Abstract
Purpose of Review
Adaptive sports (AdS), sports modified or created to accommodate persons with disabilities, have been gaining popularity over the last decade. The benefits of exercise in the able-bodied population are well-established. Literature in adaptive sport and the para-athlete continues to improve but is not yet as comprehensive as their able-bodied peers, in part due to the heterogeneity of participants. In this review, we appraise the recent literature pertaining to AdS and identify developing areas within the field.
Recent Findings
AdS have been shown to have positive health benefits as well as positive psychosocial benefits. Para-athletes often must overcome a variety of barriers to participation, such as transportation, accessibility, and socioeconomic factors. Facilitators to participation have also been identified, including pre-injury interest in sports, male sex, younger age, and more. In addition to well-known sports like handcycling and wheelchair basketball, adaptive sport continues to evolve, in part due to the COVID-19 pandemic, now including virtual options and E-sports. Para-athletes are also being more closely monitored and evaluated pre, peri, and post competition for injury and injury prevention, including in the realm of concussion management, requiring healthcare professionals, coaches, players, and all to gain further knowledge in adaptive sport and the participating para-athletes.
Summary
The physical, psychological, and social benefits of adaptive sports for individuals with disabilities are numerous. Addressing barriers to participation, including novel forms of AdS that utilize innovative technology, may allow more individuals to benefit from AdS.
Similar content being viewed by others
Introduction
There are approximately 17,900 new cases of spinal cord injury (SCI) per year in the USA and 296,000 individuals living in the USA with SCI [1]. SCI can significantly impact a person’s ability to participate in physical activity or sporting events due to mobility limitations, durable medical equipment requirements, accessibility, and socioeconomic status. However, the benefits of exercise, cardiovascular and otherwise, are well-established in both able-bodied individuals and in persons with disabilities. Though SCI is associated with poor health, economic, quality of life (QoL), and social outcomes, these outcomes are dependent on environment and physical activity [2]. Adaptive sports (AdS) offer an opportunity for everyone, including those with SCI, to experience the positive benefit of physical activity.
AdS are sports modified or created to accommodate persons with disabilities. While these sports are often pursued for recreation or competition, they serve additional purposes. AdS can be supportive and provide various physical and psychosocial benefits that continue as a tool long after acute rehabilitation is completed.
Medical providers involved in AdS must recognize that the injuries and illnesses for an adaptive athlete can pose unique and complex challenges. AdS medicine combines the practices of disability medicine with sports medicine, incorporating knowledge of specific sports, patterns of injury, and specialized equipment, all while taking into consideration the athlete’s baseline medical status, including disabling conditions such as SCI [3].
The area of AdS is fast-growing and continues to capture the attention of people living with disabilities, medical providers, and researchers. However, there is still a large gap in research on outreach, overcoming socioeconomic barriers, and sports safety concerns. Existing research on physical activity among this population is typically not as high quality compared to research involving the general population, and they are often excluded from research studies focusing on exercise and physical activity because of their disability [4]. Research into physical activity in persons with disabilities is generally challenging as this is a heterogeneous group and there is no consensus on how to define or measure disability across these populations [4].
The primary aim of this review is to discuss the established benefits and future directions for AdS. We highlight the established research supporting improved physical and psychosocial health in persons with SCI participating in AdS, as well as the common barriers and facilitators to participation. We introduce new areas of study, new sport participation, and the importance of focused safety and care of athletes with disability, including dedicated concussion evaluations.
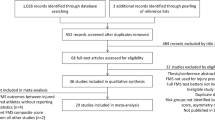
Methods
A literature review of the scientific databases PubMed and Google Scholar was performed using a combination of the following keywords or MeSH terms: “spinal cord injury” AND “sport*” OR “adaptive sport*” OR “wheelchair sport*” OR “sports for persons with disabilities” OR “paralympic” OR “para sport*” OR “para-sport*” OR “employment” OR “return to work” OR “educational status” OR “quality of life” OR “body composition” OR “nutrition.” Only articles published since 2017 pertaining to AdS in individuals with SCI were included.
Results
It has been well-established in the literature that AdS improves QoL in those with disabling conditions. QoL can be broken down into physical, psychosocial, material, and emotional wellbeing along with development and activity [5].
Physical Impacts of Adaptive Sports
Rehabilitation and Improved Function
AdS were initially created as a form of rehabilitation in the late 1700s and refined over many years [3]. Today, AdS can be a practical and cost-effective supplement to traditional rehabilitation in individuals with neurologic disabilities [6]. Recent literature regarding AdS in individuals with SCI continues to emphasize physical benefits of participation. Exercises that incorporate aerobic activities, resistance training or combined exercises, and gait training may provide the most benefit [7].
Studies show participants appreciate benefits such as improved strength and balance, maintenance of a healthy weight, improved daily function such as ease of transfer, and improved strength and stamina [8, 9]. AdS also helped participants ward off both acute and chronic medical issues by preventing weight gain and improving pulmonary function [10].
