Abstract
Background
Prevention programmes typically incur short-term costs and uncertain long-term benefits. We use the National Health Service (NHS) England Diabetes Prevention Programme (NHS-DPP) to investigate whether behaviour change programmes may be cost-effective even within the short-term participation period.
Methods
We analysed 384,611 referrals between June 2016 and March 2019. We estimated NHS costs using implementation costs and provider payments. We used linear regressions to relate utility changes to the number of sessions attended, based on responses to the five-level EQ-5D (EQ-5D-5L) at baseline and final session for 18,959 participants. We then calculated the corresponding quality-adjusted life year (QALY) change for all 384,611 referrals by combining the estimated regression coefficients with the observed level of attendance, with individuals that did not attend any programme sessions being assumed to experience zero benefit. In secondary analysis, we added weight change, recorded for 18,105 participants to the regression and applied predicted values to all referrals with missing weight change values estimated using multiple imputation with chained equations. We then estimated the cost-per-QALY generated.
Results
Average cost per referral was £119 (standard deviation: £118; 2020 price year, UK £ Sterling). Each session attended was associated with a 0.0042 increase in utility (95% confidence interval (CI): 0.0025–0.0059). This generated 1,773 QALYs across all referrals (95% CI: 889–2,656). Cost-per-QALY was £24,929 (95% CI: £16,635–49,720) when implementation costs were excluded. Secondary analysis showed each session attended and kilogram of weight lost were associated with 0.0034 (95% CI: 0.0016–0.0051) and 0.0025 (95% CI: 0.0020–0.0031) increases in utility, respectively. These generated 1,542 QALYs, at a cost-per-QALY of £28,661 when implementation costs were excluded.
Conclusion
Participants experienced small utility gains from session attendance and weight loss during their programme participation. These benefits alone made this low-cost behaviour change programme potentially cost-effective in the short-term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The NHS Diabetes Prevention Programme was associated with health gains even in the short-term programme participation period. |
These health gains alone are large enough to suggest the programme could be cost-effective, even before considering the longer-term benefits associated with diabetes prevention. |
These results support investment in public health interventions, suggesting returns on investment may occur sooner than generally thought. |
1 Introduction
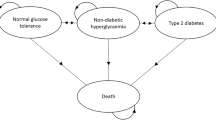
There is a rising burden of non-communicable diseases, predominantly caused by modern lifestyle factors such as smoking, poor diet and physical inactivity [1]. Prevention programmes that provide structured education on nutrition, physical activity and weight loss are being introduced to prevent such conditions from developing. However, commissioners may be reluctant to fund such programmes, given that the delivery costs are usually incurred in the short-term, whilst the anticipated benefits are expected to occur in the long-term and may be uncertain. Public health budgets may also be the first to be cut when faced with budget reductions, with short-term needs taking precedent, and a preference for generating benefits immediately [2]. Indeed there is evidence that public health budgets in England have recently been cut by up to 25% and that this is impacting prevention initiatives particularly [3]. The ability to demonstrate benefits over a shorter time horizon may encourage investment in public health interventions, balancing the needs for immediate gains with the longer-term goal of prevention. We evaluate the short-term costs and benefits of one such prevention programme to see whether investment in such programmes offers value for money to commissioners based only on the benefits observed during the short-term of programme participation. In 2016, England introduced the largest national diabetes prevention programme to date, known as the National Health Service (NHS) Healthier You: Diabetes Prevention Programme (NHS DPP). Type 2 diabetes is a condition of particular concern because of the burden it places on patients and healthcare systems, and yet, it is largely preventable [4].
Studies have shown that completion of the NHS DPP is associated with an average weight loss of 3.6 kg (95% confidence interval (CI) −3.6–−3.5) [5], a reduction in glycated haemoglobin (HbA1c) of 2.04 mmol/mol (95% CI −2.12–−1.96) [6] and reduced risk of conversion to type 2 diabetes [7]. The introduction of the NHS DPP has also been shown to have reduced population incidence of type 2 diabetes in England, with general practices in the first wave of the DPP experiencing an 8% reduction in cases of new type 2 diabetes compared with practices that were yet to implement the programme. This is equivalent to approximately 17,800 cases of type 2 diabetes prevented in 2018–2019 [8].
However, there has yet to be an evaluation exploring the real-world cost-effectiveness of the NHS DPP. We estimate the costs of delivering the NHS DPP in its first 3 years and the benefits accrued by those referred in terms of quality adjusted life years (QALYs) during the period in which they participated in the programme. This is the first time that a study has evaluated the costs of delivering the NHS DPP or the benefits associated with participation in terms of QALYs.
2 Methods
2.1 NHS DPP
The NHS DPP is a nationwide programme targeting adults across England identified as being at high risk of developing type 2 diabetes. The programme is jointly led by NHS England, Public Health England and Diabetes UK, but is delivered by commercial providers selected via a national, competitive procurement process.
