Abstract
Objectives
The aim of this study was to assess the cost effectiveness of allogeneic umbilical cord blood-derived mesenchymal stem cells with sodium hyaluronate (hUCB-MSC) compared with microfracture in patients with knee cartilage defects caused by osteoarthritis (OA) in South Korea.
Methods
A partitioned survival model approach was taken consisting of five mutually exclusive health states: excellent, good, fair, poor, and death over a 20-year time horizon. Utility values were obtained from a randomized clinical trial. Cost data were extracted from a database provided by the Health Insurance Review & Assessment Service, and the utilization of healthcare services was estimated from an expert panel of orthopedic surgeons using a structured questionnaire. The incremental cost-effectiveness ratio (ICER) in terms of quality-adjusted life-years (QALY) was calculated. Deterministic and probabilistic sensitivity analyses were performed.
Results
In the base case, the incremental costs of US$14,410 for hUCB-MSC therapy along with its associated QALY gain of 0.857 resulted in an ICER of US$16,812 (₩18,790,773) per QALY (95% confidence interval [CI] US$13,408–US$20,828) when compared with microfracture treatment from a healthcare payer perspective. From a societal perspective, the ICER was US$268 (₩299,255) per QALY (95% CI −US$2915 to US$3784). When using a willingness-to-pay threshold of US$22,367/QALY, the probability of hUCB being cost effectiveness compared with microfracture was 99% from the healthcare payer perspective and 100% from the societal perspective.
Conclusions
The study demonstrated that hUCB-MSC therapy was cost effective compared with microfracture when treating patients with knee OA. These findings should inform health policy decision makers about considerations for cost-effective therapy for treating knee OA to ultimately enhance population health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study, which is the first cost-effectiveness analysis performed for a stem cell-based drug used to treat knee cartilage defects, found that hUCB-MSC therapy was cost effective for the treatment of knee osteoarthritis when compared with microfracture. |
The calculated incremental cost-effectiveness ratio was below the current acceptable maximum willingness-to-pay threshold, which is one times the gross domestic product per capita for South Korea. |
The study findings should inform health policy decision makers about considerations for cost-effective therapy for treating knee osteoarthritis to ultimately enhance population health. |
1 Introduction
Knee osteoarthritis (OA) is a common condition that affects 240 million people globally and its occurrence is rapidly increasing due to an aging society and rising obesity rates [1]. The global prevalence of symptomatic knee OA was estimated to be 3.8%, with the highest prevalence observed in the high-income Asia Pacific region, which includes countries such as South Korea and Japan [2]. In South Korea, one-third of all adults aged 50 and older are diagnosed with knee OA [3, 4].
Knee OA has a substantial impact on a patient’s quality of life (QOL), resulting in worse outcomes compared with that of other chronic diseases or breast cancer [5,6,7,8,9]. Pain and physical disability from knee OA were the two major factors impacting QOL because of the effects on social connectedness, relationships, and emotional well-being [2, 10]. A Korean study also showed knee OA significantly adversely impacted QOL [4].
The nature of knee OA is deteriorative because of its degenerative properties and lack of self-healing potential. The current primary treatment modalities for knee OA include a combination of non-pharmacological and pharmacological interventions [11,12,13]. When pain cannot be controlled by pharmacological treatments, surgical interventions such as total knee replacement are suggested as an option for end-stage disease management. Multiple approaches to restore the structural and functional properties of cartilage or repair damaged cartilage include use of regenerative medicine and technological advancements including microfracture therapy, autologous chondrocyte implantation, and mesenchymal stem cell-based therapies, depending on patient profiles [11,12,13,14,15]. Microfracture therapy was developed to treat areas of damaged cartilage (chondral defects) by creating small holes in the bone (i.e., microfractures). This takes advantage of the body’s innate healing abilities as the microfractures provide an enriched blood supply and formation of a clot. Subsequently, progenitor cells, which aid in repair after injury, and growth factors form a cartilage layer where the damaged occurred [14,15,16]. This therapy is often used in patients with low collagen damage and has been proven efficacious for short-term functional improvement but not effective over the long term.
Autologous chondrocyte implantation is commonly used for large lesions and is less often used in the older population due to the diminished reparative potential of the autologous chondrocytes [17, 18]. Autologous chondrocyte implantation is a relatively costly procedure but provides substantial benefits to patients. Many studies found that autologous chondrocyte implantation was a cost-effective therapy compared with microfracture therapy, with some assumptions about long-term outcomes [19,20,21,22,23]. However, a few studies showed favorable cost effectiveness of microfracture therapy compared with autologous chondrocyte implantation [24, 25]. All of these cost-effectiveness studies emphasized the need to explore long-term effectiveness for autologous chondrocyte implantation and microfracture therapy.
