Abstract
Aim
To estimate the potential cost of lost labour productivity due to cancer-related premature mortality in Europe (EU-27 plus Norway, Switzerland, Iceland and United Kingdom) from 2018 to 2040.
Methods
Deaths and years of potential productive life lost due to 23 types of cancer were estimated for 2018–2040, for 31 European countries. The data were analysed by age groups, by sex and by year. Projected productivity costs were estimated by calculating gross earnings by country, gender and age group using the Human Capital Approach, adjusting for projected labour force participation and unemployment rates. Various data sources were used. Sensitivity analyses were conducted.
Results
Between 2018 and 2040, cancer is expected to cause around eight million premature deaths (58% male). The cumulative projected productivity costs in this respect are €1.3 trillion, representing an annual average of €58.7 billion, or 0.43% of the EU-27 gross domestic product. Labour productivity costs are projected to decrease by 6% from 2018 to 2040. The highest cost region is Western Europe, where Germany and France will experience the highest cumulative losses (€288 and €192 billion, respectively). The most costly cancers, in terms of total costs related to productivity losses, are of the lung and colorectum (€264.4 and €116.3 billion, respectively). In terms of average productivity cost per death, the most costly forms of cancer are Hodgkin lymphoma (€301,157) and melanoma (€260,522).
Conclusion
The novel information presented could help national policymakers anticipate possible areas for cost savings. Action should be taken on disease prevention, on reducing mortality and on delaying the age of death due to Hodgkin lymphoma, brain cancer, leukaemia and melanoma. Furthermore, the study findings enhance our understanding of macroeconomic variables and could be useful in determining a re-allocation of health expenditures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Western Europe emerges as the highest cost region accounting for 50% of all estimated productivity costs over the study period but only 36% of European deaths. However, Northern Europe is the area where the cost per cancer death is highest. |
Lung and colorectal cancer will account for the highest number of cumulative deaths during the period 2018–2040 and the largest cost. However, the most costly cancers will be Hodgkin lymphoma, melanoma, brain cancer and leukaemia. |
The economic performance indicators and the value of human capital that would be perceived as a success from a purely economic viewpoint can elevate the actual cost of a disease from a broader societal perspective, thereby further highlighting the policy need for investment in improved cancer control strategies in the future. |
1 Introduction
Cancer is the second leading cause of mortality worldwide, causing nearly 10 million deaths in 2020 (almost 1 in 6 of all deaths, or 127.8 persons per 100,000 population). Four million of these deaths corresponded to people of productive age [1].
Since 2017, the World Health Assembly has classified the reduction of premature mortality due to cancer as an urgent target in its Global Action Plan for the Prevention and Control of Noncommunicable Diseases [2]. Nevertheless, the International Agency for Research on Cancer (IARC) has estimated that cancer deaths will increase by 62% by 2040 globally and by 30% in Europe, specifically [3]. In contrast, deaths of persons of working age (15–64 years) are expected to decrease by 4% in Europe (from 527,000 in 2020 to 506,000 by 2040) [3].
Premature mortality represents both a human and a capital loss to society. The latter has been termed “productivity loss” and provides additional information on the total economic burden caused by disease. Productivity losses are an important part of the economic consequences of illness, hence the importance of quantifying their impact.
Various studies have estimated the productivity costs of cancer-related premature mortality in Europe, for all cancers [4,5,6,7,8]. The most recent investigations reported that the total value of lost productivity for premature mortality due to cancer, across 31 European countries, was €54 billion with respect to paid work [9] and €104.6 billion when both paid and unpaid work were considered [10]. All of these studies, except Jönsson et al. [6], estimated productivity costs in a single past year. However, estimating productivity costs for a future period would provide health policy makers with valuable additional information. Specifically, productivity cost projections give information in the short, medium and long term on the potential economic cost to society of premature mortality and disabilities, which could be avoided by effective investment in the prevention, early detection and treatment of cancer. Therefore, productivity cost projections can be used to inform decision making on investment in specific cancer control strategies.
Nevertheless, few projection-based studies have been made of the costs of lost productivity due to cancer. As far as we are aware, only two previous studies have estimated the projected losses of premature mortality due to cancer in European countries—one took place in Ireland [11] and the other in Russia [12]. No long-term projections have been made for Europe as a whole.