The programme involves attending group-based behaviour change sessions which include structured education on nutrition, physical activity and weight loss [9]. Providers are free to choose the location for the group sessions, but most often they are held in local, community venues [10]. The programme usually takes 9–12 months for an individual to complete, and NHS England define completion of the programme as attending at least 60% of available sessions. There were four providers during the period we examine. Of these, three providers delivered programmes consisting of a total of 13 sessions, with the remaining provider’s programme consisting of a total of 18 sessions.
Adults aged 18 years and over are eligible to be referred to the NHS DPP if a recent blood test shows HbA1c within the range of 42–47 mmol/mol (6.0–6.4%) or fasting plasma glucose level of 5.5–6.9 mmol/L [11]. Most often, individuals are identified in general practice during an NHS Health Check, opportunistically during a consultation, or via searches of general practice records where letters may be sent to patients inviting them to contact their local provider [12]. To make a referral, practitioners need to first gain patient consent to pass their details onto the local NHS DPP provider, who then arranges an initial assessment to confirm eligibility.
2.2 Data
2.2.1 Referrals
We obtained an extract of the referral-level data collected by programme providers, referred to as the minimum dataset. This extract includes referrals received by NHS DPP providers from 1 June 2016 (when the programme began) to 31 March 2020. To ensure that we only considered referrals who would have had enough time to complete the programme, we restricted our analysis cohort to those who were referred prior to 1 April 2019.
This dataset includes the date a referral was made and subsequent level of attendance on the programme. Individuals referred to the programme may or may not attend an initial assessment or any of the programme sessions. A flow chart showing the different levels of NHS DPP attendance for our analysis cohort is shown in Supplementary Material Fig. 1.
As part of the referral, basic demographic information was collected, including sex, age and the level of socio-economic deprivation in the individual’s area of residence. For individuals who attended the initial assessment, further information was collected including the individual’s ethnicity, weight, body mass index (BMI) and health-related quality of life [measured using the five-level EQ-5D (EQ-5D-5L)]. The EQ-5D-5L consists of five dimensions (mobility, self-care, usual activities, pain and discomfort, and anxiety and depression), where each dimension has five severity levels that are described by statements appropriate to that dimension [13]. These weight and EQ-5D-5L measures were collected again at the final scheduled programme session (either session 13 or 18, depending on the provider).
The weight and quality of life measures were often missing, for two main reasons. Firstly, data were missing if an individual did not attend the initial assessment or final scheduled programme sessions where this information was collected. Secondly, the provider may have failed to collect all information at these sessions. As failure to attend one of the sessions did not mean that individuals were excluded from subsequent sessions, there was considerable variability in the number of sessions attended amongst those from whom initial assessment and final programme session data were collected.
2.2.2 Costs
Costs to NHS England associated with the programme included the provider reimbursement for programme delivery as well as the costs associated with implementing and supporting the programme. Provider contract data was provided by NHS England. This data details the type of contract held by providers in each area the programme was delivered and the total amount a provider could be reimbursed for a referred individual who completed all sessions for each year the contract was in place, as well as the percentages of the contract value linked to each of the programme milestones. These programme milestones were a series of attendance markers over the course meant to encourage providers to keep participants engaged and attending. Providers were reimbursed a percentage of their total cost for each milestone that a participant met.
Providers competitively bid to deliver the programme in sites across England. At each site, provider contracts could be either: ‘activity only’ or ‘fixed and activity’ payment contracts. Under ‘activity only’ contracts, providers only received payments when participants reached set retention milestones, defined as attending a set number of sessions. The sessions corresponding to each milestone differed across the providers, as detailed in Table 1. The percentage of the contract value received for each milestone also varied across the different providers. Sites on a ‘fixed and activity’ payment contract received 25% of the estimated contract value upfront to facilitate implementation. Thus, the total amount that could be received by a provider per participant of the programme was dependent on the milestone percentages and the agreed total payment for an individual completing the course. The total payments varied by sites within the same provider and by year of the contract.
Implementation and support costs for contract management and coordination were provided by NHS England to regions and clinical networks to help establish the programme. Regions were free to choose how these funds were allocated. Some implementation costs were used to provide incentives to general practices to identify individuals at high risk of developing type 2 diabetes as well as to encourage referrals [14], whilst other areas invested in additional resources such as hiring staff to help with case finding or administrative and IT support [15]. Information on the amount of implementation and support costs for the NHS DPP is not publicly available. NHS England advised that the implementation funds were provided to regions and clinical networks to support a wider diabetes agenda, and as such it would be difficult to attribute the exact amount used solely for the NHS DPP. We therefore used estimates published in the 2016 impact assessment for the NHS DPP [16].
2.3 Analysis
We first present descriptive statistics of the number of referrals received by the NHS DPP providers, along with the characteristics of the individuals referred. We also present the participant retention rates at each of the payment milestones and the average cost per referral received.