Body Composition
In a comprehensive review of studies analyzing body composition in SCI, only dual-energy x-ray absorptiometry (DXA) showed acceptable test–retest reliability and convergent validity [11]. By means of DXA, wheelchair adaptive athletes were found to have significantly lower fat mass in the whole-body level and trunk region than wheelchair non-athletes [12]. Another study using DXA to assess body composition in elite wheelchair adaptive athletes showed female athletes had more fat mass and less fat-free mass than males [13]. There were also no significant differences found in fat and fat-free mass between participants with paraplegia, tetraplegia, or without SCI. Two separate studies analyzed the effects of training on adaptive athletes preparing for hand-cycle racing. One study documented a significant increase in peak power output, peak oxygen uptake, and a significant decrease in waist circumference over a 4-month training period [14]. The parallel study reported significantly improved peak power output, fat mass, and percentage body fat over the 4-month training period but did not find a significant decrease in waist circumference or body mass despite similar training hours, suggesting nutrition may have been a factor [15]. Despite the documented physical benefits of AdS, special attention should still be placed on athletes with SCI as they were found to have significantly higher percentage fat mass compared to able-bodied athletes and athletes with amputations, as well as significantly lower whole-body bone mineral density [16]. Furthermore, van der Sheer and colleagues noted relatively weak evidence in their literature review that consistent aerobic and strength exercises can improve bone health in chronic SCI despite moderate or high evidence regarding improvements of body composition, cardiorespiratory fitness, power output, and strength [17].
Cardiovascular/Respiratory
Autonomic dysfunction associated with SCI results in decreased cardiovascular regulation and function [18, 19] as well as impaired thermoregulation and increased risk for autonomic dysreflexia [18]. Endurance sports may induce substantial cardiac remodeling in athletes with SCI [19], but further research should be conducted on this effect depending on the level of neurological lesion [20, 21]. Additionally, respiratory muscle training with inspiratory and expiratory pressure devices may result in improved autonomic modulation of the heart [22], although no direct effects on the heart were found in a similar study [23]. Respiratory muscle training can also significantly improve pulmonary function in persons with SCI [22, 23]. Improved respiratory function can help prevent illnesses, which are more common in athletes with SCI relative to other impairments [24]. While there are many variables that influence the effects of physical training in adaptive athletes, higher training frequency and intensity are more efficient at inducing changes in aerobic fitness and pulmonary function [6, 25].
Manual muscle power is currently one of the main factors in determining classifications for adaptive athletes [26, 27]. Some argue that autonomic cardiovascular function should be included in sports classification as they can place certain athletes with SCI, especially those with a complete injury, at a disadvantage, making cardiovascular and autonomic assessments increasingly important [28, 29]. There is concern that other variables such as autonomic function or pain cannot reliably or consistently be evaluated [27].
Injury
AdS carry risk for various types of injury with unique challenges. Concussion, for example, is a clinical diagnosis which may be difficult to identify given a “normal” baseline function cannot be applied across adaptive athletes [30]. It is therefore recommended clinicians familiarize themselves with each athlete’s baseline cognitive and neuromuscular function via frequent examinations and use a revised sport concussion assessment tool 5 (SCAT5) that takes special considerations for various disabilities [30]. Until further research is done, clinicians should err on the side of caution with adaptive athletes and tailor concussion guidelines to each patient [30].
While minor soft tissue injuries are relatively common in both traditional and AdS, there is higher prevalence of upper extremity injury in adaptive athletes compared to able-bodied athletes [31, 32]. Increased age and manual wheelchair use pose higher risks of developing common extensor tendinopathy, lateral epicondylitis, and rotator cuff tears [31, 33]. Females were also found to have a higher risk than males in developing rotator cuff tears, especially when participating in a wheelchair sport [33]. A retrospective survey of 43 non-elite adaptive athletes demonstrated that 39.5% sustained an injury that required them to miss a competition or practice in 12 months, and most of those injured had no injury prevention education [34]. Additionally, approximately 42%, mostly those with SCI, experienced spasticity [34]. Over half of those injured sought medical care from multiple medical providers, and 25% of those who did not seek medical care did not because they were unsure of who to see [34].
Recently, an addendum to the International Olympic Committee’s universal methodology for recording and reporting injury was made to include special measures for individuals with impairment [35]. The addendum provides more specific definitions and recommendations for respective impairments, such as how to define and classify health problems, injury mechanism, onset, duration, and more.
Nutrition
Athletes with SCI face unique nutritional requirements compared to able-bodied athletes due to a variety of factors, such as physiological adaptations or limitations after injury, reduced exercise capacity, insufficient guidance, or secondary health complications [36, 37]. It is estimated that actual energy intake and expenditure is lower in adaptive athletes relative to able-bodied counterparts [38]. Adaptive athletes may also be at higher risk for low energy availability, which may cause a myriad of health issues [37, 38]. Sleep disturbances may also affect nutrition status and athletic performance [37] and attending training camps can cause significant reduction in total sleep time and worsen sleep quality [39]. Despite a growing body of literature, guidelines for nutrition in AdS remain unclear given the heterogeneity of the population, type of sport, and injury levels [36]. While carbohydrates, protein, vitamin D, and iron are vital nutrients that can affect performance across all types of sports and injuries, individualized nutritional plans are most effective at empowering athletes [37]. For example, many para-athletes with SCI were found to be deficient in vitamin D independent of diet and lifestyle. A sliding-scale supplementation of vitamin D in these para-athletes can maintain sufficient vitamin D levels, improve vitamin D deficiencies, and may result in increased muscle strength [40]. Overall, the nutritional guidelines for able-bodied athletes may not be well-suited for adaptive athletes and additional research needs to be done.
