Abstract
Background
Due to the high comorbidity of diabetes and hypertension, co-administration of metformin with anti-hypertensive drugs is likely. Baxdrostat is an aldosterone synthase inhibitor in development for the potential treatment of hypertension. In vitro data indicated that baxdrostat inhibits the multidrug and toxin extrusion 1 (MATE1) and MATE2-K renal transporters. Metformin is a MATE substrate, so this study assessed potential effects of baxdrostat on the pharmacokinetics of metformin.
Methods
Twenty-seven healthy volunteers received 1000 mg metformin alone and 1000 mg metformin in the presence of 10 mg baxdrostat in a randomized, crossover manner. Each treatment was separated by 10 or more days. Blood and urine samples were collected over a 3-day period after each treatment to measure plasma and urine concentrations of metformin. Safety was assessed by adverse events (AEs), physical examinations, electrocardiograms, vital signs, and clinical laboratory evaluations.
Results
There were no deaths, serious AEs, discontinuations due to treatment-emergent AEs, or noteworthy increases in AEs with either treatment, indicating that metformin and baxdrostat were well-tolerated when co-administered. Baxdrostat did not significantly affect plasma concentrations or renal clearance of metformin.
Conclusion
The results of this study suggest that diabetic patients with hypertension receiving both metformin and baxdrostat are unlikely to require dose adjustment.
Registration
ClinicalTrials.gov identifier no. NCT05526690.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study investigated whether the hypertension drug baxdrostat would have any effect on levels of the diabetes drug metformin in healthy human volunteers taking both medications. |
Baxdrostat did not significantly change the levels of metformin in the blood or urine, suggesting that diabetic patients with hypertension who take both medications are unlikely to require dose adjustment. |
Baxdrostat and metformin were both well-tolerated when taken together, with no serious adverse events observed during the study. |
1 Introduction
Type 2 diabetes mellitus (T2DM) and hypertension are 2 of the leading causes of cardiovascular disease in the United States (US) [1, 2]. Between 69% and 82% of patients with T2DM also have hypertension [3, 4]. The high comorbidity between T2DM and hypertension means that many patients receiving common anti-diabetic drugs will also require treatment with anti-hypertensive drugs and may experience drug–drug interactions. Such interactions may affect the required dosing of one or both treatments.
Metformin is the first-line pharmacologic treatment for T2DM and the most commonly prescribed oral anti-diabetic medication, taken by approximately 50% of patients with T2DM worldwide and by 60% of patients with T2DM in the US [5,6,7]. Its primary mechanism of action is to reduce liver gluconeogenesis [8]. Metformin is a substrate of the multidrug and toxin extrusion 1 (MATE1) and MATE2-K renal tubule transporter proteins [8, 9]. MATE1 and MATE2-K mediate the excretion of organic cationic compounds from the plasma into the urine [8]. Metformin is excreted unmetabolized, primarily (≈ 86%) by MATE proteins [8].
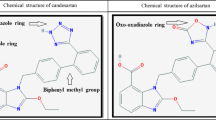
Baxdrostat (CIN-107) is a selective, small-molecule aldosterone synthase inhibitor that is in clinical development for use in the potential treatment of hypertension. As part of the renin-angiotensin-aldosterone system, aldosterone plays a critical role in the physiologic regulation of mineral and fluid homeostasis, which in turn is critical to the regulation of blood pressure (BP) [10,11,12]. Aldosterone is produced in the adrenal cortex in response to angiotensin II, adrenocorticotropic hormone (ACTH), and elevated extracellular potassium concentration [10,11,12]. Aldosterone activates mineralocorticoid receptors expressed in various tissues, leading to renal tubule reabsorption of sodium and water, thereby raising BP [10, 13].
Baxdrostat selectively inhibits aldosterone synthase (CYP11B2), the rate-limiting enzyme in the pathway of aldosterone synthesis, thereby reducing circulating aldosterone concentration. In vitro, baxdrostat was > 100-fold more selective for aldosterone synthase than for the homologous rate-limiting enzyme in the formation of cortisol, 11β-hydroxylase (CYP11B1) [14]. In vivo pharmacodynamic results from non-human primates showed that baxdrostat (1 and 7 mg/kg) inhibited aldosterone production without affecting cortisol levels [14]. Further, healthy human participants who received baxdrostat (1–360 mg) showed a significant dose-dependent reduction in aldosterone production with no meaningful effect on corticosterone or cortisol levels [14].