In view of these considerations, the aim of this study is to estimate the projected costs of productivity losses due to cancer-related premature mortality for all cancers, both combined and for 23 individual types of cancer, for the 27 European Union countries plus Norway, Switzerland, Iceland and the United Kingdom (UK) from 2018 to 2040, using a standardised methodology which ensures cross-country comparability.
2 Methodology
2.1 Mortality Projections
To measure the loss of labour productivity due to cancer-related premature mortality (henceforth, productivity) we define the productive working age in European countries as 15–64 years, with the lower limit in line with previous studies [5, 7, 10], and taking the average statutory age of retirement in Europe (65 years). Therefore, any person between 15 and 64 years old who was working and died before 65 due to cancer is assumed to generate a productivity loss for society.
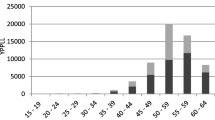
We obtained the number of premature deaths due to cancer in 2018, both for all cancers combined and for individual types of cancer, analysing the data by sex, productive age group (15–29, 30–39, 40–49, 50–59, 60–64) and European country, according to data published by the Global Cancer Observatory [1]. Twenty-three types of cancer were considered, as listed in the International Classification of Diseases, 10th revision (ICD-10). Our results are estimated for Europe as a whole (the 27 EU countries, plus Norway, Switzerland, Iceland and the UK) and were also classified into four European regions (Northern, Southern, Central-Eastern and Western Europe).
Premature cancer deaths by sex, age group and country were projected for each year from 2019 to 2040. To do so, we first took the annual projected population size from 2019 to 2040, as published by Eurostat, to calculate the rate of population growth by sex, age group and country, to determine the variation (+/−) in numbers of inhabitants per year [13]. We then projected the values for deaths, for every year from 2019 to 2040, multiplying the number of cancer deaths in 2018 (by sex, age group, country and type of cancer) by each year’s projected rate of population growth (by sex, age group and country).
Finally, a value representing years of potential productive life lost (YPPLL) was calculated, using WHO Standard Life Tables [14], as the years of life lost between the midpoint of each age group at death and at 64 years old. This value reflects the years of potential paid production that would be lost due to premature death from cancer.
2.2 Projected Earnings, Labour Force Participation and Unemployment
Following the Human Capital Approach, we use annual gross earnings projections to estimate the productivity lost due to projected cancer deaths [15]. To project the annual gross earnings for each year from 2019 to 2040, we used the annual gross earnings (nominal value, for both part and full-time jobs) for 2018 by sex, age group (15–29, 30–39…, 60–64 years) and country. We then estimated the average annual earnings growth by sex, age group and country between each of the last three waves obtained by the Eurostat Structure of Earnings Survey for 2006, 2010 and 2014 (Supplementary Table 1a and 1b) [16]. Annual earnings in the last available wave (2014) were inflated to 2018 values using the average Harmonized Index of Consumer Prices between 2008–2018 [17] and assuming a constant growth rate for each year from 2019 to 2040 (i.e. average growth rates did not change along the study period). Finally, projected earnings for each year from 2019 to 2040 were calculated by multiplying the annual earnings by average annual earnings growth [e.g., (wage 2018* (1 + growth)), (wage 2019*(1 + growth), …].
Subsequently, each projected annual earnings figure from 2019 to 2040 was adjusted to each country’s economic conditions using country-specific average labour force participation rates [18] and average unemployment rates [19] for the last 5 years (2014–2018), disaggregated by sex and age group (Supplementary Table 1a and 1b). As labour force participation rate and unemployment rate age bands are both published in five-year bands (15–19, 20–24, …, 60–64 years old), we aggregated them by calculating the average to obtain standardised annual earnings bands (15–29, 30–39…, 60–64 years). The conservative assumption was made that unemployment and labour force participation rates would remain constant over the projected timeframe (as in the case of the annual earnings growth rates). In other words, we assumed that the future economic circumstances for each country would be similar to those of previous years (2014–2018).
2.3 Projected Loss of Labour Productivity
The (incidence-based) Human Capital Approach [15] was applied to estimate labour productivity losses due to premature mortality from cancer between 2018 and 2040. In this regard, the losses arising from each cancer death were valued by multiplying YPPLL by the sex-, age group-specific and projected earnings (adjusted for labour force participation and unemployment rates) per year (from 2018 to 2040) for each country. The total projected premature mortality productivity cost was calculated as the sum of the annual projected premature productivity costs over the 22 years for each individual. These individual-level costs were then summed by age band, sex, types of cancer, country and region.
