Abstract
Introduction
Problems in the definition and classification of angioedema, leading to difficulties in its diagnosis and treatment, have been identified; therefore, an improvement in the current classification of angioedema is required.
Objective
The aim of this study was to propose a practical classification of angioedema without wheals that helps to establish a differential diagnosis and take appropriate therapeutic decisions.
Methods
An initial proposal of classification of angioedema without wheals was agreed by a scientific committee of experts and was subsequently validated by a panel of experts by means of consensus based on the Delphi methodology. Forty-five items on the classification, diagnosis, and treatment of angioedema without wheals were proposed for the survey.
Results
Most items (93.8%) were agreed after two rounds. All panelists agreed with the proposed classification, as well as with most of the clinical and treatment characteristics. The angioedema without wheals classification established three groups: histamine-mediated, bradykinin-mediated, and unknown mechanism angioedema. The clinical characteristics of the proposed types of angioedema were also agreed, except for the allergic histamine-mediated and unknown mechanism angioedema, which generated debate. Regarding treatments, although there was broad agreement with the proposed items, a lack of knowledge about some treatments in this pathology was observed.
Conclusion
The proposed classification of angioedema without wheals was accepted with a high degree of agreement; however, knowledge of available treatments needs to be increased and the definition of angioedema of unknown mechanism needs to be improved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Isolated angioedema can be difficult to classify. |
The key factor is to distinguish between bradykinin-mediated and mast cell-mediated angioedema. |
A correct diagnosis is essential because the therapeutic approach is different and bradykinin-mediated angioedema could be life-threatening. |
1 Introduction
Angioedema frequently occurs in the context of an urticaria, which is characterized by two symptoms: wheals (edema of the superficial layers) and/or angioedema (edema of the deep layers of the dermis with subtle erythema), which can appear isolated or in combination [1]. Given the great diagnostic and therapeutic challenge posed by angioedema without wheals (or isolated angioedema), we focused this article on this type of angioedema. Although mast cell-mediated angioedema can be considered as a subtype of urticaria [1], there is a lack of evidence to support this concept. Isolated angioedema with no hives does not show some specific features commonly present in chronic urticaria, such as no female predominance, less basopenia and no role of anti-IgE receptor antibodies in the pathogenesis [2, 3].
Angioedema without wheals can be difficult to precisely diagnose and manage. On the one hand, the term angioedema is used to refer to both the nosological entity and the underlying lesion. One of the proposed definitions states that angioedema is produced by a vascular reaction of the deep dermis or submucosal or subcutaneous tissues that consists of a temporary increase in the permeability of blood vessels. This increase in permeability, secondary to the release of vasoactive mediators, such as histamine or bradykinin, produces localized and self-limited edema [4,5,6].
On the other hand, there is no commonly agreed classification and nomenclature for angioedema without wheals, which generates confusion in the terms used in the clinical guidelines; to date, there are different classification proposals based on the pathogenic mechanism (histaminergic or bradykinergic) [7,8,9], endotype (due to bradykinin excess, mast cell/basophil degranulation, and idiopathic) [10], or phenotype and genotype (acquired or hereditary, with or without C1 inhibitor [C1-INH] deficiency) [5, 11, 12].
The response to treatment, mainly to antihistamines, used for the classification and diagnosis of angioedema, is also not well-defined and can be misunderstood [5]. To classify angioedema according to response to treatment, it is necessary to establish the meaning of non-response and to be sure that adequate doses of acute or maintenance treatment have been used. In 2015, a series of cases with idiopathic non-histaminergic angioedema (according to the HAWK classification) that did not respond to H1 antihistamines, but did respond to omalizumab, was published [13]. With these data, the Spanish Study Group on Bradykinin-Mediated Angioedema (GEAB) stated the need for a new classification of angioedema in which idiopathic non-histaminergic-acquired angioedema were not identified directly as a bradykinergic angioedema and the response to corticosteroids, adrenaline, omalizumab, and/or immunosuppressants was used to properly classify them as mast cell-mediated angioedema or not [11]. Subsequently, it was found that in 20 patients with angioedema without wheals that did not respond to preventive treatment with high-dose H1 antihistamines and/or tranexamic acid had a very good response to omalizumab at a dose of 300 mg every 4 weeks, with improvement in 80%, suggesting the involvement of mast cells/basophils in the pathogenesis of this type of angioedema [14]. The use of omalizumab in the classification of idiopathic angioedema may be cost saving in terms of other alternative treatments for non-histaminergic angioedema, such as plasma-derived C1-INH concentrate, lanadelumab, berotralstat or icatibant acetate.