Using in vitro assays, the potential for interactions between baxdrostat and various uptake transport proteins including MATE transporters, organic anion transporters (OATs), organic cation transporters (OCTs), and cytochrome P450 (CYP) enzymes was tested. The results indicated that baxdrostat inhibited the function of MATE1 and MATE2-K, with half maximal inhibitory concentration (IC50) values of 1.34 µM and 2.67 µM, respectively; however, there was no evidence of interactions between baxdrostat and OATs, OCTs, or CYP enzymes (data on file). Therefore, if baxdrostat were concentrated in renal cells, co-administration of baxdrostat with a substrate for those transporters, such as metformin, could alter the renal elimination of the substrate and potentially increase circulating plasma levels of metformin. Given the potential for co-administration of metformin and baxdrostat, the objective of this study was to assess the impact of baxdrostat on the pharmacokinetics (PK) of metformin. Maximum observed plasma concentration (Cmax) and the area under the plasma concentration–time curve (AUC) of metformin were primary PK parameters along with a comparison of urine excretion of metformin in the presence and absence of baxdrostat. The PK characteristics of baxdrostat were also assessed to validate the results of our current study in comparison with previous studies. Safety and tolerability of the co-administration of both drug treatments were also evaluated.
2 Methods
2.1 Study Participants
To meet the inclusion criteria of this study, men and women between the ages of 18 and 55 years must have been in good health based on medical and psychiatric history, physical examination, electrocardiogram (ECG), vital signs, and routine laboratory tests (serum chemistry, hematology, and urinalysis). Study participants had a body mass index (BMI) ≥ 18 and ≤ 30 kg/m2, adequate renal function defined as estimated glomerular filtration rate ≥ 85 mL/min/1.73 m2, and no recent nicotine use.
Individuals were excluded from participation in this study if they had a personal or family history of long QT syndrome, complex ventricular arrythmias, current or past history of clinically significant arrhythmias, family history of sudden death, prolonged QTcF (> 450 ms), seated BP > 140/90 or < 90/50 mm Hg, a resting heart rate > 100 or < 50 beats per minute, sinus node dysfunction, clinically significant heart block, postural tachycardia, or orthostatic hypotension. Other exclusionary criteria included any clinical laboratory values meaningfully outside of normal limits; a history of clinically significant or multiple drug allergies; any prior episode of lactic acidosis; a radiologic scan with contrast within 14 days prior to the first dose of study drug; or a positive test for HIV antibody, hepatitis C virus antibody, hepatitis B surface antigen, or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA. Individuals were excluded if they reported any recent illicit drug use; drank more than 14 alcoholic beverages a week; used any prescription medications including topicals, herbal/dietary supplements, nutraceuticals, or over-the-counter medications (other than occasional use of acetaminophen or nonsteroidal anti-inflammatory drugs) within the longer of 14 days or 5 half-lives before the first dose of study drug and throughout the inpatient and discharge periods.
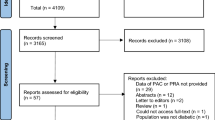
2.2 Study Design
This study was designed as a phase 1, randomized, open-label, 2-period crossover trial (Fig. 1). Each study participant participated in a screening period of up to 26 days followed by 2 inpatient treatment periods and a follow-up phone call. Study participants were randomized in a 1:1 ratio to treatment sequence AB or sequence BA for the 2 inpatient treatment periods. Treatment A was a single 1000-mg dose of metformin, and treatment B was a single 10-mg dose of baxdrostat followed by a single 1000-mg dose of metformin 2 h later. There was a minimum 10-day washout period between administration of the 2 treatments. Blood and urine sample collection for PK analysis began prior to dosing in each period and continued for 3 days after dosing in each period. Samples were collected 2, 1.5, 1, 0.5, and 0 h before dosing and 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, 12, 14, 16, 22, 24, 36, 48, and 72 h after dosing. Study participants received a follow-up phone call 3 ± 1 days after discharge from the clinic in the second dosing period.