Our baseline assumption is that from 2008 to 2018 earnings increased at the average rate of GDP growth for each European country [20]. Future productivity costs were discounted at 3.5% per annum to make our results comparable with previously published estimates for European countries [4, 5, 10, 11].
Three sensitivity analyses were then conducted to compare the values for 2018 with those for 2040. First, we applied the maximum and minimum country-specific GDP growth from 2000 to 2018; then, we assumed an extension of the current average retirement age throughout Europe to 67 years, in line with existing policy developments linked to increasing life expectancy and the prolongation of working lives [21]; finally, we assumed an annual reduction in cancer mortality rates of −1% over the time period for every form of cancer, based on the cancer mortality rates reported by Bertuccio et al., for 2007–2017 in the EU [22] and the estimations of the number of deaths, both male and female, among those aged 15–64 years in the 31 countries considered, according to IARC data [3]. All costs are expressed in 2018 euros. All data management procedures and analyses were conducted using Excel and Stata 13.0 statistical software (StataCorp LP, College Station, TX).
3 Results
3.1 Projected Mortality and Labour Productivity Costs by Region And Country
From 2018 to 2040, there are predicted to be about eight million premature deaths from cancer-related causes in Europe among persons aged 15–64 years (Table 1). Of these, 36.0% (2.9 million) will take place in Western Europe and 24.7% (1.9 million) in Southern Europe. While some countries (Iceland, The Netherlands, Ireland and Denmark) will experience similar proportions of male and female cancer-related deaths, in Portugal and Romania men will be more than twice as likely as women to die from this cause. Overall, men will account for 57.5% (4.6 million) of these deaths.
As shown in Table 1, the total estimated productivity losses from these premature deaths will be €1.3 trillion (of which 64% corresponds to male deaths). Western Europe is projected to account for half of all productivity costs in this respect in Europe (€647 billion). By countries, the highest total productivity cost will be experienced in Germany (€288 billion), France (€192 billion) and the UK (€179 billion), while the lowest will be experienced by Estonia (€1.66 billion), Iceland (€1.03 billion) and Malta (€595 million), these differences largely reflecting the respective population sizes in 2018. While Estonia was the fifth smallest country in Europe in 2018 by population size, behind Iceland, Malta, Luxembourg and Cyprus, the population in the latter two countries is expected to increase during the study period, which raises the expected productivity cost burden and ranking.
In the study period, the average productivity cost per cancer death across Europe is estimated to be €161,455 (€179,617 for males and €136,855 for females). By countries, the highest level of productivity cost per death will be experienced in Switzerland, and the lowest, in Bulgaria (€449,872 and €33,074 average productivity cost per death, respectively). By region, Northern Europe has the highest productivity cost per death (€229,205), with Norway (€411,999), Denmark (€309,118), Sweden (€295,932) and Iceland (€295,144) ranking highest in this region according to economic drivers such as higher gross earnings, lower average unemployment rates and higher rates of labour force participation (see Supplementary Table 1b). By contrast, Central-Eastern Europe has the lowest average productivity cost per cancer-related death, at €50,839, less than a quarter of the Northern Europe figure, with countries such as Romania (€37,912) and Bulgaria (€33,074).
Table 2 shows the changes in premature deaths and productivity costs from 2018 (data shown in Supplementary Table 2) to 2040. In summary, these results reflect a 4% decrease in total invasive cancer deaths among adults in Europe in 2040 versus 2018, taking into account population change in Europe; specifically, female deaths will fall by 6%, and male deaths by 2%. In the 31 European countries, productivity costs are projected to fall by 6% by 2040. By regions, Southern and Western Europe are predicted to experience 5% and 10% reductions in annual premature cancer-related deaths, respectively, between 2018 and 2040, generating overall annual productivity cost reductions of 17% and 9%. In contrast, these deaths will increase in Central-Eastern and Northern Europe, by 1% and 5%, respectively, although only Northern Europe will face increased productivity costs (7%), mainly due to the rising population and, therefore, the number of deaths.