We then compared the total costs borne by NHS England associated with delivering the programme to the estimated total benefits to the individuals who were referred, measured in terms of QALYs. We considered all referrals made to the programme, rather than just those who participated in programme sessions, as costs were still incurred for those who did not participate. Omitting these individuals from our calculations would have therefore resulted in the overall cost-effectiveness of the programme being overestimated. The time horizon of analysis is the length of time from referral to the final programme session attended, for each referral.
Where possible, we follow the recommendations set out in the National Institute for Health and Care Excellence (NICE) Reference Case for conducting economic evaluations [17].
2.3.1 Costs
We considered the cost of individuals being referred and participating in the NHS DPP as well as the implementation and central running costs of the national programme, from the perspective of NHS England. These cost elements cover all costs incurred by NHS England in delivering the programme.
Costs are presented in UK £ sterling using a common price year of 2020. Where applicable, costs were inflated using the annual Office for National Statistics Consumer Price Index (all items) [18]. Due to the time period over which costs were incurred, discounting was not required.
We used the cost information from the provider contracts together with the number of referrals and the level of attendance for each individual referral recorded within the minimum dataset to calculate the amount providers were reimbursed for each referral received. We calculated the total cost of all referrals made by 1 April 2019, based on their subsequent participation level as recorded by 31 March 2020.
In some cases, the date a referral was recorded as being received by a provider fell outside of the contract dates provided by NHS England (applicable to 3.1% of all referrals). In this instance, if the recorded date of referral was prior to the contract being established, we costed the referral according to the value of the first year of the contract. If it occurred after, we used the price from the final year of the contract. For 4.3% of referrals, we were unable to assign a contract to the referral because the provider did not match with the contract information we were provided with for that site. In these cases, we assigned an average unit cost based on other referrals to the same provider with the same level of attendance.
We used estimates published in the 2016 impact assessment of the NHS DPP [16], which estimated that implementation costs would total £8.4 million for the first 3 financial years (2016/17–2018/19). These were described as taking into account: contract management and coordination, quality assurance, regional support and funding to support local implementation.
2.3.2 Benefits
We estimated the benefits of the NHS DPP in terms of the QALYs experienced by individuals referred to the programme, from initial assessment up to programme completion. Due to the timing of EQ-5D-5L collection at initial assessment rather than referral, we made the assumption that, between referral and initial assessment, individuals did not derive any utility benefit from the programme. As participants were free to stop attending the programme at any time, the length of this time horizon varied across individuals, although typically to be delivered in full, the programme takes between 9–12 months.
We valued the responses to the EQ-5D-5L questionnaire, recorded at initial assessment and final planned programme session using the Crosswalk value set [19] to generate a utility score, as currently recommended in the NICE Reference Case [17].
To estimate quality-of-life changes for participants we considered two indicators of programme benefit:
-
(1)
The number of programme sessions attended
-
(2)
Weight change recorded between initial assessment and final planned session
First, we estimated utility gains for participants considering only the number of sessions attended, as the level of attendance is recorded for all referrals. We then carried out secondary analyses which estimated utility gains by considering the number of sessions attended in addition to participant weight change amongst the participants where this was recorded.
To estimate the overall impact of the programme, we then summed all QALY changes related to programme participation for all of the referrals received prior to the 1 April 2019. Due to the time period over which benefits were incurred, discounting was not required.
2.3.3 Main Analysis – Benefit from Session Attendance
We used ordinary least squares (OLS) regression analysis to relate final utility to the number of sessions attended, controlling for utility score at initial assessment and a range of sociodemographic characteristics. These characteristics were: sex, referral age category (and the interaction of these), index of multiple deprivation quintile (a composite measure of area deprivation across seven domains [20]) and four ethnicity categories, defined as: ‘white’ (comprising those reporting as British or mixed British, Irish or other white), ‘Asian’ (comprising those reporting Indian, Pakistani, Bangladeshi, Chinese or ‘other Asian’ ethnicity), ‘Black’ (comprising those reporting Caribbean, African or ‘other Black’ ethnicity) and ‘Mixed’ (comprising those with a Mixed or ‘other’ ethnic background). As utility scores have an upper bound of one, we explored using Tobit regression models with an upper limit of one. However, we found that OLS regressions consistently produced lower root mean squared error values compared with the equivalent sigma value of the Tobit models, indicating more accurate model predictions. This concurs with previous research by Wu et al., who also found OLS to outperform Tobit and two-part regression models when analysing health-related quality of life data [21].
We estimated these regressions separately for the three providers who offered 13 sessions and the single provider that offered 18 sessions, as the number of sessions attended had different meaning across these two groups.
We estimated these regressions on the subset of the referrals who did not have any missing data on initial assessment and final utility score, sex and referral age. To retain sample size, we used the missing indicator method for two categorical variables, the index of multiple deprivation quintile and ethnicity [22]. We investigated the representativeness of the analysis sample by comparing the descriptive statistics of those referrals included in the regression to all referrals made prior to 1 April 2019.