Study design. Study participants were randomized to receive treatment A at dose 1 and treatment B at dose 2 (treatment sequence AB) or treatment B at dose 1 and treatment A at dose 2 (treatment sequence BA). Treatment A was a single 1000-mg dose of metformin, and treatment B was a single 10-mg dose of baxdrostat followed by a single 1000-mg dose of metformin 2 h later. PK pharmacokinetic
The current study was designed in accordance with US Food and Drug Administration (FDA) guidance on Assessment of Drug–Drug Interactions [16, 17]. As the therapeutic doses of baxdrostat (≤ 10 mg) are expected in the intended patient populations and the results of nonclinical assessments indicate that baxdrostat inhibition of the renal transporters MATE1 and MATE2-K is not time-dependent, a single 10-mg dose of baxdrostat was assessed in the current study. When co-administered, baxdrostat was given 2 h prior to administration of metformin to allow sufficient time for tissue distribution of baxdrostat in order to maximize the potential to detect an interaction, if one did exist. Metformin is approved for use at dosages up to 2550 mg daily, with an individual dose of immediate-release metformin typically not exceeding 1000 mg [15]. As such, a dose of 1000 mg of immediate-release metformin was used in the current study to maximize the potential of detecting an interaction.
2.3 Pharmacokinetics Analyses
All PK sample analyses were performed by Medpace Bioanalytical Laboratories (Cincinnati, OH, USA). PK parameters were calculated using noncompartmental methods with SAS software, version 9.4 (SAS Institute). Plasma PK parameters calculated for metformin, baxdrostat, and CIN-107-M included Cmax, time to Cmax (Tmax), AUC from time 0 to 24 h post-dose (AUC0–24), AUC from time 0 to last quantifiable plasma concentration (AUC0–t), AUC from time 0 to infinity (AUC0–inf), AUC0–inf extrapolated, terminal elimination rate constant (λz), and terminal phase elimination half-life (t½). Plasma AUC from time 0 to 72 h (AUC0–72) was assessed only for baxdrostat and CIN-107-M. Cmax, AUC0–inf, and AUC0–t were the 3 plasma PK parameters analyzed statistically to detect any interaction between baxdrostat and metformin. Urine PK parameters included amount excreted in urine (Ae), renal clearance (calculated as Ae/AUC), and the fraction of dose excreted renally.
2.4 Bioanalytical Methods
Plasma and urine samples were analyzed to measure concentrations of metformin, baxdrostat, and its primary metabolite, CIN-107-M, using validated liquid chromatography tandem mass spectrometry (LC-MS/MS) methods.
The quantifiable range for metformin in plasma was 0.5–500 ng/mL, using metformin-d6 as the internal standard. Plasma samples were extracted by protein precipitation with methanol, followed by analysis by LC-MS/MS with electrospray ionization in positive mode [ESI(+)] and multiple reaction monitoring (MRM). Reversed-phase chromatographic separation with a mobile phase gradient of 15–90% was utilized, and total run time was approximately 5 min. Precursor to product ion transitions for metformin and internal standard were 130.1–71.1 and 135.4–77.0, respectively. Similarly, the quantifiable ranges for metformin in urine were 1.00–500 ng/mL (low range) and 2.00–1250 ng/mL (high range), with similar extraction and LC-MS/MS conditions. Between-day precision (coefficient of variation [CV]%) values for metformin in plasma and urine were within 5% and 10%, respectively.
The quantifiable ranges for both baxdrostat and its metabolite CIN-107-M in plasma were 0.05–50 ng/mL (low range) and 5.00–2500 ng/mL (high range), using baxdrostat-d5 and CIN-107-M-d3, respectively, as the internal standards. Plasma samples were extracted by protein precipitation with methanol, followed by analysis by LC-MS/MS with ESI(+) and MRM. Reversed-phase chromatographic separation with a mobile phase gradient of 20–90% was utilized, and total run time was approximately 5 min. Precursors to product transition for baxdrostat and its internal standard were 364.2–291.2 and 369.2–291.2, respectively. The transitions for CIN-107-M and its internal standard were 309.2–291.2 and 313.2–295.2, respectively. Between-day precision (CV%) values for baxdrostat and CIN-107-M in plasma were within 3% and 4%, respectively.
