Abstract
Objectives
There is increasing interest in expanding the elements of value to be considered when making health policy decisions. To help inform value frameworks, this study quantified preferences for disease attributes in a general public sample and examined which combination of attributes (disease profiles) are considered most important for research and treatment.
Methods
A discrete choice experiment (DCE) was conducted in a US general population sample, recruited through online consumer panels. Respondents were asked to select one of a set of health conditions they believed to be most important, characterized by attributes defined by a previous qualitative study: onset age; cause of disease; life expectancy; caregiver requirement; symptom burden (characterized by the Health Utilities Index with varying levels of ambulation independence, dexterity limitations, and degree of pain and discomfort); and disease prevalence. A fractional factorial DCE design was implemented using R, and 60 choice sets were generated (separated into blocks of 10 per participant). Data were analyzed using a mixed-logit regression model, and results used to assess the likelihood of preferring disease profiles. Based on individual attribute preferences, overall preferences for disease profiles, including a profile aligned with Duchenne muscular dystrophy (DMD), were compared.
Results
Fifty-two percent of respondents (n = 537) were female, and 70.6% were aged 18–54 years. Attributes considered most important were those related to life expectancy (odds ratio [OR], 95% confidence interval [CI] 1.88 [1.56–2.27] for a 50% reduction in remaining life expectancy vs no impact), and symptom burden (OR [95% CI] 1.84 [1.47–2.31] for severe vs mild burden). Greater importance was also found for pediatric onset, caregiver requirement, and diseases affecting more people. As an example of disease profile preferences, a DMD-like pediatric inherited disease with 50% reduction in life expectancy, extensive caregiver requirement, severe symptom burden, and 1:5000 prevalence had 2.37-fold higher odds of being selected as important versus an equivalent disease with adult onset and no life expectancy reduction.
Conclusions
Of disease attributes included in this DCE, respondents valued higher prevalence of disease, life expectancy and symptom burden as most important for prioritizing research and treatment. Based on expressed attribute preferences, a case study of an inherited pediatric disease involving substantial reductions to length and quality of life and requiring caregiver support has relatively high odds of being identified as important compared to diseases reflecting differing attribute profiles. These findings can help inform expansions of value frameworks by identifying important attributes from the societal perspective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
To help identify value elements important to consider in formulary decision-making processes and more carefully consider health plan members’ preferences in these decisions, a discrete choice experiment was conducted in a US general population sample. |
Attributes describing disease severity, pediatric onset, and higher prevalence were identified as important factors. |
These preferences can help inform how to expand value frameworks beyond the traditional metric of cost per QALY gained for stakeholders who wish to expand the perspectives being considered and incorporated. |
1 Introduction
In the USA, when deciding whether or not a treatment should be covered, formulary payers make decisions based on the perceived value provided by the treatment. Value elements traditionally considered include comparative clinical benefit, safety, budget impact, cost effectiveness, and impact on productivity [1]. There is an increasing interest in developing policies to guide health care decision-making that expand considerations beyond these traditional value elements, by accounting for a broader set of attributes. At present, these additional considerations relate to the nuances of the disease, and patients impacted are not routinely factored into such decisions [2]
The expansion of value assessment frameworks is a growing priority in the field of health care decision making [3]. Special Task Force report by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) identified and defined several components of value in a “value flower”, including the severity of disease, the value of hope, and equity, that have not historically been explored and quantified within traditional value assessment frameworks [4]. In 2019, the Memorial Sloan Kettering Cancer Center Drug Abacus also expanded its value assessment framework to include elements such as prognosis, disease rarity, and population health burden [5]. Similarly, the Institute for Clinical and Economic Review (ICER) updated its value assessment framework, to consider elements such as caregiver and family impacts, option of receiving future treatments, and complexity of regimen and real-world adherence and outcomes [6]. Other recent developments towards a more comprehensive assessment of treatment value include, for example, the generalized risk-adjusted cost-effectiveness analysis (GRACE) framework to adjust quantitative analyses for severity of disease [7], and the use of multi-criteria decision analysis in open-source economic models developed by the Innovation and Value Initiative [8]. Work by the PREFER initiative has found that internationally, health technology assessment (HTA) agencies are open to the incorporation of patient preferences into value assessment, although to date there is not a framework to do so formally and quantitatively [9].
