Abstract
Background
Psychological distress (PD) is a major health problem that affects all aspects of health-related quality of life including physical, mental and social health, leading to a substantial human and economic burden. Studies have revealed a concerning rise in the prevalence of PD and various mental health conditions among Australians, particularly in female individuals. There is a scarcity of studies that estimate health state utilities (HSUs), which reflect the overall health-related quality of life in individuals with PD. No such studies have been conducted in Australia thus far.
Objective
We aimed to evaluate the age-specific, sex-specific and PD category-specific HSUs (disutilities) in Australian adults with PD to inform healthcare decision making in the management of PD.
Methods
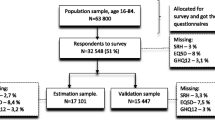
Data on age, sex, SF-36/SF6D responses, Kessler psychological distress (K10) scale scores and other characteristics of N = 15,139 participants (n = 8149 female individuals) aged >15 years were derived from the latest wave (21) of the nationally representative Household, Income and Labor Dynamics in Australia survey. Participants were grouped into the severity categories of no (K10 score: 10–19), mild (K10: 20–24), moderate (K10: 25–29) and severe PD (K10: 30–50). Both crude and adjusted HSUs were calculated from participants’ SF-36 profiles, considering potential confounders such as smoking, marital status, remoteness, education and income levels. The calculations were based on the SF-6D algorithm and aligned with Australian population norms. Additionally, the HSUs were stratified by age, sex and PD categories. Disutilities of PD, representing the mean difference between HSUs of people with PD and those without, were also calculated for each group.
Results
The average age of individuals was 46.130 years (46% male), and 31% experienced PD in the last 4 weeks. Overall, individuals with PD had significantly lower mean HSUs than those likely to be no PD, 0.637 (95% confidence interval [CI] 0.636, 0.640) vs 0.776 (95% CI 0.775, 0.777) i.e. disutility: −0.139 [95% CI −0.139, −0.138]). Mean disutilities of −0.108 (95% CI −0.110, −0.104), −0.140 (95% CI −0.142, −0.138), and −0.188 (95% CI −0.190, −0.187) were observed for mild PD, moderate PD and severe PD, respectively. Disutilities of PD also differed by age and sex groups. For instance, female individuals had up to 0.049 points lower mean HSUs than male individuals across the three classifications of PD. There was a clear decline in health-related quality of life with increasing age, demonstrated by lower mean HSUs in older population age groups, that ranged from 0.818 (95% CI 0.817, 0.818) for the 15–24 years age group with no PD to 0.496 (95% CI 0.491, 0.500) for the 65+ years age group with severe PD). Across all ages and genders, respondents were more likely to report issues in certain dimensions, notably vitality, and these responses did not uniformly align with ageing.
Conclusions
The burden of PD in Australia is substantial, with a significant impact on female individuals and older individuals. Implementing age-specific and sex-specific healthcare interventions to address PD among Australian adults may greatly alleviate this burden. The PD state-specific HSUs calculated in our study can serve as valuable inputs for future health economic evaluations of PD in Australia and similar populations.
Similar content being viewed by others
This study pioneers the creation of a comprehensive database of age-specific and sex-specific health state utility estimates within a large representative sample of Australians with psychological distress. |
The study underscores significant disparities in health state utilities, revealing lower values in individuals with psychological distress compared with those without the condition, female individuals compared with male individuals, and older age groups compared with younger age groups; emphasising the need for targeted interventions and policies to address the specific health needs of various population groups. |
Our health state utilities estimates may serve as essential inputs for economic evaluations and other work requiring measures of utility, facilitating the formulation of policies and practices aimed at improving the overall well-being of people with psychological distress in Australian and similar populations. |
1 Introduction
Psychological distress (PD), a type of mental disorder equally common among adults and seniors, is a major public health challenge that substantially contributes to the burden of disease worldwide [1, 2]. Psychological distress is predominantly defined as a condition of emotional disturbance marked by symptoms associated with mental disorders, which may encompass manifestations of depression, such as diminished interest, feelings of sadness and a sense of hopelessness, as well as symptoms of anxiety such as restlessness and tension. At times, it may be accompanied by somatic symptoms, including insomnia and headaches [3, 4].
Psychological distress has different severity levels with varying degrees of intensity, and it is characterised by typical physiological and mental symptoms. Psychological distress has been associated with various adverse outcomes, including diminished quality of life, unhealthy behaviours, heightened healthcare utilisation, diminished adherence to treatment and elevated mortality rates [5, 6]. The patient’s experience and satisfaction can be detrimentally influenced by PD, potentially contributing to an excessive utilisation of healthcare services [7]. It can cause substantial impairments in a patient’s ability to function and, in some cases, may lead to suicide. In 2019, mental disorders caused 16% of global disability-adjusted life-years and the estimated economic value associated with this burden was about USD 5 trillion [8]. It causes the second most years lived with disability, after lower back pain [9]. The prevalence of PD and subsequent human and financial costs are rising in Australia [10, 11]. Depression alone is predicted to cause a 34% increase in lost gross domestic product and a 45% increase in lost income tax revenue from 2015 to 2030 in Australia [12]. Women experiencing PD incur healthcare costs that are 15% higher compared with those without such distress [13]. The annual decrease in Australian employee productivity was estimated to be $5.9 billion [14] and the all-time loss from work due to PD was 50–60% [15]. The estimated annual value of time lost in the mining industry due to PD was $4.9 million [16].
A comparison of burden of diseases shows that depressive and anxiety disorders persist as significant contributors to the global burden of disease, holding the 13th and 24th positions, respectively, among the leading causes of disability-adjusted life-years. Their prevalence estimates and disability weights are notably higher compared with many other diseases [17]. In Australia, the leading contributors to health burden encompassed cancer, mental health issues along with substance use disorders, musculoskeletal conditions, cardiovascular diseases and neurological disorders. In 2023, mental health conditions and substance use disorders rose to the second position in the ranking contributing 15% to the total disease burden following cancer, which contributes 17% [18].
Psychological distress can affect functional impairment leading to deterioration in health-related quality of life (HRQoL) or a decline in subjective perceptions of social, occupational and health-related well-being [19, 20]. Age-specific and sex-specific health state utilities (HSUs) are commonly used to reflect HRQoL, and to calculate quality-adjusted life-years (QALYs)—a measure taking into account both the length and the quality of life [21]. Health state utilities measure the strength of preference for a particular health state, usually represented as a number between 0 and 1 (zero = dead; one = perfect health) while negative values representing states worse than dead [22]. Quality-adjusted life-years serve as the foundation for calculating the incremental cost-effectiveness ratio in a cost-utility analysis (CUA), aiming to assess the cost effectiveness of diverse healthcare interventions [23]. The practical implementation of this approach involves customising HSU inputs when comparing interventions across distinct patient demographics such as genders, ages and severities. For instance, in a hypothetical scenario, utilising age-specific, sex-specific and severity-specific HSU inputs both before and after an intervention enables a precise evaluation of QALYs and, consequently, the clinical effectiveness and/or cost effectiveness of healthcare interventions. The incremental cost-effectiveness ratio derived from these tailored QALY inputs better addresses the variations in QALYs between two scenarios.
