Abstract
The market for new drugs is changing: personalised drugs will increase the heterogeneity in patients’ responses and, possibly, costs. In this context, price regulation will play an increasingly important role. In this article, we argue that personalised medicine opens new scenarios in the relationship between value-based prices, regulation and industry listing strategies. Our focus is on the role of asymmetry of information and competition. We show that, if the firm has more information than the payer on the heterogeneity in patients’ responses and it adopts a profit-maximising listing strategy, the outcome may be independent of the choice of the type of value-based price. In this case, the information advantage that the manufacturer has prevents the payer from using marginal value-based prices to extract part of the surplus. However, in a dynamic setting where competition by a new entrant is possible, the choice of the type of value-based price may matter. We suggest that more research should be devoted to the dynamic analysis of price regulation for personalised medicines.
Similar content being viewed by others
Personalised drugs will increase the heterogeneity in patients’ responses to treatment; this opens new scenarios in the relationship between price regulation and listing strategies by the industry. |
In a static framework, if the effectiveness differential across patients can be observed only by the manufacturer, the main definitions currently proposed for value-based prices lead to the same listing strategy. This is no longer true in a dynamic setting where competition by a new entrant is possible. |
To predict accurately the implications of alternative pricing policies, it is essential for decision makers to adopt a dynamic perspective that takes the role of competition into account. |
1 Introduction
Drug expenditure accounts for about a sixth of health spending across OECD countries and is still on the rise. In Europe, where most health systems are publicly financed [1], pharmaceutical expenditure is under close scrutiny and governments have introduced stringent price regulations [2,3,4], whose desirability is controversial [5]. Another tendency of the pharmaceutical sector that is often discussed is a decrease in the productivity of research and development spending, which in turn may lead to higher prices [6,7,8]. Several possible determinants of this tendency have been discussed. One explanation is that the natural growth in the quantity and quality of products available in the market raises the hurdle for new approvals [9]. Somewhat related to this point is the idea that those problems that had a less complicated technical solution have been addressed first and led to successful innovation, whereas those areas where satisfactory solutions have not been found tend to be more challenging [10]. Some authors claim that stricter regulation of the market, meant to control increases in pharmaceutical expenditure, may negatively affect innovation [11, 12], whereas others [13, 14] argue that the costs for research and development may not fully justify the current level of prices.
The market for new drugs is changing: according to Schork [15], more than 20% of the new molecular entities approved by the US Food and Drug Administration (FDA) can be considered personalised medicine; in oncology, by 2020, 75% of new products will be listed for multiple indications [16]. In a context characterised by heterogeneity in patients’ responses and uncertainty on the outcomes and costs [17], price regulation will play an increasingly important role [18].
Since Gravelle [19], drug price regulation has shifted from cost- to value-based formulas; value-based prices have received significant attention since the Office of Fair Trading recommended their adoption [20], but the precise implementation is still uncertain [21,22,23]. When patients’ responses are heterogeneous, Claxton [24] argues that marginal value based prices (MVBP), i.e. prices based on the value corresponding to lowest health gain among treated patients, (MVBP) should be preferred because they may allow the payer to retain part of the rent. Levaggi and Pertile [25] show that MVBP are superior from the payer’s perspective only if patients are sufficiently homogeneous, whereas only average value-based prices (AVBP) ensure both static and dynamic efficiency, although at the price of higher pharmaceutical expenditure. Finally, indication value-based prices (IVBP) have also been proposed as a relevant alternative in the presence of heterogeneous responses [23, 26, 27].
We identify two issues that, in a framework where personalised medicine plays a prominent role, should receive particular attention: asymmetry of information [28] and competition. Asymmetry of information is important because the manufacturer may have an information advantage vis-à-vis the payer concerning the existence of differences in the effectiveness of the new treatment across groups of patients. Competition may be relevant because the heterogeneity in responses may lead to a segmentation of the market. The example of two cancer drugs that have entered the market in recent years, nivolumab and pembrolizumab, may be interesting in this perspective. Nivolumab was approved by the FDA in March 2015 for the treatment of patients with metastatic squamous non-small cell lung cancer after progression on platinum-based therapy. 7 months later, the drug was also approved for patients with non-squamous non-small cell lung cancer in the same setting.