Therefore, the classification of angioedema is mainly based on clinical features, genetic studies, and/or response to treatment. Its correct discrimination will depend on useful clinical tools and the availability of specific biomarkers. In clinical practice, there is likely to be a pathophysiological overlap in a considerable group of patients, which is determined by the bidirectional connection between the mast cell/basophil and the kallikrein-kinin system. That is, some patients may present characteristics that will make them eligible for inclusion in more than one group [8, 9].
Thus, the current classification of angioedema could be improved. The aim of this work was to offer a practical classification of angioedema without wheals that will help health care professionals, especially those with less experience with the disease, to establish a differential diagnosis and make correct therapeutic decisions. A Delphi methodology was used to reach a consensus and obtain expert opinion on the validity of the classification.
2 Methods
2.1 Study Design
The study used a modified Delphi method, a structured communication technique that allows a group of experts to gather opinions on a given complex or controversial topic for which there is insufficient evidence or their knowledge is incomplete or uncertain [15, 16]. In addition, it allows the opinions of a group of experts to be explored and unified without the difficulties and inconveniences inherent to consensus methods based on face-to-face discussions, such as displacements or the biases of influence or non-confidential interaction.
The study was performed in several phases: (1) project approach and creation of a scientific committee of experts in angioedema; (2) review of the most recent literature on angioedema without wheals, after which a classification was proposed based on evidence and the clinical experience of the committee members; (3) drafting of a questionnaire with the items considered most relevant and agreed by the scientific committee; (4) two successive rounds of online surveys to gather the opinion of the expert panel; and (5) compilation, analysis, and discussion of the results to draw up conclusions.
2.2 Participants
Three types of professionals participated in the study: a scientific committee, a technical team, and a panel of experts. The scientific committee consisted of three allergists with expertise in angioedema, whose role was to review the literature, propose the classification of angioedema without wheals, and draft a questionnaire with items regarding the classification and treatment of angioedema without wheals. The technical team, which directed and supervised the entire process, was responsible for the instrumental implementation of the method (search of the literature, distribution of the questionnaire to the panelists, analysis of the responses, and statistical interpretation of the consensus). Finally, the scientific committee chose the panel of experts, which was made up of a total of 36 health professionals who met the following criteria: membership of the GEAB (in Spanish ‘Grupo Español de Estudio del Angioedema Mediado por Bradicinina’), having publications related to angioedema, and/or handling cases of angioedema in their clinical practice. An adequate territorial distribution was sought among all the Autonomous Communities of Spain.
2.3 Classification of Angioedema without Wheals and the Delphi Questionnaire
After a review of the most recent literature on angioedema, the scientific committee held a series of meetings in which several aspects related to this pathology were discussed, especially those that were still unclear or controversial, such as its definition and characteristics, its classification, the tools used for its diagnosis, and the treatments available. Based on all this information, a classification of angioedema without wheals and a Delphi questionnaire consisting of 45 items grouped into the following topics were proposed: (1) classification of angioedema without wheals (6 items); (2) clinical features of the different types of angioedema (12 items); (3) treatment characteristics of the different types of angioedema (19 items); and (4) general considerations for the treatment of angioedema (8 items).
For the evaluation of the questionnaire, a single 9-point Likert-type ordinal scale was proposed, according to the model developed by the UCLA-RAND Corporation for the comparative evaluation and prioritization between different health care options (minimum 1, complete disagreement; and maximum 9, complete agreement) [16]. This scale was structured in three groups according to the level of agreement/disagreement of the statement: from 1 to 3, interpreted as rejection or disagreement; from 4 to 6, interpreted as no agreement or disagreement; and from 7 to 9, interpreted as expression of agreement or support.
