Abstract
Objective
We examined the effects of fixe-dose combinations (FDCs) versus loose-dose combinations (LDCs) on costs from the payer and patient perspective and investigated potential channels contributing to differences in costs between the two modes of treatment.
Methods
We investigated administrative data from 2017 to 2020 on diabetes patients in Germany. After using prospensity-score matching to remove dissimilarities between FDC and LDC patients, we compared changes in costs with a difference-in-differences approach. We analyzed pharmaceutical costs, inpatient and outpatient costs, other costs and total healthcare costs from the payer perspective, and co-payments from the patient perspective.
Results
The sample comprised 1117 FDC and 1272 LDC patients. Regression analysis revealed that FDC therapy significantly increased antidiabetic pharmaceutical spending in the first year by 5.5% (p < 0.01), but decreased co-payments by 33% (p < 0.01) in the first and 44% (p < 0.01) in the second year. We also observed a trend towards higher outpatient spending in the first year. No significant differences were found with respect to inpatient or other costs. The increase in antidiabetic pharmaceutical spending did not contribute to a significant increase in total healthcare expenditure. We identified a shift of co-payments to the payer and higher adherence as possible mechanisms behind the increase in antidiabetic pharmaceutical spending.
Conclusion
Although FDC therapy increased disease-specific pharmaceutical spending in the short term, this increase did not lead to differences in total healthcare costs from the payer perspective. From the patient perspective, FDC therapy may be the preferred treatment approach, because of significant saving in co-payments, which is likely attributable to the elimination of one co-payment and therefore a shift in costs to the payer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fixed-dose combinations decrease co-payments for type 2 diabetes patients compared to loose-dose combinations. |
Fixed-dose combinations for type 2 diabetes do not lead to higher total healthcare spending compared to loose-dose combinations during the study period. |
In the short term, fixed-dose combinations increase antidiabetic pharmaceutical spending, reflecting a shift in co-payments from the patient to the payer, as well as an increase in medication adherence. |
1 Introduction
Fixed-dose combinations (FDCs) contain multiple substances in a single dosage form and aim at improving medication adherence through a reduction in pill burden [1]. While the positive effect of FDCs on medication adherence has been widely studied, little is known about their economic effects [2]. On the one hand, the improvements in adherence achieved through FDCs may result in higher pharmaceutical spending because of more regular refills. Additionally, pharmaceutical companies might use FDCs for “evergreening”, i.e., the practice of seeking further patents on variations of the original drug, which might also result in higher costs to payers [3]. On the other hand, these costs may be offset by improved health outcomes and lower costs of disease progression in the long run [4]. Moreover, because FDCs must compete for market share with loose-dose combinations (LDCs), incremental innovation does not always result in increased costs [5]. Indeed, in cases where the costs of FDC products are less than the combined costs of the individual substances, FDCs might offer a financial advantage for the healthcare system. From the patient perspective in Germany, being prescribed an FDC may have the benefit of reducing co-payments because these are levied on individual packages and not on substances [6]. Yet this, in turn, might improve medication adherence because out-of-pocket spending was found to be a contributing factor to non-adherence [7]. In short, it remains unclear whether FDCs result in lower or higher expenditure for patients and payers compared to LDCs. Therefore, it was the aim of this study to investigate the economic effects of FDC therapy compared to LDC therapy in type 2 diabetes mellitus (T2D) from the payer and patient perspective. Moreover, we investigated potential channels contributing to differences in costs between the two modes of treatment.
2 Literature Review
Few studies to date have analyzed the economic effects of antidiabetic FDCs, but the results have been mainly in favor of FDC therapy, albeit predominantly in the context of the USA. Two studies analyzed the reimbursement amount paid to dispensing pharmacies by the state for Texas Medicaid patients, i.e., the perspective of the payer, based on prescription claims from 1999 till 2005 [8] and from 2004 till 2007 [9]. Both studies concluded that FDC products were less expensive than their LDC counterparts [8, 9]. Another retrospective claims-based study from the USA investigated combined health plan and patient paid amounts in a managed care population during the year after dual therapy initiation in 2007 and 2008 [10]. The authors investigated all-cause costs and diabetes-related costs and distinguished between pharmacy costs, medical costs, and total costs. They found that FDC treatment was associated with lower all-cause and lower diabetes-related healthcare costs compared to LDC therapy. Mean diabetes-related pharmacy costs were higher for FDC treatment, but the difference was not statistically significant [10].