Psychosocial Impacts of Adaptive Sports
In addition to the physical benefits for adaptive athletes, there is a growing body of literature focusing on the psychosocial benefits of AdS in individuals with SCI and other disabilities. Despite the heterogeneity of study design, backgrounds of participants, and type of sport, similar themes have emerged regarding how psychosocial benefits are mediated through intrapersonal and interpersonal effects.
Intrapersonal
AdS has been shown to increase life satisfaction and QoL in individuals with SCI [41, 42]. Persons with disabilities commonly participate in AdS for personal enrichment. Adaptive athletes may use sports to hold onto their pre-injury identity or they may view physical activities as transformative to their character, allowing them to move past their disability identity [8, 9, 43,44,45]. Disability acceptance can help mediate a sense of self-efficacy and positive life satisfaction in individuals with SCI and AdS may help mediate this transition [46]. Recent literature suggests that AdS provide persons with disabilities a sense of belonging and purpose [10, 43], self-efficacy or confidence [8, 9, 44, 47,48,49], freedom and autonomy [9, 50], continuity and structure [45, 50], and hope and motivation [9, 10, 45]. Furthermore, besides recreational purposes alone, some individuals report that sports help regulate their mood and reduce stress [8, 9, 50].
Interpersonal
AdS have also been shown to help individuals with SCI build or solidify interpersonal relationships and reintegrate into the community. In a Turkish study involving persons with disabilities, it was reported that wheelchair users were less likely to participate in community activities, but those who played AdS professionally had higher rates of community reintegration [51]. Participants with SCI have reported that AdS provided opportunities to build new relationships with their peers and community as well as strengthen current connections with family and friends [9, 45]. Some individuals pursue AdS to fulfill a need for social acceptance [43, 47], while others report that participation offers a means to socialize [44, 47, 48, 50]. Furthermore, AdS programs foster environments where individuals can comfortably discuss issues they face with their disability [10] and serve as a source of information, opportunities, and resources [44, 48, 50]. These findings are worth considering when individuals with SCI are reintegrating into their communities.
Veterans and Adaptive Sports
U.S. military veterans represent a large proportion of the individuals participating in AdS with 76% of community organizations affiliated with Veterans Affairs Medical Centers [52]. With Veterans Affairs (VA) being one of the largest healthcare systems in the world, it has been in the forefront of advocating for AdS for veterans with disability. A highly respected and active program is the National Veterans Sports Program & Special Events (NVSPSE), which has engaged in AdS since 1981 with the National Veterans Wheelchair Games [3]. Currently, NVSPSE runs six programs that have been serving veterans with various sports and recreation activities [53]. In addition, Congress has approved continued support of community organizations through NVSPSE with adaptive sports grants [54]. This grant program started in 2013 with $8,000,000 and has grown to $14,500,000 allocated for 2022. This exemplifies the importance and continuing effort by the VA to continue to break down barriers and facilitate the wellbeing of veterans with disability in achieving healthy and meaningful lives.
Barriers and Facilitators to Participation
While individuals with SCI are often included in the target populations for studies evaluating access to sporting activities, few have focused solely on SCI or other disabilities. Nonetheless, when taken together, these studies help uncover common barriers and facilitators to participation in AdS.
Barriers
One of the largest factors influencing participation in AdS throughout multiple recent studies was financial costs [44, 55,56,57,58,59]. Although expenses were reported as barriers for both adults and parents of children with disabilities, cost was a more significant challenge for adults [57]. A study in Brazil found that approximately 57% of the adaptive athletes sampled purchased assistive devices out of their own money, despite most of the participants belonging to low-income backgrounds and utilizing public resources designed to subsidize costs [60]. Although there are differing and complex influencing factors across countries, it is evident that financial limitations pose significant barriers to entry in AdS.
Time constraints and transportation concerns were also reported as significant barriers [44, 55, 57, 58]. Other barriers cited included lack of fellow athletes, coaches, or local facilities to train [58, 59, 61] as well as lack of awareness of sport opportunities among adaptive athletes [44, 47]. In line with the lack of coaches, there is also a lack of experienced healthcare professionals to guide adaptive athletes in their sport [3]. Persons with disabilities are a heterogeneous group; therefore, a healthcare provider must be knowledgeable of various disabilities, secondary health issues, and personal factors to tailor an appropriate training protocol [3]. Additional barriers reported by adult participants in AdS studies included limitations related to their condition, injury, or fear of injury [44, 47, 58] as well as environmental barriers such as lack of practical parking, ramps, or elevators [55,56,57,58, 61]. It should be noted, however, that consistent exercise is feasible even among individuals with SCI who had significantly lower mobility scores on the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 relative to other attendees when adequate facilities are available [62].
Facilitators
In a study focused on youth (age 14–20 years old) with SCI, it was found that male gender, younger age, better health, and higher levels of trust were significant factors that facilitated AdS participation [63]. Other unique facilitators for AdS participation included early or pre-injury interest in sports [44, 47, 64]. People also endorsed accommodating environmental factors such as parking or having other individuals with disability in attendance [57]. In Malaysia, a case–control study involving interviews of 65 individuals with SCI found that being able to drive a vehicle and being employed were significantly associated with participation in AdS [64]. Similar findings showing positive associations between employment among individuals with disability and community participation were reported in Turkey [51]. Social support from coaches, peers, or family were found to be important factors influencing or motivating participation [44, 47, 55,56,57]. Additional motivators included health improvement, fun and relaxation, and improving physical strength [57, 58].