3.2 Projected Labour Productivity Costs by Types of Cancer
By types of cancer (Table 3), lung and colorectal cancer are expected to produce the highest numbers of cumulative deaths during the period 2018–2040 (2.0 million and 753,000 deaths, respectively). The highest productivity costs will be caused by lung cancer (€264.4 billion) and colorectal cancer (€116.3 billion), followed by breast cancer (€113.0 billion) and brain cancer (€96.2 billion). In terms of productivity cost per premature death, the most costly forms of cancer between 2018–2040 will be Hodgkin lymphoma (€301,157), melanoma skin (€260,522), brain cancer (€249,267) and leukaemia (€213,452), due to their relatively young age of onset and age of death, and so greater time to accumulate lost production. By contrast, cancer of the larynx (€117,238), prostate (€107,085) and corpus uteri (€86,191) will generate the lowest productivity cost burdens. For cancers of the larynx, oesophagus, head and neck, the numbers of deaths and the total costs differ greatly between the sexes. Thus, cumulative deaths associated with larynx cancer will be 7.7 times greater among men than women, and 10.1 times more costly. For oesophagus cancer, the corresponding figures are 5.1 times for deaths and 7.5 times for productivity costs, and for cancers of the head and neck, 4.6 times for deaths and 6.4 times for productivity costs.
Table 4 shows the expected variations in total productivity costs between 2018 and 2040 by age group for the five costliest cancers in Europe (full data shown in Supplementary Table 3). Total productivity cost is predicted to decrease for persons aged 30–39, 40–49 and 50–59 years and to remain the same for those aged under 30 years due to a decrease in the number of deaths during the period considered (data not shown). However, for the oldest cohort (those aged 60–64 years), total average productivity costs for these five cancer types will rise by 3.3% due to the increase in the number of deaths (+4%) related to future population growth in this age group.
3.3 Sensitivity Analyses
Sensitivity analyses show that assuming the minimum economic growth for all European countries, total productivity costs will be 25% lower in 2040 than in 2018, while under the maximum economic growth assumption, total productivity costs will increase by 14% (Table 5), driven mainly by Northern Europe (+57%) and Central-Eastern Europe (+47%). A hypothetical increase in the retirement age to 67 years would raise total productivity costs by 9% in 2040 in comparison with 2018. An annual reduction of 1% in cancer-related annual mortality would reduce total productivity costs by an average of 25% by 2040. Under the scenario of a higher retirement age of 67 years combined with a 1% reduction in annual mortality by 2040, total productivity costs would fall by 12%, with Southern Europe (−20%) and Western Europe (−15%) experiencing significant cost reductions under these assumptions (Table 5).
Applying the same analysis to productivity cost projections for the five costliest types of cancer produces similar results (Table 6). Specifically, a 1% reduction in mortality would have the most significant effect on productivity (−25%). Establishing a retirement age of 67 years would produce more varied effects; thus, productivity costs would increase by 11–12% for colorectal, pancreatic and lung cancers, but only by 4% and 5% for cancers of the breast and brain, respectively.
4 Discussion
This study highlights the significant cost to society in terms of lost labour productivity due to cancer-related premature mortality. This cost has been estimated at a cumulative value of €1.3 trillion for Europe as a whole (the EU-27 plus Norway, Switzerland, Iceland and the UK) during the period 2018–2040, equivalent to €58.7 billion per annum. To put this information in context, this figure represents 0.43% of the EU’s gross domestic product in 2018 (€13,533,330 million) and it is similar to the GDP of Bulgaria and Luxembourg for 2018. From another standpoint, the entire agricultural sector contributes around 1.3% to GDP in Europe each year, or only three times more than the productivity losses attributed to cancer-related premature mortality.
In this paper, we present the geographical distribution of productivity losses considered, estimate the future development of this burden and demonstrate the role played by the interaction between economic and epidemiological factors in generating lost productivity costs. The latter consideration reflects the fact that, for a specific region, a higher number of deaths does not necessarily increase total costs or the cost per death, because these costs depend not only on epidemiological factors, but also on economic ones. For example, gross wages, rates of wage growth, labour force participation and levels of unemployment are all economic drivers that will impact on total costs, irrespective of workforce mortality. As a further, specific example, Western Europe has the highest cancer-related premature mortality productivity costs in the 31 countries considered, representing 50% of total productivity costs for 2018–2040 (€647,128 million). The main reason for this situation is that Western Europe has both the largest population (37.3%) and the largest number of cancer deaths (35.9%) among the four regions specified. In this case, the epidemiological factors have a great influence on the results. On the other hand, in spite of gross wages being the highest in the EU countries, wage growth (6.65%) and unemployment rates are lower than the average for the EU countries and labour force participation (71.64%) is the average (Supplementary Table 1b). As another example, Northern Europe ranked lowest of the four regions for the number of cancer deaths over the period; nevertheless, the productivity cost of each death is the highest in Europe, as a consequence of purely economic variables, including, primarily, elevated levels of gross wage remuneration, but also high rates of labour force participation and relatively low rates of unemployment. These results show that economic performance indicators and the value of human capital that would be perceived as a success from a purely economic viewpoint can elevate the actual productivity cost of a disease from a broader societal perspective. Therefore, to prevent the loss of this human capital through premature deaths, we must improve our strategies for cancer prevention and treatment. This is especially important in the Western world, where the value of human capital will only increase, driven by current and future shortages in the labour market.
