Abstract
Objectives
Type 2 diabetes mellitus (T2DM) is sustained by insulin resistance (IR) and reduced β-cell mass, which is largely due to insulin secretory dysfunction. Wnt5a protein is essential to islet formation and β-cell migration in the development of pancreas in vertebrates. Levels of the Wnt5a protein antagonist plasma secreted frizzled-related protein 5 (Sfrp5) were elevated in patients with T2DM. However, the association between Wnt5a, T2DM patients and diabetic kidney disease (DKD) is unknown. We aim to investigate the circulating Wnt5a levels in in different clinical stages of T2DM and evaluate its correlation of duration of diabetes mellitus chronic complication.
Methods
A total of 329 participants (187 males, 142 females; age range 40 to 80 years) were enrolled in this study. Serum Wnt5a levels were measured by an enzyme-linked immunosorbent assay (ELISA). The demographic and clinical parameters evaluated in subjects with new onset T2DM, onset T2DM after treatment and DKD at different clinical phases.
Results
Wnt5a was significantly down-regulated in newly diagnosed T2DM patients and gradually increased after 3 months of treatment. Interesting, serum wnt5a was gradually increased in patients with long-term diabetes and kidney disease compared to patients with T2DM and onset DKD.
Conclusions
We speculated that the Wnt5a protein might regulate islet function and be involved in the onset of diabetes as a protective factor. It may be one of the inflammatory factors adversely involved in the progression of diabetic nephropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is one of the most prevalent metabolic disorders in the world, with an estimated 113.9 million adults in China, and we can clearly see that the incidence rate is also dramatically rising with time [1]. The prevalence rate for prediabetes among Chinese adults reported a rate of over 50% [2]. This metabolic disorder not only affects health and quality of life, but can also bring serious physical, psychological and economical burdens to individuals and governments for a variety of chronic complications, such as macrovascular and microvascular complications. Among these complications, renal involvement occurs in a subset of diabetic patients, often playing a key role in morbidity and mortality [3]. Multiple factors have been proposed to cause pathological changes in diabetes mellitus and its renal complications. Previous studies have shown that low-grade chronic inflammation and activation of the renin-angiotensin system (RAS) all accelerate the development of diabetes and its renal complications [4, 5]. However, it is disappointing that the exact pathogenesis leading to T2DM and DKD remain not fully elucidated.
Recently, A lot of evidence has been demonstrated that the contribution of Wnt signalling in both the development and progression of T2DM and DKD. Wnt5a is involved in several non-canonical Wnt signaling pathways, through binding to its receptor Frizzled-5 (Fzd5), acts as a critical regulator in a host of developmental processes and diverse pathogenic situations, such as cancer, fibrosis, and inflammation, and it promotes renal interstitial fibrosis [6,7,8,9]. Wnt5a/Fzd5 signalling pathway plays a key role in proper insulin-cell migration and development of pancreatic islet [10]. Previous study demonstrated that levels of the Wnt5a protein antagonist plasma secreted frizzled-related protein 5 (Sfrp5) were elevated in patients with T2DM [11]. Interestingly, our recent in vitro study investigated that high expression of Wnt5a and Fzd5 could be found in islet stellate cells isolated from db/m mice, and wnt5a increased the secretion of insulin after co-culture with β cells [12]. However, the role of Wnt5a protein has not been studied in T2DM and DKD.
In this study, we analysed the expression of wnt5a protein in the presence of T2DM and its chronic complications to determine its association and clinical significance.
Methods
Patient recruitment and exclusion criteria
This study was carried out at the endocrinology department of Xuzhou Central Hospital from June 2016 to June 2017 in line with the principles enunciated in the Declaration of Helsinki. This study was reviewed and approved by the Ethical Committees of Xuzhou Central Hospital. Written informed consent was obtained from all of the participants.
A total of 109 consecutive patients with onset T2DM, 110 patients with DKD and 110 normal control patients participated in the study. The diagnosis of T2DM was based on the American Diabetes Association (ADA) 2014 criteria. Patients with onset T2DM had a plasma fasting glucose level > 7.0 mmol/L or 2 h values in the OGTT >11.1 mmol/L) without a previous diabetes diagnosis and were given lifestyle improvement and metformin treatment for 3 months.