In October of the same year, the FDA granted approval for pembrolizumab for the treatment of patients with metastatic non-small cell lung cancer who have programmed death-ligand 1 (PD-L1) expression ≥ 50%. Interestingly, in the clinical trial that led to accelerated approval of pembrolizumab by the FDA, the primary efficacy population was restricted to patients with PD-L1 expression ≥ 50%. Hence, the marketing approval of pembrolizumab introduced competition in the market, but this was restricted to a specific sub-group.
We show that, in a context of asymmetry of information, when the manufacturer has more information than the regulator on the heterogeneity in patients’ responses to a specific drug, the three definitions of value-based prices produce the same result in a static short-run context; unlike in the case of symmetric information, they do not allow the payer to extract the producer rent. However, differences may arise in a dynamic and competitive setting where their alternative use may boost or dampen incentives for the manufacturer to reveal the information concerning the heterogeneity in patients’ responses. In this case, thanks to the combination of competition and regulation, MVBP allow payers to extract part of the rent. Surprisingly, little research has been produced so far on how the combination of asymmetric information and competition affects the properties of alternative pricing policies when medicine is personalised.
2 Model
A manufacturer has developed a new active principle that has received marketing approval and has to identify the listing strategy that maximises its profit, defined as the difference between revenues and production costs. Research and development costs are clearly relevant from the manufacturer’s perspective, but they can be ignored for the purposes of the present analysis because, at this stage, they are sunk.
Let the response to treatment be heterogeneous: for n patients, effectiveness (in terms, for example, of quality-adjusted life-years gained) is equal to EH, while for a second group of size (1 − n), it is equal to EL, with EH > EL. Patients can be grouped by some observable elements, such as some genetic characteristics (as in the case of nivolumab and pembrolizumab) or the indication for which the drug is used. An example of the latter situation is bevacizumab, which was originally listed for metastatic colorectal cancer, but was later found to be effective also in the treatment of age-related macular disease.
We consider two different information settings:
-
1.
Symmetric information Both the payer and the firm are informed about the sub-group specific level of effectiveness;
-
2.
Asymmetric information The sub-group specific level of effectiveness is known to the manufacturer only.
To simplify the analysis, we assume that there are no comparators in the market, thus the effectiveness of the new drug also represents its incremental effectiveness. Let λ be the marginal willingness to pay for one unit of effectiveness from the societal perspective. Making the simplifying assumption that there are also no impacts on other non-pharmaceutical healthcare costs, λ will also correspond to the price per unit of effectiveness in a value-based framework. Moreover, λ is also the optimal price that a manufacturer would set if faced with reimbursement decisions based on incremental cost effectiveness and a maximum acceptability threshold equal to λ (see, for example, Levaggi and Pertile [25]).
The profit-maximising manufacturer is only responsible for the definition of the listing strategy, whereas the regulator may use three alternative definitions of value-based prices:
-
MVBP The price is set according to the effectiveness of the marginal patient (i.e. the patient or group of treated patients with the lowest level of effectiveness): it is equal to λEH if the firm asks for listing for the indication for which the drug is most effective (target population n) or to λEL if listing is asked for both sub-groups:
$$\begin{aligned} p_{n}^{m} & = \lambda E_{{\text{H}}} \\ p_{1}^{m} & = \lambda E_{{\text{L}}} \\ \end{aligned}$$ -
AVBP The price is set according to the average effectiveness (across groups of patients) of the new drug. The price will be equal to λEH if the firm asks for listing for the most effective indication (target population n). If listing is asked for both types, the price depends on the weighted average of effectiveness:
$$\begin{aligned} p_{n}^{a} & = \lambda E_{{\text{H}}} \\ p_{1}^{a} & = \lambda E_{{\text{A}}} = \lambda \left( {nE_{{\text{H}}} + \left( {1 - n} \right)E_{{\text{L}}} } \right) \\ \end{aligned}$$ -
IVBP The drug is marketed under two different prices, λEH for the first group of patients and λEL for the second group:
$$\begin{aligned} p_{n}^{i} & = \lambda E_{\text{H}} \\ p_{1 - n}^{i} & = \lambda E_{\text{L}} . \\ \end{aligned}$$
3 Listing Strategies Under Alternative Pricing Schemes
Let us first assume that information is symmetric. The profit-maximising strategies of the manufacturer are derived in the “Appendix” and are presented in Table 1.
