Abstract
Background
Hundreds of thousands of surgical arthroscopy procedures are performed annually in the United States (US) based on MRI findings. There are situations where these MRI findings are equivocal or indeterminate and because of this clinicians commonly perform the arthroscopy in order not to miss pathology. Recently, a less invasive needle arthroscopy system has been introduced that is commonly performed in the physician office setting and that may help improve the accuracy of diagnostic findings. This in turn may prevent unnecessary follow-on arthroscopy procedures from being performed.
Objective
The purpose of this analysis is to determine whether the in-office diagnostic needle arthroscopy system can provide cost savings by reducing unnecessary follow on arthroscopy procedures.
Methods
Data obtained from a recent trial and from a systematic review were used in comparing the accuracy of MRI and VisionScope needle arthroscopy (VSI) with standard arthroscopy (gold standard). The resultant false positive and false negative findings were then used to evaluate the costs of follow-on procedures. These differences were then modeled for the US patient population diagnosed and treated for meniscal knee pathology (most common disorder) to determine if a technology such as VSI could save the US healthcare system money. Data on surgical arthroscopy procedures in the US for meniscal knee pathology were used (calendar year [CY] 2010). The costs of performing diagnostic and surgical arthroscopy procedures (using CY 2013 Medicare reimbursement amounts), costs associated with false negative findings, and the costs for treating associated complications arising from diagnostic and therapeutic arthroscopy procedures were assessed.
Results
In patients presenting with medial meniscal pathology (International Classification of Diseases, 9th edition, Clinical Modification [ICD9CM] diagnosis 836.0), VSI in place of MRI (standard of care) resulted in a net cost savings to the US system of US$115–US$177 million (CY 2013) (use of systematic review and study data, respectively). In patients presenting with lateral meniscus pathology (ICD9CM 836.1), VSI in place of MRI cost the healthcare system an additional US$14–US$97 million (CY 2013). Overall aggregate savings for meniscal (lateral plus medial) pathology were identified in representative care models along with more appropriate care as fewer patients were exposed to higher risk surgical procedures.
Conclusions
Since in-office arthroscopy is significantly more accurate, patients can be treated more appropriately and the US healthcare system can save money, most especially in medial meniscal pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diagnostic accuracy is improved with in-office arthroscopy using VisionScope imaging (VSI) versus MRI. |
Fewer patients would go on to more invasive surgical procedures if VSI were used, and fewer patients would be exposed to unnecessary care. |
With less unnecessary care, there is the potential for significant cost savings in using VSI. |
1 Background
Magnetic resonance imaging (MRI) plus clinical evaluation is the standard of care (hereafter referred to as MRI) for assessing soft tissue injuries in the knee joint. However, MRI assessment has drawbacks: a high incidence of false positive (FP) (lesion shown to be present when in actuality there is none) and false negative (FN) (lesion shown to be negative when there is one) findings. These FPs and FNs occur most commonly with deep intra-articular structures such as the medial and lateral meniscus or cartilage of the knee. In the United States (US), for the year 2010, 502,000 surgical arthroscopic procedures were performed on the medial meniscus/cartilage of the knee, and 192,000 for the lateral meniscus/cartilage of the knee [1] (Table 1). Both of these procedures, combined, represent close to 50 % of all surgical arthroscopic procedures (Table 1). Medial and lateral meniscal tears are commonly the hardest pathology to diagnose accurately [2]. Further, clinicians view MRI findings with skepticism based on their underestimating intra-articular defects [3–5]. Due to equivocal findings with MRI, physicians commonly perform surgical arthroscopy. This is reflected in the US statistics that show 99 % of arthroscopies performed are therapeutic in nature [6]. An alternative diagnostic modality might mitigate some of the above issues.
Small bore (needle arthroscopy) has been available for a number of years and its efficacy is well established. The results reported in the literature have demonstrated similar accuracy to standard, larger sized arthroscopes [7–17]. A newer and smaller bore arthroscope with improved optics and visualization, the VisionScope system (VSI), was recently introduced into the office setting for pre- and post-operative imaging and diagnostics. The key component of this system is a proprietary 1.4-mm-diameter semi-rigid/fiber lens with 2-mm portal/trocar endoscope system, a size comparable to arthrocentesis needles. This is accomplished without having to extend the knee joint with fluid (for purposes of visualization) through a second access site.