We then used these coefficients to calculate the total utility benefit associated with the levels of session attendance for all referrals received by 31 March 2019, calculated using the regression coefficient multiplied by the number of sessions the individual attended. Here we assumed that individuals who did not attend any of the programme sessions experienced zero utility benefit.
We estimated the change in QALYs using the estimated utility change multiplied by the time elapsed between the date of initial assessment and the date of the final session attended, multiplied by 0.5. This is referred to as the ‘average’ area under the curve method and assumes that the utility score changes linearly between time points [23].
For the small number of referrals that were missing an initial assessment date (0.2%), we instead calculated the length of time that had elapsed between the last session attended and the date the referral was received, minus the average length between referral and initial assessment in the full sample of referrals where this information was available.
We then summed these QALY gains across all referrals to generate an estimate of the total number of QALYs generated for the programme overall. We estimated the uncertainty surrounding the utility gains from session attendance by using the upper and lower bounds of the 95% confidence intervals of the regression coefficients.
2.3.4 Secondary Analysis – Benefits from Session Attendance and Weight Change
We repeated the above OLS regression analysis, additionally including participant weight change between the initial assessment and the final session amongst those referrals with this information recorded.
To apply the estimated coefficients to all referrals, we used multiple imputation using chained equations with 30 iterations to impute missing weight change amongst individuals who attended at least one programme session [24]. In the imputation model, we also included the covariates used in the regressions: sex, referral age group, index of multiple deprivation and ethnicity, along with the initial assessment utility score and final utility score. Individuals not attending any programme sessions were again assumed to experience zero utility benefit.
We applied the regression coefficients for number of sessions attended and weight change to the 30 imputed datasets to estimate utility benefit, and then from this calculated the total QALY gain using the time that has elapsed between the date of their initial assessment and the date of the final session that they attended. In doing so, we generated 30 estimates of the total QALY gains due to programme participation, from which we computed an average and standard deviation.
We present the percentage of missingness for each variable included in the regression analysis in Supplementary Material Table 1. We did this for all referrals and then again for referrals that attended at least one programme session. Alongside this table is a description of the potential reason for missingness of the weight change variable, that is, whether the individual did not attend the session for the information to be recorded, or whether they attended the session but the provider did not record it.
2.3.5 Comparing Costs and Benefits
We then compared the total costs of delivering the programme with the estimated total benefits associated with programme participation to determine the cost-per-QALY generated during the programme participation period. We did this both including and excluding the implementation costs from the total cost calculation, as there was uncertainty surrounding how these implementation costs were used and their true amount. We then compare these to the standard threshold of £20,000–30,000 per QALY used in the UK when assessing whether new interventions are cost-effective [25]. The comparator in this analysis was usual care, i.e., the absence of a national diabetes prevention programme.
All analyses were conducted in Stata 16 [26]. The methods and results are reported according to the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) [27] with the completed checklist available in Supplementary Material Table 4.
3 Results
NHS DPP providers received a total of 384,611 referrals during our analysis period, from the start of the programme on 1 June 2016 to 31 March 2019. Of these, 201,686 (52.4%) went on to attend an initial assessment, and 74,306 (19.3%) completed the programme according to the NHS England definition of attending at least 60% of sessions (as shown in Supplementary Material Fig. 1). Table 2 shows the characteristics of these referrals. Individuals referred to the programme were on average 62.4 years of age [standard deviation (sd): 13.5]. Over 20% were from the most deprived index of multiple deprivation quintile (21.4%). Of those who attended the initial assessment (where ethnicity was recorded), the majority were white (70.0%).
Across all referrals, individuals attended 3.0 sessions (sd: 4.6) on average. This increased to 5.6 sessions (sd: 5.1) when considering only individuals who attended the initial assessment. Where recorded (43,184 out of the 66,464 referrals who attended the final programme session), individuals lost on average 3.3 kg (sd: 4.7 kg) between their initial assessment and final session of the programme.
3.1 Participant Retention
Table 3 shows the retention rates of these referrals according to the NHS DPP payment milestones. On average, 13.2% of referrals met milestone 5 of the programme. The milestone 5 retention rate is lower than the completion rate (19.3%), as it is possible for an individual to complete 60% of programme sessions overall without meeting the requirements for milestone 5 (for example, by attending the first 8 sessions of a 13-session programme).
3.2 Total Costs – Referrals
The total cost of all referrals received by the NHS DPP based on their level of attendance was £44,185,940. The average cost per referral received (weighted by provider) was £118.98 (sd: £117.54), compared with an average cost of £285.67 (sd: £63.45) per referral that completed at least 60% of programme sessions.
Total implementation costs up to 1 April 2019 were estimated to be £8,765,158 (in 2020 prices), equivalent to an additional cost of £22.79 per referral. The annual implementation costs estimated from the 2016 impact assessment, inflated to 2020 prices, are shown in Supplementary Material Table 2.
Therefore, when we included implementation costs in our estimates, the total cost of the programme for referrals received prior to 1 April 2019 was £52,951,098.