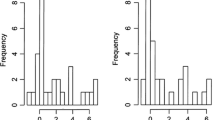
For MVBP, the decision depends on the relative difference in effectiveness and on the size of the two groups as shown in Fig. 1. On the horizontal axis, we measure the number of patients, while on the vertical axis is the price, net of the unit cost of manufacturing the drug, c. The firm chooses between two alternatives: (1) selling only to the first group of patients (n), which leads to a profit corresponding to the area 0ABn; and (2) asking for listing for both indications for a profit equal to 0CE1. The choice depends on the relative size of the two areas. It is noteworthy that in case (1) part of the potential target population (1 − n) has no access to the treatment, even though the treatment would be cost effective. Hawkins and Scott [29] discuss this risk with a specific application to the case of treatments for acute myocardial infarction.
For AVBP, the choice is between listing only for the first group with a profit equal to 0ABn, or for both groups, with a profit equal to 0FG1, which is always greater than the area 0ABn (see the “Appendix”). For IVBP, the manufacturer sells on both markets and makes profits equal to 0ABn + nDE1, which is equal to 0FG1. Therefore, AVBP and IVBP lead to the same solution, both in terms of targeted population and profit. In Fig. 1, with AVBP and IVBP, the manufacturer’s profit coincides with total surplus, meaning that the payer cannot extract any rent. The comparison with MVBP for the case where listing covers the whole population shows that MVBP allow the payer to retain a part of the rent corresponding to area ABDC. Hence, MVBP have a potential advantage in terms of expenditure from the payer’s perspective. However, the risks are a reduced access in the case where it is optimal for the manufacturer to treat only n patients and a loss in dynamic efficiency because of the weaker incentive to invest in future research and development that reduced profit may imply.
Let us now examine the case where the differential effectiveness of the drug is observed only by the manufacturer (asymmetry of information). In this case, it is easy to show that listing strategies for MVBP and AVBP are the same. Because the difference in effectiveness is private information, the industry has to choose between two strategies: (1) targeting only the first group of patients (n) at a price λEH; and (2) asking for listing for both indications, without revealing its private information. In this case, the average observed effectiveness will be equal to EA = nEL + (1 − n)EH and the price will be equal to λEA, i.e. the same price as for AVBP. Therefore, under MVBP, the manufacturer has no interest in disclosing the information concerning the difference in effectiveness between the two sub-groups.
For AVBP and IVBP, the strategic revelation of information has no impact on profit, meaning that the optimal strategy is the same as with symmetric information. Therefore, with asymmetric information, the outcome is the same for all three regulatory policies, with firm profits equal to 0ABn + nDE1. This also implies the loss of the advantage of MVBP in terms of ability for the payer to retain part of the rent, which exists in the case of symmetric information.
4 Discussion and Conclusions
The model presented above shows that, in a static context, most of the common definitions for value-based pricing are surprisingly similar and their different outcomes depend on the information structure. If the firm and the regulator are equally informed on the heterogeneity in patients responses, only under MVBP the outcome in terms of listing, profit for the industry and drug availability may be different. In this case, the industry may choose to list for both indications, or for the most effective one, depending on the effectiveness differential and the relative size of the two populations. Average value- and indication-based prices are equivalent, even though the implications from a policy point of view may be different [30, 31].
Under MVBP, if the industry decides to sell only for one indication, value for money is preserved, but a group of patients will not benefit from its use. This is one of the reasons why the World Health Organization recently criticised value-based prices [32].