Despite developments, there remains a lack of consensus on which concepts related to treatment value are most important from a societal perspective and the optimal methods needed to integrate these into treatment value assessments [2, 4, 10, 11]. To date, the most common implementation of expanded value assessment frameworks in the USA has been a “modified societal perspective” considered by ICER. That framework incorporates lost productivity costs in secondary scenario analysis but tends to omit factors that may be important from a societal perspective and influence cost-effectiveness outcomes in the quantitative analysis [12].
To help identify the important value elements to consider in formulary decision-making processes and more carefully consider societal preferences in these decisions, a more nuanced understanding is needed. Payers and decision makers are tasked with making access decisions that align with the perspectives of the individuals within their respective plans, and thus their coverage decisions should reflect the priorities that these individuals, including patients and non-patients enrolled in health plans place on diseases and their treatments.
This study aims to quantify, from the perspective of members of the general public, the importance of disease attributes that may not typically be accounted for in value assessments; and to understand which combinations of attributes would be prioritized by members of the general public to identify attributes that may be incorporated into future value frameworks. While societal preferences for disease attributes have been explored in the UK and Europe [13,14,15,16,17,18,19], to our knowledge, no such studies have been conducted in the USA with a focus on informing US value assessment to date. This could be partly because interest in considering societal perspectives in health care decision making began earlier in the UK (1990s) than the USA [20].
To illustrate these issues, Duchenne muscular dystrophy (DMD) was selected as a case study. A number of attributes identified by expanded value frameworks [4,5,6] apply in DMD; as it is a rare, severe genetic disease [21], DMD is characterized by relentless progressive muscular deterioration leading to loss of function in the lower limbs. Loss of ambulation (LOA) generally occurs before 12 years of age, with loss of function in the upper body giving rise to loss of independence, respiratory impairment, cardiomyopathy, and early mortality [21,22,23,24,25]. Given the pediatric onset of disease symptomatology and impact on patient function, DMD is associated with substantial need for caregiver support [26]. Characteristics related to DMD were therefore considered in selecting attributes to assess, to better understand their relative importance from the perspective of members of the general population. While the preferences of DMD patients and caregivers for treatment attributes have been explored qualitatively [27] and quantitatively [28,29,30], these studies did not focus on understanding the benefit-risk trade-offs patients and caregivers would be willing to make between relevant attributes of non-curative gene therapy, nor preferences for disease attributes presently unaccounted for in value assessments. The present study therefore adds to this literature, and builds on a prior qualitative study that investigated societal perspectives on disease and treatment attributes characterizing rare diseases [10].
2 Methods
A sample of adult respondents aged ≥ 18 years were recruited from the US general population to participate in an online survey. Respondents were recruited through online consumer panels. The quantitative survey included a discrete choice experiment (DCE) and demographic questions on age, sex, parental status, and personal/family history of chronic disease (autoimmune, cardiovascular, endocrine, gastrointestinal, infectious, mental health, neurology, oncology, rare disease, other). The design and analysis of the DCE were guided by best practice guidelines [31]. Before beginning the survey, as a comprehension check, respondents were asked to choose between two lives: Life A (living with a chronic lung disease for 8 years followed by death), and Life B (living in perfect health for 10 years followed by death). The survey ended for respondents who chose Life A. Those who chose Life B were asked to provide electronic click consent by agreeing to consent statements and proceeding to the survey. The survey preamble included instructions on how to answer the choice question and complete the choice task, an example choice task, and description of the attributes and levels. Respondents could review the attribute and level descriptions while completing the DCE choice task if they wished.