To date, no one has examined the economic effect of a more widespread use of office-based needle arthroscopy. The purpose of this analysis is to use the findings from a recent comparison study of VSI and MRI compared with standard arthroscopy (used as the gold standard) and; of published meta-analysis MRI findings, [18] in examining the overall costs to the US healthcare system. The hypothesis is that with the use of the VSI office arthroscopy system, considerable savings to the healthcare system can be realized and the quality of care can be improved.
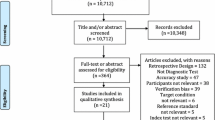
2 Methods
2.1 Data Sources and Methods
The National Survey Ambulatory Surgery 2010 (NSAS) [1], conducted periodically by the National Center for Health Statistics (NCHS), covers ambulatory surgery procedures performed in hospitals and freestanding ambulatory surgery centers in the US. The hospital universe includes noninstitutional hospitals exclusive of Federal, military, and Department of Veterans Affairs hospitals.
Sensitivity and specificity estimates for VSI and MRI plus clinical diagnoses were derived from a recent study comparing both with standard arthroscopy (the gold standard) (see electronic supplementary material [ESM], Appendix 1) (defined as the community setting case) and from published systematic reviews comparing MRI with standard arthroscopy [19] (defined as the academic medical center setting case).
Costs for diagnostic and treatment paradigms using current methods and for the VSI were Medicare’s 2013 national average actual reimbursement rates for each procedure (unless otherwise specified). Costs were calculated for both MRI and VSI positive and negative findings.
Estimates for complications (morbidity and mortality) from each diagnostic method and for treatment were derived from the literature.
Estimates of the number of diagnoses which were considered true positives (TPs), true negatives (TNs), FPs and FNs for both VSI and MRI, plus clinical diagnoses were made by using the actual number of procedures performed for both medial and lateral meniscus tears, found in Table 1. Since the standard of care for diagnosis of knee pathology is considered MRI plus clinical diagnosis, the number of procedures performed in 2010 for medial and lateral meniscus procedures were fed into a sensitivity, specificity, positive and negative predictive value table using the values obtained from the study found in Appendix 1 and from systematic review findings, also in Appendix 1 (see ESM). Further, since the number of procedures in 2010 could be considered a combination of TP and FP findings, FN and TN findings were derived from these amounts. These were then used as the base case and are identified in Table 2 (MRI medial meniscus) and Table 3 (MRI lateral meniscus). Using these values one could then calculate the total number of negative findings from MRI and consequently all diagnostics performed (negative diagnostics + positive diagnostics) that yielded the actual CY 2010 surgical arthroscopy procedure number. From these findings, the number of cases which actually had either medial or lateral meniscus pathology (i.e., sum of TPs and FNs—pathology that should be positive for a lesion; ‘actual number’) was derived. This ‘actual number’ was then fed into a similar table using VSI as the diagnostic. The ‘actual number’ was used to derive TPs, FPs, TNs, and FNs for VSI, based on study-derived VSI sensitivity and specificity values (Appendix 1, ESM). Again, these numbers were used to calculate all the diagnostics performed to yield a surgical number (hypothetical VSI number of surgeries (TPs + FPs) if one was to use VSI in place of MRI (Table 4 [VSI medical meniscus] and Table 5 [VSI lateral meniscus]). All diagnostic and therapeutic numbers were then fed into a cost model to determine the overall effect on all costs (of diagnostics plus resultant treatments) using either MRI or VSI diagnostics on the US healthcare system.
2.2 Direct Cost Calculation
The following diagnostic and treatment paradigms were used for both current (MRI) and VSI (all assumed to be performed in either the physician office or outpatient settings): International Classification of Diseases, 9th edition, Clinical Modification (ICD9CM) 836.0 (diagnosis of tear of medial cartilage or meniscus of knee); ICD9CM 836.1 (diagnosis tear of lateral cartilage or meniscus of knee). The costs for these diagnoses and treatment, including complications (morbidity and mortality) arising from the procedure, were assessed over an acute time period (from initial diagnosis, through the follow-up visit post-procedure) in the following manner (using CY 2013 Medicare reimbursement information).
MRI: orthopedic consult (using current procedural terminology [CPT] 99203—evaluation and management [E&M] for a new patient) + X-ray (CPT 73560—radiologic exam) + MRI (CPT 73721—MRI of any lower extremity joint—global) + MRI (CPT 73721-26—MRI any lower extremity joint—professional) + arthrocentesis (CPT 20610—aspiration or injection of a major joint at 10 % of time [20]) + Hospital Outpatient Arthroscopy (assumes a meniscectomy was performed when a patient was diagnosed for pathology [i.e., a TP or FP]—CPT 29881) + follow-up orthopedic consult (CPT 99213—E&M for existing patient).