To make decisions regarding allocation of scarce healthcare resources across competing disease groups and conditions, the estimates of HSUs play an important role as they provide information on the strength of people’s preferences for different health states [24]. Health state utilities are employed in a CUA, which is commonly used in health economic evaluations to inform health policy [25]. Pricing and reimbursement landscape determining patients’ access to new treatments, and manufacturers’ return on their investments in developing new products is closely associated with the outcomes of CUA [26].
Numerous direct (e.g. time trade-off and standard gamble) and indirect (e.g. Assessment of Quality of Life [AQoL]-8D, EQ-5D-5L, SF-6D) measures have been employed to estimate HRQoL. Health-related quality of life involves a wide array of experiences, states and perceptions [27] and is a multi-dimensional concept accounting for a patient’s physical, emotional and social functioning [28]. To generate HSUs for the calculation of QALYs, preference-based measures of HRQoL can be used [24, 29]. To calculate QALYs, the Short Form 6-Dimension (SF-6D) is used, which is a preference-based measure [30]. The SF-6D is derived from the Short Form 36 (SF-36) health survey, which is the most frequently used, valid and reliable generic measure of subjective well-being [31,32,33]. The SF-6D has six dimensions each comprising four to six levels including physical function, role limitation, social functioning, pain, mental health and vitality.
The growing evidence suggests that SF-6D can be considered valuable for use in the economic evaluation of interventions for a range of common mental health problems because of its responsiveness to change over time [34]. Indeed, in many cases it is proved to be more responsive than depression-specific measures owing to its potential simultaneous improvement in comorbid conditions and integrated nature of mental and physical health problems. The SF-6D can distinguish between groups based on depression severity and across differences in HRQoL of patients with depression. Additionally, the SF-6D is sensitive to clinical and quality-of-life improvement and deterioration [34].
A CUA stands as the primary method for economic evaluation in numerous countries, and a HSU serves as a pivotal data input in CUA models, significantly influencing the results [35]. Utility scores are typically derived from multi-attribute utility instruments (MAUIs) such as EQ-5D or SF-6D. Australia has established population norms for the AQoL instrument. Among others, utility values for common mental disorders with a high prevalence derived from the AQoL-4D and analysed by disorder classification can be used in a CUA in Australia. The average utility value is 0.67 and lower utility values need to be assigned to higher severity levels and some comorbidities [36]. Regarding SF-6D, the first Australian weights were produced in 2013 [37], which are generally consistent with the largely monotonic nature of the SF-6D.
Despite being crucial for economic evaluations, information about HSUs of PD is deficient even in developed countries such as Australia. Few studies have focused on finding the effect of psychological distress on HRQoL [38,39,40,41] in Australia. However, their findings do not provide any useful insights into sex-specific, age-specific and PD severity-specific aspects of the disease. Hence, there is a need to estimate updated sex-specific, age-specific and PD severity-specific HSU values to understand the human burden of PD and to be used in health economic evaluations of PD aimed at identifying cost-effective interventions to manage PD and to project the lifetime disease outcomes and the total lifetime costs.
We aim to use the most recent nationally representative data of the Household, Income, and Labor Dynamics in Australia (HILDA) survey to estimate and compare HSUs of Australian adults with PD and those without. Our HSUs estimates can be used across a broad range of health economic evaluations in Australia and similar populations. These estimates could be even more effective in the evaluations of new interventions where short-term trial data are available [42]. Factors such as age, sex and different levels of PD severity may affect HSUs; therefore, generating age-specific and sex-specific HSUs estimates could help understand the possible difference between HRQoL of male individuals and female individuals across different ages and psychological classifications. This, in turn, improves the accuracy of health economic evaluations. In this study, for the first time, we derive age-specific and sex-specific HSUs estimate elicited for PD health states for Australian adults.
We have estimated a whole battery of HSU estimates using local data. There is a lack of global agreement regarding the optimal methods for generating and applying HSUs in a CUA [19] therefore, to enhance the precision of the multi-state health economic evaluation models it is recommended to use age-sex and disease severity-specific utilities [43]. Therefore, we believe that our age-specific, sex-specific and disease-specific HSU estimates facilitates more accurate estimations of long-term disease outcomes, including measures such as QALY loss/gain and life expectancy.
2 Materials and Methods
2.1 Study Population
Data on age, sex, SF-36 responses, and other characteristics of 15,139 participants aged ≥ 15 years were derived from the latest wave (21) of the nationally representative the HILDA survey which has been carried out annually from 2001 through 2022 (waves 1–21). The 90% wave-on-wave response rates of the HILDA survey are comparable to other large longitudinal surveys in the USA and Europe [44]. Details of the HILDA sample design, survey response rates and attrition rates can be found elsewhere [44].
2.2 Measurement of HRQoL
Health state utilities offer a consolidated score reflecting HRQoL and play a crucial role in the computation of QALYs, a pivotal metric in cost utility analyses [45]. Ideally, HSUs are calculated using primary data collected through preference-based measures [42]. Health state utilities can be derived by using various multi-attribute utility instruments (e.g. EQ-5D, AQoL-8D and SF-6D). SF-36 is one of the most widely used generic measures of subjective health [46,47,48]. It is a self-reported multi-dimensional instrument used to measure general health status or quality of life. Its items or questions allow respondents to show their perceptions about their health. However, SF-36 has not been designed as an instrument to be used in economic evaluations whereas SF-6D has been widely used in a series of economic valuation studies especially in the UK [49]. The other commonly used multi-attribute utility instrument in mental health patients is EQ-5D. Significant differences in EQ-5D and SF-6D utilities exist between patients in mental disorders as they use different valuation methods to estimate their sets of utility scores [50]. However, in a range of settings, SF-6D has good psychometric characteristics [51]. For depression, the EQ-5D indicates a reduced level of utility at the most severe stage, while the SF-6D demonstrates equal or greater detriment at the milder end [52]. The predominance of physical health considerations in the EQ-5D limits its sensitivity to variations in certain mental health populations [53]. The EQ-5D exhibits insensitivity at the upper (healthy) end of the scale, while the SF-6D appears to lack a ceiling effect and can potentially capture more subtle health changes toward the upper range of the scale [54]. Furthermore, the SF-6D comprises a considerably larger size of its descriptive system that may contribute to a heightened sensitivity, thereby offering a potentially greater capacity to capture nuanced variations in health states [55].