Additional research into the barriers and facilitators of AdS participation is warranted given the complex factors influencing participation and the significant effects it may have on QoL in individuals with SCI.
Adaptive Sport and Future Considerations
Despite growing popularity and focus on AdS and exercise in persons with disabilities, there are still gaps in this field. A comprehensive literature review by Martin Ginis and her colleagues brings the current state of global research regarding people living with disabilities and their exercise rates into focus [4]. Taking these findings in context with other recent studies, directions for future research become clearer.
In their review, Martin Ginis et al. note that an estimated 20–60% of adults with disabilities do not reach the World Health Organization’s recommended physical activity levels [4]. This is consistent with a study analyzing physical activity levels with a wrist accelerometer in 96 manual wheelchair users with SCI in Spain, where approximately 43% of participants reached weekly recommended threshold of moderate-vigorous exercise, and approximately 37% who self-identified as regular exercisers did not reach recommended threshold of moderate-vigorous exercise [65]. These deficits in physical activity among individuals with disabilities were compounded by the COVID-19 pandemic. One study showed significant decreases in self-reported physical activity among individuals with SCI during lockdown in Spain [66]. However, there have been strategies implemented to promote participation in AdS and improve QoL even with social distancing.
Amid the COVID-19 pandemic, a virtual AdS exercise class was established and enrolled 47 participants with disabilities [67]. The virtual sports program had advantages and pitfalls. The nature of virtual exercise classes reduced barriers to participation, was able to reach a wider population, and was more cost-effective in staffing and in startup since it was designed to use equipment at participants’ homes [67]. The virtual platform also posed challenges. Registration and waiver completion were more difficult, the exact locations of each participant had to be tracked in case of medical emergencies, patient confidentiality was harder to protect in the virtual format, participants had less peer mentoring, and the class was less amenable to certain sports [67].
Competitive and organized video gaming, also known as E-sports, is an alternate and interesting form of AdS. While E-sports do not involve significant physical activity, there is potential to improve mental and social wellbeing. Tobacof et al. worked to design custom, adaptive video game setups to facilitate participation in E-sports among seven individuals with SCI [68]. Although social connectedness was negatively correlated with time since injury among participants, all seven members reported positive impacts on their feelings of social connectedness after participation in the program [68].
Some additional breakthroughs in recent years include new guidelines for physical activity tailored specifically towards individuals with SCI. In a separate literature review, Martin Ginis et al. propose new physical activity guidelines for people with SCI that require lower levels compared to the general population but are more achievable [69]. Specifically, they strongly recommend for adults with SCI to engage in 20 min of moderate to vigorous aerobic exercise in addition to three sets of strength training for functioning major muscle groups, at moderate to vigorous intensity for both, twice weekly for optimal cardiorespiratory and muscle strength benefits [69]. They also provide a conditional recommendation of at least 30 min of moderate to vigorous aerobic exercise three times weekly for cardiometabolic health [69]. It is recommended that healthcare professionals provide individuals with SCI information on exercise, and that the guidance should include theory-based interventions, such as behavioral change techniques, delivered via direct counseling or individualized action plans [70].
What meaningful and effective participation entails is an important perspective to consider when encouraging individuals with SCI to take on sports or exercise. A holistic definition regarding meaningful participation for persons with disabilities was proposed and goes beyond objective measures of performance to account for the subjective experience [71]. This new definition argues that autonomy, belongingness, challenge, engagement, mastery, and meaning are all vital to an impactful experience [71]. A separate study identified characteristics of quality physical activity including group cohesion and sense of community, challenge and growth, having a role, independence, and choice, based on responses from veterans with disabilities and their providers [61, 72].
There are arguments that the technology itself in AdS can be improved. Even if one overcomes the barriers to participation, there are little to no effective tools to track performance, calories burned, or longitudinal training in adaptive athletes [59]. This also poses challenges in customizing and optimizing assistive equipment, which can help reduce injury [59]. For these reasons, more robust and accurate analytical technology along with more recruitment of fellow athletes and knowledgeable trainers can help advance the field of AdS [59].
Discussion
This literature review was conducted to highlight AdS and their roles in the lives of individuals with SCI. While the primary focus was on new and interesting discoveries over the last 5 years, we discuss how these recent findings have built upon previous knowledge and may guide future studies.
Research continues to show that AdS can have numerous beneficial effects on the physical, mental, and social wellbeing of individuals with SCI and other physical disabilities. However, it should not be thought that AdS are a faultless solution to the health of SCI individuals. There remain challenging barriers in access to AdS, ranging from high financial burdens, difficulties with transportation and environmental barriers, lack of local facilities and knowledgeable trainers or volunteers, or personal limitations due to disability. Nonetheless, awareness of these issues can and should influence interventions targeting persons with disabilities. For example, we have seen AdS translate into a virtual setting to circumvent some of these challenges. While these methods have their own issues, they show potential in improving QoL. Further research into E-sports and remote training programs should be pursued.