3.3 Baseline Health-Related Quality of Life
Baseline EQ-5D-5L scores were available in 116,004 (30.2%) of all referral records, or 57.6% of individuals that attended an initial assessment, where this data was supposed to be collected. A total of 1,710 unique health states were reported, out of the 3,125 possible with the EQ-5D-5L. On average the baseline utility score was 0.808 (sd: 0.216) with a visual analogue score (VAS) of 74 (sd: 19; Table 4). Examining the scores for each domain separately, 66.5% of respondents reported no problems with the domain of mobility, 90.0% for self-care, 75.6% for usual activities, 59.9% for pain/discomfort and 59.1% for anxiety/depression. A total of 35.2% respondents reported no problems in any domain.
3.4 Main Analysis – Benefit from Session Attendance
Results of the OLS regression showed that attending a session of the NHS DPP was associated with an increase in utility of 0.0042 (95% CI: 0.0025–0.0059) per additional session attended for the providers delivering 13 sessions, and 0.0024 (95% CI: −0.0002–0.0051) per additional session attended for the provider with 18 sessions. The full regression output for this analysis can be found in Table 3 of the Supplementary Material.
On average, the time that had elapsed between initial assessment and the final programme session for individuals who attended the 13th or 18th session was 341.2 (sd: 91.8) days.
When these coefficient estimates were applied to all referrals received prior to 1 April 2019, we estimated a total of 1,772.5 QALYs (95% CI: 888.7–2,656.2) were associated with programme attendance.
The descriptive statistics for the sample of referrals included in these regressions are shown alongside the descriptive statistics for all referrals in Tables 2 and 4. As expected, referrals included in the regression sample attended a higher number of sessions on average than those who were not included (12.0 compared with 3.0). A total of 310 individuals attended less than 60% of sessions but recorded an EQ-5D-5L response at both time points. The sample included in the regression had a similar sex composition but were slightly older (66.5 years of age compared with 62.4 years) and from less deprived index of multiple deprivation quintiles – reflective of the characteristics of completers of the programme.
3.5 Secondary Analysis – Benefit from Session Attendance and Weight Change
When weight change was included as a covariate, attending a session of the NHS DPP was associated with an increase in utility of 0.0034 (95% CI: 0.0016–0.0051), and each kilogram lost was associated with an increase in utility of 0.0025 (95% CI: 0.0020–0.0031). For the provider delivering 18 sessions, we saw similar coefficients: a 0.0005 increase in utility for each session attended (95% CI: −0.002–0.0031) and 0.0028 for each kilogram lost (95% CI: 0.0017–0.0040). The regression outputs associated with these covariates are shown in Table 5, and the full regression outputs are shown in Supplementary Material Table 3.
We then used these estimates and applied them to the 30 datasets where weight change for all participants was imputed. We estimated that on average a total of 1,541.7 QALYs were generated (95% CI: 1,530.5–1,552.9).
3.6 Comparing Costs and Benefits
We present the cost-per-QALY for the main and secondary analyses in Table 6, using the total programme costs, with and without implementation costs.
If only the benefits associated with session attendance were considered, we found that the cost-per-QALY was £24,929 (95% CI: £16,635–49,720) excluding implementation costs and £29,874 (95% CI: £19,935–59,583) when implementation costs were included.
When we also considered the benefits associated with losing weight using the imputed weight change datasets, we found that this estimate increased slightly to £28,661 per QALY (95% CI: £28,454–28,870) when implementation costs were excluded and £34,346 per QALY (95% CI: £34,098–34,597) when implementation costs were included.
4 Discussion
4.1 Main Findings
We examined a nationwide diabetes prevention programme to see whether investment in such programmes can offer value for money to commissioners based only on the benefits observed during the short-term of programme participation. We examined 384,611 referrals made to the programme prior to 1 April 2019, and calculated the total cost of delivery as £44,185,940 in addition to an estimated £8,765,158 in programme implementation costs.
We found that participating in programme sessions was associated with an increase in utility, as was losing weight. We carried out two analyses, the first looking at benefit only in terms of session attendance and the second looking at number of sessions attended, along with weight change, where missing information on weight change was imputed. Our main analysis, which considered only session attendance, suggested there was a small increase in utility per additional session attended. Whilst the individual-level utility increase may be relatively small, due to the large number of referrals received by the NHS DPP, this was associated with a total of 1,772.5 (95% CI: 888.7–2,656.2) QALYs generated. In the secondary analysis, where missing weight change was imputed, we estimated a total of 1,541.7 (95% CI: 1,530.5–1,552.9) QALYs may have been generated. This estimate is lower than the estimate of total QALYs when considering only session attendance, as the coefficient on session attendance was reduced and the estimated gains from weight loss were not large enough to offset this.