Therefore, SF-36 profiles of the study participants were used to elicit HSUs for all those respondents who answered all 11 questions used in SF-6D. First, the study participants profiles were converted into a six-dimensional (i.e. physical functioning, role limitations, social functioning, pain, mental health and vitality) preference-based MAUI (the SF-6D Version 1 [v1]) applying the algorithm developed by Norman et al. [37] based on preference weight specific to the Australian population. These weights range from 0.29 to 1.00, with 1.00 indicating “full health”. The general form of the model is as follows.
where i = 1, 2, …, n represents state values of individual and j = 1, 2, …, and m represents respondents. \({Y}_{ij}\) is the dependent variable showing Standard Gamble scores for health state i valued by respondent j. X is a vector of explanatory variables (\({X}_{\mathrm{\delta \gamma }})\) for each level \(\upgamma\) of dimension \(\updelta\) of the SF-6DFootnote 1. For any given health state, \({X}_{\delta \gamma }\) is defined as
\({{\text{X}}}_{\mathrm{\delta \gamma }}=1\), if, for this state, dimension δ is at level \(\upgamma\)
\({{\text{X}}}_{\mathrm{\delta \gamma }}=0,\) if, for this state, dimension δ is not at level \(\upgamma\)
The error term comprises factors that account for interactions between the levels of different attributes. Z is a vector of personal characteristics that may also affect the value an individual assigns to a health state such as age and sex. The additive nature of the model does not necessitate an interval scale between the levels of each dimension. Ordinary least square, the most common mapping method, was used to estimate the model [56].
2.3 Kesseler Psychological Distress Scale (K10)
This study uses the Kessler Psychological Distress scale (K10) as the measure of psychological distress as the main outcome. The K10 is a widely used measure to detect PD. However, there are no international standards regarding cut-off scores of K10 to detect PD. Two factors are likely to contribute to this wide range of reported cut-off scores. First, while some studies use K10 to broadly identify mental disorders, the others seek narrow definition of major depressive disorders [57] or serious mental illness [58]. Second, culture and clinical population support the possibility of differential patterns of symptoms across different samples. In this study, the suggested cut-off scores for the K10 were 10–19 for “no PD”, 20–24 “mild PD”, 25–29 “moderate PD” and 30–50 “severe PD”. This classification is in agreement with the one suggested by 2001 Victorian Population Health Survey to estimate the prevalence of levels of PD. Likewise, Donker et al. [59] recommended 20 or higher as the best for screening for depressive disorders in a primary care setting. Vasiliadis et al. [60] and Searle et al. [61] also used ≥19 as a cut-off score to detect depression in Canadian older adults and Australian military service members, respectively.
The K10 is a self-reported measure that briefly assesses the frequency of non-specific PD during the last 30 days [62]. It is equally suitable for both general and clinical populations [63]. In an Australian context, its mental disorder detection efficiency has been tested and compared to other instruments including the General Health Questionnaire (GHQ-12). The K10 was found to be significantly better than the GHQ-12 in identifying mood and anxiety disorders [64].
The K10 comprises questions on anxiety and depression symptoms. The sum of the scores, based on a 5-point Likert-type scale, ranges from 10 to 50 with higher scores representing higher distress levels [65]. The psychometric properties of the K10 are well established in the civilian population [66] and because of its sensitivity and specificity, it is included in population surveys of many countries [67], and within the scientific community, the factor structure of this scale is regarded as the least consensual psychometric characteristic (for a detailed discussion on K10 please refer to the Electronic Supplementary Material [ESM]).
2.4 Statistical Analysis
Summary statistics were produced initially to provide an overview of the study population in terms of their sociodemographic and clinical characteristics. We compared the characteristics of respondents with PD with those without PD using a t-test (for continuous variables) and an χ2 test (for categorical variables). The difference in HRQoL between individuals with PD and those with no PD was evaluated by comparing the crude mean HSUs, and those estimates adjusted for confounders of age, sex, smoking, marital status, area of residence, education level and income using a multi-variable linear regression model. The age-specific and sex-specific difference in HRQoL by disease severity were then evaluated by comparing the disease severity crude and adjusted mean HSUs. Statistical significance was set as a p-value ≤0.05 (two-tailed) to account for multiple testing burden. The normal quantile plot of residuals and the plot of fitted versus residuals were assessed to ensure error distribution was sufficiently normal. All analyses were performed using STATA for Windows (version 17.0).
3 Results
Table 1 describes the sociodemographic and clinical characteristics of the 15,139 respondents included in this study’s sample (for sex-specific and age-specific characteristics of respondents please refer to Tables 1a and 1b of the ESM, respectively). The majority were female (54%). The average respondent’s age was recorded as 46.830 years. The number of respondents with PD (n = 4746) was less than half the number of respondents without PD (n = 10,393). When we compared respondents having PD with respondents having no PD, we found a difference in sex with female individuals having PD proportion increased significantly (from 51% with no PD to 60% with PD) [p < 0.01]. The proportion of smokers (22%: PD and 12%: no PD) significantly differed between the two groups (p < 0.01). Similarly, the proportion of respondents with an active membership of a sporting/hobby/community-based club or association in PD cohort was significantly lower (n = 1174, 25% [p < 0.01]) than no PD (n = 3680, 35%) (Table 1). We found that no PD cohort was older (+9.96 years), and the age distribution differed significantly between PD and no PD cohorts (p < 0.01). Our comparison showed that the remoteness distribution of respondents between the two groups was statistically different (p < 0.01). There were significant differences in the distribution of marital status (p < 0.01), level of education (p < 0.01) and income (p < 0.01).
Table 2 displays the percentage of participants indicating an absence of issues across the six SF-6D dimensions. Individuals of various ages seem to be inclined to report difficulties in specific dimensions, with vitality being particularly prominent. However, no uniformity is observed across domains regarding age. Physical functioning appears to have more negative ingredient in older age when compared with other domains. Across all SF-6 dimensions, female individuals reported female individuals were more likely to report problem than male individuals.
Table 3 provides the comparison of the SF-6D mean HSUs between participants with and without PD by sex and by severity of PD. Overall, individuals with PD had significantly lower mean HSUs than those without PD (0.637 vs 0.776, i.e. disutility: −0.139). Mean disutilities of −0.108, −0.140 and −0.188 were observed for PD classifications mild, moderate and severe, respectively. Disutilities of PD also differed by sex. For instance, female individuals had up to 0.050 units lower mean HSUs than male individuals across the four classifications of PD.
There was a clear decline in HRQoL with increasing age, demonstrated by lower mean HSUs in older population age groups, with a range from 0.818 (for the 15–24 years age group with no PD) to 0.496 (for the 65+ years age group with severe PD) (Table 4). Before adjusting for confounders, mean values for HSUs were significantly lower for PD respondents.
