Abstract
Purpose of Review
Coagulopathy is a complex pathological condition manifested through the insufficient or excessive tendency to form blood thrombi, which can be caused by trauma and surgery. A promising strategy to mitigate coagulopathy is the balanced restoration of the generation of thrombin — the main enzyme in the blood-coagulation system. We review studies focusing on thrombin, traumatic coagulopathy, and hemostatic balance — a concept aimed to avoid abnormally weak or excessively strong coagulation responses.
Recent Findings
Thrombin generation is impacted by coagulopathic conditions described by complex patterns, possibly depending on various factors. New methodologies of thrombin-generation measurement and analysis are emerging. Combinations of pro- and anticoagulant proteins can restore thrombin generation in coagulopathy. Balanced therapeutic strategies to improve thrombin generation may lead to favorable clinical outcomes.
Summary
Thrombin generation is an essential target of pharmacological intervention in traumatic and surgical coagulopathy.
Graphic Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma, with the resulting hemorrhage and shock, can impact the patient’s physiology on many levels. One of the most dangerous consequences of trauma is the blood-coagulation system malfunction — a complex pathological condition termed trauma-induced coagulopathy (TIC) [1••, 2–4]. Affecting ~ 25% of all trauma patients, TIC is prevalent worldwide in both civilian and military settings [1••]. Some of the factors causing TIC are intrinsically pathophysiologic, while others are iatrogenic — e.g., dilutional coagulopathy caused by the infusion of crystalloid solutions [2]. TIC may lead to severe bleeding (that often cannot be surgically controlled), or it may cause thromboembolic complications; sometimes, both types of effects are present during different temporal phases of TIC [1••]. This creates an extra layer of complexity in trauma surgery and critical care, necessitating both basic and clinical research to understand the mechanistic aspects of TIC and investigate promising pharmacological intervention strategies.
Blood coagulation in mammals is controlled by a very complex system comprising interactions between dozens of biochemical species, platelets, red blood cells (RBCs), endothelial cells, and other components, all occurring in the context of blood flow, as well as blood-vessel and wound geometry [5–7]. These different components can exist in non-activated or activated states, and the conversions between activation levels add to the combinatorial complexity of the interaction network. A central event in the blood-coagulation process is the formation of a hemostatic thrombus (“clot”) at the site of vascular injury (Fig. 1A). The main components of a thrombus are platelets and the polymeric protein fibrin [5, 6, 8]. Fibrin gives the clot the necessary mechanical stability and hydraulic resistance to perform its hemostatic function [9]. As the clot grows, fibrin is generated from its monomeric precursor, fibrinogen, and this conversion (as well as subsequent fibrin polymerization) is catalyzed by the protein thrombin [10–12]. Thrombin itself is generated from its inactive precursor — prothrombin — in response to injury, and performs multiple functions in the coagulation system (including, e.g., platelet activation and factor XIII activation for fibrin crosslinking) [5, 12]. Thrombin is often regarded as the central enzymatic component in the blood-coagulation system [5, 12], and thrombin generation (TG) impairment can play a significant role in traumatic and surgical coagulopathy [13•, 14, 15].
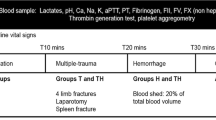
Thrombin generation: essential concepts. A Main thrombin generation (TG) steps. As a result of bleeding, plasma is exposed to tissue factor, which triggers the enzymatic blood-coagulation network. The reactions in the network lead to the cleavage of prothrombin and generation of small amounts of thrombin, which activates platelets and thereby initiates a TG burst on the platelet surfaces. Ultimately, the generated thrombin converts fibrinogen to fibrin, which becomes part of the body of the growing thrombus. B Schematic representation of TG in vitro. Phases 1, 2, and 3 (marked by colored rectangles) are the TG stages: initiation, propagation, and termination, respectively. The typical one-peaked shape of the TG curve is characterized by five quantitative parameters: lag time (LT, time to the onset of TG), time to thrombin peak (ttP), velocity index (VI, which is the maximum slope of the tangent line), thrombin peak height (PH), and ETP (endogenous thrombin potential, which is the area under the thrombin curve) [18•]. The first three parameters may be regarded as the timing parameters, and the remaining two are the amount parameters. C TG modulation by pathological states and therapeutic modalities. Coagulopathic conditions can shift the normal TG curve (blue) toward insufficient or excessive TG (dark red). Balanced therapeutic intervention acts on both types of coagulopathic TG curves and restores approximately normal TG kinetics (green). In B and C, time 0 corresponds to the TG-initiation time; square brackets denote thrombin concentration
Thrombin-generation analysis can help researchers and clinicians to obtain mechanistic insights into TIC and potentially diagnose it [12, 16••]. Furthermore, biochemical components of the TG network could serve as pharmacologic agents or targets for intervention. Here, we review the recent literature on the role of thrombin and related mechanisms in traumatic bleeding, TIC, and their mitigation. Besides TIC, we touch upon the related phenomenon of surgical coagulopathy. Performing surgery on trauma patients is a frequent challenge for anesthesiologists [3]; moreover, the surgery itself may be considered a special case of (controlled) trauma.
A crucial aspect of physiologic TG is closely linked to the notion of hemostatic balance [17]. This balance is achieved when blood coagulation at the injury site proceeds normally and leads to the cessation of bleeding (i.e., to hemostasis) without excessive intravascular clot formation. In TIC, however, the balance is disrupted [1••]. Therefore, when attempting pharmacologic correction of blood coagulation, it is essential to shift the coagulation process toward its normal state and avoid pushing it too far “to the other side” (i.e., shifting from bleeding to thrombosis and vice versa). We discuss how to avoid the Scylla of hemorrhage and the Charybdis of thrombosis through balanced TG restoration.
The Fundamentals of Thrombin Generation and Coagulopathy Factors
Thrombin generation is initiated when blood flowing from a broken vessel comes in contact with the protein termed tissue factor, which is expressed outside the vascular space. A leading role in this process is played by the enzymatic network triggered by tissue-factor binding; the network propagates enzyme-activation events until thrombin activation is achieved [5]. The main proteins promoting TG — termed procoagulants — are coagulation factors (F) II (prothrombin), FV, FVII, FVIII, FIX, and FX [5]; FXI and FXII may also play some role [7]. It should be noted that the entire protein network responsible for TG, fibrin formation, and fibrinolysis (i.e., biologically controlled fibrin degradation) is very complex and involves enzyme activation and inhibition, protein binding, cofactor action, and protein degradation and contains positive and negative regulatory feedback loops. As an illustration of this complexity, a state-of-the-art mechanistic model of these processes contains 107 protein species and 120 biochemical reactions [18•].
When investigated via in vitro experiments, TG occurs in three phases: initiation, propagation, and termination [5, 19] (alternatively, initiation, amplification, and propagation [7, 12]) (Fig. 1B). Briefly, during initiation, minute amounts of thrombin are generated in blood plasma via enzymatic reactions. Next, localized TG triggers platelet activation, leading to a TG burst on the platelet surface via a positive feedback loop (i.e., the propagation phase). Finally, in the termination phase, thrombin activity is inhibited by antithrombin (a potent direct thrombin inhibitor) and other inhibition mechanisms. Typically, thrombin concentration changes over time as a one-peaked curve (Fig. 1B). To analyze such curves and their changes in a systematic way, researchers look at quantitative TG parameters [18•]. There are five commonly used parameters (nomenclatures vary between test systems): lag time, time to thrombin peak, thrombin peak height, maximum slope of the curve (velocity index), and the area under the curve (endogenous thrombin potential) (Fig. 1B). They represent both the timing of TG and its amount across the three TG phases.