VSI: orthopedic consult (using CPT 99203—E&M for a new patient) + X-ray (CPT 73560—radiologic exam) + VSI (CPT 29870 nonfacility) + Hospital Outpatient Arthroscopy (assumes a meniscectomy was performed when a patient was diagnosed for pathology [i.e., a TP or FP]—CPT 29881) + follow-up orthopedic consult (CPT 99213—E&M for existing patient).
The costs for each of the above services/procedures, using CY 2013 Medicare reimbursement data (Table 6), include the following:
Overlay of the incidence and costs for complications associated with each procedure above and treated in the appropriate care setting. The complications evaluated were those seen with standard arthroscopy. The complication rates used for knee arthroscopy were derived from a recent article (2011) appearing in the Journal of Bone and Joint Surgery [21] (Table 7). Since the VSI disposable arthroscope is similar in size to needles used in arthrocentesis, the complication rates applied to the costs of diagnostic knee arthroscopy using VSI were derived from the literature based on the types of complications seen with arthrocentesis (Table 7), or from the assumption that since only one portal is necessary in VSI, complications were cut in half over standard arthroscopy (one portal versus two portals).
FN results on MRI and VSI were assumed to be treated first via physical therapy (PT) (CPT 97110, twice per week for 6 weeks [22] and at an adherence rate/attendance of 86 % [23] of these visits or 10.3 visits [12 × 0.86]) and then via an arthroscopic procedure based on crossover rates from randomized controlled trials [22, 24]. The PT sessions as per above are consistent with how private payers such as CIGNA cover and pay for PT [25]. This cross over from PT to a therapeutic arthroscopy procedure was estimated at 30 % for the knee [22]. If PT crossed over to a therapeutic procedure, the procedural codes used for the knee were CPT 29881, APC 0041, and CPT 99213. PT was assumed to occur for 85 % of patients, with an assumption that 15 % did not have insurance [26] and that lack of insurance was a predisposing factor to not undergoing PT [27]. The number of sessions (10.3 over a 6-week period) was reflective of this [23].
TPs and FPs on MRI and VSI were assumed to undergo PT after a surgical arthroscopy procedure, and FN crossover (FN CO) patients who underwent surgery were also assumed to undergo PT with the same number of PT sessions as per above.
This analysis reflects the direct costs of care (i.e., using a third-party payer perspective [Medicare]) and does not examine the societal or individual costs incurred.
3 Results
3.1 Knee Arthroscopies Analysis of MRI versus VSI
3.1.1 For Medial Meniscus
Based on the sensitivity, specificity, and positive and negative predictive values obtained from the study found in Appendix 1 (ESM), it was found that in order for 502,200 surgical arthroscopic procedures to be performed (both TP [395,734] and FP [106,466] MRI findings), 258,250 negative findings for MRI also resulted (both FNs and TNs). The incidence of positive and negative MRI diagnosis and resultant treatment of this condition therefore totaled 760,450 (502,200 + 258,250) patients. Expressed differently, 760,450 patients underwent an MRI in order to perform these 502,200 surgical arthroscopy procedures. Further, it was shown that those patients who actually had disease (i.e., TP + FN) totaled 486,757 patients (Table 2). This amount of actual disease was then fed into the VSI model to compute numeric values for TP, FP, TN, and FN (Table 4) based on the sensitivities and specificities as found in the study appearing in Appendix 1 (ESM). This resulted in the following values calculated: 459,499 TPs + 9,032 FPs = 468,531, which equals the number of likely surgical procedures that would be performed based on positive VSI findings and 291,919 negative findings (both FN and TN). Thus, the total number of positive and negative VSI findings and resultant treatment totaled 760,450 patients (468,531 + 291,919). Expressed differently, 760,450 patients underwent a VSI diagnostic arthroscopy in order to perform 468,531 surgical arthroscopy procedures.