After adjusting for confounders (for detail on confounder please refer to the ESM), the magnitudes of the difference in HRQoL scores between the two group was changed somewhat for HSUs but remained statistically significant (Tables 3, 4). For the individual sex-specific health dimensions, the largest statistically significant difference in the adjusted mean scores between two groups was seen in the “severe” category (−0.194 for male individuals and −0.199 for female individuals). In the age-specific health dimensions, the largest statistically significant difference (−0.236) was observed in the “severe” category of respondents in the age group of 45–64 years while the difference was smallest (−0.082) in the “mild” category of respondents in the age group of 15–24 years.
4 Discussion
Our study is the first to generate a database of age-specific and sex-specific HSU estimates in a large representative sample of Australians with PD, using a detailed preferentially sensitive SF-6D MAUI. Our descriptive results suggested that around one third of respondents reported a mild-to-severe type of PD and we found that HSUs were significantly lower in individuals with PD compared with those without, female individuals compared with male individuals, and older age groups compared with younger age groups. Health state utilities further decreased with elevated PD level (mild, moderate, severe) even when considering age and sex. This means that PD levels matter with respect to HSUs. Additionally, age-specific and sex-specific policies are warranted to address the impact of PD on HRQoL. These HSUs estimates can be used in economic evaluations and other work requiring measures of utility for the Australian context or similar populations to frame policies to address PD in this setting.
The proportion of individuals with PD (one in three) in our sample is not surprising, given the fact that over two in five (44%) Australians aged 16–85 years’ experience a mental disorder (MD) during their lifetime [68]. The difference between the National Study of Mental Health and Wellbeing and our sample is due to the variability of methods to measure prevalence of MD. The definition of PD adopted in this study is based on a K10 score, which derives estimates from self-reported patient outcome measures, whereas the National Study of Mental Health and Wellbeing employs existing diagnostic criteria. In another study, around 37.5% individuals were classified as having depression [69]. A recent systematic review and meta-analysis showed the prevalence of mental disorders at 22.1% of the study population [2]. A European study showed that 50%, 33% and 25% individuals had experienced a mental disorder in their lifetime, within the past year and currently, respectively [70]. In other populations, the prevalence of MD varies substantially, and our estimates are higher than those. For example, Arias et al. [71] found that the prevalence of depressive disorders in Europe ranges from 3% in Czech Republic to 10% in Iceland. The notable difference of MD prevalence estimates is due to the variables collected and assessed population. The possibility that diagnostic codes used in some studies could not pick up the full extent of the prevalence of MD cannot be ruled out [72, 73]. Furthermore, the inclusion of individuals who have subclinical depression or who do not fit in the diagnostic criteria of major depression might have led to the estimation of a higher prevalence rate in this study. The differences in the operational measure of MD between our study and these previous reports could be important to understand the variations found.
Individuals with more severe symptoms of PD have lower utility values when measured by SF-6D and EQ-5D. Measurement of PD severity levels can be measured in different ways that must be considered while interpreting the association between HSUs and PD. For example, while the Australian Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) version of the World Mental Health Composite International Diagnostic Interview WMH-CIDI and Clinical Interview Schedule Revised (CIS-R) were used to measure MD severity [74], another study used the Symptom Checklist (SCL-90) [50]. It is also noteworthy that despite consistent findings across studies regarding PD levels, the HSUs can differ among severity subgroups based on which MAUI is used [50, 74].
The finding that PD is associated with decreased level of HRQoL is aligned with previous literature conducted on the general adult population [75,76,77,78]. The presence of a health condition was associated with low HRQoL in Australia [79]. Among community-based adults in China, depression and HRQoL were inversely associated [80]. On all dimensions, HRQoL was found to be significantly lower in patients with chronic diseases compared with the general population in Korea [81]. Depression was found to affect HRQoL negatively in individuals with HIV [82], breast cancer [83] and diabetes mellitus [84].
Our findings that sex differences exist in HRQoL is also supported by previous studies. For example, a meta-analysis concluded that female individuals are almost twice as likely to experience depression than male individuals [85]. A cross-sectional study conducted in Sweden showed that HSU was lower among female individuals [86]. In Australia, male individuals reported a slightly higher HRQoL than female individuals [37]. Consistent results with this finding were reported in a US population-based study [87]. In Taiwan, women were found to have significantly lower mental component scores than men [88]. Different biological and psychological aspects between different sexes may also explain this difference in PD-related HRQoL. Furthermore, environmental factors can also influence this relationship, but even then, we should pay more attention to female individuals because they are more likely to be accompanied by a low level of HRQoL [75]. However, contrary to our finding, one study reported slightly higher HSUs for female individuals than male individuals across all ages and instruments [89].
The current study shows that HSUs decrease with an increase in age, which is aligned with existing literature. Using SF-6D outcomes in Australian adults, previous studies reported a consistent decline in HSUs with an advancing age [37]. A comparison of HSUs showed that with increasing age HSUs tend to decline [69, 86, 90,91,92]. This result is understandable as life experience and perceived responsibilities of young and old individuals differ considerably [93]. Depressed elderly individuals have a higher risk of morbidity and mortality, and an inclination to commit suicide and their mental disturbance and functional disability can decrease HRQoL [94]. Additionally, older individuals are likely to be isolated, which has major negative psychological effects. They may have more trouble while dealing with isolation than younger people [95,96,97]. Another explanation that supports this finding is the expression of more anxiety and concerns by older people about their family [98]. In contrast, a recent study found that age and gender had no impact on HRQoL [80]. Therefore, further studies are required to test the generalisability of this finding in other patient populations.
Our finding that SF-6D utilities were lower in participant (aged 45–64 years) than those aged 65+ years (Fig. 1b) contrasts with the majority of the studies on the subject but there are studies that report findings that are not different from our finding. For example, for an Australian population, similar findings are reported by Ngo et al. [79]. Lower EuroQol visual analog scale scores were found among Australian aged 45–54 years than adjacent age groups [99]. Lower utility values among US participants aged 55–64 years, relative to those aged 65–74 years were reported [100]. There is no clear reason for this observation; however, varying psychological well-being trends in high-income English-speaking countries can explain this finding. In these nations, emotional health and life satisfaction are lower in middle age than old age [101]. In Japan, levels of PD were found to be higher in middle-aged participants (47.4% of individuals aged 20–39 years) than older participants (40.6% and 28.3% of individuals aged 40–64 years and individuals aged 65–85 years, respectively) [102].
a Adjusted disutilities of psychological distress (PD), stratified by sex and disability severity. b Adjusted disutilities of PD, stratified by age group and disability severity. Mild PD (K10 score: 20–24), moderate PD (K10 score: 25–29), severe PD (K10 score: 30–50). K10 Kessler Psychological Distress Scale
We found that adjusted mean utility estimates of individuals with different categories of PD ranged from 0.496 to 0.656 (for female individuals) and from 0.591 to 0.645 (for male individuals). Likewise, these estimates range from 0.496 to 0.677 for older to younger age groups, respectively. This finding is in line with the previous studies. For example, a most recent survey on HSUs of depression reported that the pooled mean utilities of different depression-related health states ranged from 0.240 to 0.890 while mean utility values for mild, moderate and severe depression were 0.750, 0.660 and 0.500, respectively [103]. Another study also found that a less severe health state of depression was associated with high utility scores [104].
