Abstract
Objective
To evaluate the effect of rectal administration of buttermilk processed with medicinal plants on gut microbial composition and thereby on weight in obese individuals.
Methods
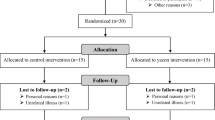
With ethics committee approval, 16 obese individuals in the age group 20–50 years (BMI ≥30 kg/m2) were recruited who received a course of 15-enemas over 15-days. Of these, 1st, 8th and 15th enemas were of sesame-oil administered after food, while other enemas were of buttermilk processed with medicinal plants administered before food. Outcome variables viz. anthropometry, body composition, blood glucose, insulin and lipid profile were evaluated on day 0, 16 and 45. Also, microbial composition of buttermilk preparation and faecal samples of patients collected on day 0, 16 and 45 were studied with the help of 16S rRNA gene sequencing.
Results
The circumferential measures and skinfold-thickness showed a decrease on day 16, which remained lower as compared to baseline till day 45. A gradual decrease in blood-glucose was seen, which was statistically significant on day 45, while insulin levels increased on day 16 and fell to baseline on day 45. There was an overall increase in bacterial diversity on day 16 that settled back to its original composition by day 45.
Conclusion
Our findings suggest that buttermilk administration per rectum is effective for a specific period and may have to be repeated for sustained benefits.







Similar content being viewed by others
References
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17.https://doi.org/10.1007/978-3-319-48382-5_1.
Heiss CN, Olofsson LE. Gut microbiota-dependent modulation of energy metabolism. J Innate Immun. 2018;10(3):163–71. https://doi.org/10.1159/000481519.
Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GA, Gasbarrini A, Mele MC. What is the healthy gut microbiota composition? a changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019;7(1):14. https://doi.org/10.3390/microorganisms7010014.
Crommen S, Simon MC. Microbial regulation of glucose metabolism and insulin resistance. Genes (Basel). 2018;9(1):16–22. https://doi.org/10.3390/genes9010010.
Tai N, Wong FS, Wen L. The role of gut microbiota in the development of type 1, type 2 diabetes mellitus and obesity. Rev Endocr Metab Disord. 2015;16(1):55–65. https://doi.org/10.1007/s11154-015-9309-0.
Patil DP, Dhotre DP, Chavan SG, Sultan A, Jain DS, Lanjekar VB, Gangawani J, Shah PS, Todkar JS, Shah S, Ranade DR, Patole MS, Shouche YS. Molecular analysis of gut microbiota in obesity among Indian individuals. J Biosci. 2012;37(4):647–57. https://doi.org/10.1007/s12038-012-9244-0.
Gonzalez S, Fernandez-Navarro T, Arboleya S, De Los Reyes-Gavilan CG, Salazar N, Gueimonde M. Fermented dairy foods: impact on intestinal microbiota and health-linked biomarkers. Front Microbiol. 2019;10. https://doi.org/10.3389/fmicb.2019.01046.
Jayashree S, Pushpanathan M, Rajendhran J, Gunasekaran P. Microbial diversity and phylogeny analysis of buttermilk, a fermented Milk product, employing 16S rRNA-based pyrosequencing. Food Biotechnol. 2013;27(3):213–21. https://doi.org/10.1080/08905436.2013.811084.
Chaudhari D, Dhotre D, Agarwal D, Gondhali A, Nagarkar A, Lad V, Patil U, Juvekar S, Sinkar V, Shouche Y. Understanding the association between the human gut, oral and skin microbiome and the Ayurvedic concept of prakriti. J Biosci. 2019;44(5):1–8. https://doi.org/10.1007/s12038-019-9939-6.
Chauhan NS, Pandey R, Mondal AK, Gupta S, Verma MK, Jain S, Ahmed V, Patil R, Agarwal D, Girase B, Shrivastava A, Mobeen F, Sharma V, Srivastava TP, Juvekar SK, Prasher B, Mukerji M, Dash D. Western Indian rural gut microbial diversity in extreme Prakriti endo-phenotypes reveals signature microbes. Front Microbiol. 2018;9:118. https://doi.org/10.3389/fmicb.2018.00118.
Steer E. A cross comparison between Ayurvedic etiology of major depressive disorder and bidirectional effect of gut dysregulation. J Ayurveda Integr Med. 2019;10(1):59–66. https://doi.org/10.1016/j.jaim.2017.08.002.