3.1.2 For Lateral Meniscus
Based on the sensitivity, specificity, and positive and negative predictive values obtained from the study found in Appendix 1 (ESM), it was found that in order for 192,177 surgical arthroscopic procedures to be performed (both TP [132,602] and FP [59,575] MRI findings), 444,677 negative findings for MRI also resulted (both FNs and TNs). The incidence of positive and negative MRI diagnosis and resultant treatment of this condition therefore totaled 636,854 (192,177 + 444,667) patients. Expressed differently, 636,854 patients underwent an MRI in order to perform these 192,177 surgical arthroscopy procedures. Further, it was shown that those patients who actually had disease (i.e., TP + FN) totaled 198,804 patients (Table 3). This amount of actual disease was then fed into the VSI model to compute values for TP, FP, TN and FN (Table 5) based on the sensitivities and specificities as found in the study appearing in Appendix 1 (ESM). This resulted in the following values calculated: 179,918 TPs + 18,886 FPs = 198,804, which equals the number of likely surgical procedures that would be performed based on VSI findings and 438,051 negative VSI findings (both FN and TN). Thus the total number of positive and negative VSI findings totaled 636,854 patients (198,804 + 438,051).
3.2 Cost Analysis
For medial meniscal tears, the overall cost savings to the healthcare system equated to US$177 million (Table 8). The main reason for these savings was that significantly fewer patients with VSI were exposed to follow-on surgical treatment from the FP findings seen with MRI. For lateral meniscal tears, the use of VSI versus MRI cost the healthcare system marginally more (US$14 million) (Table 8). However, it should be noted that more people were treated appropriately with VSI, as VSI resulted in improved accuracy of diagnosis versus MRI. Thus, these additional costs should be considered in the light of more appropriate care being provided. (For more details on the costs see Appendices 2 and 3 in the ESM). Figures 1, 2, 3 and 4 graphically depict cost of diagnosis and treatment).
Cohort of patients undergoing diagnosis and therapy for a medial meniscus tear—VSI cohort. Does not include costs of complications. APC Ambulatory Payment Classification, CPT Current Procedural Terminology, FN false negative, NPV negative predictive values, PPV positive predictive values, PT physical therapy, TP true positive, VSI VisionScope imaging
Cohort of patients undergoing diagnosis and therapy for a medial meniscus tear—MRI cohort. Does not include costs of complications. APC Ambulatory Payment Classification, CPT Current Procedural Terminology, FN false negative, NPV negative predictive values, PPV positive predictive values, PT physical therapy, TP true positive, VSI VisionScope imaging
Cohort of patients undergoing diagnosis and therapy for a lateral meniscus tear—VSI cohort. Does not include costs of complications. APC Ambulatory Payment Classification, CPT Current Procedural Terminology, FN false negative, NPV negative predictive values, PPV positive predictive values, PT physical therapy, TP true positive, VSI VisionScope imaging
Cohort of patients undergoing diagnosis and therapy for a lateral meniscus tear—MRI cohort. Does not include costs of complications. APC Ambulatory Payment Classification, CPT Current Procedural Terminology, FN false negative, NPV negative predictive values, PPV positive predictive values, PT physical therapy, TP true positive, VSI VisionScope imaging
In examining the overall cost of VSI versus MRI and using systematic review findings (defined as the ‘academic setting’) for TP, FP, FN, and TN, it was found that overall savings to the system in using VSI was US$115 million for medial meniscus tears (Table 8). Additionally, using systematic review data for MRI in assessing lateral meniscus tears, it was found that using VSI in lieu of MRI cost the healthcare system an additional US$97 million (Table 8). Again it should be noted that based on the improved accuracy of the VSI versus MRI, the additional cost in using VSI in place of MRI was mainly for more appropriate care.
A sensitivity analysis was performed on the medial and lateral meniscus findings (varying the sensitivity and specificity of MRI findings of the ‘academic setting’ or systematic review findings) while keeping the VSI sensitivity and specificity findings constant. These were then fed into the cost models (as shown in Appendix 2 [for medial meniscus] and Appendix 3 [for lateral meniscus] in the ESM). The costs findings for the medial meniscus analysis can be seen in Table 9. What these findings show is that with improved specificity (i.e., a lower incidence of FP findings), MRI can be cost saving versus VSI. What the Table 9 sensitivity analysis also demonstrates is that with improved specificity and decreased sensitivity (i.e., fewer FPs but an increase in FNs) for MRI, cost savings are greatest with MRI. Additionally, a sensitivity analysis was performed using ‘community setting’ medial meniscus data (i.e., study data) and examined the following variables that could affect cost savings: costs of the procedures ±20 %; number of procedures performed annually ±20 %; sensitivity ±10 % while keeping specificity constant; specificity ±10 % while keeping sensitivity constant; and examining the same incidence of complications between the VSI and MRI treatment paths. This analysis is shown in a tornado plot (Fig. 5). What the tornado plot shows is that the cost savings are most affected by a ±10 % variation of the sensitivity of the MRI test from the study value of 81 % (holding specificity constant at the 61 % study value). What the tornado plot also confirms is that the cost savings in using VSI versus MRI in medial meniscus pathology are robust to significant changes in MRI accuracy, number of procedures performed, a higher incidence of complications seen with MRI, and costs of procedures.