Respondents were each asked to complete 10 choice tasks. To limit cognitive burden, the choice sets were defined so that only three attributes varied within a given choice, while the remaining three remained constant across both options within the choice set. A total of 60 choice sets with varying “triplets” were generated and split into 6 blocks, with all participants randomly allocated to one block via the software program developed to administer the survey. Each participant was shown questions within their block in a randomized order. A standard dominance check was not included, as not all attributes had a natural objective ordering of “better” versus “worse”. Additional quality checks reported include the proportion of respondents “straight-lining” (i.e., selecting the option in the same position for all choice sets), as well as the proportion of participants for whom each respective attribute displayed attribute dominance (i.e., participants for whom all selections aligned with a single attribute in a common relative position compared to alternatives, e.g., a user always selecting the profile with the higher-frequency disease as “more important”, implying that they may tend to make their choice primarily based on disease frequency) [32, 33]. For the attribute dominance check, attributes were only assessed for choice tasks in which they differed across options. Given that in each choice task only three attributes were varied, even if a particular attribute dominated choices for a respondent, they would not fully dominate the collection of responses for that respondent, as they would have completed multiple choice sets without the dominating attribute factoring into their decisions as it would have been held constant across choices.
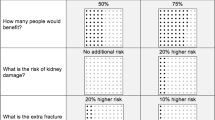
The DCE approach is a widely used method to elicit public preferences and understand trade-offs in healthcare [34, 35]. It involves asking participants to indicate their preferred hypothetical scenario from a set of scenarios, and the preferences are derived after a series of such choices are made. In this study, scenarios were developed using multiple disease characteristics and presented to participants as disease profiles, reflecting the complexity of health care decision making. Attributes and level definitions were developed based on prior in-depth qualitative interviews in an initial effort to understand how aspects of diseases and treatments were prioritized and why [10]. Based on this work, as well as value elements identified in the published literature, the final set of attributes within the DCE included: age of onset (children, adults, older adults); cause (inherited vs acquired); life expectancy (no impact, 10% reduction, 50% reduction); caregiver requirement (none, moderate, extensive); symptom burden (mild, moderate, severe) and disease prevalence (or ‘frequency’; expressed as 1:10, 1:300, 1:5000, 1:10,000, 1:2,000,000). For the symptom burden attribute, the Health Utilities Index-3 (HUI-3) was used to characterize mild, moderate, and severe levels (Fig. 1). For the life expectancy attribute, years of life remaining was based on the United States life expectancy, rounded to the nearest decade of 80 years [36]. See Supplementary Appendix 1 for attribute and level descriptions. To reduce the burden and complexity of the survey, symptom burden was described by the subset of HUI-3 attributes most relevant to DMD, including need for ambulation equipment, dexterity limitations, and degree of pain and discomfort. The disease profiles were developed to be treatment agnostic (i.e., intended to be interpreted as the relevant descriptions based on any current standard of care).
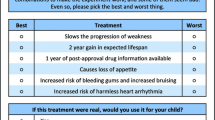
Symptom burden levels. A fractional factorial design was utilized, by maximizing D-efficiency, and implemented using R. An example choice set is shown in Fig. 2
Following initial development of the survey materials, the survey was initially pre-tested with a convenience sample of five respondents, which led to minor re-wording of some attribute descriptions for clarity. A pilot analysis was conducted after the first 50 responses were collected, and no concerns were noted regarding data quality or face validity of results; the remaining responses were then collected.
The relevance and ease of completing the DCE was evaluated through semi-structured qualitative and think-aloud interviews, and a pilot study; the six attributes included in the survey captured a sufficient range of disease characteristics without making choices excessively complex for respondents.
Data were collected over a three-month period from October to December 2021. Respondents were compensated for their participation in the form of panel points. Age and gender recruitment quotas were used to approximately align with US population norms [37].