Similarly, Lokhandawala et al. [11] compared economic outcomes for FDC versus LDC in treatment-naïve T2D patients insured through employer-sponsored plans from 2009 to 2013. Again, costs reflected all payments made to providers of care from both the health plan and the patient combined. The authors found that all-cause and T2D-related monthly costs were significantly lower when patients were treated with FDCs compared to LDCs, an exception being all-cause medical costs, for which there was no difference between the two groups. When outcomes were not adjusted, the authors observed significantly higher all-cause and diabetes-related monthly prescription costs, which contributed to significantly higher T2D-related total monthly costs [11].
Only one study specifically focused on costs to consumers [6]. It was based on a survey of retail medication prices for consumers at four local pharmacies in Columbus, Georgia, and two online pharmacies. Direct price comparisons showed that most FDCs cost the same or less than the retail purchase of the individual substances [6].
Aside from studies in the USA, there is only one study from Italy on this topic. In it, the authors compared gross expenditure on drugs from pharmacies, hospital costs, and examination costs in a descriptive statistical analysis using the ARNO Observatory claims database [12]. In line with the findings from the USA, they found that average expenditure per patient/year for FDC therapy was lower than for LDC therapy. Only DRG mean expenditure/year was higher for FDC therapy [12]. The authors did not assess, however, whether the differences were statistically significant.
Our contribution to the literature is fourfold. First, by analyzing German data, we add evidence on the economic effects of FDC therapy in a more regulated and public healthcare market than that in the USA. Second, economic effects may relate to patients, payers, or the community as a whole. By using data from a statutory health insurer in Germany, we were able to distinguish between costs for the patient and for the payer, as well as between cost components, such as pharmaceutical costs. Third, the studies published to date have not isolated the economic effects of FDCs. Establishing a causal relationship between treatment alternatives and outcomes is difficult due to selection or omitted variable bias. To overcome this, we combined prospensity-score matching (PSM) with difference-in-differences (DiD) estimation and generated a quasi-experiment. Lastly, we investigated potential mechanisms for differences in changes in outcomes between the cohorts.
3 Methods
3.1 Data and Study Cohorts
To compare the costs of dual therapy with FDCs to dual therapy with LDCs for T2D, we performed a retrospective cohort study. We used administrative data from the largest statutory health insurer in Germany, Techniker Krankenkasse, which provides coverage for more than 10 million people, i.e., about 15% of residents with statutory health insurance [13]. Almost 6% of those insured were T2D patients, which corresponds roughly to the nationwide rate of approximately 7% of the German population [14]. The data included longitudinal patient-level information on socio-demographics and all services provided to patients between 2017 and 2020. We analyzed T2D patients (ICD-GM-10-diagnosis E11) whose blood glucose was no longer sufficiently controlled by metformin monotherapy, which is the first-choice substance in oral antidiabetic treatment. To maintain their blood glucose levels, patients added a second oral substance to metformin in 2018. The dual combination could be prescribed either as an FDC or as an LDC. To ensure valid comparisons, we included FDC and LDC medications only if the additive substance was the same. In accordance with the literature, we identified FDC therapy directly using the ATC fourth level code for combination products (A10BD). We defined LDC therapy as co-administration of metformin and a second oral antidiabetic drug (ATC three-level codes A10B, except A10BD) with at least two overlap periods of 15 days or more [8, 9]. The first fill of the additive substance was defined as the index date. To allow for risk adjustment, a pre-index period of 1 year prior to the index date was set as the basis for determining patient-level risk profiles, whereas the follow-up period was 2 years. The study population was further restricted to patients who were (1) insulin-naïve, (2) not pregnant, (3) continuously enrolled (and did not die during the observation period), (4) had no antidiabetic prescription other than metformin in the pre-index period and metformin plus a second substance in the follow-up period, and (5) had been treated with metformin monotherapy for at least 6 months before the index date.
