Abstract
Introduction
Depression is the most common psychiatric disorder in patients with type 2 diabetes. There are many questionnaires to measure depression symptoms. These tools are generally used with the same cut-off points in different medical diseases. The present study investigates the optimal cut-off points of these tools in patients with type 2 diabetes in the Iranian diabetic population. The original version of this tool is prepared in Persian.
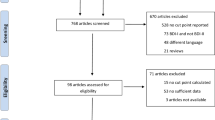
Method
Two-hundred and forty four patients with a diagnosis of diabetes were selected to participate in the study. The gold standard for diagnosing depression was the Structured Mini-International Neuropsychiatric Interview. We applied the cut-off points of the Persian versions of the Hospital Anxiety and Depression Scale (HADS), Beck Depression Inventory (BDI), Depression in Diabetes Self-Rating Scale (DDS-RS), Problematic Areas in Diabetes Survey (PAID), Hamilton Depression Rating Scale (HDRS) and Depression in Diabetes Self-Rating Scale (DDS-RS).
Results
23.8% of patients were diagnosed with depression. Depressed patients had higher levels of HbA1c and physical complaints than non-depressed patients. In all tools, the sum of Sensitivity and Specificity of our proposed cut-off points was better than the conventional cut-off points. In HADS, the results showed that this questionnaire performed better and more efficiently than other tools.
Conclusion
In patients with type 2 diabetes, it is better to use the proposed cut-off point’s specific to this disorder in the Iranian population. These cut-off points have a higher ability to identify depressed and non-depressed cases.





Similar content being viewed by others
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
Kalra G, Gill S, Tang TS. Depression and diabetes distress in South Asian adults living in low- and middle-income countries: a scoping review. Can J Diabetes. 2020;44(6):521-9.e1.
Wu CS, Hsu LY, Wang SH. Association of depression and diabetes complications and mortality: a population-based cohort study. Epidemiol Psychiatric Sci. 2020;29:e96.
Rodríguez Calvín JL, Zapatero Gaviria A, Martín Ríos MD. Prevalence of depression in type 2 diabetes mellitus. Revista Clínica Española (English Edition). 2015;215(3):156–64.
Palizgir M, Bakhtiari M, Esteghamati A. Association of depression and anxiety with diabetes mellitus type 2 concerning some sociological factors. Iran Red Crescent Med J. 2013;15(8):644–8.
Ciechanowski P, Russo J, Katon W, Von Korff M, Ludman E, Lin E, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med. 2004;66(5):720–8.
Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–72.
Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31(12):2398–403.
Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278–85.
Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with Type 2 diabetes. Diabetic Med: J Br Diabetic Assoc. 2008;25(9):1096–101.
Pouwer F, Beekman AT, Lubach C, Snoek FJ. Nurses’ recognition and registration of depression, anxiety and diabetes-specific emotional problems in outpatients with diabetes mellitus. Patient Educ Couns. 2006;60(2):235–40.
Hermanns N, Kulzer B, Krichbaum M, Kubiak T, Haak T. How to screen for depression and emotional problems in patients with diabetes: comparison of screening characteristics of depression questionnaires, measurement of diabetes-specific emotional problems and standard clinical assessment. Diabetologia. 2006;49(3):469–77.
Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiat. 2003;54(3):241–7.
Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63 Suppl 11(011):S467–72.
Tyson RL, Brammer S, McIntosh D. Telehealth in psychiatric nursing education: lessons from the field. J Am Psychiatr Nurses Assoc. 2019;25(4):266–71.
Barloon LF, Hilliard W. Legal considerations of psychiatric nursing practice. Nurs Clin North Am. 2016;51(2):161–71.
Bujang MA, Adnan TH. Requirements for minimum sample size for sensitivity and specificity analysis. J Clin Diagn Res. 2016;10(10):YE01–6. https://doi.org/10.7860/JCDR/2016/18129.8744.
Hedman E, Lekander M, Ljótsson B, Lindefors N, Rück C, Andersson G, et al. Optimal cut-off points on the health anxiety inventory, illness attitude scales and whiteley index to identify severe health anxiety. PLoS ONE. 2015;10(4):e0123412.
Kawada T. Questionnaire survey on depression for patients with heart failure: validation for selecting appropriate cut-off points. Int J Cardiol. 2012;157(2):275.
Arzaghi SM, Mahjouri MY, Heshmat R, Khashayar P, Larijani B. Psychometric properties of the Iranian version of the Problem Areas in Diabetes scale (IR-PAID-20). J Diabetes Metab Disord. 2011;10:1.
Kaviani H, Mousavi A. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran Univ Med J TUMS Publ. 2008;66(2):136–40.
Ahmadpanah M, Sheikhbabaei M, Haghighi M, Roham F, Jahangard L, Akhondi A, et al. Validity and test-retest reliability of the Persian version of the Montgomery-Asberg Depression Rating Scale. Neuropsychiatr Dis Treat. 2016;12:603–7.
Zimmerman M, Martinez JH, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton depression rating scale. J Affect Disord. 2013;150(2):384–8.
Asghari A, Saed F, Dibajnia P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int J Psychol. 2008;2(2):82–102.
Baradaran HR, Mirghorbani SM, Javanbakht A, Yadollahi Z, Khamseh ME. Diabetes distress and its association with depression in patients with type 2 diabetes in Iran. Int J Prev Med. 2013;4(5):580–4.
Safaralizadeh F, Partovazam H. The correlation between depression and body mass index in female teenagers of Khoy during year 2009. Community Health Journal. 2017;5(1):17–24.
Cichoń E, Kiejna A, Kokoszka A, Gondek TM, Radzio R, Jastrzębski A, et al. People with diabetes need a lower cut-off than others for depression screening with PHQ-9. PLoS One. 2020;15(10):e0240209. https://doi.org/10.1371/journal.pone.0240209.
Kokoszka A, Cichoń E, Obrębski M, Kiejna A, Rajba B. Cut-off points for Polish-language versions of depression screening tools among patients with type 2 diabetes. Prim Care Diabetes. 2020;14(6):663–71.
Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J. 2012;27(4):269.
Davoudi M, Taheri AA, Foroughi AA, Ahmadi SM, Heshmati K. Effectiveness of acceptance and commitment therapy (ACT) on depression and sleep quality in painful diabetic neuropathy: a randomized clinical trial. J Diabetes Metab Disorders. 2020:1–8.
Marso SP. The handbook of diabetes mellitus and cardiovascular disease. Limassol: Remedica; 2003.
Williams G, Pickup JC. Handbook of diabetes. Hoboken: Blackwell Publication; 2004.
Janghorbani M, Van Dam RM, Willett WC, Hu FB. Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol. 2007;166(5):495–505.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Before administering the investigation, an individual session was held to justify all participants. In these sessions, ethical issues and explanations about the investigation were given to the individuals. Then, a consent form was obtained for all patients. Participants were convinced that their data and identities would be kept private. All procedures used in collecting survey data on which this article relies on, are in accordance with the ethical standards of the Helsinki Declaration of 1964 and subsequent amendments or ethical standards.
Consent for publication
Consent letter for publishing data was also received from participants.
Conflicts of interest
The authors certify that they have no competing interests.
Human and animal rights
Current research does not contain any interventions or studies with animals executed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tamrchi, S., Davoudi, M., Khosrojerdi, Z. et al. Clarification the optimal cut-off values for Persian-language versions of depression screening tools in Iranian patients with type 2 diabetes. J Diabetes Metab Disord 20, 1359–1367 (2021). https://doi.org/10.1007/s40200-021-00866-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00866-4