Using the total costs and benefits estimated, we estimated the short-term cost-effectiveness of the programme in terms of cost-per-QALY generated. These are considered short-term, as we only capture the within-programme benefits and have not evaluated the potential longer-term benefits (for example participants may continue to lose weight) nor those associated with diabetes prevention. In contrast, we captured all the costs of delivering the programme which, as with many prevention programmes, are incurred up front. As such, it is likely that the cost-per-QALY of the programme over the longer-term may be lower than the estimates presented here suggest.
With this being said, we estimated the cost-per-QALY generated to be £24,929 excluding implementation costs and £29,874 when implementation costs were included, with both point estimates falling within the currently accepted willingness-to-pay threshold used by NICE of £20,000–30,000 per QALY [25]. In our secondary analysis, this estimated cost-per-QALY generated was slightly higher at £28,661 when implementation costs were excluded and £34,346 when implementation costs were included. Whilst the estimated cost-per-QALY falls within the currently accepted cost-effectiveness threshold in three out of the four scenarios we examine, there is a degree of uncertainty surrounding these estimates. We examined this uncertainty using the upper and lower bounds of the 95% confidence intervals of the regression coefficients, and our results should be interpreted with this uncertainty in mind.
Prior to introducing the NHS DPP, an impact assessment was conducted [28]. This estimated that in the first 5 years of the programme, 390,000 individuals would have participated at a cost of £105 million, with implementation and support costs estimated as £10.95 million [16]. We can compare our estimates of cost and benefit with those estimated in this impact assessment. Looking amongst those who attended at least one programme session (which is how retention was presented in the impact assessment), we find that the observed retention at milestone 5 was actually higher in reality than originally predicted in the impact assessment (34.7% compared with 20%). However, this retention rate does not capture the loss of individuals from referral to initial assessment attendance, where we observed approximately half of referrals (47.4%) failed to meet this first attendance milestone, estimates for retention from referral to initial assessment were not presented in the impact assessment.
This impact assessment estimated an average cost of £270 per participant referred to the programme. Our analysis found that the average cost per referral was in fact £118.98 (sd: 117.54; weighted by provider, 2020 price year). The low levels of retention from referral to initial assessment which we observe may explain why costs per referral were lower than originally predicted, as providers on ‘activity only’ contracts did not start receiving payments until referred individuals attended at least the initial assessment. The impact assessment also estimated that there would be 700-1,000 QALYs generated within the first 5 years of the programme; however, our analyses suggest an additional 1,541.7–1,772.5 QALYs within the first 3 years by taking into account within-programme benefits alone.
4.2 Other Studies
We can also compare the cost-effectiveness of the NHS DPP with estimates of other diabetes prevention programmes, such as the US DPP and the Norfolk Diabetes Prevention Study.
The US DPP enrolled 3,234 participants to three intervention arms: placebo, metformin and a lifestyle intervention. The lifestyle intervention included 16 core sessions, followed by monthly follow-up. The within-trial cost-effectiveness analysis which looked at a time horizon of 3 years found that the lifestyle intervention relative to the placebo had an incremental cost-effectiveness ratio (ICER) of $31,500 (2000 price year) [29]. This is equivalent to £32,251 per QALY generated when converted to £ sterling and inflated to 2020 price year (converted and inflated using [30]).
The Norfolk Diabetes Prevention Study randomised 1,028 participants (from 141,973 people invited, and 12,778 screened) to three arms: a control arm receiving usual care, a lifestyle intervention arm of 6 core and up to 15 maintenance sessions, and the same intervention with the addition of support from trained volunteer mentors who had type 2 diabetes. This study found that on average the intervention cost £122 for the lifestyle intervention or £241 for the lifestyle plus mentor arm amongst those who attended at least 1 session (using 2016–2017 prices, equivalent to: £131.98 and £260.72 for 2020 price year) [31]. These are comparable to the cost per referral found in our analysis of £118.98, and cost per completer of £285.67.
4.3 Strengths and Limitations
This is the first analysis to consider the costs and within-programme effects of the NHS DPP in terms of QALYs. We used real-world data collected from providers, and considered just under 400,000 referrals to the programme. This is a far greater number than existing studies in the literature, which look at lifestyle interventions amongst highly selected participants. We also had access to information on provider payment rates, which allowed us to calculate the total cost of delivering this nationwide diabetes prevention programme.
There are also several limitations associated with our analysis. On the cost side, we only included costs directly incurred for programme delivery by the NHS. The wider impacts on individuals’ healthcare resource use were not included because we could not link individual-level data from the programme providers to primary or secondary care health records. Additionally, the payments made to providers may differ from the costs of delivery from the provider perspective. There was also uncertainty surrounding the implementation costs involved in establishing the programme, as NHS England were not able specify this amount. We therefore used an inflated estimate from the original 2016 impact assessment. To address this uncertainty, we conducted the analyses both with and without these costs included. Furthermore, whilst we used provider reimbursement contracts to calculate the exact cost to the NHS of the referrals received, there were some instances where we had to make assumptions about the unit costs due to discrepancies in the contract data provided (7% of referrals). There is therefore some uncertainty in the estimated programme costs which we have not accounted for in a formal uncertainty analysis.