A stem cell-based medicinal product, a composite of culture-expanded allogeneic human umbilical cord blood-derived mesenchymal stem cells combined with sodium hyaluronate (hUCB-MSC), has been used for the treatment of knee cartilage defects caused by degeneration from wear and tear and/or repeated trauma in patients with knee OA [18, 26, 27]. hUCB-MSC significantly improved patients’ cartilage repair, pain, and physical functions compared with microfracture without causing serious adverse events in short-term and long-term clinical studies [18, 26]. Stem cell-based treatments such as hUCB-MSC could be a promising and effective treatment option for patients with knee OA but a cost-effectiveness analyses of hUCB-MSC has not been conducted.
The objective of this study was to assess the cost effectiveness of hUCB-MSC therapy compared with microfracture in patients who had knee cartilage defects of grade IV, which is based on criteria from the International Cartilage Repair Society (ICRS), caused by degeneration from wear and tear and/or repeated trauma (i.e., OA) from the healthcare payer and societal perspectives in South Korea, respectively, and to provide valuable information to healthcare decision makers when selecting cost-effective therapy for the treatment of knee OA.
2 Methods
2.1 Model Design
A multi-state partitioned survival model over a 20-year time horizon was developed using Microsoft Excel® (Redmond, WA, USA) to assess the potential cost effectiveness of hUCB-MSC therapy compared with microfracture in patients with knee OA from both healthcare payer and societal perspectives in South Korea. Microfracture therapy was chosen as the comparator therapy as it is a commonly used treatment option for knee OA. The model analyzed a hypothetical cohort of patients who were diagnosed with knee OA and were 55 years old at the start of the simulated model [28].
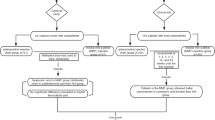
A model schematic illustrating possible transitions between five mutually exclusive health states is shown in Fig. 1. Patients entered the model after the initiation of hUCB-MSC or microfracture and then transitioned from an excellent health state to a good, fair, poor, or death health state. When a patient’s health state deteriorated to the poor health state, 18.8% of these patients received total knee replacement surgery based on clinical trial data [18, 26]. Patients were at risk of death from any health state or aging; therefore, they could always move to the death state. One-year cycles were used in the model.
Cost and effectiveness measures were discounted annually at a rate of 5% in accordance with the guidelines recommended by the Korea Health Insurance Review and Assessment Service (HIRA) [28]. A half-cycle correction was applied to improve the accuracy of the results because patients could move along health states at any point during a 1-year cycle.
2.2 Data Source
The effectiveness data used in the model were derived from a clinical trial that evaluated the surgical implantation of hUCB-MSC versus microfracture for treating full-thickness cartilage defects of the femoral condyle in a single compartment in patients with knee pain [18, 26]. Input parameters were based on the intention-to-treat analysis of all participants who were randomly assigned and received one of the surgical procedures described in the study. This clinical trial randomized 114 patients who had a full-thickness femoral cartilage defect of grade IV based on criteria from the International Cartilage Repair Society that was confirmed by arthroscopy or magnetic resonance imaging [18, 29, 30]. The mean age of these patients was 55.3 years for hUCB-MSC and 54.4 years for the microfracture group. The patients who participated in the trial were followed for 5 years. The death rate was estimated using the mortality rate of the general population obtained from age-specific life tables of the 2015 Korean population [31].
2.3 Structure of the Partitioned Survival Model
A partitioned survival analysis extrapolated data derived from the clinical trials and was used to create the cumulative probability survival curves of the five health states over the time horizon of the analysis. The four health states (excellent, good, fair, and poor) were defined using Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores at certain time points during the clinical trial.
The partitioned survival analysis model, which can demarcate the relationships between health states, used parametric survival regressions fitted to Kaplan–Meier curves and generated a survival curve for each health state (excellent, good, fair, poor, and death) using patient-level clinical trial data. The proportion of patients in each health state at a given time point was estimated from the areas under each health state survival curve [32]. The partitioned survival analysis model has similarities to state transition models but differs in its method of determining the proportion of patients in the health states at each time point [33]. The partitioned survival model was extrapolated over a 20-year time horizon. The first parametric survival curve measured the occurrence of the ‘excellent’ health state over a 5-year period and was extrapolated to estimate the cumulative probability of being in the ‘excellent’ health state according to classification of the WOMAC scores (between 0 and 14 points).
Various distributions (i.e., exponential, Weibull, Gompertz, log-logistic, and log-normal) of the standard parametric models were applied to fit the partitioned survival modeling curves for each health state [34]. The best-fitting independent survival curve was determined using the Akaike Information Criterion and the Bayesian Information Criterion goodness of fit statistics and verified using a visual inspection of the fitted survival curve. The fitted distributions selected for the parametric survival model were a log-logistic distribution for the excellent health state and log-normal for good and fair health states. The selected distributions by health state are shown in Table 1. The fitted survival functions for log-logistic and log-normal are
where t is time, μ is the scale, and σ is the shape parameter.