The DCE results were analyzed using a mixed-logit regression model with normally distributed random effects included for all attributes; the output was expressed as the odds ratio (OR) with 95% confidence interval (CI) of an attribute being selected as most important. All attributes were defined as categorical variables and dummy-coded versus a reference level. Analyses were conducted for the overall sample and for subgroups defined by self-report of personal and family history of chronic disease. A “bundled” approach is also presented, in which the probability of selecting a full profile of attributes is estimated based on the mixed-logit regression, for comparison to an alternative profile, for example to compare overall preferences for a rare severe disease versus a more common and less severe disease. This approach is used to compare a profile similar to DMD versus an alternative profile that is similar other than life expectancy implications and age of onset. This allows for assessment of preferred trade-offs across distinct combinations of attributes. A visualization tool was developed to facilitate these comparisons (Supplementary Appendix 2). This study received Institutional Review Board (IRB) approval through Advarra, Inc.
3 Results
The study sample included 537 respondents. Amongst the respondents who screened-in and passed the comprehension question, a 39% dropout rate was observed, with respondents continuing to be enrolled until quotas were met. The average time to complete the survey was 12.6 minutes (median 8.7 minutes; interquartile range 5.5–13.8 minutes).
The majority of respondents (70.6 %) were aged 18 to 54 years, over half (52.1 %) were female, and most (68.9 %) were White. The most frequent category of highest education level completed was college/university (43.0 %) while the most common income category was $50,000–$99,000 USD (25.7 %) (Table 1). The observed sociodemographic distribution was relatively consistent with current US norms [37,38,39]. Approximately one-third of respondents (34.5 %) reported a self-history of chronic disease (most commonly mental health or auto-immune diseases), and 31.1% reported a family history of chronic disease (most commonly cardiovascular or mental health diseases; Table 2).
The most important disease attributes identified by participants were life expectancy (OR [95% CI], 1.88 [1.56–2.27] for a 50% reduction in remaining life expectancy vs no impact), disease frequency (OR [ 95% CI], 0.39 [0.32–0.50] for 1:2,000,000 vs 1:10) and symptom burden (OR [ 95% CI], 1.84 [1.47–2.31] for severe vs mild burden) (Fig. 3). For respondents reporting a self- and/or family history of chronic disease, further weight was placed on life expectancy (Fig. 3). For example, for individuals with self-history of chronic disease, the OR (95% CI) for a disease associated with a 50% life expectancy reduction was 2.41 (1.71–3.41) compared to 1.85 (1.46–2.35) for individuals without a history of chronic disease. For individuals with a family history of chronic disease, the OR (95% CI) associated with a 50% life expectancy was 2.49 (1.71–3.63) vs 1.61 (1.30–1.99) for those with no family history.
Results of mixed-effects logit regression of discrete choice experiment, stratified by self-history of chronic disease family history of chronic disease. *For all attributes, an odds ratio < 1.0 indicates that the alternative option was found to be less important than the reference category for the attribute, while odds ratio >1.0 indicates that the alternative option was found to be more important than the reference category for the attribute
Increased odds of identifying diseases as more important were associated with them having the attributes of childhood onset and/or extensive caregiver requirement. Respondents reporting a self-history of chronic disease placed additional weight on extensive caregiver requirements (for diseases with extensive caregiver support the OR [95% CI] was 2.12 [1.46–3.06] for individuals with a history of chronic disease vs 1.40 [1.10–1.79] for individuals with no history; Fig. 3). Analyses were also stratified by whether respondents were a parent of a child aged <18 years, but no notable relationships were observed (results not shown).