Some relationships between AdS and SCI should be further studied. In our literature review, we found limited articles involving children with SCI in their population [48, 57, 63]. The existing literature that does include youth involves a limited range of sports and lacks evaluation of participation outcomes [73]. We also found limited studies from 2017 or later directly looking at the relationship between AdS and return to work. We found just one study in which half of veterans participating at the National Veterans Wheelchair Games believed that AdS had a positive effect on obtaining employment [74]. It was also noted that adaptive athletes who were currently working were significantly more likely to report that participation helped them achieve employment [74]. Given that economic sufficiency was found to have a significant positive association with life satisfaction in individuals with SCI, the mediating effect of AdS should be further investigated [75]. Lastly, research into the benefits of AdS in people with SCI is generally predominated by male participants and future work should strive to be more inclusive of females to address this gap.
AdS have been increasing in popularity and awareness. Beside the barriers and challenges outlined in this article, an important factor as we move into the future is the safety of athletes participating in these sports. Individuals with SCI, by the nature of their wheelchair use for daily locomotion, are at higher risk for upper extremity injuries compared to their able-bodied counterparts. Their co-morbidities can complicate their health during pre, peri, and post events. Such conditions include pressure ulcer injuries, thermoregulation issues, and sports-related concussion (SRC). There is a large gap in research and implementation of programs to prevent and evaluate SRC in AdS. Recently, there have been attempts to increase awareness and care for SRC in adaptive athletes. An international group of experts, Concussion In Parasport (CIPS), published the first position statement to start addressing the SRC in adaptive sport [30]. Shortly after that, the first book on concussion management of wheelchair athletes was published outlining a Concussion Management Program addressing evaluation and examination of SRC in wheelchair athletes [76]. Authors recognize the significant gap in addressing the safety of such athletes and need for future research.
Conclusion
SCI is a life-changing diagnosis. Persons with SCI experience physical, mental, and social consequences from their injuries. AdS are effective methods of increasing health and overall QoL for people with SCI and other disabilities. This review article highlights significant findings pertaining to AdS and SCI from 2017 onwards. It is important that medical providers and AdS programs be cognizant of common barriers to entry and strive to promote meaningful participation. As AdS continue to be recognized and become part of the mainstream sports world, it is also important to evaluate and improve on the safety of these adaptive athletes. As accessibility barriers are broken down via virtual platforms, additional research should also be focused on improving the technology that promotes effective training and participation in adaptive athletes.
References
National Spinal Cord Injury Statistical Center 2020 Annual Statistical Report for the Spinal Cord Injury Model Systems. University of Alabama at Birmingham: Birmingham, Alabama. https://www.nscisc.uab.edu. Accessed Feb. 9., 2022.
Lukersmith S. International perspectives on spinal cord injury. 2013.
Lee KK, Uihlein MJ. Adaptive sports in the rehabilitation of the disabled veterans. Phys Med Rehabil Clin N Am. 2019;30(1):289–99. https://doi.org/10.1016/j.pmr.2018.08.001.
Martin Ginis KA, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet. 2021;398(10298):443–55. https://doi.org/10.1016/S0140-6736(21)01164-8.
Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil. 1995;16(1):51–74. https://doi.org/10.1016/0891-4222(94)00028-8.
Declerck L, Kaux JF, Vanderthommen M, Lejeune T, Stoquart G. The effect of adaptive sports on individuals with acquired neurological disabilities and its role in rehabilitation: a systematic review. Curr Sports Med Rep. 2019;18(12):458–73. https://doi.org/10.1249/JSR.0000000000000662.
Gaspar R, Padula N, Freitas TB, de Oliveira JPJ, Torriani-Pasin C. Physical exercise for individuals with spinal cord injury: systematic review based on the international classification of functioning, disability, and health. J Sport Rehabil. 2019;28(5):505–16. https://doi.org/10.1123/jsr.2017-0185.
Lape EC, Katz JN, Losina E, Kerman HM, Gedman MA, Blauwet CA. Participant-reported benefits of involvement in an adaptive sports program: a qualitative study. PM R. 2018;10(5):507–15. https://doi.org/10.1016/j.pmrj.2017.10.008.
Schmid SM, Short CT, Nigg CR. Physical activity & people with disabilities—a qualitative process and outcome pilot evaluation of the non-profit organization AccesSurf Hawai’i. Hawaii J Med Public Health. 2019;78(2):52–60.
Ekelman BA, Allison DL, Duvnjak D, DiMarino DR, Jodzio J, Iannarelli PV. A wellness program for men with spinal cord injury: participation and meaning. OTJR (Thorofare N J). 2017;37(1):30–9. https://doi.org/10.1177/1539449216672170.
van der Scheer JW, et al. Assessment of body composition in spinal cord injury: a scoping review. PLoS ONE. 2021;16(5):e0251142. https://doi.org/10.1371/journal.pone.0251142.
Cavedon V, Zancanaro C, Milanese C. Body composition assessment in athletes with physical impairment who have been practicing a wheelchair sport regularly and for a prolonged period. Disabil Health J. 2020;13(4):100933. https://doi.org/10.1016/j.dhjo.2020.100933.
Flueck JL. Body composition in Swiss elite wheelchair athletes. Front Nutr. 2020;7:1. https://doi.org/10.3389/fnut.2020.00001.
