Abstract
Background
There is obscurity regarding how US hospitals determine patients’ charges. Whether insurance status influences a patient’s hospital charge has not been explored.
Objective
The objective of this study was to determine whether hospitals charge patients differently based on their insurance status.
Methods
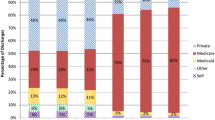
This was an analysis of the Florida Hospital Inpatient Data File for fiscal years 2011–2012 (N = 4.7 million). Multivariable regression analysis was used to adjust for patients’ age, sex, length of stay, priority of admission, principal ICD-9-CM diagnosis, and All Payer Refined Diagnosis-Related Group subdivided by Severity of Illness subclass. Hospital fixed effects were included to account for differences in hospitals’ markups.
Results
Compared with those with no insurance, patients with private insurance received hospital bills that were an average of 10.7% higher and patients with Medicare received bills that were an average of 8.9% higher. The impact of Medicaid coverage was imprecisely estimated, but the magnitude of the point-estimate was consistent with 3.5% higher charges to Medicaid patients, relative to the uninsured.
Conclusion
Conditional on patient characteristics, length of stay, and expected intensity of resource utilization, patients with private insurance and patients with Medicare were charged more (before discounting) than their uninsured counterparts within the same hospital.
Similar content being viewed by others
References
NHE Fact Sheet. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html. Accessed Dec 28, 2015.
Muhlestein D. What types of hospitals have high charge-to-reimbursement ratios? Health Affairs Blog; 2013.
Ginsburg PB. Wide variation in hospital and physician payment rates evidence of provider market power. Center for Studying Health System Change; 2010.
Morrisey MA. Cost shifting in health care: separating evidence from rhetoric. American Enterprise Institute; 1994.
Tompkins CP, Altman SH, Eilat E. The precarious pricing system for hospital services. Health Affairs. 2006;25(1):45–56.
United States Government Accountability Office. Meaningful price information is difficult for consumers to obtain prior to receiving care. GAO-11-791. http://www.gao.gov/assets/590/585400.pdf. Accessed Dec 29, 2015.
Cauchi R, Valverde H. Uncovering hospital charges: hospitals are reporting their rates for various procedures in an effort to satisfy those who want more transparency in health care costs. State Legis. 2013;39(8):28.
Public Workshop: Examining Health Care Competition. http://www.justice.gov/atr/events/public-workshop-examining-health-care-competition. Accessed Dec 29, 2015.
Carter GM, David Rumpel J. Payment rates for unusual medicare hospital cases. RAND Corporation; 1992.
The value of health insurance: few of the uninsured have adequate resources to pay potential hospital bills: assistant secretary for planning and evaluation. U.S. Department of Health and Human Services; 2011.
Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84(10):1605–8.
Lyon SM, Benson NM, Cooke CR, Iwashyna TJ, Ratcliffe SJ, Kahn JM. The effect of insurance status on mortality and procedural use in critically ill patients. Am J Respir Critical Care Med. 2011;184(7):809–15.
Fowler RA, Lori-Anne Noyahr J, Thornton D, Pinto R, Kahn JM, Adhikari NKJ, Dodek PM, et al. An official American Thoracic Society systematic review: the association between health insurance status and access, care delivery, and outcomes for patients who are critically ill. Am J Respir Crit Care Med. 2010;181(9):1003–11.
Fact Sheet: Common Types of Health Care Fraud. Centers for Medicare and Medicaid Services, July 2016. https://www.cms.gov/Medicare-Medicaid-Coordination/Fraud-Prevention/Medicaid-Integrity-Education/Downloads/fwa-factsheet.pdf. Accessed Nov 12, 2016.
3M™ APR DRG Classification System and 3M™ APR DRG Software. http://multimedia.3m.com/mws/media/478415O/3m-apr-drg-fact-sheet.pdf. Accessed Dec 29, 2015.
Ginsburg PB, Sloan FA. Hospital cost shifting. N Engl J Med. 1984;310(14):893–8.
White C. Contrary to cost-shift theory, lower Medicare hospital payment rates for inpatient care lead to lower private payment rates. Health Affairs. 2013;32(5):935–43.
Fox W, Pickering J. Hospital and physician cost shift: payment level comparison of Medicare. Medicaid, and commercial payers, Milliman; 2008.
Melnick GA, Fonkych K. Hospital pricing and the uninsured: do the uninsured pay higher prices? Health Affairs. 2008;27(2):w116–22.
Adamache KW, Sloan FA. Competition between non-profit and for-profit health insurers. J Health Econ. 1983;2(3):225–43.
Ginsburg PB. Can hospitals and physicians shift the effects of cuts in Medicare reimbursement to private payers? Health Affairs. 2003;W3:472–9.
Maeda JL, Mosher HR, Marder WD, Karaca Z, Friedman BS, Wong HS. Variation in hospital inpatient prices across small geographic areas. Am J Manag Care. 2013;20(11):907–16.
Bai G, Anderson GF. US hospitals are still using chargemaster markups to maximize revenues. Health Affairs. 2016;35(9):1658–64.
Frakt Austin B. How much do hospitals cost shift? A review of the evidence. Milbank Q. 2011;89(1):90–130.
Zammitti EP, Cohen RA, Martinez ME. Health insurance coverage: early release of estimates from the National Health Interview Survey, January–June 2016. National Center for Health Statistics; 2016. http://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201611.pdf. Accessed Nov 21, 2016.
Epstein AM, Stern RS, Tognetti J, Begg CB, Hartley RM, Cumella E Jr, Ayanian JZ. The association of patients’ socioeconomic characteristics with the length of hospital stay and hospital charges within diagnosis-related groups. N Engl J Med. 1988;318(24):1579–85.
Epstein AM, Stern RS, Weissman JS. Do the poor cost more? A multihospital study of patients’ socioeconomic status and use of hospital resources. N Engl J Med. 1990;322(16):1122–8.
Reinhardt UE. The pricing of US hospital services: chaos behind a veil of secrecy. Health Affairs. 2006;25(1):57–69.
Bai G, Anderson GF. Extreme markup: the fifty US hospitals with the highest charge-to-cost ratios. Health Affairs. 2015;34(6):922–8.
Acknowledgements
We thank the Florida Center for Health Information and Policy Analysis for assistance obtaining the data used in this study. The Florida Agency for Health Care Administration disclaims responsibility for any analysis, interpretations, or conclusions created as a result of the data they provided.
Author contribution
Woodworth contributed to the conception and design of the study, and performed all statistical analyses. All authors contributed to the interpretation of the results and assisted in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by a Grant from the Agency for Healthcare Research and Quality (AHRQ) through the Quality, Safety, and Comparative Effectiveness Research Training (QSCERT) Program (T32HS022236).
Conflict of interest
Woodworth, Romano, and Holmes declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Woodworth, L., Romano, P.S. & Holmes, J.F. Does Insurance Status Influence a Patient’s Hospital Charge?. Appl Health Econ Health Policy 15, 353–362 (2017). https://doi.org/10.1007/s40258-017-0308-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0308-z