2.4 Phases of Delphi Consensus
Following the Delphi methodology procedure [17], the questionnaire was sent to the panel of experts to respond by showing their degree of agreement with the items. In the first round, the panelists responded to the questionnaire online and were offered the possibility of adding their opinion as an open text. The technical team evaluated and presented the results of the first round using bar graphs to facilitate comments and clarifications from each participant. Non-consensus items were reformulated and sent back to the panelists to be evaluated in a second round. The results of this second round were tabulated and presented in a descriptive form. The project was closed with a meeting of the scientific committee to discuss and analyze the results.
2.5 Analysis and Interpretation of Results
To analyze the opinion and the type of consensus reached on each item, the median and interquartile range of the scores obtained for each item were used. There was consensus when two-thirds or more of the respondents scored within the 3-point range (1–3 or 7–9) that contained the median. The type of consensus reached on each item was determined by the score median. There was agreement if the median was ≥ 7, and disagreement if the median was ≤ 3. No consensus was considered when one-third or more of the panelists scored in the range of 1–3 and another third or more in the range of 7–9. When the median score fell between the range of 4–6, the items were considered uncertain to a representative majority of the group.
3 Results
Figure 1 shows the classification of angioedema without wheals proposed by the scientific committee. Three main categories were established: (1) histamine-mediated (and/or other mast cell- and basophil mediator-mediated) angioedema (AE-H); (2) bradykinin-mediated angioedema (AE-BK); and (3) unknown mechanism angioedema (AE-UNK). AE-H could be allergic or non-allergic; AE-BK could be hereditary (with or without C1-INH deficiency), acquired, or idiopathic; and AE-UNK refers to angioedema whose mediator or pathophysiologic mechanism is unknown and in which all available diagnostic and therapeutic options have been exhausted to otherwise classify it.
Classification of angioedema without wheals proposed by the scientific committee. Three main categories were established: (1) histamine-mediated (and/or other mast cell- and basophil mediators-mediated) angioedema (AE-H); (2) bradykinin-mediated angioedema (AE-BK); and (3) unknown mechanism angioedema (AE-UNK). AE-H could be allergic or non-allergic; AE-BK could be hereditary (with or without C1-INH deficiency), acquired, or idiopathic; and AE-UNK refers to angioedema whose mediator or pathophysiologic mechanism is unknown and in which all available diagnostic and therapeutic options have been exhausted to otherwise classify it. NSAIDs non-steroidal anti-inflammatory drugs, ACEI angiotensin-converting enzyme inhibitors
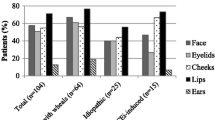
Of the 45 items proposed in the first round, consensus was reached on 38, all in agreement. The 7 non-consensus items were reformulated into another 10 items that were sent to the panelists to be assessed in a second round. Of these, consensus was reached in 7 (all in agreement) and 3 did not reach consensus. After the two rounds, and a total of 48 items, 45 reached consensus in agreement (93.8%) and 3 did not reach consensus (6.2%) (Fig. 2). Electronic supplementary material (ESM) Tables S1–S4 show in detail all the items proposed in the first and second rounds.
Main results of the Delphi consensus. Of the 45 items proposed in the first round, consensus was reached on 38, all in agreement. The 7 non-consensus items were reformulated into another 10 items that were sent to the panelists to be assessed in the second round. Of these, consensus was reached in 7 (all in agreement) and 3 did not reach consensus. After the two rounds, and a total of 48 items, 45 reached consensus in agreement (93.8%) and 3 did not reach consensus (6.2%)
3.1 Classification of Angioedema without Wheals
All items about classification of angioedema reached consensus in the first round (ESM Table S1). All panelists agreed with the three proposed angioedema groups. Despite the high degree of agreement reached on all items, the one that generated the most discussion referred to ‘non-allergic AE-H’ (item 3, 83.3% agreement).