3.2 Study Outcomes
We calculated direct medical costs from the payer perspective. We assessed all-cause total healthcare costs and distinguished between inpatient treatment costs, outpatient treatment costs, pharmaceutical costs, and other costs, such as those for aids and appliances. In addition, we analyzed patient co-payments for medications. For pharmaceutical costs and co-payments, we additionally identified costs due to T2D (ATC fourth level code A10B).
3.3 Statistical Analysis and Risk Adjustment
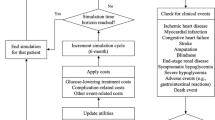
Because costs have highly right-skewed distributions and include zeros, we transformed outcomes by taking their natural logarithm plus one. Furthermore, to remove outliers, we winsorized costs at 99th percentiles.
To isolate the causal effect of receiving FDCs on costs, we combined PSM with a DiD regression. By doing so, we addressed the non-randomized treatment allocation inherent to our study design. In the first step, PSM reduces confounding by creating a sample of treated patients (the FDC cohort) that is comparable on observed covariates to a sample of untreated patients (the LDC cohort). We matched exactly on gender and 10-year age groups. To estimate the propensity score, we fitted a logistic regression in which the probability of receiving an FDC was the dependent variable. We included a set of pre-specified covariates measured in the pre-index period that were considered to have a high predictive potential for receiving an FDC or an LDC and the outcomes. These covariates included socio-demographic variables (age, insurance status as a proxy for socio-economic backgroundFootnote 1) as well as binary variables that indicate generic comorbidities (the Elixhauser groups and pharmacy-based metrics) [15, 16], additional T2D-associated conditions (eye complications, diabetic foot syndrome/neuropathy, myocardial infarction, ischemic heart disease, cerebrovascular disease, renal complications, angina pectoris; the corresponding ICD-GM-10 diagnoses can be found in Table S1 of the Online Supplementary Material (OSM)) [17], patients participating in a T2D DMP, and physicians treating any patients participating in a T2D DMP. We then applied a 2:1 greedy nearest neighbor matching without replacement, i.e., each patient receiving an FDC in the post-index period was matched with the two closest patients receiving an LDC in the post-index period who satisfied the matching criteria. This 2:1 matching has been shown to result in optimal estimation of treatment effects in the literature [18]. Matches were chosen within the recommended caliper width of 0.2 standard deviations of the logit of the propensity-score and over the common support region only [19]. Although this may not result in all intervention patients being matched, it increases precision [20].
In the second step, differences in expenditure between the FDC and the LDC cohorts, due to time-constant unobserved factors, were eliminated through DiD estimation. The DiD estimator measures whether there is a differential change in costs before and after adding a second oral substance in the FDC group relative to the LDC group. We enriched the basic DiD specification by controlling for all conditioning variables used in the balancing step to reduce the standard error of the estimate. The structural equation of interest can be described as follows:
where \({Y}_{it}\) are the cost outcomes of interest for individual \(i\) in period \(t\), \({\mathrm{Treat}}_{i}\) suggests whether patients received an FDC in the post-index period, \({\mathrm{Post}}_{it}\) indicates the period of dual therapy, i.e., after the index date, and \({X{^{\prime}}}_{i}\) is a vector of covariates. Thus, the DiD estimator of interest is \({\beta }_{3}\), indicating the average differences in changes in costs attributable to the treatment choice in the post-index period, called the average treatment effect on the treated.
Our empirical strategy relies on the assumption that in the absence of combination products (e.g., if they were not available), patients would have received the analogous LDC. This means that in the absence of treatment, the unobserved differences between the treatment and control group are the same over time. Although this assumption is not testable, we inspected the parallel trends of outcomes in the pre-index period (Fig. F1 of the OSM). Moreover, we ran an in-time placebo test by setting the index date to 6 months prior to the actual index date, resulting in a faked pre- and post-index period, each of which was limited to 6 months (Table S2 of the OSM).