2.5 Safety Analyses
Safety assessments included monitoring of adverse events (AEs), physical examinations, ECGs, orthostatic vital signs, and clinical laboratory evaluations.
2.6 Statistical Analyses
The safety population included all study participants who received a dose of any study treatment, whereas the PK evaluable population included all study participants who received any study treatment with sufficient plasma concentration data to characterize at least one PK parameter.
Descriptive statistics were used to summarize all results by treatment and collection time point. PK characterization also included geometric means and geometric coefficients of variation. Logarithmic transformations of PK parameters of metformin were analyzed using a mixed model including terms for treatment sequence, period as fixed effects, and subject nested within sequence as a random effect. Geometric means, geometric mean ratios, and associated 90% confidence intervals (CIs) are presented for plasma Cmax, AUC0–inf, and AUC0–t values for metformin following administration of metformin alone and metformin co-administered with baxdrostat. Geometric CIs were calculated using the formula CI = 100(exp(SD2) − 1)0.5, where SD is the standard deviation of the log-transformed data. If the 90% CIs of the geometric mean ratio were within 80–125% for Cmax, AUC0–inf, and AUC0–t, the absence of a drug–drug interaction was to be concluded.
The sample size for this study was determined under the hypothesis that co-administration of baxdrostat with metformin would not affect the PK characteristics of metformin. Thus, the geometric mean ratios of the Cmax and AUC of metformin in the presence or absence of baxdrostat should be 1, and the SD of the difference of PK characteristics should be 0.4 on a logarithmic scale. With 24 completed study participants, including 12 participants per treatment sequence with an intended correlation value of 0.55, the study would have 80% power to reject the null hypothesis of non-equivalence.
3 Results
3.1 Study Participants
Baseline demographics and clinical characteristics are presented in Table 1. Twenty-seven study participants were randomized into 2 cohorts, who received study drugs in treatment sequence AB or BA. Most study participants were White (56%) men (70%) who were not Hispanic or Latino. The average age was 37 years, and mean BMI was 25.6 kg/m2. Demographic and baseline characteristics were generally well matched in sex, race, and ethnicity between both treatment sequences.
3.2 Pharmacokinetics
The PK profile of metformin, when administered alone in the current study, was consistent with what would be expected based on the package insert for immediate-release metformin [15]. Furthermore, when administered after a dose of baxdrostat, metformin's plasma PK profile was both qualitatively and quantitatively similar to that of metformin alone (Fig. 2).
After confirming a lack of effect of treatment sequence, PK data for treatment A from all study participants were summarized, and PK data for treatment B from all study participants were summarized. Plasma and urine PK parameters after a dose of metformin alone or in the presence of baxdrostat are reported in Table 2. The 90% CIs of the geometric mean ratios for the plasma Cmax and AUC values for metformin in the presence of baxdrostat vs metformin alone fell entirely within the boundaries to claim bioequivalence (80–125%), demonstrating the absence of a PK drug–drug interaction [16, 17].
The urine PK parameters for metformin alone and in the presence of baxdrostat are presented in Table 3, and the Ae of metformin excreted following administration of metformin in the presence or absence of baxdrostat is presented in Fig. 3. The results confirmed that the renal excretion of metformin was not significantly affected by baxdrostat.
The PK parameters of baxdrostat and its primary metabolite (Table 4 and Fig. 4) were similar to previously published data, thereby demonstrating study validity [14]. The Cmax of baxdrostat was 118.9 ± 25.6 ng/mL, the Tmax was 1.7 ± 0.8 h, and λz was 0.033 ± 0.008 1/h.