The results of the mixed-logit regression were also used to assess the relative likelihood of selecting disease profiles (that reflect pre-defined bundles of disease attributes). In the overall respondent population, the combination of attributes most closely associated with DMD was assessed (1:5,000 prevalence, childhood onset, inherited, extensive caregiver requirement, poor life expectancy prognosis and severe symptom burden) (Fig. 4). Based on regression estimates, the probability of selecting this profile is estimated to be 83.2 %. This increases to 91.3% in the subgroup of respondents reporting a history of chronic disease, or 84.8% in the subgroup reporting family history of chronic disease. In the overall respondent population, the DMD profile is associated with an increased odds 2.37-times higher than selecting a hypothetical disease profile with adult onset and removing the life-expectancy impact from 50% reduction to none (other attributes remaining constant) (Fig. 4). For an adult-onset condition for which the life expectancy attribute for the comparison profile remains at 50% reduction but the symptom burden attribute is changed from severe to mild, the corresponding increased odds of selecting the DMD profile exhibits a small decrease from 2.37- to 2.32-times higher than the comparison profile. If both the life expectancy and symptom burden attributes are changed to the mildest levels, the odds of selecting DMD versus the comparison adult-onset disease profile are 4.37-times higher. While only a single comparison is shown in Figure 4 (DMD profile vs a comparison profile with the life expectancy attribute varied), an interactive tool has been developed to facilitate data exploration across all attributes and populations (overall and stratified by self- and family-history of chronic disease); this tool is available at https://diseasepreferences.broadstreetheor.com:
The proportion of respondents who straight-lined their responses was 6.2 %. In the attribute dominance it was found that the proportion of respondents who always selected an option with their preferred level on an individual attribute were: 18.6% for disease prevalence, 9.5% for onset age, 6.5% for cause, 18.2% for life expectancy, 20.5% for caregiver burden, and 7.9% for symptom burden. While there are not established thresholds for comparison, given that the DCE was designed to have 2 options to select from per choice set and only 3 attributes varying per choice, the magnitude of straight-lining and attribute dominance observed is likely within expected ranges and are aligned with values reported by other DCE studies [33].
4 Discussion
There is a lack of consensus on whether the current frameworks for assessing disease impact and value of treatment need to be expanded, and if so how to prioritize disease attributes beyond those traditionally considered in decision making. For example, observers debate whether these elements should be quantitatively incorporated into a deliberative cost-effectiveness process or be considered outside of the cost-effectiveness process. In weighing the various options, it is important to better understand general public preferences, to help ensure that disease features valued most strongly are appropriately accounted for by decision makers. In this US general population sample, particularly those with a history of chronic disease, respondents valued life expectancy (premature mortality), and symptom burden (prospective morbidity) as the most important attributes.
The preferences revealed in this study are consistent with preferences for attributes identified as important in a previous qualitative study, in that symptom burden and the impact on life expectancy were ranked as highly important from the perspective of the general public [10]. The results reported here also align with findings of a UK person trade-off and DCE study evaluating societal preferences on funding treatments for orphan drugs for rare diseases [40]. Results of that study indicated a preference to fund treatments that prolong survival, or for diseases that are debilitating or life threatening [40]. However, in another DCE from the UK, members of the general public preferred to provide treatments to health conditions with characteristics such as a known cause, rapid diagnosis, curable, and no reliance on care; and limited life expectancy was not prioritized [14]. These contrasting results suggest heterogeneity in public preferences for health care priority setting [13]; these may be a reflection of a number of different factors including geography and how health care is structured. Differences in preferences between patient populations and members of the general public have also been noted. For example, the Patient-Driven Values in Healthcare Evaluation (PAVE) initiative at the University of Maryland has conducted research to understand preferences for elements of value, although from a patient perspective. Results from these patient stakeholder engagement exercises suggested that high priority elements of value included aspects of treatment (such as tolerability, and risk/benefit profile) as well as economic considerations [41].
While the value of equity was not directly assessed within the DCE attributes of the present study, it is notable that the findings related to the importance of pediatric-onset disease and life expectancy are aligned with the equity-based ‘fair innings’ concept, whereby everyone deserves a “normal” lifespan and anything short of this is inequitable [42].
Respondents in the present study valued diseases with higher prevalence as more important than rare orphan diseases, a finding consistent with a number of other studies [40, 43, 44]. Responses may be sensitive to the use of ‘zero-sum’ framing, where respondents must choose between two competing options (i.e., prevalent vs rare disease), and may not understand the opportunity cost associated with having a rare disease [40, 43]. It should be noted that not all existing evidence is consistent regarding the value of treating higher prevalence diseases. For example, in a DCE completed by members of the general public in the Netherlands, respondents preferred to treat rare diseases over more prevalent diseases, although it remained that disease prevalence was rated the least important of the attributes considered [19]. Future research that focuses on the nuances and practical considerations of rare diseases (e.g., unmet need due to limited treatment availability and lack of disease-specific resources) could provide insight on whether elucidating such concepts to respondents might influence stated preferences; or whether the preference for prioritizing non-rare diseases would hold.