4 Discussion
The value of a diagnostic test should be evaluated by how it affects a patient’s health [28]. What this analysis demonstrates is not only a cost saving with VSI but less exposure to unnecessary care with VSI, based on the relative inability of MRI to rule out and rule in pathology when compared with VSI. The relative inability of MRI to rule out pathology (i.e., a FP finding) can result in follow-on surgical procedures that are unnecessary. Further, the inability of MRI to rule in pathology (i.e., missing pathology when it actually is present, or an FN finding) may send a patient down a path where their condition worsens and results in more expensive treatment, or results in worsening of a patient’s quality of life due to prolonged pain and suffering. In this cohort of patients with likely disease (based on the study design as outlined in Appendix 1, ESM), it was found that, in patients who actually had (TP + FN) medial or lateral meniscus knee pathology, a significantly lower number of patients were correctly identified as having disease (i.e., TP) with MRI versus VSI. As well, based on higher specificity values associated with using VSI, fewer patients were exposed to unnecessary procedures (i.e., FP)—thus improving quality of care. This resulted in significant cost savings to the healthcare system totaling US$163 million (US$177 million [medial meniscus pathology] + −US$14 million [lateral meniscus pathology]) when diagnosis and treatment were modeled using VSI.
The MRI findings (sensitivities, specificities, and accuracies) associated with the study outlined in Appendix 1 (ESM) are slightly worse than those found with meta-analyses—most especially for deep-seated pathology found in medial and lateral meniscus/cartilage tears [19, 29]. However, the current finding of a lower level of accuracy with MRI compared with standard arthroscopy is consistent with a trend in findings of lower accuracy over time [19] and with blinding of the clinical assessor (clinical assessor interpreting the MRI being blinded to the arthroscopy result) [29]. Use of blinding of the clinical assessor also reflects clinical practice where the MR imaging is usually performed prior to the arthroscopy. The current findings for sensitivity, specificity, and accuracy in the current study are certainly within the range of those found in meta-analyses, are similar to recent studies examining MRI accuracy for meniscal tears [30–32], and those found in non-academic clinical practice [30, 33].
A non-monetary outcome of using VSI, not discussed above, is a potential shortening of the patient’s diagnostic odyssey. With such a system, the patient is awake and can review their pathology actively with the physician. This also engages the patient in the course of diagnosis and potential treatment, and may reduce any patient anxiety that results from not knowing.
The use of in-office arthroscopy may also assist the physician in their preparation (based on better, more accurate information) for surgical intervention (when needed). There is likely a benefit of being better prepared as the clinician can plan and prepare for the appropriate surgical correction. An example of this is allograft tissue, which must be procured ahead of a surgical procedure, the use of which cannot be determined inter-operatively. While not quantified above, this may also shorten the procedure time, outcome, and costs of the therapeutic procedure.
The issue of unnecessary and inefficient use of services in healthcare is a major concern for policy makers and payers [34]. Use of the VSI system in the physician office setting reduces the need for clinicians to perform ‘definitive diagnostic’ arthroscopy procedures with FP patients (which typically turn into a surgical arthroscopy based on recent Medicare data analysis) [6], and any follow-on care resulting from MRI FN findings.