3.3 Safety
There were no deaths, serious AEs, or discontinuations due to treatment-emergent adverse events (TEAEs), and the incidence and severity of AEs were similar when metformin was administered in the presence or absence of baxdrostat (Table 5). Overall, 7 study participants experienced a total of 15 TEAEs: 5 study participants (19.2%) experienced a total of 6 TEAEs following administration of metformin alone, and 6 study participants (22.2%) experienced a total of 9 TEAEs following dosing with metformin and baxdrostat. Four of these study participants experienced TEAEs following both treatments (metformin alone and metformin following a dose of baxdrostat).
All reported TEAEs were mild; no study participants experienced moderate or severe TEAEs. The most common TEAEs were gastrointestinal disorders. Five study participants (18.5%) reported diarrhea, an AE commonly associated with metformin treatment: 3 study participants (11.5%) following administration of metformin alone, 4 study participants (14.8%) following dosing of both metformin and baxdrostat, and 2 study participants following both treatments [15]. No clinically meaningful changes were observed in physical examinations, vital signs, ECGs (including no QT prolongation), or clinical laboratory results.
4 Discussion
The PK characteristics of metformin, including Cmax and AUC, when administered alone in the current study are consistent with previously published studies of metformin PK in healthy human participants when metformin was administered alone [18, 19]. Despite the preclinical findings that baxdrostat interacts with MATE proteins and could have potentially affected metformin elimination, the current study results showed that baxdrostat did not significantly affect the plasma PK or urine clearance of metformin. The 90% CIs of the geometric mean ratios for plasma Cmax and AUC in the presence of baxdrostat fell within 90–107% of those observed in the absence of baxdrostat. These values were within the FDA-recommended parameter limits for bioequivalence (80–125%) [16, 17]; thus, the absence of a drug–drug interaction was concluded. Previous in vitro data demonstrated that baxdrostat does not inhibit OCT-2, so the lack of an observed PK interaction between baxdrostat, a demonstrated MATE inhibitor, and metformin, a known MATE substrate, is consistent with the hypothesis that the inhibition of multiple transporters (e.g., MATE and OCT) may be required to produce meaningful PK interactions [20,21,22]. Renal clearance was similar between treatments, which suggests that the urinary transporter is not inhibited by baxdrostat. The clinical implication of these results is that patients with T2DM taking metformin may be administered baxdrostat for the management of their hypertension and are unlikely to require dosage adjustments of either drug.
An understanding of whether the in vitro data translate to a potential interaction in patients is important because metformin is prescribed for most patients with T2DM, including those with hypertension, and baxdrostat is currently undergoing development as a potential treatment for hypertension. As such, there is a high likelihood of their co-administration in patients with both T2DM and hypertension. In the context of a specific potential interaction, in which inhibition of a transporter necessary for clearance of metformin may increase exposure and pose a safety risk, the most critical plasma PK parameters would be Cmax, AUC, and the AUC ratio comparing the AUC of metformin before and after exposure to baxdrostat; these represent standard expected and required parameters for assessing PK interactions according to the US FDA [16, 17]. Additionally, comparison of urine excretion of metformin in the presence and absence of baxdrostat is critical to understand the impact on renal excretion.
The PK characteristics of baxdrostat were also assessed to validate the results of our current study in comparison with previous studies. The PK parameters of baxdrostat in the presence of metformin in the current study were similar to previously published data on the PK of baxdrostat alone [14]. In 2017, Bogman et al. reported an average hourly drug exposure (Cavg, calculated as AUC0–24/24) of 66 ± 5.9 ng/mL, which equates to an AUC0–24 of 1584 ng/mL [14]. Here we report an AUC0–24 of 1637 ng/mL with a Cavg of 68 ng/mL, which suggests that clinically relevant exposures of baxdrostat and its metabolite were attained. Further, the Tmax and rate of elimination were similar to those published by Freeman et al. [24]. The similarity of the PK of baxdrostat in the current study as compared with prior studies confirms the validity of the current study. Further, these data demonstrate that the PK of baxdrostat and its primary metabolite, which is not believed to contribute substantially to the therapeutic effects of baxdrostat, are unaffected by metformin, as would be expected based on our in vitro data.