The proportion of patients in the ‘excellent’ health state at time t was directly estimated using the survival function S(t)1. The survival function for the ‘good’ health state S(t)2 was estimated sequentially, and the proportion of patients was derived from the difference between S(t)1 and S(t)2. The proportion of patients in the ‘fair’ health state was determined by calculating the difference between S(t)2 and the survival curve for S(t)3. Finally, the proportion of patients in the ‘poor’ health state was calculated as 1 − S(t)3. Because knee OA is not a life-threatening condition, the mortality rate of patients with knee OA was assumed to be the same as that of the general population. This model used the mortality rate of the general population obtained from the age-specific life tables of the 2015 Korean population [31]. All statistical and parametric survival analyses were performed using R version 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria) and the flexsurv package [35].
2.4 Utility Values
The degree of joint pain improvement was measured using a visual analog scale, and knee-specific patient-reported outcomes were measured using the WOMAC during clinical trials [36, 37]. The WOMAC is a multidimensional self-administered evaluation instrument that measures clinically important, patient-relevant symptoms in knee or hip OA. This instrument contains 24 questions consisting of three subscales including pain (five items scored 0–4, corresponding to 0–20 points), stiffness (two items scored 0–4, corresponding to 0–8 points), and physical function (17 items scored 0–4, corresponding to 0–68 points), where higher scores reflect worse health status [38]. The number of patients in each health state was calculated using the WOMAC scores collected during a 60-month follow-up period. In the present study, the WOMAC scores were used to classify patient health states into four levels: excellent, good, fair, and poor [18, 26, 39,40,41]. WOMAC scores from 0 to 14 points corresponded to the ‘excellent’ health state, 15–28 points corresponded to ‘good,’ 29–38 points corresponded to ‘fair,’ and >38 points corresponded to ‘poor’ [39,40,41].
Utility values for health states were derived from the WOMAC scores collected during the clinical trial [18, 26, 27]. WOMAC scores from the clinical trials were converted to utility index using the EQ-5D mapping algorithm as follows [42]: utility index value = 0.886 − (0.012 × WOMAC_pain) + (0.006 × WOMAC_stiffness) − (0.009 × WOMAC_functioning). This study used the EQ-5D-3L mapping algorithm to estimate utility values for the health states for consistency because the utility values of total knee replacement were previously measured using EQ-5D-3L [43]. This study applied a mean utility value of 0.717 for patients who received total knee replacement surgery [43]. Quality-adjusted life-years (QALYs) were calculated by multiplying the length of time spent in a particular health state by the utility value of the health state at a certain point in time.
2.5 Resource Use and Costs
This study included costs for hUCB-MSC medication, the initial operation, post-operation, and treatment after recurrence of the poor health state [44]. Medical costs were estimated based on utilized medical services which were collected using a structured questionnaire from an expert panel of seven orthopedic surgeons who performed hUCB-MSC or microfracture surgeries at university hospitals. The questionnaire consisted of questions for hUCB-MSC and microfracture regarding utilization of medical services during initial operation and post-operation (e.g., type, frequency, and duration of medical services for outpatient, hospitalization, and physical therapy, respectively) and medication use (e.g., dosage, strength, and duration of medications, incidence and treatment of adverse effects). This study assumed that two vials of hUCB-MSC (2.5 mL) were administered based on the results of the phase III clinical trials, and the market price per vial was US$6735 (₩8,000,000 Korean won).
Initial operation costs included those associated with hUCB-MSC, microfracture surgery, hospital stay, outpatient visits, and post-operation treatment and monitoring (including physical therapy) during hospitalization. The average hospital stay was 9 days for patients treated with hUCB-MSC and 8 days for patients treated with microfracture based on surveying the expert panel of seven orthopedic surgeons using structured questionnaires. Post-operation costs included the annual costs of outpatient visits, which were assumed to be once a month, monitoring, physical therapy follow-up, and post-operation medication. After patients received total knee replacement surgery, the treatment costs included the costs of operation, monitoring, medication, and physical therapy, which was assumed to be 20 times per month for 3 months following the operation.
Those unit costs were retrieved from the Korean Medical Service Fee, and the price of drugs was listed by the HIRA [48]. The treatment costs of total knee replacement surgery were retrieved from the nationwide average cost reported by the HIRA. All costs were adjusted to 2021 Korean won (₩) based on the medical cost component of the consumer price index. These costs were then converted to 2021 United States dollars (US$) using the average currency exchange rate between January 1 and June 30, 2021 (₩1 = US$0.00089467). Cost inputs in the model are presented in Table 1.