In a static context, if information is asymmetric MVBP, AVBP and IVBP are however equivalent in terms of listing, profit and expenditure because even with MVBP the manufacturer has no incentive to reveal the difference in effectiveness. Under MVBP, the best strategy is to present results that pool the effectiveness across the two groups of patients. In this way, it would in fact obtain a price equal to AVBP, hence also the same profit as with AVBP and IVBP. The case of a manufacturer not revealing the differential information on effectiveness may be questioned on ethical and legal grounds; this scenario may be interpreted in terms of incentives in promoting research aimed at assessing heterogeneity across patients, e.g. by undertaking a sub-group analysis in clinical trials.
What would change if, in the framework with asymmetric information, we allow for the possibility that a new competitor enters the market at a subsequent point in time? Let us assume that the drug developed by the potential new entrant has the same characteristics in terms of group-specific effectiveness as the first entrant. If the new drug is launched, it will be accepted for listing and sold at the same price. In this case, a strategy by the incumbent of not disclosing the information concerning the difference in effectiveness between the two groups may not be sustainable in the long term. Let us assume that the incumbent does not disclose the difference in effectiveness. In this case, the new entrant might decide to follow the same strategy and obtain half of the market, or it may disclose the difference in effectiveness between the two groups and enter just one segment. Targeting only the low-effectiveness market is not feasible because the group-specific level of effectiveness (EL) would be lower than the level of effectiveness perceived by the regulator (nEL + (1 − n)EH). What might be both feasible and convenient for the new entrant, under some conditions, is to target only the high effectiveness market. With a price equal to λEH, the new entrant would present a higher level of effectiveness and the same incremental cost-effectiveness ratio ICER (λ) as the incumbent. In this case, it is reasonable to assume that the incumbent would lose the high-effectiveness market. By backward induction, the threat of a new entry to the market makes the decision not to disclose the difference in effectiveness less appealing in a framework with asymmetric information, even when the pricing policy is based on MVBP. Hence, competition may enable the payer to extract part of the rent from the manufacturer, as was the case in the situation with symmetric information in a static setting.
The example of nivolumab and pembrolizumab presented in the Introduction may be also interpreted from this perspective. Pembrolizumab, which entered the market for the second-line treatment of non-small cell lung cancer after nivolumab, has been approved only for the sub-group of patients with PD-L1 expression ≥ 50%. Although no direct comparison is available, results from the registration trials seem to point in the direction of an advantage in terms of effectiveness in this sub-group of patients for pembrolizumab, for which the response rate is 41% [33]. The response rate for nivolumab in the corresponding registration trial, which includes also subjects with values of PD-L1 < 50%, was 20% [34]. It cannot be ruled out that nivolumab is also more effective for the sub-group of patients with high levels of PD-L1. For example, using data from several trials, [35] an absolute difference of 16.4% was found in the overall response rate in favour of PD-L1-positive vs. PD-L1-negative patients treated with nivolumab. It is therefore possible that for nivolumab the manufacturer preferred a broader indication and potentially a larger market, despite a possibly lower price.
Our analysis shows that the framework in which the implications of alternative pricing policies are considered may have a substantial impact on the conclusions. The additional complexity implied by the ongoing development of personalised medicine, makes this result even more relevant. Very little research exists on the dynamic implications of different value-based price schemes in the context of personalised medicine. We believe that this avenue may set the agenda for the future research on pharmaceutical price regulation.
References
OECD. Health at a glance 2013: OECD indicators. Paris: OECD Publishing; 2013.
Carone G, Schwierz C, Xavier A. Cost-containment policies in public pharmaceutical spending in the EU. MPRA Paper:1-67. 2012. https://doi.org/10.2765/27111
Panos K, Taylor D, Manning J, Carr M. Implementing value-based pricing for pharmaceuticals in the UK. 2020Health; 2010.
OECD. Health at a glance 2011. Paris: OECD indicators; 2011.
Wettermark B, Godman B, Jacobsson B, Haaijer-Ruskamp F. Soft regulations in pharmaceutical policymaking: an overview of current approaches and their consequences. Appl Health Econ Health Policy. 2009;7:137–47.