The special contribution of the present study is that it is the first to estimate future labour productivity costs arising from the premature mortality caused by 23 types of cancer, in the context of 31 European countries. All previous studies in this field have concerned frameworks that are more restricted, in time and space (USA: 2000–2020 [24], Ireland: 2011–2030 [11] and Russia: 2001–2030 [12]). As a tangible result, our projection shows that cancer productivity costs in Europe will decrease by 6% from 2018 to 2040 (concentrated primarily in Southern Europe (−5%) and Western Europe (−10%). The projected decrease in productivity costs is probably a consequence of various factors, including changes in the labour market, a generally slower population growth and a demographic shift resulting in proportionately more workers being older than the upper bound for working age defined in this study (65 years).
On the other hand, there is some similarity between our findings and those reported in earlier studies, for example in the ranking of productivity costs by cancer type. Thus, we corroborate the previously reported finding that lung cancer is the most costly in terms of lost productivity, followed by colorectal cancer and breast cancer. These forms are particularly significant because they generally present the highest incidence and mortality rates in countries with a high or very high ranking in the human development index [1, 9, 12, 25]. However, a different pattern is observed for productivity costs per cancer death. Our study reveals that Hodgkin lymphoma (€301,157) is the most costly in this respect, followed by melanoma (€260,522), brain cancer (€249,267) and leukaemia (€213,452) due to their relatively young age of onset and age of death, which means that more time elapses in which lost production accumulates. These cancers tend to be under-prioritised in public healthcare policies because of their relatively low incidence and mortality. Nevertheless, our findings suggest that great value could be achieved by focusing public health efforts on the prevention and cure of these “young cancers”, which affect a population sector characterised by its youth and by its foreseeably high level of future productivity for society.
Contrasting results have been reported elsewhere. Thus, a study conducted in the USA found that testicular cancer—which is rare but has a very young age at onset—was the most expensive ($1.3 million), followed by Hodgkin lymphoma ($544,118), brain cancer ($392,853) and cervical cancer ($387,440) [24]. An Irish study also found testicular cancer to be the most expensive (€364,000) [11], while for one conducted in Russia bone cancer was the most expensive [12]. Special mention should be made of brain cancer. In this case, not only is the patient’s young age a significant factor but, moreover, the diagnosis is often delayed. In line with this consideration, all the studies consulted include brain cancer among the three most costly to productivity, highlighting the dramatic impact of a relatively young age of diagnosis combined with a high mortality rate. This finding has significant implications for cancer control strategies and offers an important economic perspective to traditional epidemiological measures of brain cancer.
4.1 Projected Labour Productivity Costs in Individual Countries
Projected productivity costs from 2018 to 2040 differ substantially among European countries. In Europe as a whole, the total number of cancer-related deaths among people of working age is predicted to fall, thus reducing productivity costs. This is true for all regions except Northern Europe, which will experience a slight increase in the number of deaths in 2040, and hence higher total productivity costs. From a country-specific perspective, the economic burden will rise by over 30% in Malta, Cyprus, Iceland and Luxembourg, but it will fall by over 19% in Lithuania, Italy and Greece. These variations are partially due to changes in the numbers of cancer deaths in each country. In Iceland, however, the increase in total productivity costs is mainly due to the rising death rate combined with an increase in wages, extremely high levels of labour force participation and reduced unemployment, throughout the study period. In Greece, the main cause of productivity cost reduction is falling levels of wages together with rising unemployment; and in Italy, the projection is that not only will the amount of cancer-related deaths fall, but also there will be small increases in wages and in the rate of unemployment.