2.6 Time and Productivity Costs
When the cost-effectiveness analysis was performed from the societal perspective, the model included time and productivity costs which included costs associated with treatment, such as time spent by patients, their families, and caregivers; costs associated with lost or impaired ability to work or to enjoy leisure activities due to morbidity; and economic productivity loss due to death [45]. Costs associated with patients and caregivers were based on length of time spent on treatment-related activities/services collected from an expert panel of seven orthopedic surgeons, and wage data were derived from reports of government statistics (Table 1).
Time costs related to receiving treatment were estimated based on the mean hourly wage of labor conditions by employment type [46], and the mean time spent for outpatient visits and hospitalization was based on a survey examining national medical care resources and utilization. The average labor wage was calculated by applying a weighted average to the age distribution of trial participants multiplied by the time spent for treatment. Caregiver time costs were calculated by multiplying the number of hospitalization days by the market labor wages per day for caregivers. Transportation costs for clinic visits (i.e., direct nonmedical costs) were calculated using the Third Korea National Health and Nutrition Examination Survey [47].
Absenteeism, which measures the number of days patients were absent from work per year, and presenteeism, which measures the proportion of reduced work performance, affected by knee OA were indirectly measured by a clinical expert using the Work Productivity and Activity Impairment Structured questionnaire (general health V2.0) [48]. Costs associated with work productivity loss stratified by health state and type of knee operation were calculated using the following equation: costs associated with work productivity loss = ([number of days absent from work/total number of yearly working days] + [number of working days/total number of yearly working days × proportion of impaired ability to work]) × (average labor wage).
2.7 Sensitivity Analyses
The robustness of the study results was tested using one-way sensitivity and probabilistic sensitivity analyses.
2.7.1 One-Way Deterministic Sensitivity Analysis
A one-way sensitivity analysis was performed to measure the relative impact of key parameters on the cost effectiveness of hUCB-MSC treatment. Parameters tested for model outcomes included discount rates (ranging between 0% and 7.5% for cost and effectiveness) and utility values (varied using 95% confidence intervals [CIs] of change in utilities for each health state). The model also varied costs using a range of ± 20% of the point estimates, which included medical test costs per year after surgery, the cost of total knee replacement, and the cost of hUCB-MSC.
2.7.2 Probabilistic Sensitivity Analysis
Probabilistic sensitivity analyses were performed with 10,000 Monte Carlo simulations to assess the joint impact of key input parameter uncertainties on the cost effectiveness of hUCB-MSC therapy. The assumptions and distributions for the input parameters are listed in Table 1. Utilities were varied using the beta distribution, and cost parameters were varied using gamma distributions [49].
The model calculated the cumulative costs and QALYs for 20 years following the year of the surgery using a 5% discount rate. The ICERs and their respective 95% CIs between hUCB-MSC and microfracture were calculated. Cost-effectiveness acceptability curves were constructed over a wide range of willingness-to-pay thresholds to determine the probability that hUCB-MSC treatment was a cost-effective therapy.
3 Results
The base-case analysis comparing hUCB-MSC therapy with microfracture is presented in Table 2. An additional 0.857 QALYs were gained with the hUCB-MSC therapy (8.256 QALYs) compared with microfracture (7.399 QALYs). From a healthcare payer perspective, the total cost per patient was US$23,831 for the hUCB-MSC therapy and US$9421 for microfracture. These cost and health outcomes resulted in an ICER of US$16,812 (₩18,790,773) per QALY gained (95% CI US$13,408–US$20,828). From a societal perspective, the total cost per patient was US$65,623 for the hUCB-MSC therapy and US$65,394 for microfracture. The incremental costs of hUCB-MSC therapy compared with microfracture were US$229 (₩256,498), with an associated gain of 0.857 QALYs, resulting in an ICER of US$268 (₩299,255) per QALY (95% CI −US$2915 to US$3784) in the base-case analysis.
The one-way sensitivity analysis presents the eight variables that had the most influential effects on the ICER values out of the key study variables (Fig. 2). From the healthcare payer perspective, the duration of analysis was the most influential parameter that caused ICER value change, followed by the discount rate for effectiveness. However, from the societal perspective, the discount rate for cost was the most influential model parameter, followed by reduced productivity of presenteeism in the poor health state.
The uncertainty around ICERs was plotted on the cost-effectiveness plane using Monte-Carlo simulations (Fig. 3). As shown in the cost-effectiveness planes from the societal and healthcare payer perspectives, all ICER simulations were located in the right-hand quadrants for both perspectives, suggesting hUCB-MSC therapy was potentially cost effective or dominant. When using a willingness-to-pay threshold of US$22,367/QALY, the probability of hUCB being cost effective compared with microfracture was 99% from the healthcare payer perspective and 100% from the societal perspective (Fig. 4).