3.2 Clinical Features of the Different Types of Angioedema
Most of the 12 proposed items reached consensus with a high degree of agreement in the first round (ESM Table S2); however, no consensus was reached on three of them. Item 8 on the characteristics of ‘allergic AE-H’ was reformulated into two other items, of which only the one that defined it as a rare cause of isolated angioedema and that usually occurred together with wheals, was agreed (88.9% agreement), probably due the fact to that in the current classifications, this type of angioedema is not considered. There was no consensus on the item that said its frequency depended on the allergen involved. Item 9 on ‘spontaneous AE-H’ was reformulated into a different item that clarified that it starts in adulthood and mainly affects the upper airway and, to a lesser extent, the gastrointestinal tract. This reformulated item increased the degree of agreement to 75%. Finally, item 17 on ‘AE-UNK’ was reformulated to describe it as one that does not have defined clinical characteristics and could have those of other types of angioedema (86.1% agreement).
3.3 Characteristics of the Treatment of the Different Types of Angioedema
Of the 19 items proposed, 15 reached consensus with a high degree of agreement in the first round (ESM Table S3). Item 24 was reformulated into another item to emphasize that the main therapeutic strategy for ‘allergic AE-H’ is avoidance of allergen exposure, eliminating the information that if allergen avoidance did not work, ‘allergic AE-H’ would be ruled out (94.4% agreement). Item 36 on the treatment of ‘idiopathic AE-BK’ was reformulated into two items to indicate that maintenance treatment in cases with very frequent episodes should be with tranexamic acid, and that when there is no response to this drug or to H1 antihistamines, a trial with a plasma-derived C1-INH concentrate, lanadelumab or omalizumab can be considered. Both items reached a discrete consensus of 69.4% each.
Reformulation of the other two items that did not reach consensus in the first round also did not reach consensus in the second round. In the first round, item 28 proposed that mixed ‘mast cell/basophil-mediated and AE-BK’ may respond to tranexamic acid. In the second round was reformulated to that it may respond to tranexamic acid, H1 antihistamines, or their combination. Regarding item 33, it initially stated that the treatment of ‘acquired AE-BK’ was the same as for ‘hereditary AE-BK’. In the absence of consensus, it was reformulated into two items. One added that both were C1-INH-deficient, but this item was not agreed, and the other stated that ‘acquired AE-BK with C1-INH deficiency’ can be treated with rituximab when episodes are frequent, which was also not agreed.
3.4 General Considerations for the Treatment of Angioedema
The eight proposed items were agreed in the first round (ESM Table S4). Item 38, which stated that patients with recurrent angioedema with at least one episode per month, regardless of the mechanism, should be given preventive treatment, obtained the lowest agreement (69.4% agreement). The panelists provided various arguments. One of the most recurrent was that preventive treatment depends on the angioedema location, quality of life, and intensity of the flare-ups. It was also mentioned that some patients with this condition prefer on-demand treatment.
Another controversial issue was item 42, which stated that response to acute treatment is defined as no progression of angioedema within 2 h, or complete disappearance of angioedema in <12 h (75% agreement). The panelists argued that in some cases, complete resolution within 12 h may be uncertain, even if response has been obtained. Furthermore, some of the panelists said that some episodes of mast cell-mediated angioedema may resolve spontaneously within 12–24 h and that failure to progress may be because the peak of the episode had been reached before treatment was administered.
4 Discussion
The most widely accepted classifications of angioedema without wheals make it difficult to manage due to a number of limitations [5]. There is a great need to clarify such classification and simplify its approach. For this reason, a group of experts in this condition proposed a practical classification of angioedema without wheals, especially useful for those health care professionals with less experience in this pathology, to facilitate a correct differential diagnosis and improve management. Using a consensus based on Delphi methodology, through which the opinion of a panel of experts in the disease was obtained, the suitability of the proposed classification and its applicability for diagnosis and treatment could be verified.