3.4 Complementary Analyses
One explanation for differences in costs between the FDC and the LDC cohort may be differences in medication adherence. To test whether there was empirical support for this mechanism, we divided the cohorts according to their adherence rate in the pre-index period. We measured adherence as the Proportion of Days Covered (PDC) with medication [21]. The PDC is calculated as the ratio of the number of days covered by the prescription fills (based on defined daily doses) divided by the number of days in the specified time interval (365 days). In line with literature on adherence, we defined individuals with PDC ≥ 0.8 as highly adherent, 0.8 > PDC ≥ 0.5 as moderately adherent, and PDC < 0.5 as non-adherent [22]. We repeated the DiD regression for each subgroup.
Another possible mechanism for differences in cost outcomes between the two cohorts may be differences in co-payments. If only one combination product is prescribed, patients may benefit from a reduction in co-payments. Therefore, out-of-pocket spending may be a contributing factor to medical consumption or non-adherence. Moreover, reductions in co-payments could be shifted towards the payer. To test the role of co-payments, we identified patients who were exempt from these due to the hardship clause in German social law. In Germany, co-payments are made only up to an individual annual limit (1% of annual gross income for the chronically ill). If the limit is reached within a calendar year, no additional payments are made for the remainder of the year. For this purpose, our baseline specification (Eq. (1)) was enriched by a dummy variable, indicating co-payment-exemption at index date as follows, whereby \({\text{No copay}}_{i}\) indicates whether an individual was exempt from co-payments at the index date, and \({\beta }_{7}\) is the coefficient of interest:
4 Results
4.1 Matching Results and Descriptive Statistics
In total, 1117 individuals who received an FDC in the post-index period were matched with 1272 individuals who received an LDC in the post-index period. Table 1 shows which second substance was used to supplement metformin in the two cohorts and at which frequency.
In both cohorts, most patients added sitagliptin as a second substance to metformin (85.50% in the FDC cohort and 81.68% in the LDC cohort). Other second substances were dapagliflozin (11.64% in the FDC cohort and 17.30% in the LDC cohort), saxagliptin (2.24% in the FDC cohort and 0.79% in the LDC cohort), and vildagliptin (0.63% in the FDC cohort and 0.24% in the LDC cohort).Footnote 2
Table 2 shows the mean of the covariates before and after applying PSM together with their standardized mean difference. After PSM, none of the covariates were significantly different between the two groups.
In both cohorts, patients were about the same age at the index date, averaging 63.11 years in the FDC cohort and 63.63 years in the LDC cohort. In both cohorts, 30% of the patients were female. The proportion of patients with voluntary insurance status and thus potentially higher income was 15% in the FDC cohort and 17% in the LDC cohort. Total healthcare costs were € 3323.31 in the FDC cohort and € 3599.76 in the LDC cohort. Adherence, expressed as the PDC with medication, was 69% in the FDC cohort and 71% in the LDC cohort in the pre-index period. In total, 74% of the patients were participating in a DMP, and 92% of the physicians were involved in DMPs, regardless of the cohort. Although there were significant differences (d > 0.10) for two Elixhauser groups and one T2D-associated comorbidity group before PSM, no significant differences remained after matching.
4.2 Regression Results
The results of the in-time placebo regression and figures showing pre-index trends for the outcomes for both cohorts are provided in Table S2 and Fig. F1 of OSM. When we artificially set the time of intervention in a placebo regression, the DiD estimators were significant at the five percent level only for T2D-related co-payments and inpatient costs. Our additional graphical inspection of common trends in the pre-index period suggests that the LDC cohort is an adequate control group.
Estimation results from the DiD regression are presented in Table 3. We did not observe any differences in changes in inpatient costs, other costs, or total healthcare costs from the payer perspective between the two cohorts in either year. There was a trend towards lower outpatient costs for the FDC cohort compared to the LDC cohort in the first year of the post-index period (− 0.065, p < 0.10), but the effect was no longer significant in the second year. We also did not observe any significant difference in changes in all-cause pharmaceutical spending between the two cohorts. However, pharmaceutical costs due to T2D significantly increased for the FDC cohort compared to the LDC cohort in year one (0.055, p < 0.01). From the perspective of the patient, we observed a significant decrease in co-payments in the FDC cohort compared to the LDC cohort in both years (− 0.160, p < 0.01; − 0.248, p < 0.01), this decrease was due mostly to antidiabetic prescriptions (− 0.330, p < 0.01; − 0.438, p < 0.01).