4 Discussion
To the best of our knowledge, this is the first cost-effectiveness analysis performed for a stem cell-based drug used to treat knee cartilage defects using 5-year long-term follow-up data from a randomized clinical trial. This study found that hUCB-MSC therapy was cost effective, with an ICER per QALY gained of US$268 (₩299,255) from the societal perspective and US$16,812 (₩18,790,773) from the healthcare payer perspective for the treatment of knee OA when compared with microfracture. This ICER was below the acceptable maximum willingness-to-pay threshold for a new drug (except for cancer) of US$22,367 (₩25,000,000) per QALY, as commonly used by the HIRA in Korea. The differences in ICER between the two perspectives were attributable to a much lower productivity loss with the hUCB-MSC therapy. Although HIRA requested a cost-effectiveness analysis from the healthcare payer perspective, this study conducted analyses from both the healthcare payer and societal perspectives to help readers compare the results of this study to those of other studies [50].
Most previous studies assessed or summarized cost effectiveness of autologous chondrocyte implantation compared with a common comparator such as microfracture, which was the prevailing therapy for the treatment of cartilage defects of the knee prior to the introduction of hUCB-MSC therapy [15, 19,20,21,22,23,24,25]. The ICER values of autologous or characterized chondrocyte implantation compared with microfracture (using USD currency and the US medical service price index in 2021) ranged from US$25,251/QALY to US$81,600/QALY depending on scenarios [20,21,22]. Cost-effectiveness analyses using a decision tree model with a 40-year time horizon from the global healthcare payer perspective in Belgium found that the ICER value was US$25,251/QALY (as of 2021) [20]. A study conducted using a decision tree model with a duration of 47 years from the German statutory health insurance perspective estimated ICER values ranged from US$58,656 to US$81,600 per QALY (as of 2021) [21]. A cost-effectiveness study of characterized chondrocyte implantation compared with microfracture estimated the ICER values to be US$32,929/QALY (as of 2021) when a Markov model was applied for a 75-year time horizon from the UK National Health Service perspective [22]. In contrast, a review study reported that microfracture was the most effective treatment option compared with autologous chondrocyte implantation for the chondral lesions in the knee; this finding was later supported by another review study [24, 25]. Both review studies recommended well designed clinical trials with an appropriately long-term time duration to ensure robust outcomes.
In general, the range of ICER values found for autologous chondrocyte implantation from the literature was slightly higher than those found in the present study. This difference can be partially explained by the clinical characteristics of autologous chondrocyte implantation, which requires two arthroscopic procedures: one to collect the cells and one to implant them. If the most recent autologous chondrocyte implantation method, a one-step procedure, was applied, the ICER values would likely be lower.
The present study had several strengths, including the use of long-term outcome data collected during 5-year follow-up clinical trials, and a partitioned survival model that constructed survival curves from Kaplan–Meier curves, which the present study used to construct health states [18, 33]. Therefore, long-term efficacy, utility, and safety data were available to establish a comprehensive partitioned survival model. The survival functions that inform patient proportion estimates in the partitioned survival analysis make the models intuitively appealing, easy to construct and use to communicate results, and able to be replicated using in-trial data [33]. The time frame of this study was 20 years (i.e., life-time horizon) with patients who were 55 years old at the start of the model. Because knee OA is a disease that persists throughout an individual’s life, the lifetime horizon used for the model was appropriate, and a similar time frame was also observed in previous cost-effectiveness studies of autologous chondrocyte implantation for cartilage defects [20, 22, 23, 51].
The present study estimated the cumulative probabilities between the four health states with a partitioned survival analysis using actual WOMAC scores that were measured annually to assess the efficacy and functional status during 5-year clinical trials [18, 26]. Using these four health states and the death state throughout the model analyses was one of the study’s strengths because these states reflected detailed post-operation outcomes during the 5-year long-term follow-up period. The cut-off points of WOMAC scores for each of the health states corresponded to the pre-existing classification of severe arthritis, defined as a WOMAC score of 39 or greater [39,40,41]. A recent study suggested that the four health states of WOMAC scores can also be classified based on the level of patient satisfaction after total knee arthroplasty [52].
In the present study, the costs considered from a healthcare payer perspective were similar to previous cost-effectiveness studies of autologous chondrocyte implantation that used a Markov model [22, 23]. The cost of microfracture was estimated to be between US$4092 and US$5523, including the costs of the procedure, inpatient stay, outpatient visits, and rehabilitation [22, 23]. The present study assumed that hUCB-MSC required 9 inpatient days and microfracture required 8 days, and outpatient visits for both therapies required two visits before the surgery and three visits annually after the surgery. These assumptions were based on data collected from an expert panel of orthopedic surgeons. Despite the fact that the frequency of inpatient or outpatient visits for the procedure could be slightly varied, the cost of microfracture therapy was assumed to be US$798 (₩892,236).