4.2 Projected Productivity Costs and Cancer
Over the next 22 years, lung cancer, colorectal cancer, breast cancer and brain cancer are expected to account for the largest proportion of the economic productivity cost burden in Europe. Among other reasons, this is because these cancers have a very high incidence. In some cases, moreover, behavioural factors such as tobacco or alcohol consumption play an important role. It is estimated that nearly 90% of deaths from lung cancer are caused by smoking cigarettes or by second-hand smoke exposure [26]. Smoking also causes other types of cancers, such as those of the larynx, oesophagus, mouth, liver, pancreas, stomach, kidney, ovary, bladder and cervix, as well as some types of leukaemia [27]. In the European Union in 2019, the proportion of habitual smokers aged 15 years and over was higher among men (22.3%) than among women (4.8%), which partly explains our higher productivity losses ascribed to larynx, oesophagus and head and neck cancer in males than in females. It is especially relevant the case of larynx cancer where deaths are 7.7 times higher in males than females (95,481 versus 12,427) and 10.1 times costlier (€11,500 versus €1140 million). In the second inequality rank, oesophagus cancer deaths are 5.1 times higher in males than females (206,253 versus 40,724) and 7.5 times costlier (€37,700 versus €5030 million). In the third inequality position, head and neck cancer deaths are 4.6 times higher in males than females (302,845 versus 65,371) and 6.4 times costlier (€51,600 versus €8100 million). Our results are in line with other studies [28] and highlight the need to re-educate the society. The comprehensive implementation of tobacco control programmes is of crucial importance in reducing smoking consumption in Europe and in males, and hence reducing cancer-related deaths and costs [29].
In addition to combating cancer through primary prevention measures, medical progress in areas such as screening programmes to obtain an early diagnosis may enable effective therapies to be applied and premature deaths reduced, thus alleviating direct and indirect costs in this respect throughout society. On the other hand, as the average age of death rises, health care costs will inevitably rise in parallel.
4.3 Limitations
The present study is subject to certain limitations, which should be acknowledged. Firstly, there is some uncertainty regarding the economic assumptions made. Our predictions for future economic conditions are based on previous rates of labour force participation and unemployment, and previous gross wages growth. However, these parameters may be stable in some countries and highly unstable elsewhere. To address this possibility, sensitivity analyses were performed, in which the above assumptions were relaxed. The 1% reduction assumed for cancer deaths is based on Bertuccio et al. (2019) and on IARC data [3, 22]. However, this value does not reflect the existence of variations among different types of cancer, among different countries and, very probably, in the sexes and among different age groups. On the other hand, our study aim is to illustrate the impact of falling mortality, not to model it precisely. Furthermore, additional impacts of the coronavirus disease 2019 (COVID-19) pandemic on cancer deaths may emerge in the years to come, because the emergency situation prevented many people from getting regular cancer screening and treatments were delayed, which may result in future increases in cancer deaths [30]. A recent paper calculated the premature deaths and productivity costs associated with the pandemic, and reported a significant excess of deaths and costs during the period in question [31]. We acknowledge the potential impact of the pandemic on our estimates (the consequences of which will remain unknowable for some time and cannot yet form a basis for analysis), but the fundamental long-term trends are complementary.
A second limitation to our paper is that of the uncertainty regarding the number of future deaths. Although this number is inherently unpredictable, we estimated a value for each of the years considered, taking 2018 as the baseline and adjusting it according to total population growth. Sensitivity analyses were then performed to relax this assumption.
A third limitation is that no estimation was made of the “unpaid production” lost. This constitutes another fruitful area for future research, because, as observed above, women’s productivity is undervalued by 73% when only “paid production” is considered [10]. In addition, the same population trends that produce a fall in cancer deaths among the working age population will generate significantly rising numbers of cancer deaths among persons of retirement age, which could have a significant impact on “unpaid productivity” and hence on the wider economy. This question, too, remains to be addressed in future work.
In considering our study results, it is important to take into account that the use of gender-specific economic data for wages, labour force participation and unemployment inevitably introduces an inequality into the calculations. For example, women’s gross wages are lower than men’s, they are more likely to be absent from the workforce and, therefore, their cancers are assigned a lower value. One study has highlighted the need to include “unpaid production” costs in the estimations made, regarding aspects such as household work and caregiving (which are mainly performed by women), because these activities provide an important economic value that is often missing from research studies [10].