Microalbuminuria has been defined as 30 to 300 mg of albumin in a 24-h urine collection, DKD was defined as either the presence of microalbuminuria (30 to 299 mg albumin/24 h or an albumin to creatinine ratio [ACR] of 30 to 299 mg/g) or macroalbuminuria (> 300 mg albumin/24 h or ACR > 300 mg/g). The DKD I/II/III groups were defined as having ACR ≤ 29 mg/g (ACR1 group), 30 to 299 mg/g (ACR2 group) and ≥ 300 mg/g (ACR3 group), respectively.
The participants underwent a routine medical examination. Subjects meeting any of the following criteria were excluded from this study: (1) T1DM; (2) acute complications of diabetes, such as diabetic ketoacidosis, hyperglycaemic hyperosmolar state, lactic acidosis and hypoglycaemic coma; (3) history of other disease known to be associated with nephropathy besides DKD; (4) pregnancy; (5) Patients with heart failure, haematologic disease, liver dysfunction, or taking steroids were also excluded.
Biochemical assays
Whole blood samples were collected into 5 ml Vacutainer tubes from the control veni-puncture after an overnight fast. In the onset T2DM and DKD groups, the blood samples were drawn on admission before treatment with blood and at the time of discharge from the hospital. The blood samples were drawn again for the onset T2DM group treated by lifestyle improvement and metformin for 3 months. Laboratory tests were performed using laboratories’ routine clinical methods in the hospital laboratory. HbA1c was measured with an HbA1c Meter from Bio-Rad Laboratories, Ltd. (Shanghai, China), with reference value mmol/mol. The concentrations of plasma Wnt5a were detected using the ELISA kit (ISBio, United States of America). The analytical sensitivities were 1.0 ng/mL for Wnt5a.
Statistical methods
Data are shown as the mean ± standard deviation (SD). SAS statistical software (version 9.1; SAS Institute, Inc.) was used for data management and statistical analyses. Analysis of variance (ANOVA) statistical technique is conducted to examine differences between groups. Correlations of Wnt5a and clinical parameters were performed using Pearson’s correlations or Spearman’s rank correlation coefficient. The odds ratio (OR) of Wnt5a for DKD was determined by logistic regression models adjusted for covariates, including age, BMI, SBP, DBP, FBG, TG, TC, HDL and LDL. All reported P-values are two-tailed. Variables with P-values <0.05 were considered statistically significant.
Results
Participants and baseline characteristics
A total of 329 subjects (187 males, 142 females; age range 40–80 years) participated in the study. The baseline demographic and clinical characteristics of the three enrolled populations are summarized in Table 1. The glycaemic variables were significantly higher in the two diabetic patient groups (plasma glucose: 7.28 ± 2.64 mmol/L and 8.04 ± 3.07 mmol/L, respectively; HbA1c: 7.84 ± 3.37% and 8.3 ± 4.23%, respectively, for onset T2DM and DKD) than in the control group (plasma glucose: 5.14 ± 1.32 mmol/L, HbA1c: 5.21 ± 1.87%) (all P < 0.001). With respect to age and gender, there were no significant differences among the three groups. The BMIs were significantly higher in the two diabetic patient groups (27.9 ± 9.28 and 25.4 ± 4.03 for onset T2DM and DKD, respectively) than in the control group (22.1 ± 3.54). Both the systolic and diastolic blood pressures were lower in the control group and higher in the onset T2DM and DKD group (P < 0.001).
Wnt5a levels decreased in onset T2DM and gradually increased after treatment
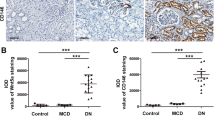
We measured fasting serum Wnt5a levels in the subjects with onset T2DM and onset T2DM after treatment using a newly developed ELISA assay (Table 2 and Fig. 1a, c). Wnt5a levels decreased in the diabetic group patients compared to healthy controls (64.73 ± 8.49 ng/ml versus 69.38 ± 5.68 ng/ml, P < 0.001), and increased Wnt5a was detected after 3 months of treatment (64.73 ± 8.49 ng/ml versus 67.52 ± 3.06 ng/ml, P < 0.001).