As it relates to the sensitivity analysis performed, as seen in Table 9, a systematic review of MRI accuracy, sensitivities, specificities, positive predictive values, and negative predictive values for medial meniscus tears show values of 86.3 %, 91.4 %, 81.1 %, 83.2 %, and 90.1 %, respectively [19]. The data used in this meta-analysis [19] were mainly from academic institutions where MRI assessment/accuracy of diagnosis is typically better than what is seen in the community setting. At these ‘academic’ sensitivities and specificities, use of VSI versus MRI still results in considerable savings to the system, exceeding US$115 million for diagnosing and treating medial meniscal tears. As mentioned, the findings from the MRI/VSI study (found in Appendix 1 in the ESM) may be more in line with what is found in a community setting, and the savings as well. The sensitivity analysis (Table 9) shows that, in an academic setting with MRI sensitivity and specificity results versus standard arthroscopy (the gold standard), the use of VSI in place of MRI results in cost savings approximately half the time when varying the sensitivities and specificities higher and lower. The only times MRI demonstrated a consistent cost savings was when the MRI sensitivities were <75 % (i.e., when there was an increased number of FN findings). Since diagnostic tests are designed to identify disease/pathology when it is present (e.g., rule in disease), it is unlikely that these cost-saving findings with a ‘low sensitivity’ (with concurrent high specificities) from MRI in Table 9 would ever be realized. Further, as shown in the shaded sections of Table 9, where most sensitivity and specificity MRI findings are likely to be found for medial meniscus diagnosis [30, 35, 36], cost savings result when using VSI. Thus, it can be concluded that the VSI cost savings are robust for permutations of MRI sensitivity/specificity. Additionally, as depicted in the Tornado plot (Fig. 5), these cost savings continue to exist when varying (up or down) factors that might affect these savings, including the cost of the procedure, complications, and the number of procedures (using study data). What is most interesting is that cost savings were most affected by varying the sensitivity of the MRI test. At lower MRI sensitivities, less savings resulted from VSI use and at higher sensitivities, much higher savings were realized. Since diagnostic tests are designed to rule in disease (i.e., possess relatively high sensitivities), it is unlikely that this ‘low sensitivity’ scenario would occur. As well, at lower sensitivities, more patients would be misdiagnosed as not having a meniscal tear when one actually exists and thus likely go down a path of inappropriate care/treatment.
4.1 Limitations
The following limitations of the above analysis should be taken into account.
-
It assumes the most conservative treatment when a FP result under MRI was treated with knee procedures (i.e., meniscectomy versus repair). This may have underestimated the complication rates and costs reported on above with MRI, as more aggressive treatment may have been undertaken with these FP findings.
-
It assumes that FP MRI results always result in a surgical arthroscopy procedure. This in turn may have overestimated the actual costs of the MRI paradigm. However, in pathology that appears positive under MRI and is difficult to interpret as in the pathology described herein (e.g., deep tissue), surgical arthroscopy is commonly performed.
-
Since no ‘good’ data exist in the literature on the complication rates seen with small needle/single access site arthroscopy, the complication rate assumed in this analysis with the VSI procedure was an estimate based on half of what the complication rate would be with arthroscopy (i.e., single access versus two access sites with traditional arthroscopy). In reports of case series on small needle arthroscopy, none of the complication rates noted above were seen [15]. The only estimated complication used with VSI was for infections at a rate of 0.01 %.
-
The use of a full course of PT (6 weeks and 10 visits at US$1,318) was assumed to be 85 % in the FN, FN CO, TP, and FP patients. The assumption was that since an orthopedist prescribed the PT, it was closely adhered to [23, 27]. Some patients may have taken it upon themselves to rehab at home, or not undergone PT, and thus may not have incurred this cost.
-
This does not include the costs of pain medications which may be higher with MRI due to a higher number of FN findings.
-
Analysis utilizes Medicare reimbursement. If private payer reimbursement were used in place of Medicare, savings would likely be higher as reimbursement is typically higher with private payers. As an example, as depicted in Fig. 5, with an increase of 20 % for reimbursement, the corresponding savings realized in using VSI would be US$206 million versus US$177 million (at baseline) for medial meniscus pathology.
5 Conclusion
More frequent use of the VSI system in the physician office setting as a diagnostic tool may reduce downstream and unnecessary procedures and costs in deep-seated knee pathology. Unnecessary procedures are by definition poor quality of care. Thus, reducing unnecessary procedures improves quality of care. More widespread utilization of the VSI diagnostic imaging system could save the US healthcare system significant dollars—most especially in medial meniscus pathology. These cost savings may also translate to other countries that perform arthroscopy procedures in similar settings (e.g., hospital outpatient setting).
Abbreviations
- CPT:
-
Current procedural terminology
- CY:
-
Calendar year
- E&M:
-
Evaluation and management
- FN:
-
False negative
- FN CO:
-
False negative cross over
- FP:
-
False positive
- ICD9CM:
-
International classification of diseases, 9th edition, clinical modification
- MRI:
-
Magnetic resonance imaging
- NCHS:
-
National Center for Health Statistics
- NSAS:
-
National Survey Ambulatory Surgery
- PT:
-
Physical therapy
- SOC:
-
Standard of care
- TN:
-
True negative
- TP:
-
True positive
- US$:
-
United States $
- VSI:
-
VisionScope imaging
References
National Ambulatory Medical Care Survey (NAMCS) 2010 and National Hospital Ambulatory Medical Care Survey (NHAMCS) 2010. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NAMCS/ and ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHAMCS/. Accessed 5 Dec 2013.