Despite the above limitations, our study makes a significant contribution to the literature, as it is the first of its kind to project the productivity cost of the premature mortality caused by 23 types of cancer in the geographic context of 31 European countries. This focus enables us to compare results across time, countries, regions and types of cancer. Our results illustrate the economic burden imposed by cancer in Europe and provide novel, valuable information for policymakers to achieve future cost savings by acting not only on cancer prevention and treatment (for example, by reallocating healthcare expenditure), but also regarding macroeconomic variables. Among their macroeconomic objectives, all developed countries aim to foster employment, increase labour force participation and thus increase the GDP. Success in these areas would benefit the economy and the social sphere. However, lower rates of unemployment, higher gross wages and higher rates of labour force participation also imply greater labour productivity costs. This impacts directly on the opportunity cost of losing a worker prematurely (as is the case of one who dies from cancer). Therefore, policymakers in every country must address these three economic variables, seeking to maximise wages and labour force participation and minimise unemployment; at the same time, they should seek to reduce premature mortality and other undesirable health outcomes.
4.4 Conclusion
Overall, our study reveals an intriguing finding. For the first time in the literature on cancer productivity projection, we identify and discuss a decrease in the productivity costs associated with premature mortality, in a long-term analysis focused on 31 European countries. The causes of this decrease are myriad and interlinked, in which epidemiological factors interact with economic ones and are subject to certain underlying assumptions (which we test through various sensitivity analyses), but the underlying message, when European countries are compared under the same assumptions, is a positive one (countries are reducing cancer deaths and related healthcare costs). Our results provide a novel insight in terms of productivity costs as part of the impact produced on society by cancer, indicating where investment and government priorities may be most appropriately targeted among competing healthcare programmes. Progress can be made in relieving the productivity burden of diseases such as lung, colorectal and breast cancer, but targeted interventions should also be made against high productivity cost cancers such as Hodgkin lymphoma, melanoma and brain cancer. Success in the latter areas—which are not commonly recognised by the epidemiological metrics traditionally used by healthcare policymakers—could pay substantial dividends.
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global cancer observatory: cancer today. International Agency for Research on Cancer. Lyon, France (2020).
World Health Organisation. WHO Discussion Paper on the development of an implementation roadmap 2023-2030 for the WHO Global Action Plan for the Prevention and Control of NCDs 2023-2030. 2021. https://www.who.int/publications/m/item/implementation-roadmap-2023-2030-for-the-who-global-action-plan-for-the-prevention-and-control-of-ncds-2023-2030.
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global cancer observatory: cancer tomorrow. International Agency for Research on Cancer. Lyon, France. 2020. https://gco.iarc.fr/projects.
Hofmarcher T, Lindgren P, Wilking N, Jönsson B. The cost of cancer in Europe 2018. Eur J Cancer. 2020;28:41–9.
Łyszczarz B. Production losses associated with premature mortality in 28 European Union countries. J Global Health. 2019;9: 020418.
Jönsson B, Hofmarcher T, Lindgren P, Wilking N. The cost and burden of cancer in the European Union 1995–2014. Eur J Cancer. 2016;66:162–70.
Hanly P, Soerjomataram I, Sharp L. Measuring the societal burden of cancer: the cost of lost productivity due to premature cancer-related mortality in Europe. Int J Cancer. 2015;136:E136–45.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14:1165–74.
Hanly P, Ortega-Ortega M, Soerjomataram I. Cancer premature mortality costs in Europe in 2020: a comparison of the human capital approach and the friction cost approach. Curr Oncol. 2022;29:3552–64.
Ortega-Ortega M, Hanly P, Pearce A, Soerjomataram I, Sharp L. Paid and unpaid productivity losses due to premature mortality from cancer in Europe in 2018. Int J Cancer. 2022;150:580–93.
Pearce A, Bradley C, Hanly P, O’Neill C, Thomas AA, Molcho M, Sharp L. Projecting productivity losses for cancer-related mortality 2011–2030. BMC Cancer. 2016;16:804.
Barchuk A, Bespalov A, Huhtala H, Chimed T, Belyaev A, Moore M, Anttila A, Auvinen A, Pearce A, Soerjomataram I. Productivity losses associated with premature mortality due to cancer in Russia: a population-wide study covering 2001–2030. Scand J Public Health. 2019;2019:482–91.
Eurostat. Population on 1st January by age, sex and type of projection (proj_18np). 2020. https://ec.europa.eu/eurostat/web/main/data/database. Accessed December 2020.