Hoekstra S, Valent L, Gobets D, van der Woude L, de Groot S. Effects of four-month handbike training under free-living conditions on physical fitness and health in wheelchair users. Disabil Rehabil. 2017;39(16):1581–8. https://doi.org/10.1080/09638288.2016.1200677.
de Groot S, Kouwijzer I, Baauw M, HandbikeBattle RB, Valent LJ. Effect of self-guided training for the HandbikeBattle on body composition in people with spinal cord injury. Spinal Cord Ser Cases. 2018;4:79. https://doi.org/10.1038/s41394-018-0103-6.
Cavedon V, Sandri M, Peluso I, Zancanaro C, Milanese C. Body composition and bone mineral density in athletes with a physical impairment. PeerJ. 2021;9:e11296. https://doi.org/10.7717/peerj.11296.
van der Scheer JW, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89(7):736–45. https://doi.org/10.1212/WNL.0000000000004224.
Cruz S, Blauwet CA. Implications of altered autonomic control on sports performance in athletes with spinal cord injury. Auton Neurosci. 2018;209:100–4. https://doi.org/10.1016/j.autneu.2017.03.006.
Pelliccia A, et al. Physiologic and clinical features of the paralympic athlete’s heart”. JAMA Cardiol. 2021;6(1):30–9. https://doi.org/10.1001/jamacardio.2020.4306.
Alrashidi AA, Nightingale TE, Krassioukov AV. Time to reconsider the importance of autonomic function in paralympic athletes with spinal cord injury. JAMA Cardiol. 2021;6(8):976–7. https://doi.org/10.1001/jamacardio.2021.1130.
Bernardi M, Cavarretta E, Pelliccia A. Time to reconsider the importance of autonomic function in paralympic athletes with spinal cord injury-reply. JAMA Cardiol. 2021;6(8):977. https://doi.org/10.1001/jamacardio.2021.1153.
Legg Ditterline BE, Aslan SC, Randall DC, Harkema SJ, Castillo C, Ovechkin AV. Effects of respiratory training on heart rate variability and baroreflex sensitivity in individuals with chronic spinal cord injury. Arch Phys Med Rehabil. 2018;99(3):423–32. https://doi.org/10.1016/j.apmr.2017.06.033.
Gee CM, Williams AM, Sheel AW, Eves ND, West CR. Respiratory muscle training in athletes with cervical spinal cord injury: effects on cardiopulmonary function and exercise capacity. J Physiol. 2019;597(14):3673–85. https://doi.org/10.1113/JP277943.
Derman W, et al. Sport, sex and age increase risk of illness at the Rio 2016 Summer Paralympic Games: a prospective cohort study of 51 198 athlete days. Br J Sports Med. 2018;52(1):17–23. https://doi.org/10.1136/bjsports-2017-097962.
Skucas K, Pokvytyte V. Short-term moderate intensive high volume training program provides aerobic endurance benefit in wheelchair basketball players. J Sports Med Phys Fitness. 2017;57(4):338–44. https://doi.org/10.23736/S0022-4707.16.06141-7.
Beckman EM, Connick MJ, Tweedy SM. Assessing muscle strength for the purpose of classification in Paralympic sport: a review and recommendations. J Sci Med Sport. 2017;20(4):391–6. https://doi.org/10.1016/j.jsams.2016.08.010.
Ungerer G. Classification in para sport for athletes following cervical spine trauma. Handb Clin Neurol. 2018;158:371–7. https://doi.org/10.1016/B978-0-444-63954-7.00035-5.
Gee CM, Currie KD, Phillips AA, Squair JW, Krassioukov AV. Spinal cord injury impairs cardiovascular capacity in elite wheelchair rugby athletes. Clin J Sport Med. 2020;30(1):33–9. https://doi.org/10.1097/JSM.0000000000000561.
West CR, Krassioukov AV. Autonomic cardiovascular control and sports classification in paralympic athletes with spinal cord injury. Disabil Rehabil. 2017;39(2):127–34. https://doi.org/10.3109/09638288.2015.1118161.
Weiler R, et al. Concussion in para sport: the first position statement of the Concussion in Para Sport (CIPS) Group (in eng). Br J Sports Med. 2021;55(21):1187–95. https://doi.org/10.1136/bjsports-2020-103696.
Cyr AK, Colorado BS, Uihlein MJ, Garlanger KL, Tarima SS, Lee K. Prevalence of lateral epicondylosis in veteran manual wheelchair users participating in adaptive sports. J Spinal Cord Med. 2020:1–7. https://doi.org/10.1080/10790268.2020.1771243.
Tuakli-Wosornu YA, Mashkovskiy E, Ottesen T, Gentry M, Jensen D, Webborn N. Acute and chronic musculoskeletal injury in para sport: a critical review. Phys Med Rehabil Clin N Am. 2018;29(2):205–43. https://doi.org/10.1016/j.pmr.2018.01.014.
Pepke W, et al. [Risk factors for the development of rotator cuff tears in individuals with paraplegia: a cross-sectional study]. Risikofaktoren fur Rotatorenmanschettenrupturen bei Paraplegikern : Eine Querschnittstudie. Orthopade. 2018;47(7):561–6. https://doi.org/10.1007/s00132-018-3546-3.
Soo Hoo JA, Latzka E, Harrast MA. A descriptive study of self-reported injury in non-elite adaptive athletes. PM R. 2018. https://doi.org/10.1016/j.pmrj.2018.08.386.