This study has a number of limitations. First, although the sample size was large, it may not be representative of the US general public with respect to geography, race, and/or ethnicity. Second, several simplifying measures to the design were applied to reduce the burden and complexity of the survey for respondents, which may have limited the capture of perspectives on some relevant disease attributes. For example, ambulation, dexterity, and pain/discomfort were selected as attributes to describe disease symptom burden, but other factors such as vision, hearing, cognitive function, and/or mental health impacts may more comprehensively capture symptom burden in some disease populations. As an additional simplifying measure, the scope of the survey was limited to tangible attributes of a disease from a patient perspective, and while this extends beyond the quality-adjusted life year (QALY), it does not extend to value flower elements such as value of hope or insurance value. Given the relative complexity of some value flower concepts it is anticipated that dedicated studies should be conducted to better understand preferences around these values, to ensure that respondents are able to provide nuanced responses without being overburdened. Finally, the design of the survey did not allow for the evaluation of interactions between the attributes. It is possible that caregiver requirement is partly addressed by symptom burden, so preferences around caregiver requirement may have been overvalued.
This study adds to previous qualitative work by quantifying societal preferences for specific disease attributes and provides an additional perspective on value elements that might affect treatment and research prioritization decisions.
5 Conclusion
On the basis of their preferences for disease attributes included in the DCE, this US general population sample may be more inclined to consider diseases more important for research and treatment if they impact life expectancy, or have a high prevalence and symptom burden. Based on these attribute preferences, a case study of an inherited disease with pediatric onset, premature mortality, substantial morbidity, and requiring caregiver support has relatively high odds of being identified as important, compared to diseases reflecting different attributes.
References
Jakab I, Whittington MD, Franklin E, et al. Patient and payer preferences for additional value criteria. Front Pharmacol. 2021;12: 690021.
Neumann PJ, Garrison LP, Willke RJ. The History and Future of the “ISPOR Value Flower”: addressing limitations of conventional cost-effectiveness analysis. Value Health. 2022;25(4):558–65.
Kristensen FB, Husereau D, Huić M, et al. Identifying the need for good practices in health technology assessment: summary of the ISPOR HTA Council Working Group Report on Good Practices in HTA. Value Health. 2019;22(1):13–20.
Lakdawalla DN, Doshi JA, Garrison LP Jr, Phelps CE, Basu A, Danzon PM. Defining elements of value in health care—a health economics approach: an ISPOR Special Task Force report [3]. Value in Health. 2018;21(2):131–9.
Lanitis T, Ambavane A, Zheng Y, Schlichting M, Phatak H. Value assessment of immuno-oncology in the treatment of rare tumors in the era of accelerated conditional approvals. Future Oncol. 2019;15(35):4057–67.
Institute for Clinical and Economic Review (ICER). 2020-2023 Value Assessment Framework. Boston January 31, 2020 2020.
Lakdawalla DN, Phelps CE. Health technology assessment with diminishing returns to health: the generalized risk-adjusted cost-effectiveness (GRACE) approach. Value Health. 2021;24(2):244–9.
Innovation and Value Initiative. Open-source value project. https://thevalueinitiative.org/open-source-value-project/. Accessed 12 Apr 2023.
van Overbeeke E, Forrester V, Simoens S, Huys I. Use of patient preferences in health technology assessment: perspectives of Canadian, Belgian and German HTA Representatives. Patient. 2021;14(1):119–28.
Szabo SM, Audhya IF, Feeny D, Neumann P, Malone DC, Gooch KL. Societal perspectives on disease and treatment attributes characterizing rare diseases: a qualitative study from the United States. J Patient-Report Outcomes. 2022;6(1):1–13.