In terms of measuring the benefits associated with the programme, the nature of the real-world data collection resulted in large amounts of missingness. Only individuals who attended the initial assessment had their initial EQ-5D-5L collected, and this was only collected again for individuals who attended the final planned programme session. In some instances, there was also the issue of providers not collecting data, even if participants attended the session. This meant that we were only able to include a fraction of all referrals within our main regression analysis (18,959 out of 384,611 referrals, 4.9%). To overcome this we applied the coefficients estimated from the regression analyses to the sample of all referrals, which enabled us to estimate the benefits associated with programme attendance for individuals even if their initial or final utility score was not collected.
Estimating the benefits associated with each programme session attended as we have done could potentially misestimate the benefits for those who attended fewer sessions, as there were only a small number of individuals within our regression sample that had not attended at least 60% of programme sessions (n = 309, 1.6%). It also means that in our analysis we compared with individuals who were referred but did not attend any programme sessions beyond the initial assessment. This effectively assumes that individuals gain no utility benefit from the programme unless they attended at least one session. We took this approach due to the timing of the EQ-5D-5L data collection, which did not begin until initial assessment. However, it may be that individuals do receive some benefit from the initial assessment, or from merely being referred to the programme, which we were unable to capture. If this is the case, then our estimates would represent the lower bound of the utility gains associated with the programme over the short-term.
Lastly, whilst we controlled for socio-demographic factors in our regression analyses, these analyses did not directly consider the distribution of effects across different individuals (equity) and instead focused on the benefit associated with number of sessions attended and units of weight change (efficiency). Indeed, other research of the NHS DPP has shown that there are socio-demographic differences in those who are referred to the programme and those who go on to complete it [5, 32]. It found that individuals who engaged in the programme were older, more likely to be from the least deprived socioeconomic quintile and were more likely to be white compared with those referred. These differences are also seen in terms of outcomes of the programme, with individuals from minority ethnic groups being found to lose less weight than white participants after 6 months of participating in the programme, although the reductions in blood glucose levels (HbA1c) were similar across patient subgroups [5]. This may have important equity considerations, but is beyond the scope of the current analysis which followed the recommendations set out in the NICE Reference Case, stating that “an additional QALY should receive the same weight regardless of any other characteristics of the people receiving the health benefit" [17]. Such distributional issues could be explored in future research.
5 Conclusion
We estimated the costs and short-term benefits associated with the NHS DPP. Our analysis suggests that the NHS DPP may be considered cost-effective even in the short-term, when only benefits measured during programme participation were considered. This provides support for the recommissioning of such services and to protect public health budgets responsible for commissioning such prevention programmes, given they may still be cost-effective when considering only short-term benefit but all costs.
Data Availability
Provider data on referrals to the programme (the minimum dataset) were provided by NHS England via a data sharing agreement. The authors are not permitted to share this data. Data on the costs of the programme are considered commercially sensitive, and the authors are not permitted to share this data. The wider project protocol is available from: https://fundingawards.nihr.ac.uk/award/16/48/07, and ethical approval was received from the North West – Greater Manchester East Research Ethics Committee (REC reference 17/NW/0426). The DIPLOMA research project was developed in collaboration with a public and patient involvement group.
Code Availability
The Stata code used for the analysis described in this manuscript is available from the corresponding author upon reasonable request.
References
Everest G et al. Addressing the leading risk factors for ill health. The Health Foundation. Accessed, 2022. 1.
McDaid D. Using economic evidence to help make the case for investing in health promotion and disease prevention. In: Kluge H, Figueras J, editors. Policy briefs. Copenhagen: WHO Regional Office for Europe; 2018.
Barry E, et al. Explaining the UK’s ‘high-risk’ approach to type 2 diabetes prevention: findings from a qualitative interview study with policy-makers in England. BMJ Open. 2023;13(2): e066301.
Fletcher B, Gulanick M, Lamendola C. Risk factors for type 2 diabetes mellitus. J Cardiovasc Nurs. 2002;16(2):17–23.
Marsden AM, et al. ‘Finishing the race’–a cohort study of weight and blood glucose change among the first 36,000 patients in a large-scale diabetes prevention programme. Int J Behav Nutr Phys Act. 2022;19(1):1–10.
Valabhji J, et al. Early outcomes from the English National Health Service Diabetes Prevention Programme. Diabetes Care. 2020;43(1):152–60.
Ravindrarajah R, et al. Referral to the NHS Diabetes Prevention Programme and conversion from nondiabetic hyperglycaemia to type 2 diabetes mellitus in England: a matched cohort analysis. PLoS Med. 2023;20(2): e1004177.
McManus E, et al. Population level impact of the NHS Diabetes Prevention Programme on incidence of type 2 diabetes in England: an observational study. Lancet Regional Health Europe. 2022;19: 100420.