Aswathy Y, Anandaraman P. Therapeutic influence of some dietary articles on gut microbiota in the pathogenesis of rheumatoid arthritis (Amavata) – a review. AYU. 2019;40(3):147. https://doi.org/10.4103/ayu.ayu_192_19.
Mallikarjun, Channabasavanna BM. Srinivasulu. A clinical study on Takra Basti in the management og grahani W.S.R To I.B.S. prayeshana. Int J Ayu Res. 2017;2(2)26–34.
Gupte P, Harke S, Deo V, Bhushan Shrikhande B, Mahajan M, Bhalerao S. A clinical study to evaluate the efficacy of herbal formulation for obesity (HFO-02) in overweight individuals. J Ayurveda Integr Med. 2020;11(2):159–62. https://doi.org/10.1016/j.jaim.2019.05.003.
Thatte U, Chiplunkar S, Bhalerao S, Kulkarni A, Ghungralkar R, Panchal F, Vetale S, Teli P, Kumbhar D, Munshi R. Immunological & metabolic responses to a therapeutic course of Basti in obesity. Indian J Med Res. 2015;142:53–62. https://doi.org/10.4103/0971-5916.162099.
Dhariwal A, Chong J, Habib S, King IL, Agellon LB, Xia J. MicrobiomeAnalyst: a web-based tool for comprehensive statistical, visual and meta-analysis of microbiome data. Nucleic Acids Res. 2017;45(W1):W180–8. https://doi.org/10.1093/nar/gkx295.
Zhang J, Kobert K, Flouri T, Stamatakis A. PEAR: a fast and accurate Illumina paired-end reAd mergeR. Bioinformatics. 2014;30(5):614–20. https://doi.org/10.1093/bioinformatics/btt593.
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–3. https://doi.org/10.1038/nmeth.3869.
Quast C, Pruesse E, Yilmaz P, Gerken J, Schweer T, Yarza P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41(D1):590–6. https://doi.org/10.1093/nar/gks1219.
Iwai S, Weinmaier T, Schmidt BL, Albertson DG, Poloso NJ, Dabbagh K, Desantis T. Piphillin: improved prediction of metagenomic content by direct inference from human microbiomes. PLoS One 2016;11(11):1–18. https://doi.org/10.1371/journal.pone.0166104.
Kho ZY, Lal SK. The human gut microbiome - a potential controller of wellness and disease. Front Microbiol. 2018;9:1–23. https://doi.org/10.3389/fmicb.2018.01835.
Rezac S, Kok CR, Heermann M, Hutkins R. Fermented foods as a dietary source of live organisms. Front Microbiol. 2018;9. https://doi.org/10.3389/fmicb.2018.01785.
George Kerry R, Patra JK, Gouda S, Park Y, Shin HS, Das G. Benefaction of probiotics for human health: a review. J Food Drug Anal. 2018;26(3):927–39. https://doi.org/10.1016/j.jfda.2018.01.002.
Barukcic I, Jakopovic KL, Bozanic R. Valorisation of whey and buttermilk for production of functional beverages - an overview of current possibilities. Food Technol Biotechnol. 2019;57(4):448–60. https://doi.org/10.17113/ftb.57.04.19.6460.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity Committee of the Council on nutrition. Physical Circulation. 2006;113(6):898–918. https://doi.org/10.1161/CIRCULATIONAHA.106.171016.
Lee YH, Lee HW, Choi HJ. GLP-1 based combination therapy for obesity and diabetes. J Obes Metab Syndr. 2017;26(3):155–60. https://doi.org/10.7570/jomes.2017.26.3.155.
Cornejo-Pareja I, Martín-Núñez GM, Roca-Rodríguez MM, Cardona F, Coin-Aragüez L, Sánchez-Alcoholado L, Gutiérrez-Repiso C, Muñoz-Garach A, Fernández-García JC, Moreno-Indias I, Tinahones FJ. H. pylori eradication treatment alters gut microbiota and GLP-1 secretion in humans. J Clin Med. 2019;8(4):451. https://doi.org/10.3390/jcm8040451.
Hossain FB, Shawon SR, Adhikary G, Chowdhury A. Association between body mass index (BMI) and hypertension in South Asian population: evidence from demographic and health survey. Clin Hypertens. 2019;25:28. https://doi.org/10.1101/605469.
Pérez-Pérez A, Sánchez-Jiménez F, Vilariño-García T, Sánchez-Margalet V. Role of leptin in inflammation and vice versa. Int J Mol Sci. 2020;21(16):1–24. https://doi.org/10.3390/ijms21165887.