The classification of angioedema without wheals proposed by the scientific committee was accepted by all the panelists consulted, with a high level of agreement. However, although 93.8% of the proposed items on the definitions of the different types of angioedema reached consensus in the agreement, the panelists helped to refine and improve some of these items. On the other hand, the lack of consensus shown in some of the items regarding the treatment of angioedema highlights the knowledge gaps that some health care professionals have in the management of such infrequent disease, especially with regard to the treatment of ‘acquired AE-BK with C1-INH deficiency’ or ‘idiopathic AE-BK’. This may be due, apart from the low prevalence of these diseases, to the lack of approved drugs for these indications and to the lack of current consensus documents on their treatment.
With 83.3% agreement, the most discussed subtype was ‘non-allergic AE-H’. The panelists argued that an episode of angioedema is acute by definition and, when recurrent, the frequency of episodes may be greater or lesser, but without influencing its classification as acute or chronic. Although both chronic spontaneous urticaria and isolated AE-H are mediated by mast cells and respond to the same treatment, we consider that AE-H deserves separate attention.
Recent urticaria international guidelines suggest that urticaria and angioedema can be considered as the same condition [1]. However, angioedema without wheals has been considered a different entity by international groups of experts [2, 3, 5]. Although chronic spontaneous urticaria and AE-H share some pathophysiological features, such as the pivotal role of mast cells and basophils, there are some specific clinical and pathogenic characteristics that show they are probably different entities. Chronic spontaneous urticaria manifests more frequently on the lips and eyelids, while AE-H is more frequent on the tongue [2]. Nevertheless, further studies showing the differences or similarities of urticaria and angioedema are needed before considering them as the same.
The results of this study highlight the need to disseminate knowledge about the treatment of angioedema subtypes and new drugs for the treatment of ‘hereditary AE-BK with C1-INH deficiency’, such as lanadelumab. Although there was consensus in agreement that when no response was obtained to H1 antihistamines (at quadruple doses) and/or omalizumab, ‘mast cell- and basophil-mediated angioedema’ should be ruled out, some panelists stated that response to cyclosporine should also be checked as an additional measure of exclusion. The lack of consensus on the use of rituximab in ‘acquired AE-BK with C1-INH deficiency’ could be due, apart from the aforementioned lack of experience of use, to the fact that this is a very rare disease and that this drug is indicated in lymphoproliferative diseases. In fact, several panelists commented that it should only be used if proliferative disease is detected or anti-C1-INH autoantibodies are present. However, this drug can be used even in the absence of associated lymphoproliferative disease or anti-C1-INH autoantibodies, a fact that seems to be unknown to most of the panelists [18, 19].
When angioedema does not respond to continuous supratherapeutic doses of H1 antihistamines and is not considered histamine-mediated, it does not necessarily have to be bradykinin-mediated. Indeed, for the first time, this study proposed a therapeutic scale for the prevention of the spontaneous AE-H in four steps (first-line H1 antihistamines at marketed doses, second-line H1 antihistamines at supratherapeutic doses, third-line adding omalizumab, and fourth-line adding other drugs) and for idiopathic AE-BK in two steps (first-line tranexamic acid, and if no response, a therapeutic trial with off-label plasma C1-INH concentrate, lanadelumab or omalizumab may be considered).
The main strength of this study is that it offers a global classification of angioedema without wheals that includes the state-of-the-art angioedema subtypes and treatment, from an acute and preventive perspective, and that it is agreed by a group of experts in angioedema using a Delphi methodology. The main limitation of the study is the small number of panelists. Although they are health care professionals with recognized expertise in angioedema, the extrapolation of the consensus results to the entire medical community could be a handicap. Likewise, the proposed classification of angioedema without wheals should be understood as a way to facilitate its diagnosis and treatment. Although it is based on other established classifications supported by evidence, it has been modified according to the clinical experience of the scientific committee. Another limitation is that the low prevalence of some types of angioedema, such as ‘acquired AE-BK with C1-INH deficiency’ or ‘hereditary AE-BK with normal C1-INH’, could translate into reduced clinical experience of some of the panelists, in addition to the lack of approved drugs.