This review is focused on the generation of thrombin. However, other elements of blood coagulation are also essential, and in vivo clot growth can be modulated by any of the following: platelet count and function, polymerization and degradation of fibrin, endothelial activation, blood-flow geometry, and immune-cell activity [1••, 5, 7]. Multiple mechanisms limit excessive clot growth, but most frequently discussed are three endogenous anticoagulants: antithrombin, tissue factor pathway inhibitor (TFPI), and protein C [5]. The existence of these and other control mechanisms in the mammalian blood-coagulation system alludes to the importance of thrombin-level regulation of hemostasis.
TIC and surgical coagulopathy affect the mechanistic aspects of blood coagulation through various coagulopathy factors (i.e., mechanistic drivers of coagulopathy; not to be confused with coagulation factors). The traditional view of coagulopathy emphasized three coagulopathy factors: hemodilution, hypothermia, and acidosis [2]. However, it has become clear that coagulopathic (specifically, prohemorrhagic) conditions can be detected before the onset of, and independently from, the above three factors. This early coagulopathy is termed acute traumatic coagulopathy [20]. Active research of that condition implicated the involvement of protein C as a primary mechanism, but alternative views of that phenomenon exist [21, 22•, 23, 24]. Increased fibrinolysis plays a significant role in coagulopathy [22•, 25], and so does the depletion of specific coagulation factors, such as FV and FVIII [26, 27]. Platelet dysfunction and deficiency, as well as fibrinogen deficiency, can exacerbate coagulopathy [28]. Besides platelets, endothelial cells actively regulate the clot-formation environment, and their dysfunction (endotheliopathy) can contribute to TIC [29]. Thus, many of these (and other) coagulopathy factors can potentially impact TG. Importantly, different coagulopathy factors can be present simultaneously and be manifested to varying degrees in a given TIC case (multifactorial coagulopathy) [2]. Moreover, traumatic coagulopathy is often present in distinct phenotypes, with distinct coagulopathy factors dominant in different patient groups [30•, 31•, 32, 33]. Ultimately, our ability to mitigate coagulopathy is determined by our knowledge of how various coagulopathy factors and their combinations affect different aspects of blood clotting, including TG.
The multifactorial nature of TIC makes it difficult to come up with a single intervention or treatment algorithm applicable to a heterogeneous population of patients. Combined with the natural intersubject variability, the variability in coagulopathy-factor combinations can result in a broad range of phenotypic responses and outcomes. In the presence of this variability, injury severity appears to be a common denominator, with increased injury severity typically leading to more pronounced coagulopathic states [1••, 2]. Severity of the injury can be assessed at bedside using hemodynamic parameters and stat laboratory test results (e.g., lactate) along with pre-defined injury scores and the need for massive transfusion. These clinical parameters may not be easily incorporated into laboratory models of TIC research, but the recent studies have adopted computational, in vitro, and in vivo (mouse) models to investigate the effects of blood-vessel injury size on thrombus growth [34, 35, 36•]. While these studies do not address coagulopathy, they provide a conceptual foundation for future mechanistic research on the effects of coagulation-trigger strength under coagulopathic conditions.
Methods of Thrombin-Generation Measurement
Thrombin generation is measured in vitro, typically in samples collected from human subjects or experimental animals [37, 38]. The samples contain whole blood or plasma and are sometimes altered to represent specific pathological conditions. Thrombin generation is usually initiated by supplementing a reagent containing tissue factor (or a recalcifying agent, if tissue factor is already included in the system), which reflects blood exposure to this protein upon initiation of bleeding [38]. An alternative measurement strategy involves measuring prothrombin-cleavage fragments in the subject’s blood samples, which may be interpreted as characteristic of ongoing TG in the subject’s blood due to (unspecified) intrinsic causes [39, 40].
Conceptually, measuring TG in minimally altered whole blood should be preferable because the latter incorporates all cellular and humoral elements [41]. However, the first whole-blood TG measurements in trauma research were cumbersome (used manual subsampling) and measured the thrombin–antithrombin complex rather than thrombin itself [42, 43]. A different methodological solution relied on fluorogenic thrombin substrates in plasma, which allowed for more efficient, automated thrombin-kinetics measurements. That method, named calibrated automated thrombinoscopy (CAT), has become widely spread [44]. Most CAT applications in trauma and anesthesiology research use platelet-poor plasma, wherein platelets are replaced with externally added phospholipids; the latter form micelles supporting the enzymatic reactions leading to TG. Platelet-poor plasma has often been the preferred choice in TG measurements because of simplified assay standardization and data comparisons. Yet, the CAT assay is also applicable to platelet-rich plasma [38]. Recently, the automated assay was developed further to measure TG in whole blood; the use of this assay — including cases of trauma and coagulopathy — is being actively explored [45•, 46, 47, 48•, 49•]. Moreover, in the form of microfluidic devices, experimental blood-flow models have emerged as a new blood-coagulation investigation strategy [50–52].
To what extent do in vitro TG measurements characterize in vivo TIC? Can we diagnose coagulopathy using TG assays? Currently, the use of TG assays, such as the CAT, for diagnostic purposes in trauma and surgery is problematic and precluded for at least two reasons: assay variability and difficulty of use in clinical settings [38, 53]. Thus, more traditional methods are utilized for coagulopathy diagnostics, such as prothrombin time and viscoelastic coagulation tests [4, 54]. Consequently, in trauma and surgery, TG assays are used predominantly as research tools [53]. Yet, the sensitivity of TG suggests that it could eventually become an informative means of clinical diagnostics [38, 53]. This is particularly true for the recently emerged whole-blood TG measurement technology [16••]. The development of TG-based clinical assays is desirable because that would allow one to verify that the TG-targeting therapeutic interventions are genuinely balanced. A recent example of TG use to guide anticoagulant therapy suggests that this goal may be within reach [55•].
Two challenges complicate the potential of TG as a clinical diagnostic assay. One of them is the intersubject TG variability [18•], which might complicate the diagnostics of coagulopathy based on TG parameters alone. Future development of personalized medicine may provide access to normal TG parameters for each patient, facilitating informative diagnostic comparisons with the subject-specific baseline. Yet, this future currently appears to be remote. In the meantime, TG may need to be used in conjunction with other assays to ascertain reliable diagnostic results. The second challenge is related to TG being an in vitro test. For example, a recent study showed that TG could be preserved even if the plasma is 95% diluted [56]. However, the applicability of this conclusion to clinical situations is doubtful. Deep research is needed to assess the full potential of TG as a point-of-care assay.