Kleinke JD. The price of progress: prescription drugs in the health care market. Health Aff. 2001;20:43–60.
DiMasi JA, Hansen RW, Grabowski HG. The price of innovation: new estimates of drug development costs. J Health Econ. 2003;22:151–85.
DiMasi JA, Grabowski HG, Hansen RW. Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ. 2016;47:20–33.
Scannell JW, Blanckley A, Boldon H, Warrington B. Diagnosing the decline in pharmaceutical R&D efficiency. Nat Rev Drug Discov. 2012. https://doi.org/10.1038/nrd3681.
Schnee JE. R&D strategy in the US pharmaceutical industry. Res Policy. 1979;8(4):364–382. https://doi.org/10.1016/0048-7333(79)90003-9.
Danzon PM, Chao L-W. Does regulation drive out competition in pharmaceutical markets? J Law Econ. 2000;43:311–57.
Bardey D, Bommier A, Jullien B. Retail price regulation and innovation: reference pricing in the pharmaceutical industry. J Health Econ. 2010;29:303–16.
Yu N, Helms Z, Bach PB. R&D costs for pharmaceutical companies do not explain elevated US drug prices. Health affairs blog. 2017. Retreived 28 November 2019. https://www.healthaffairs.org/do/10.1377/hblog20170307.059036/full/.
Walton SM, Basu A, Mullahy J, Hong S, Schumock GT. Measuring the value of pharmaceuticals in the US health system. Pharmacoeconomics. 2017;35:1–4.
Schork N. Personalized medicine: time for one-person trials. Nature. 2015;520:609–11.
Aitken M, Blansett L, Mawrie R. Developments in cancer treatments, market dynamics, patient access and value. Global oncology trend report. IMS Institute; 2015. P. 1–46.
Davis JC, Furstenthal L, Desai AA, Norris T, Sutaria S, Fleming E, et al. The microeconomics of personalized medicine: today’s challenge and tomorrow’s promise. Nat Rev Drug Discov. 2009;8:279–81.
Eichler HG, Abadie E, Breckenridge A, Flamion B, Gustafsson LL, Leufkens H, et al. Bridging the efficacy-effectiveness gap: a regulator’s perspective on addressing variability of drug response. Nat Rev Drug Discov. 2011;10:495–506.
Gravelle HSE. Ex post value reimbursement for pharmaceuticals. Med Decis Mak. 1998;18:S27–38.
Office of Fair Trade. The pharmaceutical price regulation scheme: an OFT market study. OFT: London; 2007.
Sussex J, Towse A, Devlin N. Operationalizing value-based pricing of medicines. Pharmacoeconomics. 2013;31:1–10.
Claxton K, Sculpher M, Carroll S. Value-based pricing for pharmaceuticals: its role, specification and prospects in a newly devolved NHS. CHE Research Paper 60. University of York; 2011, P. 1–27. https://www.york.ac.uk/media/che/documents/papers/researchpapers/CHERP60_value_based_pricing_for_pharmaceuticals.pdf.
Kaltenboeck A, Bach PB. Value-based pricing for drugs theme and variations. JAMA. 2018;319:2165–6.
Claxton K. OFT, VBP: QED? Health Econ. 2007;16:545–58.
Levaggi R, Pertile P. Pricing policies when patients are heterogeneous: a welfare analysis. Working Papers 17/2016. University of Verona, Department of Economics; 2016.
Chandra A, Garthwaite C. The economics of indication-based drug pricing. N Engl J Med. 2017;377:103–6.
Bach PB. Indication-specific pricing for cancer drugs. JAMA. 2014;312:1629–30.
Ghislandi S, Kuhn M. Asymmetric information in the regulation of the access to markets. Department of Economics Working Paper Series, 219. Vienna: WU Vienna University of Economics and Business. P. 1–33. https://www.wu.ac.at/economics/forschung/wp/.
Hawkins N, Scott DA. Reimbursement and value-based pricing: stratified cost-effectiveness analysis may not be the last word. Health Econ. 2011;20:688–98.