Metformin and baxdrostat were well-tolerated when co-administered. The most common TEAEs were gastrointestinal (e.g., diarrhea), which was expected with a high dose of metformin. One study participant experienced a TEAE of postural dizziness following administration of metformin with baxdrostat that was considered related to metformin. Because no increase in incidence or severity of TEAEs was observed when study participants received metformin and baxdrostat compared with when they received metformin alone, baxdrostat does not appear to increase the risk of AEs when co-administered with metformin.
Strengths of this study include that the design, including dose levels and administration of baxdrostat sufficiently ahead of metformin to attain Cmax, was selected to maximize the chance of observing any interactions with metformin. Also, the study enrolled enough participants to be statistically powered to evaluate drug–drug interactions. The primary limitation of this study was that it was conducted in healthy individuals, such that further investigation is warranted to evaluate the safety and efficacy of baxdrostat in patients with comorbid hypertension and T2DM, particularly in patients with non-severe kidney disease.
5 Conclusions
The results of the current study demonstrated that single doses of metformin and baxdrostat were well-tolerated when co-administered to healthy individuals, with mostly mild gastrointestinal AEs observed, as was expected with a large dose of metformin. Baxdrostat did not significantly affect plasma concentrations or renal clearance of metformin. Therefore, diabetic patients with hypertension receiving metformin and baxdrostat are unlikely to require a dose adjustment of metformin due to a PK interaction.
References
Wang Z, Yang T, Fu H. Prevalence of diabetes and hypertension and their interaction effects on cardio-cerebrovascular diseases: a cross-sectional study. BMC Public Health. 2021;21(1):1224.
Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017–2018. NCHS Data Brief, no 364. Hyattsville, MD: National Center for Health Statistics; 2020.
Centers for Disease Control and Prevention. The facts, stats, and impacts of diabetes. https://www.cdc.gov/diabetes/library/spotlights/diabetes-facts-stats.html. Accessed 8 Jul 2022.
Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–52.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(1):S111–S24.
Drzewoski J, Hanefeld M. The current and potential therapeutic use of metformin-the good old drug. Pharmaceuticals (Basel). 2021;14(2):122.
Raval AD, Vyas A. National trends in diabetes medication use in the united states: 2008 to 2015. J Pharm Pract. 2020;33(4):433–42.
Yonezawa A, Inui K. Importance of the multidrug and toxin extrusion MATE/SLC47A family to pharmacokinetics, pharmacodynamics/toxicodynamics and pharmacogenomics. Br J Pharmacol. 2011;164(7):1817–25.
Tanihara Y, Masuda S, Sato T, Katsura T, Ogawa O, Inui K. Substrate specificity of MATE1 and MATE2-K, human multidrug and toxin extrusions/H(+)-organic cation antiporters. Biochem Pharmacol. 2007;74(2):359–71.
Marney AM, Brown NJ. Aldosterone and end-organ damage. Clin Sci (Lond). 2007;113(6):267–78.
Bomback AS, Klemmer PJ. The incidence and implications of aldosterone breakthrough. Nat Clin Pract Nephrol. 2007;3(9):486–92.
Deinum J, Riksen NP, Lenders JW. Pharmacological treatment of aldosterone excess. Pharmacol Ther. 2015;154:120–33.
Hargovan M, Ferro A. Aldosterone synthase inhibitors in hypertension: current status and future possibilities. JRSM Cardiovasc Dis. 2014;3:2048004014522440.
Bogman K, Schwab D, Delporte ML, Palermo G, Amrein K, Mohr S, et al. Preclinical and early clinical profile of a highly selective and potent oral inhibitor of aldosterone synthase (CYP11B2). Hypertension. 2017;69(1):189–96.
Glucophage (metformin hydrochloride). Package insert. Bristol-Myers Squibb Company; 2018.
US Food and Drug Administration. Statistical approaches to establishing bioequivalence: US Food and Drug Administration; 2001. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/statistical-approaches-establishing-bioequivalence. Accessed 25 Jul 2022.
