of substitutions between reference and biosimilar products [10] and each European country adopted specific policies [11]. If the diffusion of biosimilars is to be encouraged, its use cannot be limited to naïve patients. It inevitably requires that both European and national medicines agencies, as well as scientific societies, are more proactive in presenting the transition from reference to biosimilar products as a safe option. The awareness that switching is frequently conducted between products that have not gone through a comparability exercise may represent a further argument that can be used in discussions with physicians.
The main limitations of our study concern the lack of information on the indication for the prescriptions (e.g., whether epoetins were prescribed in patients with renal or oncological conditions) and on the reasons for switching. As for other pharmacoepidemiological studies using prescription databases, it was not possible to ascertain whether the dispensed drug was actually taken by the patient; however, as these drugs are indicated for chronic diseases, it is unlikely that the results would be altered by this possible misclassification.
5 Conclusions
Our study shows that switching is related to the duration of drug therapy and equally affects all epoetins. The practice of switching mainly concerns drugs that have not undergone the direct comparability testing that is carried out before marketing a biosimilar product. These data, when taken together with other sources of comparative evidence, may provide reassurance to physicians regarding the substitution of reference with biosimilar epoetins.
References
European Medicines Agency. Guideline on non-clinical and clinical development of similar biological medicinal products containing recombinant erythropoietins. (EMEA/CHMP/BMWP/301636/2008). 2010. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/04/WC500089474.pdf. Accessed 5 Aug 2015.
Ebbers HC, Muenzberg M, Schellekens H. The safety of switching between therapeutic proteins. Expert Opin Biol Ther. 2012;12:1473–85.
Więcek A, Ahmed I, Scigalla P, Koytchev R. Switching epoetin alfa and epoetin zeta in patients with renal anemia on dialysis: posthoc analysis. Adv Ther. 2010;27:941–52.
AIFA position paper. I farmaci biosmilari. 2013. http://www.agenziafarmaco.gov.it/sites/default/files/AIFA_POSITION_PAPER_FARMACI_BIOSIMILARI.pdf. Accessed 5 Aug 2015.
Farmaci biosimilari: sicurezza, efficacia, omogeneità di trattamento e corretta informazione. Un Manifesto dei diritti dei pazienti. 2014. http://www.amrer.it/download_documenti/manifesto-farmaci-biosimilari.pdf. Accessed 17 Dec 2015.
Pani L, Montilla S, Pimpinella G. Bertini Malgarini R. Biosimilars: the paradox of sharing the same pharmacological action without full chemical identity. Expert Opin Biol Ther. 2013;13:1343–6.
Loiacono C, Sgroi C, Coppolino S, Cannata A, Ferrara R, Arcoraci V, et al. How much are biosimilars used in southern Italy? A retrospective analysis of epoetin utilization in the local health unit of Messina in the years 2010–2011. BioDrugs. 2012;26:113–20.
La Vecchia C, Franceschi S, Apolone G. Drug distribution and expenditure: the issue of epoetin in Italy. Eur J Public Health. 2003;13:367.
Ingrasciotta Y, Giorgianni F, Bolcato J, Chinellato A, Pirolo R, Tari DU, et al. How much are biosimilars used in clinical practice? A retrospective Italian population-based study of erythropoiesis-stimulating agents in the years 2009–2013. BioDrugs. 2015;29:275–84.
Covic A, Cannata-Andia J, Cancarini G, Coppo R, Frazão JM, Goldsmith D, et al. Biosimilars and biopharmaceuticals: what the nephrologists need to know—a position paper by the ERA-EDTA Council. Nephrol Dial Transplant. 2008;23:3731–7.
Niederwieser D, Schmitz S. Biosimilar agents in oncology/haematology: from approval to practice. Eur J Haematol. 2011;86:277–88.
Author contributions
GT conceived and designed the study; CD and RDC analyzed the data; CD and GT wrote the manuscript; GT, CD, RDC, and MR contributed to the discussion and reviewed the manuscript. GT acts as guarantor for the paper. All authors saw, commented upon, and approved the final version of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approvals
This study was carried out within the research protocol coordinated by the National Institute of Health and the Umbria region (“Analysis of drug prescriptions in the Umbria region”). Only anonymized individual codes that did not allow identification of the study subjects were available for the analysis.
Funding
Only public employees of the National or Regional health authorities were involved in conceiving, planning, and conducting the study; no ad hoc funding was received. The corresponding author had full access to all study data and approved the manuscript for publication.
Conflict of interest
CD, RDC, MR, and GT declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
D’Amore, C., Da Cas, R., Rossi, M. et al. Switching Between Epoetins: A Practice in Support of Biosimilar Use. BioDrugs 30, 27–32 (2016). https://doi.org/10.1007/s40259-015-0155-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-015-0155-0