Computational Modeling
Complementary to the traditional experimental models of thrombin and fibrin generation in vitro, mechanistic computational modeling has become an essential part of the systems biology concept in blood-coagulation and coagulopathy research [41, 57, 58]. Unlike the statistical models ubiquitous in biomedical literature, these computational models typically consist of time-dependent equations that reflect the production, depletion, binding, activation, and interconversion between the molecular and cellular components represented in the model. Thus, such models can provide a direct link between an observed biological response and its mechanistic underpinnings. The need for computational modeling arises due to the intrinsic complexity of the blood coagulation system, which makes it challenging to generate hypotheses about the system behavior using intuition alone. Computational models facilitate rapid, quantitative hypothesis generation via “virtual screenings” and guide laboratory experimentation and perhaps even clinical studies. Most of such computational models are based on nonlinear ordinary differential equations [18•, 59•, 60••, 61••, 62•, 63, 64, 65•], but algebraic equations [66, 67] and computational fluid dynamics [50, 57, 68•, 69] have also been used. Computational modeling plays a key role in several of the studies cited in this review.
Trauma-induced coagulopathy is not fully understood, and different (often competing) theories exist about its predominant mechanisms [1••, 2]. Experimental research and computational modeling, including TG studies, provide opportunities for focused studies of single or multiple known coagulopathy factors, such as plasma dilution, depletion of specific coagulation proteins, and hypothermia. As mechanistic information accumulates, the models become more accurate, more comprehensive, and increasingly useful in hypothesis generation. These developments hold the promise of providing tools that will ultimately help to unravel the complete mechanistic picture of TIC.
Most traditional computational-modeling approaches focus on TG biochemistry, sometimes combined with blood flow. However, besides the enzymatic reactions, TG (and blood coagulation in general) depends on other factors, such as platelet-activation kinetics and endothelial cells. To reflect this, the new generation of computational models includes additional features, such as platelet action [57] and (hyper)fibrinolysis [68•, 70]. The simplifying assumptions used in model development can be regarded as the necessary first step toward more realistic representations of biology. However, the clinical reality is much more complex, especially in patients with comorbidities and those taking medications (such as antiplatelet drugs) [2]. In such situations, the effects of coagulopathy per se on TG may be particularly difficult to tease out. In any case, the models are mainly intended to streamline laboratory research and are not directly applicable to clinical practice. Therefore, their main benefit is comparable to the discovery and preclinical phases of the typical drug-development process.
Impact of Trauma-Induced Coagulopathy on Thrombin Generation
There are two distinct approaches to investigate the impact of coagulopathy on TG in human blood. One involves using blood (or plasma) samples taken directly from trauma patients. Thrombin generation measured in such samples can be ascribed to TIC superimposed with the individual TG profile of a given patient. However, because the patient’s TG is not measured pre-trauma, there is no baseline to tease out the patient-specific contributions of coagulopathy to the post-trauma TG. (If coagulopathy is expected to result from a planned surgery, then pre-surgery baseline measurements are feasible and should be made.) Moreover, because TIC is often multifactorial, and the information about the severity of each contributing coagulopathy factor may not be readily available, it can be challenging to derive mechanistic conclusions from such measurements.
Another approach is creating coagulopathic states in the test tube — e.g., diluting, cooling, and acidifying plasma or whole blood collected from healthy volunteers. In this analytic approach, we know the contributing coagulopathy factors (and their severities), and subject-specific baseline data are available. However, it can hardly be claimed that such “controlled coagulopathy” fully captures the impact of trauma on blood and its coagulation. The two approaches are complementary, and ultimately both are needed. A third approach, where controlled coagulopathy is induced in an animal, has also been explored [43, 71••, 72]. However, data obtained from animal models cannot be directly used for clinical management in humans due to species-specificity considerations [73, 74].
Initial applications of the CAT assay indicated increased TG in the trauma-patient plasma compared to the normal control group [19, 75]. Other studies also reported elevated TG in trauma but showed that more severely injured and coagulopathic patients had reduced TG compared to the less severely injured ones [76••, 77]. These results can be understood if we posit that, while the occurrence of injury per se increases the TG potential in patient plasma, the onset of coagulopathy (particularly in severe cases) leads to its relative reduction. This notion is supported by a very recent study using a prototype point-of-care device to measure TG in trauma-patient whole blood [16••]. In that study, TG in trauma patients treated as one group exceeded that in the healthy control group; however, in the subgroup of trauma patients with shock and those requiring early massive transfusion, TG was reduced, with thrombin-peak height falling below the healthy-control level. Another recent study, using a different experimental assay, concluded that TG in trauma patients was adequate despite the presence of acute traumatic coagulopathy [40]. Thus, it is plausible that, under the conditions of the study, the coagulopathy phenotype did not affect TG, which happens in some animal trauma models [72]. Alternatively, the trauma-induced TG increase and the coagulopathy-induced TG decrease could have offset each other.
Cardiac surgery — particularly the use of a cardiopulmonary bypass — typically reduces thrombin generation [14, 59•, 65•, 78]. However, in certain situations, thromboembolic complications (apparently associated with uncontrolled thrombin activity) are possible [79, 80]. Remarkably, post-bypass TG can be delayed but have a higher peak than pre-bypass TG, rendering the bypass effects on TG equivocal [81]. As a different example, analysis of TG during liver transplants shows a time-dependent TG-impairment pattern [82•]. Taken together, coagulopathy and TG impairment are relatively common in certain types of complex surgery, but the diagnostic utility of TG has not been firmly established.
A detailed computational and experimental study of controlled multifactorial coagulopathy induced in vitro demonstrated that dilution with normal saline reduces plasma TG, consistent with many prior in vitro studies [18•]. At the same time, it is known that the quantitative effects of dilution on TG can depend on the diluent [42]. Moreover, under certain conditions, TG remains sufficient despite the dilution [56]. The effects of hypothermia on TG are somewhat ambivalent. When assessed by measuring the thrombin–antithrombin complex in whole blood, hypothermia decreases the TG rate [43, 83]. However, when TG is measured in human plasma using the CAT, hypothermia delays the onset of the thrombin peak (consistent with the whole-blood results) but robustly increases the area under the thrombin curve [18•]. What is needed now is to better understand how these in vitro effects translate to in vivo traumatic coagulopathy. For example, the abovementioned ambivalence of hypothermia effects on in vitro TG may suggest that hypothermia exacerbates both the early prohemorrhagic and late prothrombotic TIC phenotypes [18•].
Computational modeling predicted a significant plasma-TG reduction under acidosis [18•], consistent with earlier whole-blood measurements in a porcine model of coagulopathy [43]. However, the corresponding plasma CAT experiment showed no significant effect of acidosis on TG [18•]. An independent study of a synthetic coagulation proteome showed a moderate acidosis-induced late-TG increase, and this result was correlated with reduced inhibitory activity of antithrombin [84]. Recent laboratory studies underscore the technical challenges of rigorous assessment of acidosis effects in vitro [85•, 86, 87]. In summary, a mechanistic understanding of the effects of acidosis on TG, as well as its clinical consequences, requires further in-depth investigations [88•].
Restoration of Thrombin Generation in Coagulopathy
Because TG can be insufficient or excessive in trauma and surgery, it is necessary to develop robust measures for therapeutic TG improvement. Naturally, this improvement should aim to shift TG closer to its normal state but avoid shifting it too far. In that sense, TG restoration should be balanced [17, 89].