Hawkes RE, et al. The NHS Diabetes Prevention Programme: an observational study of service delivery and patient experience. BMC Health Serv Res. 2020;20(1):1–12.
NHS England. NHS Diabetes Prevention Programme National Service Specification (2016). 2016. Available from: https://www.england.nhs.uk/publication/nhs-dpp-national-service-specification/.
Bansal N. Prediabetes diagnosis and treatment: a review. World J Diabetes. 2015;6(2):296.
NHS England. Diabetes prevention programme information governance and data flows. 2016. Available from: https://www.england.nhs.uk/wp-content/uploads/2019/09/diabetes-prevention-programme-information-governance-and-data-flows-framework.pdf.
EuroQol. About EQ-5D. 2023; Available from: https://euroqol.org/eq-5d-instruments/.
McManus E, et al. The effects of structure, process and outcome incentives on primary care referrals to a national prevention programme. Health Econ. 2021;30(6):1393–416.
Stokes J, et al. Implementing a national diabetes prevention programme in England: lessons learned. BMC Health Serv Res. 2019;19(1):1–12.
NHS England. NHS England Impact Analysis of implementing NHS Diabetes Prevention Programme, 2016 to 2021. 2016; Available from: https://www.england.nhs.uk/wp-content/uploads/2016/08/impact-assessment-ndpp.pdf.
National Institute for Health and Care Excellence. Position statement on use of the EQ-5D-5L value set for England (updated October 2019). 2019; Available from: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l.
Office for National Statistics. CPI Annual Rate 00: All items 2015=100. 2022; Available from: https://www.ons.gov.uk/economy/inflationandpriceindices/timeseries/d7g7/mm23.
Van Hout B, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–15.
Kontopantelis E, et al. Geographical epidemiology of health and overall deprivation in England, its changes and persistence from 2004 to 2015: a longitudinal spatial population study. J Epidemiol Community Health. 2018;72(2):140–7.
Wu M, et al. Examining the impact of 11 long-standing health conditions on health-related quality of life using the EQ-5D in a general population sample. Eur J Health Econ. 2015;16:141–51.
Groenwold RH, et al. Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. Can Med Assoc J. 2012;184(11):1265–9.
Ganiats T, Browner D, Kaplan R. Comparison of two methods of calculating quality-adjusted life years. Qual Life Res. 1996;5(1):162–4.
Azur MJ, et al. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–9.
National Institute for Health and Care Excellence. Guide to the methods of technology appraisal. 2013; Available from: https://www.nice.org.uk/process/pmg9/chapter/the-reference-case.
StataCorp. Stata statistical software: release 16. College Station: StataCorp LLC; 2019.
Husereau D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25(1):10–31.
Shah K, et al. Is the aim of the English health care system to maximize QALYs? J Health Serv Res Policy. 2012;17(3):157–63.
Diabetes Prevention Program Research Group. Within-trial cost-effectiveness of lifestyle intervention or metformin for the primary prevention of type 2 diabetes. Diabetes Care. 2003;26(9):2518–23.
Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evidence Policy. 2010;6(1):51–9.
Sampson M, et al. Lifestyle intervention with or without lay volunteers to prevent type 2 diabetes in people with impaired fasting glucose and/or nondiabetic hyperglycemia: a randomized clinical trial. JAMA Intern Med. 2021;181(2):168–78.
Chatzi G, et al. Could diabetes prevention programmes result in the widening of sociodemographic inequalities in type 2 diabetes? Comparison of survey and administrative data for England. J Epidemiol Community Health. 2023. https://doi.org/10.1136/jech-2022-219654.
Funding
The authors of this manuscript were funded by the National Institute for Health and Care Research [The Health and Social Care Delivery Research (HSDR) Programme, 16/48/07 – Evaluating the NHS Diabetes Prevention Programme (NHS DPP): the DIPLOMA research programme (Diabetes Prevention – Long Term Multimethod Assessment)]. The views and opinions are those of the authors and do not necessarily reflect those of the National Institute for Health and Care Research or the Department of Health and Social Care. The authors declare no other sources of funding relating to this work.
Author information
Authors and Affiliations
Contributions
MS, EM and RM conceived the idea for the paper. EM acquired the datasets for analysis. EM and MS undertook the analysis. EM took the lead in writing the manuscript. All authors were involved in editing the manuscript. All authors have had full access to and verify the underlying study data. They accept responsibility to submit for publication.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors report no conflicts of interest.
Ethical Approval
Ethical approval was received for the wider DIPLOMA project from the North West – Greater Manchester East Research Ethics Committee (REC reference 17/NW/0426).
Consent to Participate
Not applicable.
Consent for Publication (from Patients/Participants)
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McManus, E., Meacock, R., Parkinson, B. et al. Evaluating the Short-Term Costs and Benefits of a Nationwide Diabetes Prevention Programme in England: Retrospective Observational Study. Appl Health Econ Health Policy 21, 891–903 (2023). https://doi.org/10.1007/s40258-023-00830-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00830-8