Derman W, et al. Para sport translation of the IOC consensus on recording and reporting of data for injury and illness in sport. Br J Sports Med. 2021;55(19):1068–76. https://doi.org/10.1136/bjsports-2020-103464.
Ruettimann B, Perret C, Parnell JA, Flueck JL. Carbohydrate considerations for athletes with a spinal cord injury. Nutrients. 2021;13(7). https://doi.org/10.3390/nu13072177.
Scaramella J, Kirihennedige N, Broad E. Key nutritional strategies to optimize performance in para athletes. Phys Med Rehabil Clin N Am. 2018;29(2):283–98. https://doi.org/10.1016/j.pmr.2018.01.005.
Figel K, Pritchett K, Pritchett R, Broad E. Energy and nutrient issues in athletes with spinal cord injury: are they at risk for low energy availability? Nutrients. 2018;10(8). https://doi.org/10.3390/nu10081078.
Murphy CJ, Hartescu I, Roberts IE, Leicht CA, Goosey-Tolfrey VL. Sleep characteristics of highly trained wheelchair rugby athletes with and without a cervical spinal cord injury during the competitive season. Front Sports Act Living. 2021;3:643233. https://doi.org/10.3389/fspor.2021.643233.
Pritchett K, Pritchett RC, Stark L, Broad E, LaCroix M. Effect of vitamin D supplementation on 25(OH)D status in elite athletes with spinal cord injury. Int J Sport Nutr Exerc Metab. 2019;29(1):18–23. https://doi.org/10.1123/ijsnem.2017-0233.
Kouwijzer I, et al. Changes in quality of life during training for the HandbikeBattle and associations with cardiorespiratory fitness. Arch Phys Med Rehabil. 2020;101(6):1017–24. https://doi.org/10.1016/j.apmr.2019.12.015.
Filipcic T, Sember V, Pajek M, Jerman J. Quality of life and physical activity of persons with spinal cord injury. Int J Environ Res Public Health. 2021;18(17). https://doi.org/10.3390/ijerph18179148.
Allan V, Smith B, Côté J, Martin Ginis KA, Latimer-Cheung AE. Narratives of participation among individuals with physical disabilities: a life-course analysis of athletes’ experiences and development in parasport. Psychol Sport Exerc. 2018;37:170–8. https://doi.org/10.1016/j.psychsport.2017.10.004.
McLoughlin G, Weisman Fecske C, Castaneda Y, Gwin C, Graber K. Sport participation for elite athletes with physical disabilities: motivations, barriers, and facilitators. Adapt Phys Activ Q. 2017;34(4):421–41. https://doi.org/10.1123/apaq.2016-0127.
Chun S, Lee Y. Racing made me feel strong and more positive: Experiencing personal meaning in life through leisure following traumatic spinal cord injury. Leisure Sciences. 2020;1–18. https://doi.org/10.1080/01490400.2020.1713937
Ahn H, Lee K, So Y. The mediating effect of disability acceptance in individuals with spinal cord injury participating in sport for all. Int J Environ Res Public Health. 2021;18(20). https://doi.org/10.3390/ijerph182010883.
Ballas J, Buultjens M, Murphy G, Jackson M. Elite-level athletes with physical impairments: barriers and facilitators to sport participation. Disabil Soc. 2020:1–20. https://doi.org/10.1080/09687599.2020.1862642.
Jeffress M, Brown W. Opportunities and benefits for powerchair users through power soccer. Adapt Phys Activ Q. 2017;34:235–55. https://doi.org/10.1123/apaq.2016-0022.
Goraczko A, Zurek A, Lachowicz M, Kujawa K, Zurek G. Is self-efficacy related to the quality of life in elite athletes after spinal cord injury? Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph182010866.
Labbe D, Miller WC, Ng R. Participating more, participating better: health benefits of adaptive leisure for people with disabilities. Disabil Health J. 2019;12(2):287–95. https://doi.org/10.1016/j.dhjo.2018.11.007.
Akyurek G, Bumin G, Crowe TK. The factors associated with community participation: employment and education of people with disabilities in Turkey. Scand J Occup Ther. 2020;27(1):28–38. https://doi.org/10.1080/11038128.2019.1587502.
Whiting ZG, Falk D, Lee J, Weinman B, Pines JM, Lee K. Community organization factors affecting veteran participation in adaptive sports (in eng). J Spinal Cord Med. 2020:1–7. https://doi.org/10.1080/10790268.2020.1803657.
VA adaptive sports and therapeutic arts. https://www.blogs.va.gov/nvspse/. Accessed Feb. 8, 2022.
Adaptive Sports Grant Program. https://www.blogs.va.gov/nvspse/grant-program/. Accessed Feb. 8, 2022.
Amberkar O, Agarwal BM, Singh Y, Shete R, Mullerpatan RP. Level of sports participation and performance among people with spinal cord injury. 2019;31(1):43–51. https://doi.org/10.1615/CritRevPhysRehabilMed.2019029750
Becerra MAG, Manzini MG, Martinez CMS. Perception of rugby athletes on wheelchairs on supports received for an adapted sport practice. Cadernos Brasileiros de Terapia Ocupacional. 2019;27:615–27.