4.3 Complementary Analyses
Table 4 shows the results of our subgroup analysis, in which we divided the sample into three groups according to their medication adherence in the pre-index period. We found a significant increase in T2D-related pharmaceutical costs in the FDC cohort compared to the LDC cohort among individuals who were highly adherent in the pre-index period, whereas no significant differences could be found for patients with low or moderate medication adherence. In contrast, we observed a significant decrease in co-payments for antidiabetic medication in the FDC cohort compared to the LDC cohort, regardless of the patients’ level of adherence.
Table 5 presents the regression results after accounting for whether individuals were exempt from co-payments. As expected, if patients were exempt from co-payments, no significant differences in changes in antidiabetic prescription costs were found (–0.027 (0.067); 0.181 (0.154)).
5 Discussion
In this paper, we examined the economic effects of the mode of drug administration on healthcare costs from the perspectives of the payer and the patient. To do so, we compared FDCs with LDCs in the treatment of T2D. To reduce confounding, we implemented a two-stage risk adjustment and combined a matching approach with a DiD regression. We found that compared to receiving an LDC, FDC therapy significantly increased antidiabetic prescription costs in year one. The increase in pharmaceutical costs was, however, observable only in patients with high adherence and in patients who were subject to co-payments. This means the choice of dual therapy made no difference in terms of costs for patients who were already taking their medication infrequently before the index date.
Because we did not find any significant differences in pharmaceutical spending in the second year, the higher costs of FDC treatment seem to matter only in the short run. Moreover, the increase in pharmaceutical spending did not contribute to a significant increase in total healthcare spending for the payer. Hospital costs and other costs were also not significantly different between the two cohorts. From the perspective of the patient, however, we found a significant decrease in all-cause and diabetes-related co-payments for patients treated with FDCs compared to patients treated with LDCs. This was partly to be expected because co-payments generally fall between € 5 and € 10 per package in Germany. This implies that co-payments for FDCs (one package) are about half of the co-payments of LDCs (two separate packages) for each pharmacy refill. In fact, average antidiabetic co-payment was € 40.25 per year for the FDC cohort and € 60.42 per year for the LDC cohort. Therefore, eliminating one co-payment offers a financial advantage to patients treated with FDCs.
Most of the previous literature on this subject has focused exclusively on the USA. Although patients there face particularly high out-of-pocket costs, owing to the large uninsured population and the often burdensome cost-sharing requirements for those who do have coverage [27], these studies have only analyzed costs to the payer [8, 9] or combined costs for the payer and patients [10, 11]. In contrast to the results of our analysis, all four studies reported significantly lower costs for FDC therapy compared to LDC therapy. Two of the four studies found weak indicators of higher pharmaceutical expenditure attributable to FDC treatment [10, 11]. However, in one study, the difference between the two groups was not statistically significant [10], and in the other study, the results were not robust after adjusting for covariates [11].
We provide three possible explanations for the higher pharmaceutical costs in the FDC cohort revealed in this study. First, these might be caused by higher medication adherence due to a reduction in pill burden. If patients take their medication more regularly, refills will naturally increase pharmaceutical spending in the short run. Previous literature suggests that compared to LDC therapy, FDC therapy significantly improves adherence to antidiabetic medication [28]. A higher medication adherence could also explain the observed trend towards higher outpatient costs if patients receiving FDCs visited their physicians more regularly than did patients receiving LDCs. Indeed, in our sample, the average adherence rate of the FDC cohort was 90.37%, indicating that patients were highly adherent in the first year of dual therapy. In contrast, the average adherence rate for metformin was 68.82% and for the second substance 80.33% in the LDC cohort. Counting only days when both substances were available for the patient, this results in a combined adherence rate of 56.39% in the LDC cohort in the first year of the post-index period. In the FDC cohort, 943 patients were highly adherent in the first year of dual therapy with an average PDC of 95.77%, compared with 281 patients in the LDC cohort with an average PDC of 90.04% among those highly adherent. In the long run, however, higher adherence could improve health outcomes and reduce costs of disease progression, resulting in a net reduction of overall health care costs [4].