It has been suggested that to achieve balanced restoration of TG — and of thrombus formation in general — the pharmacologic intervention must itself be balanced (Fig. 1C). This conclusion was reached in studies of a simplified in vitro system reflecting the possible use of prothrombin complex concentrates (PCCs), which are combinations of purified pro- and anticoagulant proteins [61••, 90]. Such combinations have recently emerged as potential next-generation therapeutics for traumatic and surgical coagulopathy, and their optimal composition is a research topic [91]. Currently available PCC products contain therapeutic amounts of vitamin K–dependent coagulation factors, but they contain notably below-therapeutic amounts of antithrombin [91]. This is logical by design, because most PCCs are generally intended to be used for defined procoagulant-factor deficiency states, including warfarin therapy and hereditary prothrombin deficiency. In addition, PCCs are increasingly used to treat bleeding conditions associated with direct factor Xa and thrombin inhibitors — such as rivaroxaban and dabigatran — when direct antidotes are unavailable [92]. The main purpose of using PCCs in the current clinical practice is to enhance TG, and thus considerations for regulating TG have been largely omitted [93].
Computational modeling with subsequent in vitro experiments suggested that the combination of the procoagulant factors FII, FIX, and FX with a sufficiently large amount of antithrombin can accurately restore TG in plasma diluted with normal saline [61••, 90]. The benefits of combining procoagulants with antithrombin were also highlighted in an independent computational study, where the diluted-plasma composition data had been taken directly from patients on cardiopulmonary bypass [59•]. Traditional coagulation tests, including prothrombin time and thromboelastography, have focused on how fast clotting takes place, but not on the balance of coagulation. If factor Xa and thrombin are not inhibited by antithrombin in a timely manner, there is an increased risk of intravascular thrombus formation [79, 80]. Thus, in the setting of highly complex multifactorial- coagulopathy reduction [18•], it may be logical to supplement both pro- and anticoagulant proteins.
As a next step, it would be informative to explore the efficacy and safety of the balanced-intervention therapeutic paradigm under more complex coagulopathy scenarios, e.g., including hypothermia and acidosis. Computations using an existing model of controlled multifactorial coagulopathy can guide such analysis in the presence of intersubject variability [18•]. Reassuringly, a recent study using a porcine model of trauma concluded that combining PCCs with additional antithrombin improves therapeutic outcomes and reduces the occurrence of thromboembolic events [71••]. The published retrospective study of patients with TIC using the US national Trauma Quality Improvement Program (TQIP) data set over 2 years suggested that the cohort who received fresh frozen plasma (FFP) plus PCC early (< 60 min of the admission) seemed to have lower transfusion requirements in RBCs and FFP when compared to the propensity-matched cohort who received FFP without PCC [94••]. The authors’ secondary analyses suggested a lower in-hospital mortality was associated with FFP plus PCC compared to FFP alone (17.5% vs. 27.7%, P = 0.01) without increasing the risk of deep-vein thrombosis and pulmonary thromboembolism. However, more clinical data are needed to fully assess the safety and efficacy of PCC, as well as PCC in combination with other agents.
There are some clinical data suggesting rebound hypercoagulability and thrombotic potential following the administration of PCCs in trauma patients [95•, 96••]. The use of antithrombin as a primary anticoagulant in a PCC formulation is theoretically supported by its potency as a natural anticoagulant [61••] in the setting of acquired AT deficiency due to traumatic bleeding and surgery [97•, 98]. This concept is further supported by computational modeling and in vitro measurements [61••, 65•, 90, 99]. Further clinical evaluations of antithrombin supplementation are warranted to assess its efficacy to reduce the incidence of venous thromboembolism in trauma [100].
In the context of PCC use to enhance TG, of note is the interaction between thrombin and fibrin. Clinically, fibrinogen supplementation is often used to mitigate coagulopathy by improving thrombus formation [101••]. At the same time, in vitro assays indicate that fibrin reduces thrombin activity by binding with it [102]. However, in other in vitro assays, the resulting decrease in thrombin activity is temporary and is more than compensated by the subsequent TG increase [103]. It is unknown how this would translate to in vivo situations, but computational analyses suggest that both PCC and fibrinogen should be supplemented for simultaneous normalization of thrombin and fibrin levels in coagulopathy [50, 70].
Logically, a balanced therapeutic strategy involving both pro- and anticoagulants could potentially be used for both insufficient and excessive TG (Fig. 1C). While early TIC (hours after trauma) is typically associated with a prohemorrhagic phenotype, late coagulopathy (2–3 days after trauma) may shift the phenotype to a prothrombotic state [1••]. Overall, it is often unclear how the bleeding tendency will develop over time after trauma. Therefore, anticoagulants may need to be administered concurrently with, or following, procoagulant administration. Illustrating this notion, the ability to reduce the risk of both excessive and insufficient TG has been reported for FFP [104••].
FFP has been, and remains, the standard therapeutic strategy to treat traumatic bleeding and coagulopathy, particularly so in the USA [105, 106]. Because FFP is expected to contain all the biochemical blood-coagulation components naturally present in plasma, it may be regarded as an intrinsically balanced intervention to restore normal TG. (Due to its molecular composition, FFP can influence blood coagulation components other than thrombin. For example, it may impact fibrinogen availability and fibrinolysis control.) The same principle is expected to hold for a related product, lyophilized plasma [107]. More generally, the 1:1:1 (plasma:platelets:RBCs) resuscitation paradigm extends the concept of balanced TG to include platelets required for TG enzymes to be fully functional [3, 5].
Despite the perceived advantage of FFP in restoring both procoagulant and anticoagulant proteins, the concentrations and activity status of the coagulation proteins in FFP can be variable; other complications linked to FFP use may also arise [108–110]. To find robust alternatives to FFP, active research is ongoing to compare the efficacy and safety of PCCs with those of FFP in trauma and surgery [111]. Some European centers are starting to use PCC instead of FFP. Indeed, PCC appears to reduce blood-transfusion requirements in coronary surgery [112•], which is consistent with the results of a propensity score–matched cohort study of PCC use in cardiac surgery [113••]. PCCs are now included in the European trauma and surgery recommendations [101••, 114]. Two very recent pilot clinical trials have suggested the feasibility of using PCC as an alternative to FFP [115, 116], and another randomized trial suggested the superiority of PCCs [117••].
A re-emerging paradigm involves using whole blood rather than FFP to mitigate traumatic coagulopathy [118, 119•, 120, 121]. This approach, which has a long history in (mainly military) trauma [120], may be another step in developing the balanced-intervention concept. Published reports indicate similar or improved outcomes when using whole blood compared to blood components [119•, 120, 122]. However, there are also some reservations [1••]. It is possible that, just like the existence of distinct phenotypes in coagulopathy, specific therapeutic modalities (PCCs, FFP, whole blood, etc.) will prove to be advantageous in different traumatic and surgical scenarios [123].
As a final illustration of the concept of balance, here is an example of an unbalanced therapeutic strategy. Recombinant activated FVII (commonly abbreviated as rFVIIa) is a strong procoagulant that was previously considered a promising drug for traumatic bleeding; later its benefits were reconsidered due to accumulating evidence of thromboembolic complications [124]. Both computational and experimental in vitro research on TG in diluted plasma suggested that rFVIIa brings about an intrinsically unbalanced TG modulation. Indeed, it accelerates TG, but the resultant TG profile remains distorted and does not approximate a normal TG time course [61••, 65•, 90]. It is plausible that this distortion is responsible for the high probability of thromboembolism associated with this drug, which came to be regarded only as a means of last resort in traumatic bleeding [125, 126].