Nickinson R, Darrah C, Donnell S. Accuracy of clinical diagnosis in patients undergoing knee arthroscopy. Int Orthop. 2010;34:39–44.
Campbell AB, Knopp MV, Kolovich GP, Wei W, Jia G, Siston RA, Flanigan DC. Preoperative MRI underestimates articular cartilage defect size compared with findings at arthroscopic knee surgery. Am J Sports Med. 2013. doi:10.1177/0363546512472044.
Bouju Y, Carpentier E, Bergerault F, De Courtivron B, Bonnard C, Garaud P. The concordance of MRI and arthroscopy in traumatic meniscal lesions in children. Orthop Traumatol: Surg Res. 2011;97:712–8.
Fieeroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I. Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy. 2007;23(3):312–5.
CPT code analyses for knee arthroscopies using Medicare data 2003–2011: comparison of diagnostic arthroscopy versus therapeutic arthroscopy. http://www.cms.gov/Research-Statistics-Data-and-Systems/Files-for-Order/NonIdentifiableDataFiles/PartBNationalSummaryDataFile.html. Accessed 2 Oct 2013.
Halbrecht JL, Jackson DW. Office arthroscopy: a diagnostic alternative. J Arthrosc Relat Surg. 1992;8(3):320–6.
Juff JP, Segueira W, Harris CA. Survey of physicians doing office-based arthroscopy. Arthritis Rheum. 1992;35(supplement):S292.
Halbrecht JL, Wolf EM. Office arthroscopy of the shoulder: a comparison with magnetic resonance imaging. Arthroscopy. 1993;9(3):348–9.
Ayral X, Dougados M, Listrat V, Bonvarlet J, Simonnet J, Poiraudeau S, Amor B. Chondroscopy: a new method for scoring chondropathy. Semi Arthritis Rheum. 1993;22:289–97.
O’Rourke KS, Ike RW. Diagnostic arthroscopy in the arthritis patient. Rheum Dis Clin North Am. 1994;20(2):321–42.
Szachnowski P, Wei N, Arnold WJ, Cohen LM. Complications of office based arthroscopy of the knee. J Rheumatol. 1995;22:1722–5.
Reece R, Emery P. Needle arthroscopy. Br J Rheumatol. 1995;34(12):1102–4.
Meister K, Harris NL, Indelicato PA, Miller G. Comparison of an optical catheter office arthroscopy with a standard rigid rod-lens arthroscopy in the evaluation of the knee. Am J Sports Med. 1996;24(6):819–23.
Baeten D, Van den Bosch F, Elewaut D, Stuer A, Veys EM, De Keyser F. Needle arthroscopy of the knee with synovial biopsy sampling: technical experience in 150 patients. Clin Rheumatol. 1999;18:434–41.
Ostendorf B, Peters R, Dann P, Becker A, Scherer A, Wedekind F, Friemann J, Schulitz K, Mödder U, Schneider M. Magnetic resonance imaging and miniarthroscopy of metacarpophalangeal joints. Arthritis Rheum. 2001;44(11):2492–502.
Batcheleor R, Henshaw K, Astin P, Emery P, Reece R, Leeds DJV. Rheumatological needle arthroscopy: a 5-year follow-up study of safety and efficacy. Arthritis Rheum Ann Sci Meet Abst. 2001;S9:Abstract #1578:S316.
Diagnosis and management of meniscal knee tears/pathology. http://orthoinfo.aaos.org/topic.cfm?topic=a00358. Accessed 3 Apr 2013.
Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23.
National ambulatory medical care survey data 2010—estimate of use of arthrocentesis in diagnosing knee pathology. Ten percent figure arrived at based on number of arthrocenteses performed for medial meniscal knee injury (100,000) divided by overall number medial meniscal knee diagnostic and therapeutic procedures for 2012 (970,000). Therefore 100,000/970,000 =10%.
Jameson SS, Dowen D, James P, Serrano-Pedraza I, Reed MR, Deehan DJ. The burden of arthroscopy of the knee. A contemporary analysis of data from the English NHS. JBJS. 2011;93-B:1327–33.
Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, Donnell-Fink LA, Guermazi A, Haas AK, Jones MH, Levy BA, Mandl LA, Martin SD, Marx RG, Miniaci A, Matava MJ, Palmisario J, Reinke EK, Richardson BE, Rome BN, Safran Norton CE, Skoneicki DJ, Solomon DH, Smith MV, Spindler KP, Stuart MJ, Wright J, Wright RW, Losina E. Surgery versus physical therapy for a meniscal tear and osteoarthritis. NEJM. 2013;368(18):1675–84.