Duncan SH, Lobley GE, Holtrop G, Ince J, Johnstone AM, Louis P, et al. Human colonic microbiota associated with diet, obesity and weight loss. Int J Obes. 2008;32(11):1720–4. https://doi.org/10.1038/ijo.2008.155.
Nadal I, Santacruz A, Marcos A, Warnberg J, Garagorri JM, Moreno LA, Martin-Matillas M, Campoy C, Martí A, Moleres A, Delgado M, Veiga OL, García-Fuentes M, Redondo CG, Sanz Y. Shifts in clostridia, bacteroides and immunoglobulin-coating fecal bacteria associated with weight loss in obese adolescents. Int J Obes. 2009;33(7):758–67. https://doi.org/10.1038/ijo.2008.260.
Tims S, Derom C, Jonkers DM, Vlietinck R, Saris WH, Kleerebezem M, et al. Microbiota conservation and BMI signatures in adult monozygotic twins. ISME J. 2013;7(4):707–17. https://doi.org/10.1038/ismej.2012.146.
Koliada A, Syzenko G, Moseiko V, Budovska L, Puchkov K, Perederiy V, et al. Association between body mass index and Firmicutes/Bacteroidetes ratio in an adult Ukrainian population. BMC Microbiol. 2017;17(1):4–9. https://doi.org/10.1186/s12866-017-1027-1.
Schwiertz A, Taras D, Schäfer K, Beijer S, Bos NA, Donus C, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity [Internet]. 2010;18(1):190–5. https://doi.org/10.1038/oby.2009.167.
Magne F, Gotteland M, Gauthier L, Zazueta A, Pesoa S, Navarrete P, Balamurugan R. The firmicutes/bacteroidetes ratio: a relevant marker of gut dysbiosis in obese patients? Nutrients. 2020;12(5)1474. https://doi.org/10.3390/nu12051474.
Donohoe DR, Garge N, Zhang X, Sun W, O’Connell TM, Bunger MK, et al. Microbiome, the regulate, butyrate metabolism. Energy Cell Metab. 2011;13(5):517–26. https://doi.org/10.1016/j.cmet.2011.02.018.
Litvak Y, Byndloss MX, Bäumler AJ. Colonocyte metabolism shapes the gut microbiota single sentence summary. Science. 2018;36(6418). https://doi.org/10.1126/science.aat9076.
Jun X, Chen HB, Li SL. Understanding the molecular mechanisms of the interplay between herbal medicines and gut microbiota. Med Res Rev. 2017;37(5):1140–185. https://doi.org/10.1002/med.21431.
Lu YM, Xie JJ, Peng CG, Wang BH, Wang KC, Li LJ. Enhancing clinical efficacy through the gut microbiota: a new field of traditional Chinese medicine. Engineering. 2019;5(1):40–9. https://doi.org/10.1016/j.eng.2018.11.013.
Acknowledgements
The authors would like to thank Miss. Simran Kaur Cheema (Intern at NCMR-NCCS) and Mr. Deepak Khairnar (Research fellow at NCMR-NCCS) for their help in DNA extraction from stool and buttermilk samples.
Author information
Authors and Affiliations
Contributions
SM- Contributed for anthropometry assessment, coordination among all three study sites, management of data, manuscript drafting and revision.
KKD- Contributed for stool and buttermilk DNA extractions, microbiome data generation and analysis, manuscript drafting and revision.
NL- Contributed for Study drug preparation, patient recruitment and treatment procedure follow up of patients, clinical assessment.
PK- Contributed for Ethical approval and CTRI registration, counselling of participants and supervision of clinical part.
DD- Contributed for Supervision of conduct and data interpretation of microbiome study, manuscript revision.
YSS- Contributed for Critical inputs in planning the study, approval for microbiome study and analysis methodology, manuscript revision.
SB- Contributed for Study conception and design, data monitoring, data analysis and interpretation, manuscript revision.
Corresponding authors
Ethics declarations
Institutional Ethics Committee BVDUCOA/EC/−3482/2017–18.
Clinical Trial Registry of India CTRI/2018/02/011859.
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(XLSX 176 kb)
Rights and permissions
About this article
Cite this article
Mane, S., Dixit, K.K., Lathwal, N. et al. Rectal administration of buttermilk processed with medicinal plants alters gut microbiome in obese individuals. J Diabetes Metab Disord 20, 1415–1427 (2021). https://doi.org/10.1007/s40200-021-00879-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00879-z