Second, costs may be driven by pharmaceutical prices. Thus, higher pharmaceutical costs may simply reflect higher product prices if one FDC is more expensive than the sum of the costs of its components. Often, FDCs are launched just before one component loses its exclusivity protection, while the other is still in the early product life cycle. This can keep the cost of the FDC high while the LDC is replaced by cheaper generics. However, this approach does not apply to the analyzed antidiabetic drugs since metformin has long been exposed to generic competition and the added substances lose market exclusivity at the same time. In fact, according to official list prices, the FDCs in question were less expensive than the combined prices for metformin and sitagliptin, which was the most widely prescribed combination in our sample. This is in line with findings from previous studies that reported that FDCs for T2D cost less than the sum of the individual substances [6, 29]. Thus, higher prices are not the reason for increased costs, but have an effect in the opposite direction.
Finally, the increased cost could mark a shift in expenditure from patients to the payer, as we observed decreasing patient co-payments at the same time. Moreover, this explanation is supported by the fact that we did not observe differences in pharmaceutical expenditure when patients were exempt from co-payments. Results from the main DiD regression showed that the absolute increase in antidiabetic pharmaceutical spending in the FDC cohort relative to the LDC cohort was € 24.17, whereas the absolute decrease in antidiabetic co-payments was € 16.88. Therefore, a shift in expenditure from patients to the payer can explain two-thirds of the total increase in antidiabetic pharmaceutical spending. The remaining increase can then be explained by a difference in adherence between the two cohorts.
5.1 Limitations
Limitations must be considered when interpreting our results. First, our identification strategy relies on the assumption that in the absence of FDCs, patients would have been treated with two separate pills. This assumption is not testable, and there is limited information available on why physicians choose to prescribe one type of medical treatment over another for a given patient. Reasons may include preferences, adherence, drug tolerability, costs, or guidelines. Although the results of the placebo test could not reveal zero effects for all outcomes, we believe that the LDC cohort is a suitable control group in our setting. Even before matching, the covariates’ means were quite similar in both cohorts, which indicates that the LDC cohort is appropriate. To minimize the bias due to confounding, we accounted for all observable and unobservable time-invariant differences by combining PSM with DiD estimation.
Moreover, our study investigates a period of only 2 years. However, T2D-associated complications attributable to different treatments might occur in later years. In this context, it would be of interest to include costs of claims due to chronic micro- and macrovascular complications of T2D. In the long run, higher adherence achieved by FDC therapy might postpone or eliminate treatment of comorbidities, resulting in lower healthcare spending. One approach to achieve an extended time horizon could be a Markov model that simulates long-term benefits.
Finally, since diabetes patients may differ from patients with other diseases, for example, in terms of their health behavior and adherence, the results of this study cannot be generalized.
6 Conclusions
We found that, from the payer perspective, antidiabetic FDC therapy increased disease-specific pharmaceutical spending in the first year of dual therapy compared to LDC therapy, but did not lead to differences in total healthcare costs. From the patient perspective, FDC therapy resulted in a decrease in co-payments compared to LDC therapy, a finding that is probably attributable to the elimination of co-payment for one product. We found that the increase in antidiabetic pharmaceutical spending for the payer could be explained in roughly two-thirds by a shift in co-payments to the payer, and the remainder may be explained by a higher medication adherence of the FDC cohort. However, the increase is mitigated by lower prices of the FDC product.
Change history
23 January 2023
Missing Open Access funding information has been added in the Funding Note.
Notes
For historical reasons, higher-income individuals in Germany may choose between statutory health insurance and fully substitutive private health insurance. Those who choose statutory health insurance are classified as being voluntarily insured in the statutory system. Below a certain income threshold, enrolment in statutory health insurance is mandatory.
By law, if new pharmaceuticals do not have an added therapeutic benefit over the current standard of care, they should not lead to annual treatment costs higher than those of the comparator in Germany [23]. The low number of observations for vildagliptin and saxagliptin may be due to the fact that no added benefit was determined for those substances by the Federal Joint Committee (Gemeinsamer Bundesausschuss) [24, 25]. For dapagliflozin, the assessment varied depending on patient subgroups [26].