Grindley EJ, Zizzi SJ, Nasypany AM. Use of protection motivation theory, affect, and barriers to understand and predict adherence to outpatient rehabilitation. Phys Ther. 2008;88(12):1529–40.
Brox JI, Gjengedal E, Uppheim G, Bøhmer AS, Brevik JI, Ljunggren AE. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2.5 year follow-up. J Shoulder Elbow Surg. 1999;8:102–11.
CIGNA coverage policy for physical therapy. Coverage policy number: 0096; effective date: 3/15/2013.
Percent uninsured as of 2009, Gallup poll taken June 2009. http://www.gallup.com/poll/121820/one-six-adults-without-health-insurance.aspx. Accessed 31 May 2013.
Freburger JK, Carey TS, Holmes GM. Physical therapy for chronic back pain in North Carolina: overuse, underuse, or misuse? Phys Ther. 2011;91(4):484–95.
di Ruffano LF, Hyde DJ, McCaffery KJ, Bossuyt PMM. Assessing the value of diagnostic tests: a framework for designing and evaluating trials. Brit Med J. 2012;344:e686. doi:10.1136/bmj.e686.
Oei EHG, Nikken JJ, Verstijnen ACM, Ginai AZ, Hunink MGM. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003;226:837–48.
Hardy JC, Evangelista GT, Grana WA, Hunter RE. Accuracy of magnetic resonance imaging of the knee in the community setting. Sports Health. 2012;4(3):222–31.
Rayan F, Bhonsle S, Shukla DD. Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. Int Orthop. 2009;33:129–32.
Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkeivicz P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc. 2007;15:533–6.
Ben-Galim P, Steinberg EL, Amir H, Ash N, Dekel S, Arbel R. Accuracy of magnetic resonance imaging of the knee and unjustified surgery. Clin Orthop Relat Res. 2006;447:100–4.
Yong PL, Saunders RS, Olsen LA. The healthcare imperative. Lowering costs and improving outcomes. Institute of Medicine National Academies Press. 2010. ISBN:978-0-309-14433-9.
Odgaard F, Tuxoe J, Lange B, Lausten G, Brettlau T, Thomsen HS. Clinical decision making in the acutely injured knee based on repeat clinical examination and MRI. Scan J Med Sci Sports. 2002;12:154–62.
Yan R, Wang H, Yang Z, Ji ZH, Guo YM. Predicted probability of meniscus tears: comparing history and physical examination with MRI. Swiss Med Weekly. 2011;41:w13314.
Spyropoulos AC, Lin J. Direct medical costs of venous thromboembolism and subsequent hospital readmission rates: an administrative claims analysis from 30 managed care organizations. JMCP. 2007;13(6):475–86 (Costs were inflated from 2007 to 2012 using CPI medical index).
Hasselbacher P. Arthrocentesis, synovial fluid analysis, and synovial biopsy. In: Schumaker HR, Klippel JH, Koopman WJ, editors. Primer on rheumatic diseases. 10th ed. Atlanta: Arthritis Foundation; 1993. p. 67–72.
Authors’ contributions
JV, MM, and BH developed the hypothesis and laid out the methodology for testing the hypothesis. JV and BH developed the first draft of the manuscript. MM provided the appropriate statistical analysis. JV and BH developed the first draft of the manuscript. MM provided the appropriate statistical analysis. JV performed the literature search for relevant articles. MM extensively reviewed the first draft and made edits. MM further reviewed the statistics and ensured the integrity of the data. JV, MM, and BH read and approved the final manuscript. JV is the guarantor of the content.
Conflict of interest
Jeff Voigt works as a reimbursement consultant for Visionscope Technologies, an office-based arthroscopy technology mentioned in the manuscript. Jeff Voigt was paid an unrestricted grant for the writing of this manuscript.
Michal Mosier has no competing interests.
Bryan Huber works as a clinical consultant for Visionscope Technologies, an office-based arthroscopy technology mentioned in the manuscript.
Study funding
Study funding was provided by an unrestricted grant by Visionscope Technologies for the analysis and writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Voigt, J.D., Mosier, M. & Huber, B. Diagnostic Needle Arthroscopy and the Economics of Improved Diagnostic Accuracy: A Cost Analysis. Appl Health Econ Health Policy 12, 523–535 (2014). https://doi.org/10.1007/s40258-014-0109-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-014-0109-6