Serum levels of Wnt5a in different groups of the study population. a Wnt5a serum levels decreased significantly in newly diagnosed (64.73 ± 8.49 ng/ml, p < 0.001) and T2DM with DKD patients (50.42 ± 10.46 ng/ml, p < 0.001) compared to healthy controls (69.38 ± 5.68 ng/ml). Data are presented as the means ± SD, *p < 0.05, **p < 0.001. b Wnt5a serum levels increased slightly in DKDII (ACR ≥ 30, ACR ≤ 299) (51.34 ± 4.30 ng/ml, p < 0.001) and DKDIII (ACR ≥ 300) (63.89 ± 2.57 ng/ml, p < 0.001) compared to DKDI (38.02 ± 4.02 ng/ml). Data are presented as the means ± SD, *p < 0.05, **p < 0.001. c Wnt5a serum levels increased significantly after treatment with lifestyle improvement and metformin for 3 months (67.52 ± 3.06 ng/ml, P < 0.001, p < 0.001) compared to onset T2DM patients (64.73 ± 8.49 ng/ml). Data are presented as the means ± SD, *p < 0.05, **p < 0.001
Wnt5a levels changed with the duration of DKD
Wnt5a levels were clearly decreased in DKD patients compared to onset T2DM and healthy controls (50.42 ± 10.46 ng/ml versus 69.38 ± 5.68 ng/ml and 64.73 ± 8.49 ng/ml, P < 0.001) (Fig. 1a and Table 3). A negative correlation between FBG, 2hPG, HbA1c and Wnt5a was also found in all the participants (r = −0.349, −0.435, −0.382, respectively) (Fig. 2a, b, c). However, there was no association between Wnt5a and age, gender, BMI and the systolic and diastolic blood pressures.
Notably, we found that Wnt5a levels were gradually higher in the DKD II/III group compared with those in DKD I group (51.34 ± 4.30 ng/ml and 63.89 ± 2.57 ng/ml versus 38.02 ± 4.02 ng/ml, P < 0.001) (Fig. 1b). There was a positive correlation between Wnt5a and ACR. In the logistic regression model adjusted for age and BMI, the odds ratio [OR, 95% confidence interval (95%CI)] was 1.12 (1.081~1.177). After further adjustment for SBP, DBP and FBG, the odds ratio was 1.321 (1.21~1.492). In the three models adjusted for age, BMI, SBP, DBP, FBG, TG, TC, HDL and LDL, the odds ratio was 1.422 (1.271~1.658) (Table 4).
Discussion
The present study analysed wnt5a levels in patients with different stages of T2DM. First, patients with early onset T2DM and DKD had significantly decreased wnt5a levels. However, our study also provided interesting evidence that wnt5a gradually increased in long-term T2DM patients with kidney disease. To our knowledge, this is the first report to describe the expression of wnt5a protein playing difference roles in the presence of T2DM and its chronic kidney complications.
In the present study, we have shown that Wnt5a gradually decreased in patients with onset diabetes and gradually increased after treatment with lifestyle improvement and metformin for 3 months, albeit at a relatively high level under normal conditions, which may provide some insight into one mechanism by which Wnt5a protein may influence development of T2DM. The causes of type 2 diabetes include both genetic, lifestyle and environmental elements that affect β-cell function and insulin sensitivity [13]. However, the mechanisms controlling the interplay of these three impairments remain not fully elucidated. Previous studies have shown that the deposition of islet amyloid and low-grade chronic inflammation all associated with the procession of T2DM [14]. Numerous pro-inflammatory cytokines such as IL-1b, TNF-a, and IL-6 is the most promising part for development of T2DM. These cytokines released from adipose tissues induce inflammation not only in the corresponding tissue but also in the β-cells of pancreatic islets and block the activation of insulin signaling receptors, ultimately linked to insulin resistance [15,16,17].