References
Bangalore S, Shahane A, Parkar S, Messerli FH. Compliance and fixed-dose combination therapy. Curr Hypertens Rep. 2007;9(3):184–9.
Baumgartner A, Drame K, Geutjens S, Airaksinen M. Does the polypill improve patient adherence compared to its individual formulations? A systematic review. Pharmaceutics. 2020. https://doi.org/10.3390/pharmaceutics12020190.
Beall RF, Nickerson JW, Kaplan WA, Attaran A. Is patent “Evergreening” restricting access to medicine/device combination products. PLoS ONE. 2016;11(2): e0148939. https://doi.org/10.1371/journal.pone.0148939.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005:521–30.
Wertheimer AI, Morrison A. Combination drugs: innovation in pharmacotherapy. Pharm Ther. 2002;27(1):44–9.
Leichter SB, Thomas S. Combination medications in diabetes care: an opportunity that merits more attention. Clin Diabetes. 2003;21(4):175–8. https://doi.org/10.2337/diaclin.21.4.175.
Gibson TB, Song X, Alemayehu B, Wang SS, Waddell JL, Bouchard JR, Forma F. Cost sharing, adherence, and health outcomes in patients with diabetes. Am J Manag Care. 2010;16(8):589–600.
Cheong C, Barner JC, Lawson KA, Johnsrud MT. Patient adherence and reimbursement amount for antidiabetic fixed-dose combination products compared with dual therapy among texas medicaid recipients. Clin Ther. 2008;30:1893–907. https://doi.org/10.1016/j.clinthera.2008.10.003.
Barner JC. Adherence to oral antidiabetic agents with pioglitazone and metformin: comparison of fixed-dose combination therapy with monotherapy and loose-dose combination therapy. Clin Ther. 2011;33:1281–8. https://doi.org/10.1016/j.clinthera.2011.07.016.
Williams SA, Buysman EK, Hulbert EM, Bergeson JG, Zhang B, Graham J. Hemoglobin A 1c outcomes and health care resource use in type 2 diabetes mellitus patients treated with combination oral antidiabetic drugs through step therapy and loose-dose and fixed-dose combinations. Manag Care. 2012;21:40–8.
Lokhandwala T, Smith N, Sternhufvud C, Sörstadius E, Lee WC, Mukherjee J. A retrospective study of persistence, adherence, and health economic outcomes of fixed-dose combination vs loose-dose combination of oral anti-diabetes drugs. J Med Econ. 2016;19:203–12. https://doi.org/10.3111/13696998.2015.1109518.
Colombo GL, Rossi E, de Rosa M, Benedetto D, Gaddi AV. Antidiabetic therapy in real practice: indicators for adherence and treatment cost. Patient Prefer Adher. 2012;6:653–61. https://doi.org/10.2147/PPA.S33968.
Techniker Krankenkasse. Unternehmensdaten [cited 24 Jul 2022]. Available from: https://www.tk.de/presse/tk-unternehmensdaten-2051018.
Tönnies T, Röckl S, Hoyer A, Heidemann C, Baumert J, Du Y, et al. Projected number of people with diagnosed Type 2 diabetes in Germany in 2040. Diabet Med. 2019;36(10):1217–25. https://doi.org/10.1111/dme.13902.
Elixhauser A, Steiner C, Harris DR. Comorbidity measures for use with Administrative Data Author (s): Anne Elixhauser, Claudia Steiner, D. Robert Harris and Rosanna M. Coffey Published by: Lippincott Williams & Wilkins Stable. Med Care. 1998;36:8–27. http://www.jstor.org/stable/3766985 Accessed: 26-07.
Kuo RN, Dong Y, Liu J, Chang C, Shau W, Lai MS. Predicting healthcare utilization using a pharmacy-based metric with the WHO's anatomic therapeutic chemical algorithm. Med Care. 2011:1031–9.
von Ferber L, Köster I, Hauner H. Kosten der antihyperglykämischen Behandlung des Diabetes mellitus: Einfluss von Lebensalter, Therapieart und Komplikationsstatus: Ergebnisse der KoDiM-Studie 2001. Med Klin (Munich). 2006;101(5):384–93. https://doi.org/10.1007/s00063-006-1050-8.
Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172(9):1092–7. https://doi.org/10.1093/aje/kwq224.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–61. https://doi.org/10.1002/pst.433.
Rassen JA, Shelat AA, Myers J, Glynn RJ, Rothman KJ, Schneeweiss S. One-to-many prospensity score matching in cohort studies. Pharmacoepidemiol Drug Saf. 2012;21:69–80.
Pharma Quality Alliance. Adherence. PQA adherence measures. 2018 [cited 24 Apr 2020]. Available from: https://www.pqaalliance.org/adherence-measures.
Krousel-Wood M, Holt E, Joyce C, Ruiz R, Dornelles A, Webber LS, et al. Differences in cardiovascular disease risk when antihypertensive medication adherence is assessed by pharmacy fill versus self-report: the Cohort Study of Medication Adherence among Older Adults (CoSMO). J Hypertens. 2015;33(2):412–20. https://doi.org/10.1097/HJH.0000000000000382.
Lauenroth VD, Stargardt T. Pharmaceutical pricing in Germany: how is value determined within the scope of AMNOG. Value Health. 2017;20(7):927–35. https://doi.org/10.1016/j.jval.2017.04.006.
Gemeinsamer Bundesausschuss. Nutzenbewertung nach § 35a SGB V. Nutzenbewertungsverfahren zum Wirkstoff Vildagliptin/Metformin (Diabetes mellitus Typ 2). 2014 [cited 18 Dec 2021]. Available from: https://www.g-ba.de/bewertungsverfahren/nutzenbewertung/53/.
Gemeinsamer Bundesausschuss. Nutzenbewertung nach § 35a SGB V. Nutzenbewertungsverfahren zum Wirkstoff Saxagliptin/Metformin (Neubewertung nach Fristablauf: Diabetes mellitus Typ 2, Mono- oder Kombination mit Insulin). 2016 [cited 18 Dec 2021]. Available from: https://www.g-ba.de/bewertungsverfahren/nutzenbewertung/246/.
Gemeinsamer Bundesausschuss. Nutzenbewertung nach § 35a SGB V. Nutzenbewertungsverfahren zum Wirkstoff Dapagliflozin/Metformin (Erneute Nutzenbewertung § 14: Diabetes mellitus Typ 2). 2019 [cited 18 Dec 2021]. Available from: https://www.g-ba.de/bewertungsverfahren/nutzenbewertung/470/.
Sarnak DO, Squires D, Kuzmak G, Bishop S. Paying for prescription drugs around the world: why is the US an outlier. Issue Brief. 2017;2017:1–14.
Böhm A-K, Schneider U, Aberle J, Stargardt T. Regimen simplification and medication adherence: fixed-dose versus loose-dose combination therapy for type 2 diabetes. PLoS ONE. 2021;16(5): e0250993. https://doi.org/10.1371/journal.pone.0250993.
Bell DSH. Combine and conquer: advantages and disadvantages of fixed-dose combination therapy. Diabetes Obes Metab. 2013;15(4):291–300. https://doi.org/10.1111/dom.12015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. Funding was received from the European Union Framework Programme for Research and Innovation Horizon 2020 under Grant Agreement No. 721402.
Conflict of interest
The authors declare no conflicts of interest.
Availability of data and material
This study uses claims data from a German health insurance company that are subject to strict data protection rules according to SGB V. Therefore, the data cannot be made publicly accessible.
Code availability
The analysis is based on claims data from a German health insurance company that are subject to strict data protection rules according to SGB V. Therefore, the estimation code cannot be made publicly accessible.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
AB and TS developed the idea of the study. AB and TS developed the study design. AB and US contributed to the data preparation. AB performed the statistical analysis. All authors contributed to the interpretation of the results and read and approved the final version of the paper.
Additional information
Anna-Katharina Böhm was a research associate at the University of Hamburg when this work was conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Böhm, AK., Schneider, U. & Stargardt, T. Economic Effects of Fixed-Dose Versus Loose-Dose Combination Therapy for Type 2 Diabetes Patients. Appl Health Econ Health Policy 21, 109–118 (2023). https://doi.org/10.1007/s40258-022-00760-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00760-x