World Health Organisation. WHO methods and data sources for global burden of disease estimates 2000–2016. 2018. https://www.readkong.com/page/who-methods-and-data-sources-for-global-burden-of-disease-5356763. Accessed June 2022.
Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223–55.
Eurostat. Mean annual earnings by sex, age and occupation. 10 employees or more. 2014. https://ec.europa.eu/eurostat/web/labour-market/earnings/database. Accessed June 2022.
Eurostat. Harmonized Index of Consumer Price- inflation rate. Annual average rate of change. 2019. https://ec.europa.eu/eurostat/databrowser/product/page/TEC00118. Accessed June 2022.
International Labour Organization (ILOSTAT). Labour force participation rate by sex and age. Percentage of total population. 2021. https://ilostat.ilo.org/data/. Accessed June 2022.
Eurostat. Unemployment rates by sex, age and country of birth (%). 2018.https://ec.europa.eu/eurostat/web/lfs/data/database. Accessed June 2022.
Eurostat. GDP and main components (output, expenditure and income). Current prices. 2020. https://ec.europa.eu/eurostat/web/main/data/database. Accessed December 2020.
Hess M, Naegele L, Becker L, Mäcken J, De Tavernier W. Planned retirement timing in Europe: are europeans adapting to the policy of extending working lives. Front Sociol. 2021;6: 691066.
Bertuccio P, Alicandro G, Malvezzi M, Carioli G, Boffetta P, Levi F, La Vecchia C, Negri E. Cancer mortality in Europe in 2015 and an overview of trends since 1990. Ann Oncol. 2019;30:135–69.
International Labour Organization (ILOSTAT). World employment and social outlook: trends 2021. 2021.https://www.iloorg/global/research/global-reports/weso/trends2021/WCMS_795453/lang--en/indexhtm. Accessed June 2022.
Bradley CJ, Yabroff KR, Dahman B, Feuer EJ, Mariotto A, Brown ML. Productivity costs of cancer mortality in the United States: 2000–2020. J Nat Cancer Inst. 2008;100:1763–70.
Wong M, Lao XQ, Ho K-F, Goggins WB, Tse SL. Incidence and mortality of lung cancer: global trends and association with socioeconomic status. Sci Rep. 2017;7:14300.
Kulhánová I, Forman D, Vignat J, Espina C, Brenner H, Storm HH, Bauld L, Soerjomataram I. Tobacco-related cancers in Europe: the scale of the epidemic in 2018. Eur J Cancer. 2020;139:27–36.
International Agency for Research of Cancer. IARC monographs on the evaluation of carcinogenic risks to humans. In: A review of human carcinogens. Vol 100. Part E: Personal Habits and Indoor Combustions. Lyon, France (2012).
Eurostat. Tobacco consumption statistics. 2022. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Tobacco_consumption_statistics#Daily_smokers_of_cigarettes. Accessed August 2022.
Eurostat. Tobacco control measures. 2023. https://www.who.int/teams/health-promotion/tobacco-control/implementing/measures. Accessed March 2023.
Shiels MS, Haque AT, de González AB, Freedman ND. Leading causes of death in the US during the COVID-19 pandemic, March 2020 to October 2021. JAMA Intern Med. 2022;182:883–6.
Hanly P, Ahern M, Sharp L, Ursul D, Loughnane G. The cost of lost productivity due to premature mortality associated with COVID-19: a Pan-European study. Eur J Health Econ. 2022;23:249–59.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Author Contributions
All authors contributed to the study conception and design. Data collection was performed by I.S., data preparation and analyses were performed by M.O.O. All the authors discussed the results. This draft of the manuscript was written by all the authors and all of them commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research was funded by the XXXIX Edition of the Research Grant in Health Economics and Health Services, financed by the Spanish Health Economics Association in June 2019. We also appreciate the support of the Spanish Ministry of Education, Culture and Sport within the framework of the State Program for the Promotion of Talent and its Employability in R+D+i, State Mobility Subprogram 2019.
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer/World Health Organization.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication (from Patients/Participants)
Not applicable.
Availability of Data and Material
Any further data is available from the corresponding author upon request.
Code Availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ortega-Ortega, M., Hanly, P., Pearce, A. et al. Projected Impact on Labour Productivity Costs of Cancer-Related Premature Mortality in Europe 2018–2040. Appl Health Econ Health Policy 21, 877–889 (2023). https://doi.org/10.1007/s40258-023-00824-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00824-6