Furthermore, it is plausible that a similar type of TG distortion may also characterize PCC formulations lacking anticoagulant components. While it is conceivable that TG may be increased by careful PCC dosing (without supplementing antithrombin) [96••], it may be challenging to achieve a robust balance between insufficient and excessive TG using the dose of procoagulants as the only tunable parameter. Moreover, supplementing antithrombin with PCC may provide a robust solution for the late-phase coagulopathy with a prothrombotic phenotype.
Conclusion
The pivotal roles of TG in hemostasis and pathological thrombosis have been extensively explored through various techniques, including plasma marker measurements, TG assays, and computational modeling. The latter technique is relatively new, but it has provided significant insights into optimal regulation of TG and further development of balanced therapeutic strategies. There are yet many unanswered questions about the applicability of computational TG models to in vivo coagulation. However, computational models are increasingly improved to capture platelet-vascular interactions and platelet-surface TG reactions. These newer models are likely to fill the gap between in silico and in vivo, and they will fuel the future growth of this research field in the years to come.
Change history
23 October 2022
Springer Nature’s version of this paper was updated to structure the references accordingly.
10 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40140-022-00546-w
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Moore EE, Moore HB, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, et al. Trauma-induced coagulopathy Nat Rev Dis Primers. 2021;7:30 An up-to-date, comprehensive review of traumatic coagulopathy.
Savioli G, Ceresa IF, Caneva L, Gerosa S, Ricevuti G. Trauma-induced coagulopathy: overview of an emerging medical problem from pathophysiology to outcomes. Medicines (Basel). 2021;8:16.
Curry N, Brohi K. Surgery in traumatic injury and perioperative considerations. Semin Thromb Hemost. 2020;46:73–82.
Gratz J, Oberladstatter D, Schöchl H. Trauma-induced coagulopathy and massive bleeding: current hemostatic concepts and treatment strategies. Hamostaseologie. 2021;41:307–15.
Mann KG. Thrombin generation in hemorrhage control and vascular occlusion. Circulation. 2011;124:225–35.
van der Meijden PEJ, Heemskerk JWM. Platelet biology and functions: new concepts and clinical perspectives. Nat Rev Cardiol. 2019;16:166–79.
Versteeg HH, Heemskerk JW, Levi M, Reitsma PH. New fundamentals in hemostasis. Physiol Rev. 2013;93:327–58.
Kattula S, Byrnes JR, Wolberg AS. Fibrinogen and fibrin in hemostasis and thrombosis. Arterioscler Thromb Vasc Biol. 2017;37:e13–21.
Wufsus AR, Macera NE, Neeves KB. The hydraulic permeability of blood clots as a function of fibrin and platelet density. Biophys J. 2013;104:1812–23.
Crawley JT, Zanardelli S, Chion CK, Lane DA. The central role of thrombin in hemostasis. J Thromb Haemost. 2007;5(Suppl 1):95–101.
Di Cera E. Thrombin. Mol Aspects Med. 2008;29:203–54.
Negrier C, Shima M, Hoffman M. The central role of thrombin in bleeding disorders. Blood Rev. 2019;38:100582.
Cardenas JC. Thrombin generation following severe trauma: mechanisms, modulators, and implications for hemostasis and thrombosis. Shock. 2021;56:682–90 This informative review highlights the importance of TG studies in trauma.
Fitzgerald J, McMonnies R, Sharkey A, Gross PL, Karkouti K. Thrombin generation and bleeding in cardiac surgery: a clinical narrative review. Can J Anaesth. 2020;67:746–53.
Harr JN, Moore EE, Wohlauer MV, Droz N, Fragoso M, Banerjee A, et al. The acute coagulopathy of trauma is due to impaired initial thrombin generation but not clot formation or clot strength. J Surg Res. 2011;170:319–24.
Coleman JR, Moore EE, Samuels JM, Cohen MJ, Silliman CC, Ghasabyan A, et al. Whole blood thrombin generation in severely injured patients requiring massive transfusion. J Am Coll Surg. 2021;232:709–16 This study demonstrates that trauma can decrease TG below the normal baseline.
Brummel-Ziedins KE. Developing individualized coagulation profiling of disease risk: thrombin generation dynamic models of the pro and anticoagulant balance. Thromb Res. 2014;133(Suppl 1):S9–11.
Mitrophanov AY, Szlam F, Sniecinski RM, Levy JH, Reifman J. Controlled multifactorial coagulopathy: effects of dilution, hypothermia, and acidosis on thrombin generation in vitro. Anesth Analg. 2020;130:1063–76 State-of-the-art computational modeling and experimental validation of the effects of multifactorial coagulopathy on TG parameters.
Dunbar NM, Chandler WL. Thrombin generation in trauma patients. Transfusion. 2009;49:2652–60.
Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003;54:1127–30.
Campbell JE, Meledeo MA, Cap AP. Comparative response of platelet fV and plasma fV to activated protein C and relevance to a model of acute traumatic coagulopathy. PLoS One. 2014;9:e99181.
Chapman MP, Moore EE, Moore HB, Gonzalez E, Gamboni F, Chandler JG, et al. Overwhelming tPA release, not PAI-1 degradation, is responsible for hyperfibrinolysis in severely injured trauma patients. J Trauma Acute Care Surg. 2016;80:16–23 An insightful analysis of the main hyperfibrinolysis trigger in trauma patients.
Davenport RA, Guerreiro M, Frith D, Rourke C, Platton S, Cohen M, et al. Activated protein C drives the hyperfibrinolysis of acute traumatic coagulopathy. Anesthesiology. 2017;126:115–27.
Howard BM, Kornblith LZ, Cheung CK, Kutcher ME, Miyazawa BY, Vilardi RF, et al. Inducing acute traumatic coagulopathy in vitro: the effects of activated protein C on healthy human whole blood. PLOS ONE. 2016;11:e0150930.
Colomina MJ, Mendez E, Sabate A. Altered fibrinolysis during and after surgery. Semin Thromb Hemost. 2021;47:512–9.
Kunitake RC, Howard BM, Kornblith LZ, Christie SA, Conroy AS, Cohen MJ, et al. Individual clotting factor contributions to mortality following trauma. J Trauma Acute Care Surg. 2017;82:302–8.
Rizoli SB, Scarpelini S, Callum J, Nascimento B, Mann KG, Pinto R, et al. Clotting factor deficiency in early trauma-associated coagulopathy. J Trauma. 2011;71:S427–34.
John AE, White NJ. Platelets and fibrinogen: emerging complexity in trauma-induced coagulopathy. Semin Thromb Hemost. 2020;46:125–33.
Kozar RA, Pati S. Syndecan-1 restitution by plasma after hemorrhagic shock. J Trauma Acute Care Surg. 2015;78:S83–6.
Christie SA, Kornblith LZ, Howard BM, Conroy AS, Kunitake RC, Nelson MF, et al. Characterization of distinct coagulopathic phenotypes in injury: pathway-specific drivers and implications for individualized treatment. J Trauma Acute Care Surg. 2017;82:1055–62 This study analyzes heterogeneity in coagulopathic phenotypes.
White NJ, Contaifer D Jr, Martin EJ, Newton JC, Mohammed BM, Bostic JL, et al. Early hemostatic responses to trauma identified with hierarchical clustering analysis. J Thromb Haemost. 2015;13:978–88 This study uses data analysis to identify distinct coagulopathic response phenotypes in trauma.