5 Conclusions
The classification of angioedema without wheals into three main types (AE-H, AE-BK, and AE-UNK) was accepted with a high degree of agreement among the panelists; however, the lack of consensus observed in some types, such as AE-UNK, requires improvement and clarification of its definition. Likewise, the lack of consensus observed in the items regarding treatment suggests the need to improve knowledge on the treatment of some types of angioedema and the need for consensus documents.
References
Zuberbier T, Abdul Latiff AH, Abuzakouk M, Aquilina S, Asero R, Baker D, et al. The international EAACI/GA2LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy. 2022;77(3):734–66.
Sabaté-Brescó M, Rodriguez-Garijo N, Azofra J, Baeza ML, Donado CD, Gaig P, et al. A comparative study of sex distribution, autoimmunity, blood, and inflammatory parameters in chronic spontaneous urticaria with angioedema and chronic histaminergic angioedema. J Allergy Clin Immunol Pract. 2021;9(6):2284–92.
Rodríguez-Garijo N, Sabaté-Brescó M, Azofra J, Baeza ML, Donado CD, Gaig P, et al. Angioedema severity and impact on quality of life: Chronic histaminergic angioedema versus chronic spontaneous urticaria. J Allergy Clin Immunol Pract. 2022. https://doi.org/10.1016/j.jaip.2022.07.011.
Craig T, Aygören-Pürsün E, Bork K, Bowen T, Boysen H, Farkas H, et al. WAO guideline for the management of hereditary angioedema. World Allergy Organ J. 2012;5(12):182–99.
Cicardi M, Aberer W, Banerji A, Bas M, Bernstein JA, Bork K, et al. Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy. 2014;69(5):602–16.
Marzano AV, Maronese CA, Genovese G, Ferrucci S, Moltrasio C, Asero R, et al. Urticarial vasculitis: clinical and laboratory findings with a particular emphasis on differential diagnosis. J Allergy Clin Immunol. 2022;149(4):1137–49.
Pedrosa M, Prieto-García A, Sala-Cunill A, Spanish Group for the Study of Bradykinin-Mediated Angioedema and the Spanish Committee of Cutaneous Allergy. Management of angioedema without urticaria in the emergency department. Ann Med. 2014;46(8):607–18.
Andrási N, Veszeli N, Kohalmi KV, Csuka D, Temesszentandrási G, Varga L, et al. Idiopathic nonhistaminergic acquired angioedema versus hereditary angioedema. J Allergy Clin Immunol Pract. 2018;6(4):1205–8.
Lenschow M, Bas M, Johnson F, Wirth M, Strassen U. A score for the differential diagnosis of bradykinin- and histamine-induced head and neck swellings. Eur Arch Otorhinolaryngol. 2018;275(7):1767–73.
Giavina-Bianchi P, Aun MV, Motta AA, Kalil J, Castells M. Classification of angioedema by endotypes. Clin Exp Allergy. 2015;45(6):1142–3.
Prieto-García A, Marcos C, Caballero T, Spanish Group for Study of Bradykinin-Mediated Angioedema. Classification of angioedema without wheals. Ann Allergy Asthma Immunol. 2016;116(2):177.
Sala-Cunill A, Guilarte M. The role of mast cells mediators in angioedema without wheals. Curr Treat Options Allergy. 2015;2(4):294–306.
Azofra J, Diaz C, Antepara I, Jauregui I, Soriano A, Ferrer M. Positive response to omalizumab in patients with acquired idiopathic nonhistaminergic angioedema. Ann Allergy Asthma Immunol. 2015;114(5):418 e1-419.
Guilarte M, Galván-Blanco P, Sala-Cunill A, Labrador-Horrillo M, Luengo O, Cardona V, editors. Response to omalizumab. A useful tool to clasify idiopathic angioedema. EAACI Congress: 26–30 May 2018; Munich.
Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–80.
Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lázaro P, et al. The RAND/UCLA Appropriateness Method User's Manual. 2021. http://www.rand.org/pubs/monograph_reports/MR1269.html. Accessed 8 Dec 2021.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
Levi M, Cohn D, Zeerleder S, Dziadzio M, Longhurst H. Long-term effects upon rituximab treatment of acquired angioedema due to C1-inhibitor deficiency. Allergy. 2019;74(4):834–40.