Wnt5a is involved in several non-canonical Wnt signaling pathways, and it is a prototypical wnt of the β-catenin-independent branch, which is highly conserved among species and plays key roles in numerous biological processes. Wnt5a signalling is associated with several human pathologies such as pulmonary fibrosis, renal fibrosis, post-infarct cardiac remodelling and hypertrophic scars [18,19,20,21,22]. Several studies suggested that wnt5a is also expressed in mammalian adipose tissue and expression in mice was induced by a high-fat diet and obesity [23]. Wnt5a/Fzd5 signalling plays a role in proper insulin-cell migration and islet formation during vertebrate pancreatic development [10]. Plasma levels of the Wnt5a protein receptor Sfrp5 were elevated in patients with T2DM [11]. However, the underlying mechanisms of Wnt5a-β cells in diabetes remain to be elucidated. Interestingly, our recent in vitro study showed that Wnt5a protein expression from islet stellate cells (ISCs) was higher in db/m mice than in db/db mice, and Wnt5a increased the secretion of insulin by co-culture with islets; the results revealed that the Wnt5a protein is a key modulator of ISC-mediated maintenance of islet function [12].
In the current study, we found negative correlations between wnt5a levels and HbA1c, as well as fasting blood glucose (FBG) and 2-h postprandial glucose (2hPG), implying that the decreased wnt5a levels might have a close association with insulin resistance and β cell dysfunction. The decreased wnt5a level observed in patients with onset T2DM in this study may suggest that changes in the wnt5a level represent a regulatory mechanism to counteract metabolic stress and β cell dysfunction in diabetes. The results revealed that Wnt5a protein maybe a key modulator in the development of T2DM.
Our studies have identified that patients with CKD have significantly decreased Wnt5a levels. However, our studies have also revealed that Wnt5a levels were gradually higher in the DKD II/III group than in the DKD I group. Diabetic kidney disease (DKD) is one of the most frequent and dangerous microvascular complications in diabetes mellitus and is independently correlated with an increased risk of developing end stage renal failure (ESRD) [24,25,26]. Multiple factors have been proposed to cause pathological changes in T2DM patients with kidney disease, such as the interactions between hyperglycaemia-induced hemodynamic and metabolic disorders, as well as the accumulation of extracellular matrix (ECM) proteins in the kidney microenvironment [27]. However, the exact pathogenesis controlling the DKD remain not fully elucidated. Wnt/β-catenin signaling pathway is re-activated in a wide variety of animal models of proteinuric kidney and in human kidney disorders [28,29,30,31]. Whereas some study demonstrated to a protective role of Wnt signalling in repair after acute kidney injury, Emerging evidence suggests that sustained activation of Wnt/β-catenin is associated with the development and progression of renal fibrosis [32,33,34,35,36]. However, the Wnt/β-catenin mechanisms controlling interplay of DKD are unclear. In the present study, we analysed wnt5a levels in patients with DKD and revealed a close relationship between wnt5a levels and DKD patients. Serum wnt5a was gradually increased in long-term diabetes patients with kidney disease compared to T2DM with onset DKD patients. More importantly, these results further imply that wnt5a signalling may play an important role in facilitating the development and progression of DKD. However, this needs to be clarified in future studies. The mechanisms underlying diabetes and its microvascular chronic complications are multiple and complex, and our study population was relatively small. Thus, Further studies with larger populations are required to elucidate fully the role of Wnt5a in patients with different stages of T2DM. We speculate that the Wnt5a protein may regulate islet function and be involved in the onset of diabetes as protective factors. It may be one of the inflammatory factors adversely involved in the progression of diabetic nephropathy.
Some limitations of this study need to be considered. First, owing to its observational characteristic, this hypothesis requires a randomized, controlled trial to definitively determine the role of Wnt5a in patients with T2DM. Finally, the exact origin of decreased Wnt5a in onset T2DM and gradually increased trend in DKD patients is unknown. Thus, further studies with larger populations and basic research are required.
In conclusion, we report that Wnt5a levels correlated with the duration of diabetes. Therefore, Wnt5a might play an important role in the development of type 2 diabetes mellitus and its renal complications. Future trials are required to reassess performance and evaluate the mechanisms of Wnt5a-β cell-microvascular complications.