Shafrin J, Dennen S, Pednekar P, et al. For which diseases do broader value elements matter most? An evaluation across 20 ICER evidence reports. J Manag Care Spec Pharm. 2021;27(5):650–9.
Kruzikas DT, Malone DC, Pham S, Reinsch TK, Akehurst R. HTA and economics in the United States: a systematic review of ICER reports to evaluate trends, identify factors associated with recommendations, and understand implications. J Manag Care Spec Pharm. 2020;26(12):1548–57.
Mason H, van Exel J, Baker R, et al. From representing views to representativeness of views: Illustrating a new (Q2S) approach in the context of health care priority setting in nine European countries. Soc Sci Med. 2016;166:205–13.
Morrell L, Buchanan J, Rees S, Barker RW, Wordsworth S. What aspects of illness influence public preferences for healthcare priority setting? A discrete choice experiment in the UK. Pharmacoeconomics. 2021;39:1443–54.
Nicolet A, van Asselt AD, Vermeulen KM, Krabbe PF. Value judgment of new medical treatments: Societal and patient perspectives to inform priority setting in The Netherlands. PLoS ONE. 2020;15(7): e0235666.
Reckers-Droog V, van Exel J, Brouwer W. Equity weights for priority setting in healthcare: severity, age, or both? Value in Health. 2019;22(12):1441–9.
Rowen D, Brazier J, Mukuria C, et al. Eliciting societal preferences for weighting QALYs for burden of illness and end of life. Med Decis Making. 2016;36(2):210–22.
Shah KK, Tsuchiya A, Wailoo AJ. Valuing health at the end of life: A stated preference discrete choice experiment. Soc Sci Med. 2015;124:48–56.
Van de Wetering E, Van Exel N, Rose J, Hoefman R, Brouwer W. Are some QALYs more equal than others? Eur J Health Econ. 2016;17:117–27.
Mitton C, Smith N, Peacock S, Evoy B, Abelson J. Public participation in health care priority setting: a scoping review. Health Policy. 2009;91(3):219–28.
Wein N, Alfano L, Flanigan KM. Genetics and emerging treatments for Duchenne and Becker muscular dystrophy. Pediatr Clin North Am. 2015;62(3):723–42.
Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17(3):251–67.
Yiu EM, Kornberg AJ. Duchenne muscular dystrophy. J Paediatr Child Health. 2015;51(8):759–64.
Seferian AM, Moraux A, Canal A, et al. Upper limb evaluation and one-year follow up of non-ambulant patients with spinal muscular atrophy: an observational multicenter trial. PLoS ONE. 2015;10(4): e0121799.
Mirski KT, Crawford TO. Motor and cognitive delay in Duchenne muscular dystrophy: implication for early diagnosis. J Pediatr. 2014;165(5):1008–10.
Landfeldt E, Edström J, Buccella F, Kirschner J, Lochmüller H. Duchenne muscular dystrophy and caregiver burden: a systematic review. Dev Med Child Neurol. 2018;60(10):987–96.
Landrum Peay H, Fischer R, Tzeng JP, et al. Gene therapy as a potential therapeutic option for Duchenne muscular dystrophy: a qualitative preference study of patients and parents. PLoS ONE. 2019;14(5): e0213649.
Crossnohere NL, Fischer R, Vroom E, Furlong P, Bridges JF. A comparison of caregiver and patient preferences for treating duchenne muscular dystrophy. Patient-Patient-Centered Outcomes Res. 2022;15(5):577–88.
Hollin IL, Peay HL, Apkon SD, Bridges JF. Patient-centered benefit–risk assessment in Duchenne muscular dystrophy. Muscle Nerve. 2017;55(5):626–34.
Peay HL, Hollin I, Fischer R, Bridges JF. A community-engaged approach to quantifying caregiver preferences for the benefits and risks of emerging therapies for Duchenne muscular dystrophy. Clin Ther. 2014;36(5):624–37.
Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value in Health. 2011;14(4):403–13.
Janssen EM, Marshall DA, Hauber AB, Bridges JF. Improving the quality of discrete-choice experiments in health: how can we assess validity and reliability? Expert Rev Pharmacoecon Outcomes Res. 2017;17(6):531–42.
Johnson FR, Yang J-C, Reed SD. The internal validity of discrete choice experiment data: a testing tool for quantitative assessments. Value Health. 2019;22(2):157–60.
Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72.
Arias E, Tejada-Vera B, Kochanek KD, Ahmad FB. Provisional life expectancy estimates for 2021. US Centers for Disease Control and Prevention. National Center for Health Statistics (U.S.) Vital Statistics Rapid Release. 2022. https://stacks.cdc.gov/view/cdc/118999.
Blakeslee L, Caplan Z, Meyer JA, Rabe MA, Roberts AW. Age and sex composition: 2020. Washington, DC; 2023. C2020BR-06.
McElrath K, Marti M. Bachelor’s degree attainment in the United States: 2005 to 2019. Washington, DC: U.S. Census Bureau; 2021. ACSBR-009.
Shrider EA, Kollar M, Chen F, Semega J. Income and poverty in the United States: 2020. Washington, DC: U.S. Census Bureau; 2021. ACSBR-009.
Bourke SM, Plumpton CO, Hughes DA. Societal preferences for funding orphan drugs in the United Kingdom: an application of person trade-off and discrete choice experiment methods. Value Health. 2018;21(5):538–46.
dosReis S, Butler B, Caicedo J, et al. Stakeholder-engaged derivation of patient-informed value elements. Patient. 2020;13(5):611–21.
Williams A. Intergenerational equity: an exploration of the “fair innings” argument. Health Econ. 1997;6(2):117–32.
Dragojlovic N, Rizzardo S, Bansback N, Mitton C, Marra CA, Lynd LD. Challenges in measuring the societal value of orphan drugs: insights from a Canadian stated preference survey. Patient. 2015;8(1):93–101.
Desser AS, Gyrd-Hansen D, Olsen JA, Grepperud S, Kristiansen IS. Societal views on orphan drugs: cross sectional survey of Norwegians aged 40 to 67. BMJ. 2010;341: c4715.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Sarepta Therapeutics Inc.
Competing Interests and Funding
IA and KG are employees of Sarepta Therapeutics Inc (no grant number). KMJ, JD, and SMS are employees of Broadstreet HEOR, which received funds from Sarepta to conduct this study. DF, PN, and DCM received consulting fees related to this work. DF has a proprietary interest in Health Utilities Incorporated, Dundas, Ontario, Canada. HUInc. distributes copyrighted Health Utilities Index (HUI) materials and provides methodological advice on the use of HUI.
Consent to Participate
In the conduct of this study, survey respondents provided electronic click consent after reviewing study information, by agreeing to consent statements and proceeding to the survey.
Consent for Publication
Survey respondents were informed that results may be published prior to providing consent to participate.
Availability of Data and Material
De-identified data and study materials are available from the corresponding author on request.
Code Availability
Fractional factorial design and analysis R code are available from the corresponding author on request.
Authors' Contributions
KJ, IA, JD, DF, PN, DM, SS, and KG conceived the study, interpreted the results, and prepared the manuscript. KJ, IA, JD, DF, PN, DM, SS, and KG developed/reviewed the survey. KJ analyzed the data. All authors critically reviewed the manuscript and approved the final draft.
Ethics Approval
This study received institutional review board (IRB) approval through Advarra, Inc. (Pro00052976). This study was performed in accordance with the Declaration of Helsinki—Version 2008.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Johnston, K.M., Audhya, I.F., Dunne, J. et al. Comparing Preferences for Disease Profiles: A Discrete Choice Experiment from a US Societal Perspective. Appl Health Econ Health Policy 22, 343–352 (2024). https://doi.org/10.1007/s40258-023-00869-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00869-7