Our utility estimates for severe PD (0.592) were lower than utilities reported in the chronic medical disease literature (e.g. severe angina 0.870 [105] and chronic renal disease 0.630 [38]). In another review, the range of HSUs was reported from 0.615 for patients with very severe MD to 0.806 for patients with mild MD [106]. In contrast, estimated utilities for multiple sclerosis relapse onset 0.390 [107] was lower than our utility estimates. A study by Kolovos et al. [104] reported adjusted mean utilities of different classifications of depression that are lower than our adjusted estimates of utilities (0.590 vs 0.679 mild; 0.560 vs 0.636 moderate; 0.550 vs 0.588 severe). The difference in the estimated utilities is possible as different samples and utility assessment instruments were used across studies that necessitates caution while interpreting these findings. Our finding that mean utility estimates vary (0.091 points) by level of PD (mild to severe) is also supported by previous literature. For example, a 0.06-point difference was reported in the utilities of patients with severe depression and in patients with less severe depression [38].
Our identification of a notable negative trend in the vitality domain of SF-6D among older participants and female individuals aligns with previous research findings. Specifically, respondents from various age groups and genders consistently reported encountering more issues in the vitality domain. Moreover, our observations parallel previous research, where a significant decline in the physical functioning domain was noted with an increase in participant age. Likewise, the lack of uniformity in the occurrence of burden across all six domains has been a consistent theme in earlier studies [37]. This lack of uniformity underscores the complex and varied nature of HR-QoL experiences, emphasising the need for a nuanced understanding of the distinct challenges individuals may face across different dimensions.
Our estimates of HSUs can be compared with previous literature to a limited extent as, to our knowledge, no previous study has provided age-specific and sex-specific utility estimates for the same breakdown of PD severity levels. It is noteworthy that a comparison of utility values is generally limited as utility values can be generated using different methods [108, 109]. Findings reached in the current study contribute to the existing literature in PD, illustrating that HSUs and PD are negatively linked, but builds upon previous research by having demonstrated that the HSUs differ across age and sex.
There is a significant gap between the high incidence of PD and the insufficient resources allocated to address this issue in Australia highlighting the need for cost-effective interventions to enhance PD management. Adoption of target interventions instead of universal intervention may be more effective because of their cost effectiveness [110]. Boosting government expenditure has the potential to generate a set of interventions that are more cost effective and can save a greater number of disability-adjusted life-years [111]. Allocation of resources towards two main components of PD, depression and anxiety, could result in significant gains in health outcomes bringing greater efficiency in mental health services [112].
The key strength and novelty of the current paper is that it is the first study to generate age-specific and sex-specific HSUs to estimate hidden toll of PD in Australians adults. This suggests that future PD management policy and practice should be tailored to the age, sex and PD severity profiles of people with PD, and future health economic evaluations of PD should incorporate age-specific, sex-specific and severity-specific HSU inputs to improve the current modelling practice. Another major strength of this study is the use of a large, most recent and nationally representative dataset with a sufficient number of respondents with PD and cases for analysis by PD classification.
The lack of consensus regarding the definition of PD is a challenge of the current study that limits comparison to past papers. The PD levels were classified following the K10 scores, which is a proven and a stable assessment of PD and is commonly used for measuring PD, not the clinical diagnosis. Furthermore, the results in self-reported questionnaires on which the K10 method is based may be biased especially when the respondents are aged with cognitive impairment. Therefore, despite the novelty of our study, future studies of PD by severity type in other parts of the world are needed to validate our baseline findings.
5 Conclusions
Using a multi-attribute utility instrument (SF-6D), our study provides significant data on age-specific and sex-specific HSUs and investigates the association between HSUs and different types of disease severity that can be used for a range of health economic evaluations across the populations. Additionally, we have suggested that HSUs of individuals with PD differ significantly by severity level. The set of age-specific and sex-specific HSUs generated in this study can be used to calculate QALYs to be employed in health economic evaluations to guide policy and decision making for PD in Australia and similar populations. These findings are equally important in evaluating the cost effectiveness of preventive and management actions for PD. Because the focus of this study was to assess HSUs cross-sectionally, a longitudinal assessment has not been performed; however, HRQoL of people with PD and factors affecting HRQoL may change over time, so this should be an agenda item for future research based on longitudinal data.
Notes
For instance, \({X}_{31}\) denotes dimension \(\delta =3\) (social functioning), level \(\gamma =1\) (health limits social activities none of the time).
References
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394(10194):240–8.
LAbate L. Mental illnesses: understanding, prediction and control. BoD–Books on Demand; 2012.
Matthews G. Distress. In: Stress: concepts, cognition, emotion, and behavior. Amsterdam: Elsevier; 2016. p. 219–26.
Giesinger JM, Kuster MS, Behrend H, Giesinger K. Association of psychological status and patient-reported physical outcome measures in joint arthroplasty: a lack of divergent validity. Health Qual Life Outcomes. 2013;11(1):1–6.
Hamer M, Stamatakis E, Saxton JM. The impact of physical activity on all-cause mortality in men and women after a cancer diagnosis. Cancer Causes Control. 2009;20:225–31.
Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manage. 2014;3(2):77.
Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54:101675.
Pesudovs K, Melaku YA, Collaborators GBoDS. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013 diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800.
Harvey SB, Deady M, Wang MJ, Mykletun A, Butterworth P, Christensen H, et al. Is the prevalence of mental illness increasing in Australia? Evidence from national health surveys and administrative data, 2001–2014. Med J Aust. 2017;206(11):490–3.
Moon L, Garcia J, Laws P, Dunford M, On ML, Bishop K, et al. Measuring health loss in Australia: the Australian burden of disease study. J Korean Med Sci. 2019. https://doi.org/10.3346/jkms.2019.34.e61.
Schofield D, Cunich M, Shrestha R, Tanton R, Veerman L, Kelly S, et al. Indirect costs of depression and other mental and behavioural disorders for Australia from 2015 to 2030. BJPsych Open. 2019;5(3): e40.
Jayawardana D, Gannon B, Doust J, Mishra GD. Excess healthcare costs of psychological distress in young women: evidence from linked national Medicare claims data. Health Econ. 2023;32(3):715–34.