References
Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31–40.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Singh S, Sonkar SK, Sonkar GK, et al. Diabetic kidney disease: a systematic review on the role of epigenetics as diagnostic and prognostic marker. Diabetes Metab Res Rev. 2019;20:e3155.
Gonzalez LL, Garrie K, Turner MD. Type 2 diabetes - an autoinflammatory disease driven by metabolic stress. Biochim Biophys Acta Mol basis Dis. 2018;1864(11):3805–23.
Shen J, Huang YM, Song XN, et al. Protection against death and renal failure by renin-angiotensin system blockers in patients with diabetes and kidney disease. J Renin-Angiotensin-Aldosterone Syst. 2016;17(3):1470320316656481.
Asem MS, Buechler S, Wates RB, et al. Wnt5a signaling in cancer. Cancers (Basel). 2016;8(9):E79.
Yamaguchi TP, Bradley A, McMahon AP, Jones S. A Wnt5a pathway underlies outgrowth of multiple structures in the vertebrate embryo. Development. 1999;126(6):1211–23.
Kim HJ, Schleiffarth JR, Jessurun J, et al. Wnt5 signaling in vertebrate pancreas development. BMC Biol. 2005;3:23.
Nusse R, Clevers H. Wnt/β-catenin signaling, disease, and emerging therapeutic modalities. Cell. 2017;169(6):985–99.
Wang M, Chen DQ, Chen L, Liu D, Zhao H, Zhang ZH, et al. Novel RAS inhibitors Poricoic acid ZG and Poricoic acid ZH attenuate renal fibrosis via a Wnt/β-catenin pathway and targeted phosphorylation of smad3 signaling. J Agric Food Chem. 2018;66(8):1828–42.
Lu YC, Wang CP, Hsu CC, Chiu CA, Yu TH, Hung WC, et al. Circulating secreted frizzled-related protein 5 and wingless-type MMTV integration site family member 5a levels in patients with type 2diabetes mellitus. Diabetes Metab Res Rev. 2013;29(7):551–6.
Xu W, Liang J, Geng HF, et al. Wingless-type MMTV integration site family member 5a is a key secreted islet stellate cell-derived product that regulates islet function. Int J Endocrinol. 2019;2019:7870109.
Brunton S. Pathophysiology of type 2 diabetes: the evolution of our understanding. J Fam Pract. 2016;65(4 Suppl):supp_az_0416.
Hayden MR, Sowers JR. Isletopathy in type 2 diabetes mellitus: implications of islet RAS, islet fibrosis, islet amyloid, remodeling, and oxidative stress. Antioxid Redox Signal. 2007;9:891–910.
Kohlgruber A, Lynch L. Adipose tissue inflammation in the pathogenesis of type 2 diabetes. Curr Diab Rep. 2015;15(11):92.
Tilg H, Moschen AR. Inflammatory mechanisms in the regulation of insulin resistance. Mol Med. 2008;14:222–31.
Johnson AMF, Hou S, Li P. Inflammation and insulin resistance: new targets encourage new thinking: Galectin-3 and LTB4are pro-inflammatory molecules that can be targeted to restore insulin sensitivity. Bioessays. 2017; 39(9).
Vuga LJ, Ben-Yehudah A, Kovkarova-Naumovski E, et al. WNT5A is a regulator of fibroblast proliferation and resistance to apoptosis. Am J Respir Cell Mol Biol. 2009;41:583–9.
Newman DR, Sills WS, Hanrahan K, Ziegler A, Tidd KM, Cook E, et al. Expression of WNT5A in idiopathic pulmonary fibrosis and its control by TGF-β and WNT7B in human lung fibroblasts. J Histochem Cytochem. 2016;64(2):99–111.
Rydell-Törmänen K, Zhou XH, Hallgren O, et al. Aberrant nonfibrotic parenchyma in idiopathic pulmonary fibrosis is correlated with decreased β-catenin inhibition and increased Wnt5a/b interaction. Phys Rep. 2016;4(5):e12727.
Ho C, Hsu YC, Lei CC, et al. Curcumin rescues diabetic renal fibrosis by targeting superoxide-mediated Wnt signaling pathways. Am J Med Sci. 2016;351(3):286–95.