US Food and Drug Administration. Bioequivalence studies with pharmacokinetic endpoints for drugs submitted under an abbreviated new drug application: US Food and Drug Administration; 2021. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioequivalence-studies-pharmacokinetic-endpoints-drugs-submitted-under-abbreviated-new-drug. Accessed 25 Jul 2022.
Yamazaki T, Desai A, Goldwater R, Han D, Lasseter KC, Howieson C, et al. Pharmacokinetic interactions between isavuconazole and the drug transporter substrates atorvastatin, digoxin, metformin, and methotrexate in healthy subjects. Clin Pharmacol Drug Dev. 2017;6(1):66–75.
Yi L, Zhang H, Zhang JW, You XM, Ning ZQ, Yu J, et al. Study on drug-drug interactions between chiglitazar, a novel PPAR pan-agonist, and metformin hydrochloride in healthy subjects. Clin Pharmacol Drug Dev. 2019;8(7):934–41.
Chen Y, Li S, Brown C, Cheatham S, Castro RA, Leabman MK, et al. Effect of genetic variation in the organic cation transporter 2 on the renal elimination of metformin. Pharmacogenet Genomics. 2009;19(7):497–504.
Morrissey KM, Stocker SL, Chen EC, Castro RA, Brett CM, Giacomini KM. The effect of nizatidine, a MATE2K selective inhibitor, on the pharmacokinetics and pharmacodynamics of metformin in healthy volunteers. Clin Pharmacokinet. 2016;55(4):495–506.
Stage TB, Brosen K, Christensen MM. A comprehensive review of drug-drug interactions with metformin. Clin Pharmacokinet. 2015;54(8):811–24.
Freeman MW, Bond M, Murphy B, Hui J, Isaacsohn J. Results from a phase 1, randomized, double-blind, multiple ascending dose study characterizing the pharmacokinetics and demonstrating the safety and selectivity of the aldosterone synthase inhibitor baxdrostat in healthy volunteers. Hypertens Res. 2023;46(1):108–18.
Acknowledgements
The authors would like to thank all study participants and Leela Vrishabhendra, MD, who was the principal investigator for this study. Technical and editorial support for this article was provided by MedLogix Communications, LLC, Itasca, IL, and funded by CinCor Pharma, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by CinCor Pharma, Inc.
Competing Interests
Mason Freeman, MD, is an employee of CinCor Pharma Inc. and receives stock-based compensation. Mary Bond, MS, MBA, is an employee of and has equity in CinRx Pharma, LLC, which has an equity stake in CinCor Pharma Inc. Brian Murphy, MD, MPH, is an employee of and has equity in CinRx Pharma, LLC, which has an equity stake in CinCor Pharma Inc. James Hui, PhD, is an employee of CinCor Pharma Inc. and receives stock-based compensation. Jonathan Isaacson, MD, is an employee of and has equity in CinRx Pharma, LLC, which has an equity stake in CinCor Pharma Inc.
Author Contributions
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Ethics Approval
The protocol and informed consent form were submitted to and approved by the Advarra Institutional Review Board prior to initiation of the study. A copy of the letter of approval and the institutional review board membership roster were received by the sponsor prior to any drug shipment. The study was conducted in accordance with the Declaration of Helsinki and with all applicable laws and regulations of the locale and country where the study was conducted and in compliance with Good Clinical Practice Guidelines.
Consent to Participate
The rationale of the study, procedural details, and investigational goals were explained to each study participant, along with potential risks and benefits. Each study participant was assured of their right to withdraw from the study at any time. Prior to the initiation of any study procedures, each study participant signed and dated an approved informed consent form. The original was kept on file by the investigator with the study participant’s records, and a copy was given to each study participant.
Consent for Publication
Not applicable.
Data Availability Statement
The data sets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Freeman, M.W., Bond, M., Murphy, B. et al. Results From a Randomized, Open-Label, Crossover Study Evaluating the Effect of the Aldosterone Synthase Inhibitor Baxdrostat on the Pharmacokinetics of Metformin in Healthy Human Subjects. Am J Cardiovasc Drugs 23, 277–286 (2023). https://doi.org/10.1007/s40256-023-00572-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-023-00572-x