Hilton MF, Scuffham PA, Vecchio N, Whiteford HA. Using the interaction of mental health symptoms and treatment status to estimate lost employee productivity. Aust N Z J Psychiatry. 2010;44(2):151–61.
Milczarek M, Schneider E, González E. European Risk Observatory Report: OSH in figure: stress at work-facts and figures. European Agency for Safety and Health at Work, Luxembourg, Office for Official Publications of the European Communities; 2009:20-1.
Ling R, Kelly B, Considine R, Tynan R, Searles A, Doran CM. The economic impact of psychological distress in the Australian coal mining industry. J Occup Environ Med. 2016;58(5):e171–6.
Collaborators GMD. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
AIHW. Australian Burden of Disease Study 2023: Australian Institute of Health and Welfare 2023. Available from https://www.aihw.gov.au/reports/burden-of-disease/australian-burden-of-disease-study-2023/contents/key-findings. Accessed 21 March 2023.
Rowen D, AzzabiZouraq I, Chevrou-Severac H, van Hout B. International regulations and recommendations for utility data for health technology assessment. Pharmacoeconomics. 2017;35(Suppl. 1):11–9.
Cuijpers P. The challenges of improving treatments for depression. JAMA. 2018;320(24):2529–30.
Kind P, Lafata JE, Matuszewski K, Raisch D. The use of QALYs in clinical and patient decision-making: issues and prospects. Value Health. 2009;12:S27-30.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Edney LC, Haji Ali Afzali H, Cheng TC, Karnon J. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36:239–52.
Brazier J, Ratcliffe J, Saloman J, Tsuchiya A. Measuring and valuing health benefits for economic evaluation. Oxford: Oxford University Press; 2017.
Jakubiak-Lasocka J, Jakubczyk M. Cost-effectiveness versus cost-utility analyses: what are the motives behind using each and how do their results differ? A Polish example. Value Health Reg Issues. 2014;4:66–74.
Wolowacz SE, Briggs A, Belozeroff V, Clarke P, Doward L, Goeree R, et al. Estimating health-state utility for economic models in clinical studies: an ISPOR good research practices task force report. Value Health. 2016;19(6):704–19.
Calman KC. Definitions and dimensions of quality of life. The quality of life of cancer patients. Pharmacoeconomics. 1987;36(2):239–52.
Fayers PM, Machin D. Quality of life: the assessment, analysis and reporting of patient-reported outcomes. New Jersey: John Wiley & Sons; 2015.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 2016.
Wang L, Poder TG. A systematic review of SF-6D health state valuation studies. J Med Econ. 2023;26(1):584–93.
Brazier J. The short-form 36 (SF-36) health survey and its use in pharmacoeconomic evaluation. Pharmacoeconomics. 1995;7:403–15.
Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 health survey (with a supplement documenting version 1). Lincoln, RI: Quality Metric Incorporated; 2005.
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725.
Mulhern B, Mukuria C, Barkham M, Knapp M, Byford S, Brazier J. Using generic preference-based measures in mental health: psychometric validity of the EQ-5D and SF-6D. Br J Psychiatry. 2014;205(3):236–43.
Yang Z, Zeng X, Huang W, Chai Q, Zhao A, Chuang L-H, et al. Characteristics of health-state utilities used in cost-effectiveness analyses: a systematic review of published studies in Asia. Health Qual Life Outcomes. 2023;21(1):1–11.
Mihalopoulos C, Engel L, Le LK-D, Magnus A, Harris M, Chatterton ML. Health state utility values of high prevalence mental disorders in Australia: results from the National Survey of Mental Health and Wellbeing. Qual Life Res. 2018;27:1815–25.
Norman R, Church J, Van Den Berg B, Goodall S. Australian health-related quality of life population norms derived from the SF-6D. Aust N Z J Public Health. 2013;37(1):17–23.
Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord. 1998;48(1):25–36.
Griffiths S, Hay P, Mitchison D, Mond JM, McLean SA, Rodgers B, et al. Sex differences in the relationships between body dissatisfaction, quality of life and psychological distress. Aust N Z J Public Health. 2016;40(6):518–22.
Joshy G, Thandrayen J, Koczwara B, Butow P, Laidsaar-Powell R, Rankin N, et al. Disability, psychological distress and quality of life in relation to cancer diagnosis and cancer type: population-based Australian study of 22,505 cancer survivors and 244,000 people without cancer. BMC Med. 2020;18:1–15.
Aitken L-A, Hossan SZ. The psychological distress and quality of life of breast cancer survivors in Sydney, Australia. Healthcare. 2022;10:2017.
Lartey ST, Si L, de Graaff B, Magnussen CG, Ahmad H, Campbell J, et al. Evaluation of the association between health state utilities and obesity in sub-Saharan Africa: evidence from World Health organization study on global ageing and adult health wave 2. Value Health. 2019;22(9):1042–9.
Brazier J, Ara R, Azzabi I, Busschbach J, Chevrou-Séverac H, Crawford B, et al. Identification, review, and use of health state utilities in cost-effectiveness models: an ISPOR good practices for outcomes research task force report. Value Health. 2019;22(3):267–75.
Summerfield M, Dunn R, Freidin S, Hahn M, Ittak P, Kecmanovic M, et al. HILDA user manual–release 10. Melbourne, VIC: Melbourne Institute of Applied Economic and Social Research, University of Melbourne; 2011.
Zhou T, Chen Z, Li H, Xie F. Using published health utilities in cost-utility analyses: discrepancies and issues in cardiovascular disease. Med Decis Making. 2021;41(6):685–92.
Zhang Y, Bo Q, Lun S-S, Guo Y, Liu J. The 36-item short form health survey: reliability and validity in Chinese medical students. Int J Med Sci. 2012;9(7):521.
Weinberger M, Samsa GP, Hanlon JT, Schmader K, Doyle ME, Cowper PA, et al. An evaluation of a brief health status measure in elderly veterans. J Am Geriatr Soc. 1991;39(7):691–4.
Kim S-H, Kim S-O, Lee S-I, Jo M-W. Deriving a mapping algorithm for converting SF-36 scores to EQ-5D utility score in a Korean population. Health Qual Life Outcomes. 2014;12:1–10.
Kharroubi SA, Brazier JE, Roberts J, O’Hagan A. Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ. 2007;26(3):597–612.
Lamers L, Bouwmans C, van Straten A, Donker M, Hakkaart L. Comparison of EQ-5D and SF-6D utilities in mental health patients. Health Econ. 2006;15(11):1229–36.
Zhao FL, Yue M, Yang H, Wang T, Wu JH, Li SC. Validation and comparison of EuroQol and short form 6D in chronic prostatitis patients. Value Health. 2010;13(5):649–56.