Abraityte A, Vinge LE, Askevold ET, et al. Wnt5a is elevated in heart failure and affects cardiac fibroblast function. J Mol Med (Berl). 2017;95(7):767–77.
Ouchi N, Higuchi A, Ohashi K, Oshima Y, Gokce N, Shibata R, et al. Sfrp5 is an anti-inflammatory adipokine that modulates metabolic dysfunction in obesity. Science. 2010;329:454–7.
Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164–76.
Ilyas Z, Chaiban JT, Krikorian A. Novel insights into the pathophysiology and clinical aspects of diabetic nephropathy. Rev Endocr Metab Disord. 2017 Mar;18(1):21–8.
Shimizu M, Furuichi K, Wada T. Epidemiology and pathogenesis of diabetic nephropathy. Nihon Jinzo Gakkai Shi. 2017;59(2):43–9.
Genovese F, Manresa AA, Leeming DJ, et al. The extracellular matrix in the kidney: a source of novel non-invasive biomarkers of kidney fibrosis? Fibrogenesis Tissue Repair. 2014;7(1):4.
Edeling M, Ragi G, Huang S, et al. Developmental signalling pathways in renal fibrosis: the roles of notch, Wnt and Hedgehog. Nat Rev Nephrol. 2016;12(7):426–39.
Dai C, Stolz DB, Kiss LP, et al. Wnt/beta-catenin signaling promotes podocyte dysfunction and albuminuria. J Am Soc Nephrol. 2009;20:1997–2008.
Wang Y, Zhou CJ, Liu Y. Wnt signaling in kidney development and disease. Prog Mol Biol Transl Sci. 2018;153:181–207.
Surendran K, Schiavi S, Hruska KA. Wnt-dependent beta-catenin signaling is activated after unilateral ureteral obstruction, and recombinant secreted frizzled-related protein 4 alters the progression of renal fibrosis. J Am Soc Nephrol. 2005;16:2373–84.
Beaton H, Andrews D, Parsons M, Murphy M, Gaffney A, Kavanagh D, et al. Wnt6 regulates epithelial cell differentiation and is dysregulated in renal fibrosis. Am J Physiol Ren Physiol. 2016;311(1):F35–45.
Wong DWL, Yiu WH, Chan KW, et al. Activated renal tubular Wnt/β-catenin signaling triggers renal inflammation during overload proteinuria. Kidney Int. 2018;93(6):1367–83.
Feng Y, Liang Y, Ren J, Dai C. Canonical Wnt signaling promotes macrophage proliferation during kidney fibrosis. Kidney Dis (Basel). 2018;4(2):95–103.
Lin X, Zha Y, Zeng XZ, Dong R, et al. Role of the Wnt/β-catenin signaling pathway in inducing apoptosis and renal fibrosis in 5/6-nephrectomized rats. Mol Med Rep. 2017;15(6):3575–82.
Gewin LS. Renal tubule repair: is Wnt/β-Catenin a friend or foe? Genes (Basel). 2018;9(2):E58.
Acknowledgements
We acknowledge and thank all participants for their cooperation and sample contributions.
Funding
This work was supported by generous grants from the Natural Science Foundation of Jiangsu Province (BK20171171) and Xuzhou Science and Technology Bureau project (KC16SH110) to Wei Xu. The author gratefully acknowledges the support of K.C.Wong Education Foundation, Hong Kong. This article was made open access with the financial support of King’s College London.
Author information
Authors and Affiliations
Contributions
All authors took part in the conception and design of the study, as well as either drafting or critically revising the manuscript. All authors have approved the final version of the manuscript. Jun Liang is responsible for the integrity of the work as a whole. Wei Xu, HF Geng and XK Liu contributed equally to this work.
Corresponding authors
Ethics declarations
Duality of interest
All authors declare that there is no duality of interest associated with this manuscript.
Disclosure statement
The authors have nothing to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Xu, W., Geng, H., Liu, X. et al. Wingless-type MMTV integration site family member 5a: a novel biomarker regulated in type 2 diabetes mellitus and diabetic kidney disease. J Diabetes Metab Disord 18, 525–532 (2019). https://doi.org/10.1007/s40200-019-00461-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-019-00461-8