Although this study provides valuable information on the cost effectiveness of hUCB-MSC therapy for patients with knee OA using long-term follow-up data collected in a randomized clinical trial, the findings should be interpreted carefully because of limitations. First, because healthcare utilization, productivity loss, and effectiveness data were derived from a clinical trial conducted in Korea, treatment costs may need to be adjusted for each country’s healthcare delivery and health insurance systems. Thus, the generalizability of these results to other countries should be interpreted with caution.
The use of clinical trial data might cause some inherent bias for the effectiveness of treatments. The costs may not have been estimated accurately because of factors such as the evaluation of patients’ healthcare utilization patterns and proxy of work productivity losses using structured questionnaires filled out by clinical experts. Utility values were converted from WOMAC scores using the mapping algorithm of EQ-5D, which was developed based on the UK population, because a mapping algorithm for the Korean population was not available. Utility values were also assumed to be the same for both the healthcare payer and societal perspectives because of limited data. However, performing deterministic and probabilistic sensitivity analyses may have addressed some of these uncertainties. Also, the main limitation of the partitioned survival model is its fundamental structural assumption that the survival endpoints are independent. Assuming independence between endpoints reduces the value of a partitioned survival model as a means of quantifying decision uncertainty [33]. A previous study that used a partitioned survival analysis and Markov models produced very similar expected costs, outcomes, and ICERs [53].
5 Conclusion
This study found that hUCB-MSC therapy for patients with knee OA was cost effective when compared with microfracture from both the healthcare payer (ICER = US$18,790/QALY gained) and societal perspectives (ICER = US$268/QALY gained). Patients and healthcare providers may consider hUCB-MSC therapy an economically attractive treatment option compared with microfracture, addressing an unmet need for improving overall outcomes. This study provides a framework for healthcare payers and practitioners to assess the cost effectiveness of stem cell-based medical products for treating cartilage regeneration in patients with knee OA. The findings should inform health policy decision makers about considerations for cost-effective therapy for treating patients with knee OA to enhance patient QOL. Future research should explore the long-term cost effectiveness of hUCB-MSC therapy with less uncertainty regarding the study parameters.
Change history
21 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40258-022-00768-3
References
Neuprez AH, Kaux J-F, Kurth W, Daniel C, Thirion T, et al. Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin Rheumatol. 2020;39:861–71. https://doi.org/10.1007/s10067-019-04811-y.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:1323–30.
Hong JW, Noh JH, Kim D-J. The prevalence of and demographic factors associated with radiographic knee osteoarthritis in Korean adults aged ≥ 50 years: the 2010–2013 Korea National Health and Nutrition Examination Survey. PLoS ONE. 2020;15(3): e0230613. https://doi.org/10.1371/journal.pone.0230613 (eCollection 2020).
Lee S, Kim S-J. Prevalence of knee osteoarthritis, risk factors, and quality of life: the Fifth Korean National Health And Nutrition Examination Survey. Int J Rheum Dis. 2017;20(7):809–17.
Vitaloni M, Bemden AB-V, Contreras RMS, Scotton D, Bibas M, Quintero M, et al. Global management of patients with knee osteoarthritis begins with quality of life assessment: a systematic review. BMC Musculoskelet Disord. 2019;20:493. https://doi.org/10.1186/s12891-019-2895-3.
Hunter DJ, Riordan EA. The impact of arthritis on pain and quality of life: an Australian survey. Int J Rheum Dis. 2014;17:149–55.
Kimman ML, Dirksen CD, Lambin P, Boersma LJ. Responsiveness of the EQ-5D in breast cancer patients in their first year after treatment. Health Qual Life Outcomes. 2009;7:11. https://doi.org/10.1186/1477-7525-7-11.
Matza LS, Boye KS, Yurgin N. Validation of two generic patient-reported outcome measures in patients with type 2 diabetes. Health Qual Life Outcomes. 2007;5:47. https://doi.org/10.1186/1477-7525-5-47.
Schweikert B, Hahmann H, Leidl R. Validation of the EuroQol questionnaire in cardiac rehabilitation. Heart. 2006;92:62–7.
Kiadaliri A, Lamm C, de Verdier M, Engström G, Turkiewicz A, Lohmander L, et al. Association of knee pain and different definitions of knee osteoarthritis with health-related quality of life: a population-based cohort study in southern Sweden. Health Qual Life Outcomes. 2016;14:121. https://doi.org/10.1186/s12955-016-0525-4.
Zhang W, Moskowitz R, Nuki G, Abramson S, Altman R, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartil. 2008;16:137–62.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartil. 2019;11:1578–89. https://doi.org/10.1016/j.joca.2019.06.011.
Bruyère O, Honvo G, Veronese N, Arden NK, Branco J, Curtis EM, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49:337–50. https://doi.org/10.1016/j.semarthrit.2019.04.008.