Gobert D, Bouillet L, Armengol G, Coppo P, Defendi F, Du-Thanh A, et al. Acquired angioedema due to C1-inhibitor deficiency: CREAK recommendations for diagnosis and treatment. Rev Med Interne. 2020;41(12):838–42.
Acknowledgments
The authors thank Fernando Sánchez Barbero, PhD, on behalf of Springer Healthcare, for providing medical writing and editorial support, as well as for coordination support in the execution of the Delphi Panel, which was funded by Novartis Pharmaceuticals in accordance with Good Publication Practice (GPP3) guidelines. The authors would also like to thank the panelists who graciously participated in the two rounds of the Delphi: Ramón Almero (allergologist), Ascensión Aranzábal (allergologist), María Luisa Baeza (allergologist), Rosario Cabañas (allergologist), Pedro Carretero (allergologist), Stefan Cimbollek (allergologist), Amparo Conde (allergologist), Carmen Díaz-Donado (allergologist), Ana Entrala (allergologist), Lucía Ferrer (allergologist), Blanca García-Figueroa (allergologist), José María García-Ruiz de Morales (immunologist), Pedro Manuel Gamboa (allergologist), Carlos Hernando de Larramendi (allergologist), Lys Herráez (allergologist), Ethel Ibáñez (allergologist), Piliar Iriarte-Sotés (allergologist), Ignacio Jáuregui (allergologist), Jesús Jurado-Palomo (allergologist), Milagros Lázaro (allergologist), Ramón Lleonart (allergologist), Teófilo Lobera (allergologist), Teresa Macías (allergologist), Carmen Marcos (allergologist), Lluís Marqués (allergologist), Ruth Mielgo (allergologist), Javier Miquel (dermatologist), María Pedrosa (allergologist), María Dolores del Pozo (allergologist), Alicia Prieto (allergologist), Nieves Prior (allergologist), Blanca Sáenz de San Pedro (allergologist), Anna Sala (allergologist), Isabel Sánchez-Matas (allergologist), María Eugenia Sanchís (allergologist), and Beatriz Veleiro (allergologist).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions (consent to participate/consent for publication)
All authors equally participated in the development of the Delphi study and the manuscript, had full editorial control, reviewed and edited various drafts, and provided their final approval of all content and submission for publication.
Funding
Novartis Pharmaceuticals provided economic funding for this work. The sponsor had no role in the design, analysis and interpretation of the data, the wording of the article, or the decision to send the article for publication.
Conflicts of interest/competing interest
Teresa Caballero is/has been a member of advisory boards for BioCryst, CSL Behring, Novartis, Octapharma, Pharming, and Takeda; is/has been a member of speakers’ bureaus for CSL Behring, Novartis, Pharming, and Takeda; has received grants or honoraria from BioCryst, CSL Behring, Novartis, and Takeda; has received funding to attend conferences/educational events from CSL Behring, Novartis, and Takeda; is/has been a clinical trial/registry investigator for BioCryst, CSL Behring, Novartis, Pharming, and Takeda; and is a researcher from the IdiPAZ program for promoting research activities. Marta Ferrer has been a speaker, advisory board member, and/or investigator for Genentech, Novartis, Sanofi, Menarini, Uriach, FAES, and MSD; and has received grants from GSK and Novartis. Mar Guilarte has received honoraria for educational purposes from CSL Behring, Novartis, and Takeda; has participated in advisory boards organized by CSL Behring, Novartis, and Takeda; has received funding to attend conferences and educational events from CSL Behring, Novartis, Pharming, and Takeda; and is a clinical trial/registry investigator for BioCryst, CSL Behring, Novartis, Pharming, Pharvaris, and Takeda, and a researcher from the VHIR program for promoting research activities.
Ethics approval
Not applicable.
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Caballero, T., Ferrer, M. & Guilarte, M. Classification and Treatment of Angioedema without Wheals: A Spanish Delphi Consensus. Am J Clin Dermatol 24, 135–141 (2023). https://doi.org/10.1007/s40257-022-00735-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00735-7