Neri M, Towse A, Garau M. Multi-indication pricing (MIP): practical solutions and steps to move forward. Briefings 002084. Office of Health Economics; 2018. https://www.ohe.org/publications/multi-indication-pricing-mip-practical-solutionsand-steps-move-forward.
Towse A, Cole A, Zamora B. The debate on indication-based pricing in the U.S. and five major European countries. OHE consulting report. 2018. https://www.ohe.org/system/files/private/publications/OHE%20IBP%20Final%20Report%20May%202018%20%28Revised%29.pdf.
WHO. Pricing of cancer medicines and its impacts: a comprehensive technical report for the World Health Assembly Resolution 70.12: operative paragraph 2.9 on pricing approaches and their impacts on availability and affordability of medicines for the prevention and treatment of cancer. World Health Organization; 2018. https://apps.who.int/iris/handle/10665/277190.
Sul J, Blumenthal GM, Jiang X, He K, Keegan P, Pazdur R. FDA approval summary: pembrolizumab for the treatment of patients with metastatic non-small cell lung cancer whose tumors express programmed death-ligand 1. Oncologist. 2016;21:643–50.
Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35. https://doi.org/10.1056/NEJMoa1504627.
Carbognin L, Pilotto S, Milella M, et al. Differential activity of nivolumab, pembrolizumab and MPDL3280A according to the tumor expression of programmed death-ligand-1 (PD-L1): sensitivity analysis of trials in melanoma, lung and genitourinary cancers. PLoS One. 2015;10(6):e0130142. https://doi.org/10.1371/journal.pone.0130142.
Acknowledgements
The authors would like to thank the reviewers and the Editor for their helpful comments. The usual disclaimer applies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of Interest
Rosella Levaggi and Paolo Pertile have no conflicts of interest that are directly relevant to the content of this article.
Author Contributions
Both authors contributed to the development of the model described in Sect. 2 and to its draft. Rosella Levaggi wrote the first draft of the introduction while Paolo Pertile wrote the first draft of the Discussion and Conclusions. Both authors commented on previous versions of the manuscript. Both authors read and approved the final manuscript.
Appendix
Appendix
1.1 Marginal Value-Based Prices
Let us assume that the firm is about to list a drug that has been approved so that any sunk cost for its discovery has already been borne. If the firm decides to list only for the patients with the highest effectiveness, the price is \(\lambda E_{\text{H}}\) and the corresponding profit \(\varPi_{n}^{m} = \left( {\lambda E_{\text{H}} - c} \right)n\). If the firm asks for listing for both types of patients, price and profit are respectively, λEL and \(\varPi_{1}^{m} = \left( {\lambda E_{\text{L}} - c} \right)\). The firm chooses the alternative that allows the maximization of the profit by comparing,
with,
We can write these conditions in terms of EH for choosing the first alternative:
Hence, the maximum profit is,
1.2 Average Value-Based Prices
If the firm decides to list only for the patients with the highest effectiveness, the price will be equal to \(\lambda E_{\text{H}}\) and the profit will be \(\varPi_{n}^{a} = \left( {\lambda E_{\text{H}} - c} \right)n\). If the firm asks for listing for both types of patients, the price is \(\lambda E_{\text{A}} = \lambda \left( {nE_{\text{H}} + \left( {1 - n} \right)E_{\text{L}} } \right)\) and the profit is \(\varPi_{1}^{a} = \left( {\lambda E_{\text{A}} - c} \right)\). The firm chooses the alternative that allows the maximization of profit by comparing,
with,
so that,
which can be written as,
This proves that under average value-based prices, listing of both sub-groups is always preferred by the manufacturer.
Rights and permissions
About this article
Cite this article
Levaggi, R., Pertile, P. Value-Based Pricing Alternatives for Personalised Drugs: Implications of Asymmetric Information and Competition. Appl Health Econ Health Policy 18, 357–362 (2020). https://doi.org/10.1007/s40258-019-00541-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-019-00541-z