Mithoefer K, McAdams T, Williams R, Kreuz P, Mandelbaum B. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systemic analysis. Am J Sports Med. 2009;37:2053–63.
Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint—a golden standard? J Clin Orthop Trauma. 2016;7:145–52.
Steadman JR, Rodkey WG, Briggs KK. Microfracture: Its history and experience of the developing surgeon. Cartilage. 2010;1:78–86. https://doi.org/10.1177/1947603510365533.
Harris JD, Siston RA, Pan X, Flanigan DC. Autologous chondrocyte implantation: a systematic review. J Bone Jt Surg Am. 2010;92:2220–33. https://doi.org/10.2106/JBJS.J.00049.
Lim HC, Park YB, Ha CW, Cole BJ, Lee BK, Jeong HJ, et al. Allogeneic umbilical cord blood-derived mesenchymal stem cells implantation versus microfracture for large full-thickness cartilage defects in elderly patients: randomized clinical trial & extended 5-year clinical follow-up. Orthop J Sports Med. 2021;9(1):2325967120973052. https://doi.org/10.1177/2325967120973052.
Clar C, Cummins E, Mclntyre L, Thomas S, Lamb J, Bain L, et al. Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation. Health Technol Assess. 2005;9:1–101.
Gerlier L, Lamotte M, Wille M, Kreuz P, Vanlauwe J, Dubois D, et al. The cost utility of autologous chondrocytes implantation using ChondroCelect in symptomatic knee cartilage lesions in Belgium. Pharmacoeconomics. 2010;28:1129–46.
Koerber F, Rolauffs B, Rogowski W. Early evaluation and value-based pricing of regenerative medicine technologies. Regen Med. 2013;8:747–58. https://doi.org/10.2217/rme.13.69.
Elvidge J, Bullement A, Hatswell AJ. Cost effectiveness of characterised chondrocyte implantation for treatment of cartilage defects of the knee in the UK. Pharmacoeconomics. 2016;34:1145–59.
Mistry H, Connock M, Pink J, Shyangdan D, Clar C, Royle P, et al. Autologous chondrocyte implantation in the knee: systematic review and economic evaluation. Health Technol Assess. 2017;21:1–328. https://doi.org/10.3310/hta21060.
Aae TF, Randsborg P-H, Luras H, Aroen A, Lian OB. Microfracture is more cost-effective than autologous chondrocyte implantation: a review of level 1 and level 2 studies with 5 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26:1044–52. https://doi.org/10.1007/s00167-017-4802-5.
Schrock JB, Kraeutler MJ, Houck DA, McQueen MB, McCarty EC. A Cost-effectiveness analysis of surgical treatment modalities for chondral lesions of the knee: microfracture, osteochondral autograft transplantation, and autologous chondrocyte implantation. Orthop J Sports Med. 2017;5(5):2325967117704634. https://doi.org/10.1177/2325967117704634.
Park Y, Ha CW, Kim M. Allogeneic umbilical cord blood-derived mesenchymal stem cells versus microfracture for large full-thickness cartilage defects. Cytotherapy. 2020;22(5):S29–30. https://doi.org/10.1016/j.jcyt.2020.03.013.
Park YB, Ha CW, Lee CH, Yoon YC, Park YG. Cartilage regeneration in osteoarthritic patients by a composite of allogeneic umbilical cord blood-derived mesenchymal stem cells and hyaluronate hydrogel: results from a clinical trial for safety and proof-of-concept with 7 Years of extended follow-Up. Stem Cells Transl Med. 2017;6:613–21.
Korea Health Insurance Review & Assessment Service. Korean guidelines for economic evaluations analysis. Korea Health Insurance Review & Assessment Service; 2011.
Mainil-Varlet P, Aigner T, Brittberg M, Bullough P, Hollander A, Hunziker E, et al. Histological assessment of cartilage repair: a report by the Histology Endpoint Committee of the International Cartilage Repair Society (ICRS). J Bone Joint Surg Am. 2003;85-A(Suppl 2):45–57.
Van den Borne MP, Raijrnakers NJ, Vanlauwe J, Victor J, de Jong SN, Bellernans J, et al. International Cartilage Repair Society (ICRS) and oswestry macroscopic cartilage evaluation scores validated for use in autologous chondrocyte implantation (ACI) and microfracture. Osteoarthritis Cartil. 2007;15(12):1397–402. https://doi.org/10.1016/j.joca.2007.05.005.
Korea Statistical Information Service. Population/Household: Life Tables 1970-2019. 2019. https://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ETITLE&parmTabId=M_01_01&statId=1994042&themaId=#A5.2. Accessed 18 Oct 2020.
Smare C, Lakhdari K, Doan J, Posnett J, Johal S. Evaluating partitioned survival and markov decision-analytic modeling approaches for use in cost-effectiveness analysis: estimating and comparing survival outcomes. Pharmacoeconomics. 2019. https://doi.org/10.1007/s40273-019-00845-x.