Brazier J, Connell J, Papaioannou D, Mukuria C, Mulhern B, Peasgood T, et al. A systematic review, psychometric analysis and qualitative assessment of generic preference-based measures of health in mental health populations and the estimation of mapping functions from widely used specific measures. Health Technol Assess. 2014;18(34):vii.
de Willige GV, Wiersma D, Nienhuis FJ, Jenner JA. Changes in quality of life in chronic psychiatric patients: a comparison between EuroQol (EQ-5D) and WHOQoL. Qual Life Res. 2005;14:441–51.
Bryan S, Longworth L. Measuring health-related utility: why the disparity between EQ-5D and SF-6D? Eur J Health Econ. 2005;6:253–60.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–92.
Brazier JE, Yang Y, Tsuchiya A, Rowen DL. A review of studies mapping (or cross walking) non-preference based measures of health to generic preference-based measures. Eur J Health Econ. 2010;11:215–25.
Jong Won M, Sun HL. Validation of the K6/K10 scales of psychological distress and their optimal cutoff scores for older Koreans. Intl J Aging Hum Dev. 2015;80(3):264–82.
Oakley Browne MA, Wells JE, Scott KM, McGee MA, Team NZMHSR. The Kessler psychological distress scale in Te Rau Hinengaro: the New Zealand mental health survey. Aust N Z J Psychiatry. 2010;44(4):314–22.
Donker T, Comijs H, Cuijpers P, Terluin B, Nolen W, Zitman F, et al. The validity of the Dutch K10 and extended K10 screening scales for depressive and anxiety disorders. Psychiatry Res. 2010;176(1):45–50.
Vasiliadis H-M, Chudzinski V, Gontijo-Guerra S, Préville M. Screening instruments for a population of older adults: the 10-item Kessler Psychological Distress Scale (K10) and the 7-item Generalized Anxiety Disorder Scale (GAD-7). Psychiatry Res. 2015;228(1):89–94.
Searle AK, Van Hooff M, McFarlane AC, Davies CE, Fairweather-Schmidt AK, Hodson SE, et al. The validity of military screening for mental health problems: diagnostic accuracy of the PCL, K10 and AUDIT scales in an entire military population. Int J Methods Psychiatric Res. 2015;24(1):32–45.
Pereira A, Oliveira CA, Bártolo A, Monteiro S, Vagos P, Jardim J. Reliability and factor structure of the 10-item Kessler Psychological Distress Scale (K10) among Portuguese adults. Ciencia Saude Coletiva. 2019;24:729–36.
Peixoto EM, Zanini DS, de Andrade JM. Cross-cultural adaptation and psychometric properties of the Kessler Distress Scale (K10): an application of the rating scale model. Psicol Reflexão Crít. 2021;34:21.
Anderson TM, Sunderland M, Andrews G, Titov N, Dear BF, Sachdev PS. The 10-item Kessler psychological distress scale (K10) as a screening instrument in older individuals. Am J Geriatr Psychiatry. 2013;21(7):596–606.
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9.
Bougie E, Arim RG, Kohen DE, Findlay LC. Validation of the 10-item Kessler psychological distress scale (K10) in the 2012 Aboriginal Peoples Survey. Health Rep. 2016;27(1):3.
Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357–62.
Australian Institute of Health and Welfare (AIHW). Mental health. 2023. Available from https://www.aihw.gov.au/mental-health. Accessed 21 Mar 2023.
Levkovich I, Shinan-Altman S, Essar Schvartz N, Alperin M. Depression and health-related quality of life among elderly patients during the COVID-19 pandemic in Israel: a cross-sectional study. J Prim Care Commun Health. 2021;12:2150132721995448.
Andreas S, Schulz H, Volkert J, Dehoust M, Sehner S, Suling A, et al. Prevalence of mental disorders in elderly people: the European MentDis_ICF65+ study. Br J Psychiatry. 2017;210(2):125–31.
Arias-de la Torre J, Vilagut G, Ronaldson A, Serrano-Blanco A, Martín V, Peters M, et al. Prevalence and variability of current depressive disorder in 27 European countries: a population-based study. Lancet Public Health. 2021;6(10):e729–38.
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):2861.
Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, De Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1):1–16.
Roberts J, Lenton P, Keetharuth AD, Brazier J. Quality of life impact of mental health conditions in England: results from the adult psychiatric morbidity surveys. Health Qual Life Outcomes. 2014;12(1):1–10.
Han K, Yang S, Jia W, Wang S, Song Y, Cao W, et al. Health-related quality of life and its correlation with depression among Chinese centenarians. Front Public Health. 2020;8: 580757.
Sivertsen H, Bjørkløf GH, Engedal K, Selbæk G, Helvik A-S. Depression and quality of life in older persons: a review. Dementia Geriatr Cogn Disord. 2015;40(5–6):311–39.
Van der Weele GM, Gussekloo J, De Waal MW, De Craen AJ, Van der Mast RC. Co-occurrence of depression and anxiety in elderly subjects aged 90 years and its relationship with functional status, quality of life and mortality. Int J Geriatr Psychiatry. 2009;24(6):595–601.
Hajek A, Brettschneider C, Ernst A, Lange C, Wiese B, Prokein J, et al. Complex coevolution of depression and health-related quality of life in old age. Qual Life Res. 2015;24:2713–22.
Ngo PJ, Wade S, Banks E, Karikios DJ, Canfell K, Weber MF. Large-scale population-based surveys linked to administrative health databases as a source of data on health utilities in Australia. Value Health. 2022;25(9):1634–43.
Wang J, Zou R, Wu N, Fu H, He Y, Crawford P, et al. Depressive symptoms, social support, and health-related quality of life: a community-based study in Shanghai, China. Compr Psychiatry. 2022;113: 152292.
Park Y, Park K. Health-related quality of life and depressive symptoms of patients with chronic diseases and the general population before and during the COVID-19 pandemic in Korea. Front Psychol. 2023;14:1117369.
Olson B, Vincent W, Meyer JP, Kershaw T, Sikkema KJ, Heckman TG, et al. Depressive symptoms, physical symptoms, and health-related quality of life among older adults with HIV. Qual Life Res. 2019;28:3313–22.
Reyes-Gibby CC, Anderson KO, Morrow PK, Shete S, Hassan S. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health. 2012;21(3):311–8.
Atlantis E, Goldney RD, Eckert KA, Taylor AW, Phillips P. Trends in health-related quality of life and health service use associated with comorbid diabetes and major depression in South Australia, 1998–2008. Soc Psychiatry Psychiatric Epidemiol. 2012;47:871–7.
Malhi G, Mann J. Depression. Lancet. 2018;392(10161):2299–312.