Savage SA, Zarzaur BL, Brewer BL, Lim GH, Martin AC, Magnotti LJ, et al. 1:1 Transfusion strategies are right for the wrong reasons. J Trauma Acute Care Surg. 2017;82:845–52.
Chin TL, Moore EE, Moore HB, Gonzalez E, Chapman MP, Stringham JR, et al. A principal component analysis of postinjury viscoelastic assays: clotting factor depletion versus fibrinolysis. Surgery. 2014;156:570–7.
Mitrophanov AY, Govindarajan V, Zhu S, Li R, Lu Y, Diamond SL, et al. Microfluidic and computational study of structural properties and resistance to flow of blood clots under arterial shear. Biomech Model Mechanobiol. 2019;18:1461–74.
Mitrophanov AY, Merrill-Skoloff G, Grover SP, Govindarajan V, Kolanjiyil A, Hariprasad DS, et al. Injury length and arteriole constriction shape clot growth and blood-flow acceleration in a mouse model of thrombosis. Arterioscler Thromb Vasc Biol. 2020;40:2114–26.
Tomaiuolo M, Matzko CN, Poventud-Fuentes I, Weisel JW, Brass LF, Stalker TJ. Interrelationships between structure and function during the hemostatic response to injury. Proc Natl Acad Sci U S A. 2019;116:2243–52 A detailed microscopic study of in vivo thrombus formation during hemostasis.
Kintigh J, Monagle P, Ignjatovic V. A review of commercially available thrombin generation assays. Res Pract Thromb Haemost. 2018;2:42–8.
Lancé MD. A general review of major global coagulation assays: thrombelastography, thrombin generation test and clot waveform analysis. Thromb J. 2015;13:1.
Chandler WL, Velan T. Estimating the rate of thrombin and fibrin generation in vivo during cardiopulmonary bypass. Blood. 2003;101:4355–62.
Woolley T, Gwyther R, Parmar K, Kirkman E, Watts S, Midwinter M, et al. A prospective observational study of acute traumatic coagulopathy in traumatic bleeding from the battlefield. Transfusion. 2020;60(Suppl 3):S52–61.
Mann KG, Brummel-Ziedins K, Orfeo T, Butenas S. Models of blood coagulation. Blood Cells Mol Dis. 2006;36:108–17.
Brummel-Ziedins K, Whelihan MF, Ziedins EG, Mann KG. The resuscitative fluid you choose may potentiate bleeding. J Trauma. 2006;61:1350–8.
Martini WZ, Pusateri AE, Uscilowicz JM, Delgado AV, Holcomb JB. Independent contributions of hypothermia and acidosis to coagulopathy in swine. J Trauma. 2005;58:1002–9.
Hemker HC, Giesen P, Al Dieri R, Regnault V, de Smedt E, Wagenvoord R, et al. Calibrated automated thrombin generation measurement in clotting plasma. Pathophysiol Haemost Thromb. 2003;33:4–15.
Ferrara MJ, MacArthur TA, Butenas S, Mann KG, Immermann JM, Spears GM, et al. Exploring the utility of a novel point-of-care whole blood thrombin generation assay following trauma: a pilot study. Res Pract Thromb Haemost. 2021;5:395–402 This study compares whole-blood TG measurements in trauma with the standard CAT assay.
Prior SM, Mann KG, Freeman K, Butenas S. Continuous thrombin generation in whole blood: new applications for assessing activators and inhibitors of coagulation. Anal Biochem. 2018;551:19–25.
Wan J, Konings J, Yan Q, Kelchtermans H, Kremers R, de Laat B, et al. A novel assay for studying the involvement of blood cells in whole blood thrombin generation. J Thromb Haemost. 2020;18:1291–301.
Ninivaggi M, Apitz-Castro R, Dargaud Y, de Laat B, Hemker HC, Lindhout T. Whole-blood thrombin generation monitored with a calibrated automated thrombogram-based assay. Clin Chem. 2012;58:1252–9 This study introduces the whole-blood TG assay.
Coleman JR, Moore EE, Samuels JM, Ryon JJ, Nelson JT, Olson A, et al. Whole blood thrombin generation is distinct from plasma thrombin generation in healthy volunteers and after severe injury. Surgery. 2019;166:1122–7 An informative comparative analysis of whole-blood vs. plasma TG.
Govindarajan V, Rakesh V, Reifman J, Mitrophanov AY. Computational study of thrombus formation and clotting factor effects under venous flow conditions. Biophys J. 2016;110:1869–85.
Li R, Elmongy H, Sims C, Diamond SL. Ex vivo recapitulation of trauma-induced coagulopathy and preliminary assessment of trauma patient platelet function under flow using microfluidic technology. J Trauma Acute Care Surg. 2016;80:440–9.
Trevisan BM, Porada CD, Atala A, Almeida-Porada G. Microfluidic devices for studying coagulation biology. Semin Cell Dev Biol. 2021;112:1–7.
Pagano MB, Chandler WL. Thrombin generation assay: are we ready for prime time? J Appl Lab Med. 2017;2:135–7.
Sumislawski JJ, Christie SA, Kornblith LZ, Stettler GR, Nunns GR, Moore HB, et al. Discrepancies between conventional and viscoelastic assays in identifying trauma-induced coagulopathy. Am J Surg. 2019;217:1037–41.
Menon N, Sarode R, Zia A. Rivaroxaban dose adjustment using thrombin generation in severe congenital protein C deficiency and warfarin-induced skin necrosis. Blood Adv. 2018;2:142–5 A case study demonstrating successful clinical use of a TG assay.
Gratz J, Schlimp CJ, Honickel M, Hochhausen N, Schochl H, Grottke O. Sufficient thrombin generation despite 95% hemodilution: an in vitro experimental study. J Clin Med. 2020;9:3805.
Tsiklidis E, Sims C, Sinno T, Diamond SL. Multiscale systems biology of trauma-induced coagulopathy. Wiley Interdiscip Rev Syst Biol Med. 2018;10:e1418.
Cohen MJ. Use of models in identification and prediction of physiology in critically ill surgical patients. Br J Surg. 2012;99:487–93.
Kremers RM, Bosch YP, Bloemen S, de Laat B, Weerwind PW, Mochtar B, et al. A reduction of prothrombin conversion by cardiac surgery with cardiopulmonary bypass shifts the haemostatic balance towards bleeding. Thromb Haemost. 2016;116:442–51 An insightful study of the potential benefits of antithrombin combined with PCC to improve TG in surgical coagulopathy.
Menezes AA, Vilardi RF, Arkin AP, Cohen MJ. Targeted clinical control of trauma patient coagulation through a thrombin dynamics model. Sci Transl Med. 2017;9:eaaf5045 A computational approach to guide clotting-factor supplementation to mitigate coagulopathy.
Mitrophanov AY, Szlam F, Sniecinski RM, Levy JH, Reifman J. A step toward balance: thrombin generation improvement via procoagulant factor and antithrombin supplementation. Anesth Analg. 2016;123:535–46 This computational and experimental in vitro study analyzes how PCC combined with antithrombin can normalize TG in dilutional coagulopathy.