Woods B, Sideris E, Palmer S, Latimer N, Soares M. NICE DSU Technical Support Document 19. Partitioned Survival Analysis for Decision Modeling in Health Care: A Critical Review. 2017.
Latimer NR. Survival analysis for economic evaluations alongside clinical trials–extrapolation with patient-level data: inconsistencies, limitations, and a practical guide. Med Decis Making. 2013;33:743–54.
Jackson CH. Flexsurv: a platform for parametric survival modeling in R. J Stat Softw. 2016. https://doi.org/10.18637/jss.v070.i0.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40.
Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum. 1989;18:14–7. https://doi.org/10.1016/0049-0172(89)90010-3.
Wright JG, Young NL. The patient-specific index: asking patients what they want. J Bone Jt Surg Am. 1997;79a(7):974–83. https://doi.org/10.2106/00004623-199707000-00003.
Park SS, Lee SH, Kim WH, Ha SH. Cementless total hip arthroplsty using the conical femoral stem. J Korean Orthop Assoc. 2013;48:426–32.
Sohn OJ, Lee DC, Cho JH. Comparison between mobile bearing and fixed bearing T.K.A. in the same patient. J Korean Orthop Assoc. 2008;43:200–6.
Hawker GA, Wright JG, Coyte PC, Williams I, Harvey B, Glazier R, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–22. https://doi.org/10.1056/NEJM200004063421405.
Barton GR, Sach TH, Jenkinson C, Avery AJ, Doherty M, Muir KR. Do estimates of cost-utility based on the EQ-5D differ from those based on the mapping of utility scores? Health Qual Life Outcomes. 2008;6:51. https://doi.org/10.1186/477-7525-6-51.
Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, et al. The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet. 2019;394:746–56. https://doi.org/10.1016/S0140-6736(19)31281-4.
Health Insurance Review & Assessment Service. Medica Service Fee Schedule in South Korea. 2020. https://www.hira.or.kr/rd/insuadtcrtr/bbsView.do?pgmid=HIRAA030069000400&brdScnBltNo=4&brdBltNo=50936&isPopupYn=Y#none. Accessed 17 Mar 2021.
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. 2nd ed. New York: Oxford University Press; 2017.
Ministry of Korea Employment and Labor. Survey Report on Wages by Employment Type 2017. http://laborstat.moel.go.kr. Accessed 25 May 2021.
Ministry of Korea Health and Welfare. Korea National Health and Nutrition Examination Survey (KNHANES) 2005. http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=336053&page=1. Accessed 25 Jan 2021.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Phmarmacoeconomics. 1993;4:353–65.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. New York: Oxford University Press; 2006.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316:1093–103. https://doi.org/10.1001/jama.2016.12195.
Saris DB, Vanlauwe J, Victor J, Haspl M, Bohnsack M, Fortems Y, et al. Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture. Am J Sports Med. 2008;36:235–46. https://doi.org/10.1177/0363546507311095.
Walker LC, Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, et al. The WOMAC score can be reliably used to classify patient satisfaction after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018. https://doi.org/10.1007/s00167-018-4879-5.
Goeree R, Villeneuve J, Goeree J, Penrod JR, Orsini L, Tahami Monfared AA. Economic evaluation of nivolumab for the treatment of second-line advanced squamous NSCLC in Canada: a comparison of modeling approaches to estimate and extrapolate survival outcomes. J Med Econ. 2016;19:630–44. https://doi.org/10.3111/13696998.2016.1151432.
Acknowledgments
The authors would like to thank Yuseon Jung, Pharm.D. for searching the literature and writing the first draft of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was partially funded by an unrestricted research grant from Medipost Co., Ltd (the manufacturer of Cartistem), South Korea. The funding source did not have any role in the study design, collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Conflicts of interest
The authors declare that they have no conflict of interest to disclose.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Code availability
The model used for the present study is available from the corresponding author upon reasonable request.
Author contributions
KS contributed to the study conception and design, data collection, analysis and interpretation of the data, and manuscript development. BJC, AG, SML CWH, DCS, and MKK participated in data collection and analysis and writing the draft manuscript. DCS, HC, GYH, and SML performed the cost-effectiveness analysis and simulation. KS and SML had full access to all the data in the study and take responsibility for the integrity of the work as a whole. All authors contributed to the final manuscript’s writing, editing, and approval.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication (from patients/participants)
Not applicable.
Additional information
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Suh, K., Cole, B.J., Gomoll, A. et al. Cost Effectiveness of Allogeneic Umbilical Cord Blood-Derived Mesenchymal Stem Cells in Patients with Knee Osteoarthritis. Appl Health Econ Health Policy 21, 141–152 (2023). https://doi.org/10.1007/s40258-022-00762-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00762-9