Iverson M, et al. Navigator role for promoting adaptive sports and recreation participation in individuals with disabilities. Am J Phys Med Rehabil. 2021;100(6):592–8. https://doi.org/10.1097/PHM.0000000000001533.
de Groot S, et al. Sport participation after the HandbikeBattle: benefits, barriers, facilitators from the event—a follow-up survey. Spinal Cord Ser Cases. 2020;6(1):54. https://doi.org/10.1038/s41394-020-0301-x.
Khurana R, Wang A, Carrington P. Beyond adaptive sports: challenges & opportunities to improve accessibility and analytics. Presented at the The 23rd International ACM SIGACCESS Conference on Computersand Accessibility (ASSETS ’21), Virtual Event, USA, October 18–22, 2021, 2021.
Marques MP, Alves ACJ. Investigating environmental factors and paralympic sports: an analytical study. Disabil Rehabil Assist Technol. 2021;16(4):414–9. https://doi.org/10.1080/17483107.2020.1780483.
Shirazipour CH, et al. Quality participation experiences in the physical activity domain: perspectives of veterans with a physical disability. Psychol Sport Exerc. 2017;29:40–50. https://doi.org/10.1016/j.psychsport.2016.11.007.
Nalla S, Huang K, Spangenberg J, Chen L, Jayabalan P. The demographic and disability characteristics of individuals who regularly attend an urban adaptive fitness center: an observational study. PM R. 2021. https://doi.org/10.1002/pmrj.12720.
Moll AM, Bester G. Factors that relate to sport participation of adolescents with a mobility impairment. Afr J Disabil. 2019;8:614. https://doi.org/10.4102/ajod.v8i0.614.
Zainudin MF, Ahmad Fauzi A. Factors associated with sports participation amongst people with spinal cord injury in a Malaysian tertiary hospital. J Spinal Cord Med. 2021:1–8. https://doi.org/10.1080/10790268.2021.1950454.
Ferri-Caruana A, Millan-Gonzalez L, Garcia-Masso X, Perez-Nombela S, Pellicer-Chenoll M, Serra-Ano P. Accelerometer assessment of physical activity in individuals with paraplegia who do and do not participate in physical exercise. J Spinal Cord Med. 2020;43(2):234–40. https://doi.org/10.1080/10790268.2018.1550597.
Marco-Ahullo A, Montesinos-Magraner L, Gonzalez LM, Morales J, Bernabeu-Garcia JA, Garcia-Masso X. Impact of COVID-19 on the self-reported physical activity of people with complete thoracic spinal cord injury full-time manual wheelchair users. J Spinal Cord Med. 2021:1–5. https://doi.org/10.1080/10790268.2020.1857490.
Blauwet CA, Robinson D, Riley A, MacEwan K, Patstone M, Dubon ME. Developing a virtual adaptive sports program in response to the COVID-19 pandemic. PM R. 2021;13(2):211–6. https://doi.org/10.1002/pmrj.12481.
Tabacof L, Dewil S, Herrera JE, Cortes M, Putrino D. Adaptive esports for people with spinal cord injury: new frontiers for inclusion in mainstream sports performance. Front Psychol. 2021;12:612350. https://doi.org/10.3389/fpsyg.2021.612350.
Martin Ginis KA, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56(4):308–21. https://doi.org/10.1038/s41393-017-0017-3.
Todd KR, Martin Ginis KA. Physical activity and spinal cord injury: lessons learned at the lowest end of the physical activity spectrum. Hum Kinet. 2019;8(1):54–62.
Martin Ginis KA, Evans MB, Mortenson WB, Noreau L. Broadening the conceptualization of participation of persons with physical disabilities: a configurative review and recommendations. Arch Phys Med Rehabil. 2017;98(2):395–402. https://doi.org/10.1016/j.apmr.2016.04.017.
Fakolade AO, Latimer-Cheung AE, Shirazipour CH. Quality participation: perspectives of physical activity service providers for veterans with disabilities. Disabil Health J. 2021;14(3):101094. https://doi.org/10.1016/j.dhjo.2021.101094.
Bragg E, Pritchard-Wiart L. Wheelchair physical activities and sports for children and adolescents: a scoping review. Phys Occup Ther Pediatr. 2019;39(6):567–79. https://doi.org/10.1080/01942638.2019.1609151.
Kim W, Lee L, Lans D, Tostenrude D, Lee K. Perception of employment by the veterans participating in the national veterans wheelchair games: a survey study. PM R. 2018;10(3):263–8. https://doi.org/10.1016/j.pmrj.2017.09.002.
Karatas G, Metli N, Yalcin E, Gunduz R, Karatas F, Akyuz M. The effects of the level of spinal cord injury on life satisfaction and disability. Ideggyogy Sz. 2020;73(1–2):27–34. https://doi.org/10.18071/isz.73.0027. A gerincvelo-serules helye es a rokkantsag, valamint az eletminoseg kapcsolata.
Lee K, Harper M, Uihlein M, McCrea M. Concussion management for wheelchair athletes: Evaluation and examination. 1 ed. Springer Cham; 2021. p. 227.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spinal Cord Injury Rehabilitation
Rights and permissions
About this article
Cite this article
Rayes, R., Ball, C., Lee, K. et al. Adaptive Sports in Spinal Cord Injury: a Systematic Review. Curr Phys Med Rehabil Rep 10, 145–153 (2022). https://doi.org/10.1007/s40141-022-00358-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-022-00358-3