Tanaka KA, Mazzeffi MA, Strauss ER, Szlam F, Guzzetta NA. Computational simulation and comparison of prothrombin complex concentrate dosing schemes for warfarin reversal in cardiac surgery. J Anesth. 2016;30:369–76 A thorough computational study of warfarin-reversal strategies in cardiac surgery.
Wu TB, Orfeo T, Moore HB, Sumislawski JJ, Cohen MJ, Petzold LR. Computational model of tranexamic acid on urokinase mediated fibrinolysis. PLoS One. 2020;15:e0233640.
Bravo MC, Tejiram S, McLawhorn MM, Moffatt LT, Orfeo T, Jett-Tilton M, et al. Utilizing plasma composition data to help determine procoagulant dynamics in patients with thermal injury: a computational assessment. Mil Med. 2019;184:392–9.
Guzzetta NA, Szlam F, Kiser AS, Fernandez JD, Szlam AD, Leong T, et al. Augmentation of thrombin generation in neonates undergoing cardiopulmonary bypass. Br J Anaesth. 2014;112:319–27 An experimental and computational study demonstrating the effects of a 3-factor-PCC compared to rFVIIa in improving TG after cardiac surgery.
Collins PW, Solomon C, Sutor K, Crispin D, Hochleitner G, Rizoli S, et al. Theoretical modelling of fibrinogen supplementation with therapeutic plasma, cryoprecipitate, or fibrinogen concentrate. Br J Anaesth. 2014;113:585–95.
Schöchl H, Grottke O, Sutor K, Dony K, Schreiber M, Ranucci M, et al. Theoretical modeling of coagulation management with therapeutic plasma or prothrombin complex concentrate. Anesth Analg. 2017;125:1471–4.
Wu TB, Wu S, Buoni M, Orfeo T, Brummel-Ziedins K, Cohen M, et al. Computational model for hyperfibrinolytic onset of acute traumatic coagulopathy. Ann Biomed Eng. 2018;46:1173–82 A spatial model of hyperfibrinolysis and tranexamic acid treatment in coagulopathy.
Link KG, Stobb MT, Di Paola J, Neeves KB, Fogelson AL, Sindi SS, et al. A local and global sensitivity analysis of a mathematical model of coagulation and platelet deposition under flow. PLOS ONE. 2018;13:e0200917.
Mitrophanov AY, Wolberg AS, Reifman J. Kinetic model facilitates analysis of fibrin generation and its modulation by clotting factors: implications for hemostasis-enhancing therapies. Mol BioSyst. 2014;10:2347–57.
Grottke O, Honickel M, Braunschweig T, Reichel A, Schöchl H, Rossaint R. Prothrombin complex concentrate-induced disseminated intravascular coagulation can be prevented by coadministering antithrombin in a porcine trauma model. Anesthesiology. 2019;131:543–54 This study demonstrates the benefits of antithrombin combined with PCC treatment of coagulopathy in an animal model.
Zentai C, van der Meijden PE, Braunschweig T, Hueck N, Honickel M, Spronk HM, et al. Hemostatic therapy using tranexamic acid and coagulation factor concentrates in a model of traumatic liver injury. Anesth Analg. 2016;123:38–48.
van Zyl N, Reade MC, Fraser JF. Experimental animal models of traumatic coagulopathy: a systematic review. Shock. 2015;44:16–24.
Brannstrom A, von Oelreich E, Degerstedt LE, Dahlquist A, Hanell A, Gustavsson J, et al. The swine as a vehicle for research in trauma-induced coagulopathy: introducing principal component analysis for viscoelastic coagulation tests. J Trauma Acute Care Surg. 2021;90:360–8.
Park MS, Xue A, Spears GM, Halling TM, Ferrara MJ, Kuntz MM, et al. Thrombin generation and procoagulant microparticle profiles after acute trauma: a prospective cohort study. J Trauma Acute Care Surg. 2015;79:726–31.
Cardenas JC, Rahbar E, Pommerening MJ, Baer LA, Matijevic N, Cotton BA, et al. Measuring thrombin generation as a tool for predicting hemostatic potential and transfusion requirements following trauma. J Trauma Acute Care Surg. 2014;77:839–45 This study demonstrates the dependence of TG on injury severity in trauma patients.
Matijevic N, Wang YW, Wade CE, Holcomb JB, Cotton BA, Schreiber MA, et al. Cellular microparticle and thrombogram phenotypes in the Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study: correlation with coagulopathy. Thromb Res. 2014;134:652–8.
Coakley M, Hall JE, Evans C, Duff E, Billing V, Yang L, et al. Assessment of thrombin generation measured before and after cardiopulmonary bypass surgery and its association with postoperative bleeding. J Thromb Haemost. 2011;9:282–92.
Williams B, Wehman B, Mazzeffi MA, Odonkor P, Harris RL, Kon Z, et al. Acute intracardiac thrombosis and pulmonary thromboembolism after cardiopulmonary bypass: a systematic review of reported cases. Anesth Analg. 2018;126:425–34.
Lison S, Dietrich W, Braun S, Boehm J, Schuster T, Englhard A, et al. Enhanced thrombin generation after cardiopulmonary bypass surgery. Anesth Analg. 2011;112:37–45.
Franklin SW, Szlam F, Fernandez JD, Leong T, Tanaka KA, Guzzetta NA. Optimizing thrombin generation with 4-factor prothrombin complex concentrates in neonatal plasma after cardiopulmonary bypass. Anesth Analg. 2016;122:935–42.
Abuelkasem E, Hasan S, Mazzeffi MA, Planinsic RM, Sakai T, Tanaka KA. Reduced requirement for prothrombin complex concentrate for the restoration of thrombin generation in plasma from liver transplant recipients. Anesth Analg. 2017;125:609–15 This study demonstrates that PCC can be more efficient than plasma at TG restoration in liver transplant recipients.
Whelihan MF, Kiankhooy A, Brummel-Ziedins KE. Thrombin generation and fibrin clot formation under hypothermic conditions: an in vitro evaluation of tissue factor initiated whole blood coagulation. J Crit Care. 2014;29:24–30.
Gissel M, Brummel-Ziedins KE, Butenas S, Pusateri AE, Mann KG, Orfeo T. Effects of an acidic environment on coagulation dynamics. J Thromb Haemost. 2016;14:2001–10.
Jackson JW, Surov SS, Liang Y, Parunov LA, Ovanesov MV. Effect of pH on thrombin activity measured by calibrated automated thrombinography. Res Pract Thromb Haemost. 2020;4:944–5 This brief article emphasizes the technical difficulties of measuring the effects of pH changes on TG.
Kristensen SR, Nybo J, Pedersen S. Reply to a letter from Jackson J et al. Effect of pH on thrombin activity measured by calibrated automated thrombinography. Res Pract Thromb Haemost. 2020;4:1065.
Kristensen SR, Nybo J, Pedersen S. The effect of pH on thrombin generation - an unrecognized potential source of variation. Res Pract Thromb Haemost. 2020;4:224–9.
Rudnick MR, Blair GJ, Kuschner WG, Barr J. Lactic acidosis and the role of sodium bicarbonate: a narrative opinion. Shock. 2020;53:528–36 An insightful analysis of physiological effects of acidosis.
Brown AC, Levy JH. Maintaining hemostatic balance in treating disseminated intravascular coagulation. Anesthesiology. 2019;131:459–61.