Lundberg L, Johannesson M, Isacson DG, Borgquist L. Health-state utilities in a general population in relation to age, gender and socioeconomic factors. Eur J Public Health. 1999;9(3):211–7.
Fryback DG, Dasbach EJ, Klein R, Klein BE, Dorn N, Peterson K, et al. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making. 1993;13(2):89–102.
Yu T, Enkh-Amgalan N, Zorigt G, Hsu Y-J, Chen H-J, Yang H-Y. Gender differences and burden of chronic conditions: impact on quality of life among the elderly in Taiwan. Aging Clin Exp Res. 2019;31:1625–33.
Hanmer J, Kaplan RM. Update to the report of nationally representative values for the noninstitutionalized US adult population for five health-related quality-of-life scores. Value Health. 2016;19(8):1059–62.
Azizabadi Z, Aminisani N, Emamian MH. Socioeconomic inequality in depression and anxiety and its determinants in Iranian older adults. BMC Psychiatry. 2022;22(1):1–9.
Morasae EK, Forouzan AS, Majdzadeh R, Asadi-Lari M, Noorbala AA, Hosseinpoor AR. Understanding determinants of socioeconomic inequality in mental health in Iran’s capital, Tehran: a concentration index decomposition approach. Int J Equity Health. 2012;11:1–13.
Veisani Y, Delpisheh A. Decomposing of socioeconomic inequality in mental health: a cross-sectional study into female-headed households. J Res Health Sci. 2015;15(4):218–22.
Gandhi M, Tan RS, Ng R, Choo SP, Chia WK, Toh CK, et al. Comparison of health state values derived from patients and individuals from the general population. Qual Life Res. 2017;26:3353–63.
Farzianpour F, Foroushani AR, Badakhshan A, Gholipour M, Roknabadi EH. Quality of life for elderly residents in nursing homes. Glob J Health Sci. 2016;8(4):127.
Shrira A, Hoffman Y, Bodner E, Palgi Y. COVID-19-related loneliness and psychiatric symptoms among older adults: the buffering role of subjective age. Am J Geriatr Psychiatry. 2020;28(11):1200–4.
Ayalon L. There is nothing new under the sun: ageism and intergenerational tension in the age of the COVID-19 outbreak. Int Psychogeriatr. 2020;32(10):1221–4.
Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5): e256.
Yanover C, Mizrahi B, Kalkstein N, Marcus K, Akiva P, Barer Y, et al. What factors increase the risk of complications in SARS-CoV-2–infected patients? A cohort study in a Nationwide Israeli Health Organization. JMIR Public Health Surveill. 2020;6(3): e20872.
McCaffrey N, Kaambwa B, Currow DC, Ratcliffe J. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):1–12.
Fryback DG, Dunham NC, Palta M, Hanmer J, Buechner J, Cherepanov D, et al. US norms for six generic health-related quality-of-life indexes from the National Health Measurement study. Med Care. 2007;45(12):1162.
Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–8.
Saito Y, Nakamura S, Watanabe K, Ikegami H, Shinmura N, Sato S, et al. Age group differences in psychological distress and leisure-time exercise/socioeconomic status during the COVID-19 pandemic: a cross-sectional analysis during 2020 to 2021 of a cohort study in Japan. Front Public Health. 2023;11:1233942.
Balázs PG, Erdősi D, Zemplényi A, Brodszky V. Time trade-off health state utility values for depression: a systematic review and meta-analysis. Qual Life Res. 2023;32(4):923–37.
Kolovos S, Bosmans JE, van Dongen JM, van Esveld B, Magai D, van Straten A, et al. Utility scores for different health states related to depression: individual participant data analysis. Qual Life Res. 2017;26:1649–58.
Nease RF, Kneeland T, O’Connor GT, Sumner W, Lumpkins C, Shaw L, et al. Variation in patient utilities for outcomes of the management of chronic stable angina: implications for clinical practice guidelines. JAMA. 1995;273(15):1185–90.
Brockbank J, Krause T, Moss E, Pedersen AM, Mørup MF, Ahdesmäki O, et al. Health state utility values in major depressive disorder treated with pharmacological interventions: a systematic literature review. Health Qual Life Outcomes. 2021;19:1–17.
Ahmad H, van der Mei I, Taylor B, Zhao T, Xia Q, Palmer AJ. Does health-related quality of life differ between people with relapse onset and progressive onset Multiple Sclerosis? Multiple Scler Relat Disord. 2021;54: 103138.
Peasgood T, Brazier J. Is meta-analysis for utility values appropriate given the potential impact different elicitation methods have on values? Pharmacoeconomics. 2015;33:1101–5.
Sonntag M, Koenig H-H, Konnopka A. The estimation of utility weights in cost-utility analysis for mental disorders: a systematic review. Pharmacoeconomics. 2013;31:1131–54.
Le LK-D, Esturas AC, Mihalopoulos C, Chiotelis O, Bucholc J, Chatterton ML, et al. Cost-effectiveness evidence of mental health prevention and promotion interventions: a systematic review of economic evaluations. PLoS Med. 2021;18(5): e1003606.
Gureje O, Chisholm D, Kola L, Lasebikan V, Saxena S. Cost-effectiveness of an essential mental health intervention package in Nigeria. World Psychiatry. 2007;6(1):42.
Vos T, Haby MM, Magnus A, Mihalopoulos C, Andrews G, Carter R. Assessing cost-effectiveness in mental health: helping policy-makers prioritize and plan health services. Aust N Z J Psychiatry. 2005;39(8):701–12.
Acknowledgements
This paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) Survey 2022. The HILDA Project was initiated and is funded by the Australian Government Department of Social Services and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this paper, however, are those of the authors and should not be attributed to the universities, Department of Social Services or the Melbourne Institute. The authors are responsible for all findings and views expressed in this paper.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study did not receive any type of funding.
Conflicts of Interest
Muhammad Iftikhar ul Husnain, Mohammad Hajizadeh, Hasnat Ahmad and Rasheda Khanam have no conflicts of interest that are directly relevant to the content of this article.
Availability of Data and Material
The data used are not publicly available but can be made available upon reasonable request and with permission from the custodians/owners of HILDA database (Department of Social Services, Australia).
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
The code is available from the corresponding author on reasonable request.
Author Contributions
MIuH: conceptualisation, methodology, data curation, writing - original draft preparation. MH: conceptualization, supervision, writing - reviewing and editing. HA: data curation, methodology, writing - reviewing and editing. RK: conceptualisation, visualisation, investigation, writing - reviewing and editing.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
ul Husnain, M.I., Hajizadeh, M., Ahmad, H. et al. The Hidden Toll of Psychological Distress in Australian Adults and Its Impact on Health-Related Quality of Life Measured as Health State Utilities. Appl Health Econ Health Policy (2024). https://doi.org/10.1007/s40258-024-00879-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s40258-024-00879-z