Mitrophanov AY, Rosendaal FR, Reifman J. Therapeutic correction of thrombin generation in dilution-induced coagulopathy: computational analysis based on a data set of healthy subjects. J Trauma Acute Care Surg. 2012;73:S95–102.
Grottke O, Levy JH. Prothrombin complex concentrates in trauma and perioperative bleeding. Anesthesiology. 2015;122:923–31.
Tanaka KA, Shettar S, Vandyck K, Shea SM, Abuelkasem E. Roles of four-factor prothrombin complex concentrate in the management of critical bleeding. Transfus Med Rev. 2021;35:96–103.
Hasan S, Abuelkasem E, Williams B, Henderson R, Mazzeffi MA, Tanaka KA. Factor IX from prothrombin complex concentrate augments low dose tissue factor-triggered thrombin generation in vitro. Br J Anaesth. 2018;121:936–43.
Zeeshan M, Hamidi M, Feinstein AJ, Gries L, Jehan F, Sakran J, et al. Four-factor prothrombin complex concentrate is associated with improved survival in trauma-related hemorrhage: a nationwide propensity-matched analysis. J Trauma Acute Care Surg. 2019;87:274–81 A thorough study highlighting the benefits of PCC use in trauma.
Ekezue BF, Sridhar G, Ovanesov MV, Forshee RA, Izurieta HS, Selvam N, et al. Clotting factor product administration and same-day occurrence of thrombotic events, as recorded in a large healthcare database during 2008–2013. J Thromb Haemost. 2015;13:2168–79 A retrospective analysis of coagulation-factor administration and thromboembolic effects.
Schöchl H, Voelckel W, Maegele M, Kirchmair L, Schlimp CJ. Endogenous thrombin potential following hemostatic therapy with 4-factor prothrombin complex concentrate: a 7-day observational study of trauma patients. Crit Care. 2014;18:R147 A clinical study of PCC effects on TG in trauma patients.
Ehrhardt JD Jr, Boneva D, McKenney M, Elkbuli A. Antithrombin deficiency in trauma and surgical critical care. J Surg Res. 2020;256:536–42 An informative review of acquired antithrombin deficiencies in trauma and surgery.
Matsumoto H, Takeba J, Umakoshi K, Kikuchi S, Ohshita M, Annen S, et al. Decreased antithrombin activity in the early phase of trauma is strongly associated with extravascular leakage, but not with antithrombin consumption: a prospective observational study. Thromb J. 2018;16:17.
Gratz J, Ponschab M, Iapichino GE, Schlimp CJ, Cadamuro J, Grottke O, et al. Comparison of fresh frozen plasma vs. coagulation factor concentrates for reconstitution of blood: an in vitro study. Eur J Anaesthesiol. 2020;37:879–88.
Cardenas JC, Wang YW, Karri JV, Vincent S, Cap AP, Cotton BA, et al. Supplementation with antithrombin III ex vivo optimizes enoxaparin responses in critically injured patients. Thromb Res. 2020;187:131–8.
Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98 An up-to-date, authoritative collection of best practices from the European experts on trauma and coagulopathy.
Mosesson MW, Antithrombin I. Inhibition of thrombin generation in plasma by fibrin formation. Thromb Haemost. 2003;89:9–12.
Hulshof AM, Hemker HC, Spronk HMH, Henskens YMC, Ten Cate H. Thrombin-fibrin(ogen) interactions, host defense and risk of thrombosis. Int J Mol Sci. 2021;22:2590.
Cardenas JC, Cap AP, Swartz MD, Huby Mdel P, Baer LA, Matijevic N, et al. Plasma resuscitation promotes coagulation homeostasis following shock-induced hypercoagulability. Shock. 2016;45:166–73 This study investigates the ability of FFP to both reduce excessive TG and improve insufficient TG in trauma.
Chang R, Holcomb JB. Implementation of massive transfusion protocols in the United States: the relationship between evidence and practice. Anesth Analg. 2017;124:9–11.
Treml AB, Gorlin JB, Dutton RP, Scavone BM. Massive transfusion protocols: a survey of academic medical centers in the United States. Anesth Analg. 2017;124:277–81.
Iapichino GE, Ponschab M, Cadamuro J, Sussner S, Gabriel C, Dieplinger B, et al. Concentrated lyophilized plasma used for reconstitution of whole blood leads to higher coagulation factor activity but unchanged thrombin potential compared with fresh-frozen plasma. Transfusion. 2017;57:1763–71.
Matijevic N, Kostousov V, Wang YW, Wade CE, Wang W, Letourneau P, et al. Multiple levels of degradation diminish hemostatic potential of thawed plasma. J Trauma. 2011;70:71–9.
Mitrophanov AY, Szlam F, Sniecinski RM, Levy JH, Reifman J. In Response. Anesth Analg. 2017;124:699–700.
Muller MC, Straat M, Meijers JC, Klinkspoor JH, de Jonge E, Arbous MS, et al. Fresh frozen plasma transfusion fails to influence the hemostatic balance in critically ill patients with a coagulopathy. J Thromb Haemost. 2015;13:989–97.
van den Brink DP, Wirtz MR, Neto AS, Schöchl H, Viersen V, Binnekade J, et al. Effectiveness of prothrombin complex concentrate for the treatment of bleeding: a systematic review and meta-analysis. J Thromb Haemost. 2020;18:2457–67.
Biancari F, Ruggieri VG, Perrotti A, Gherli R, Demal T, Franzese I, et al. Comparative analysis of prothrombin complex concentrate and fresh frozen plasma in coronary surgery. Heart Lung Circ. 2019;28:1881–7 This study suggests that PCC compared to FFP may reduce the need for blood transfusion in cardiac surgery.
Nemeth E, Varga T, Soltesz A, Racz K, Csikos G, Berzsenyi V, et al. Perioperative factor concentrate use is associated with more beneficial outcomes and reduced complication rates compared with a pure blood product-based strategy in patients undergoing elective cardiac surgery: a propensity score-matched cohort study. J Cardiothorac Vasc Anesth. 2022;36:138–46 This article suggests that PCC use leads to a reduction in blood-product needs in cardiac surgery.
Erdoes G, Koster A, Ortmann E, Meesters MI, Bolliger D, Baryshnikova E, et al. A European consensus statement on the use of four-factor prothrombin complex concentrate for cardiac and non-cardiac surgical patients. Anaesthesia. 2021;76:381–92.
Karkouti K, Bartoszko J, Grewal D, Bingley C, Armali C, Carroll J, et al. Comparison of 4-factor prothrombin complex concentrate with frozen plasma for management of hemorrhage during and after cardiac surgery: a randomized pilot trial. JAMA Netw Open. 2021;4:e213936.
Green L, Roberts N, Cooper J, Agarwal S, Brunskill SJ, Chang I, et al. Prothrombin complex concentrate vs. fresh frozen plasma in adult patients undergoing heart surgery - a pilot randomised controlled trial (PROPHESY trial). Anaesthesia. 2021;76:892–901.
Innerhofer P, Fries D, Mittermayr M, Innerhofer N, von Langen D, Hell T, et al. Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017;4:e258-71 A clinical trial whose results suggest PCC superiority compared to FFP for coagulopathy mitigation.
Sheppard FR, Schaub LJ, Cap AP, Macko AR, Moore HB, Moore EE, et al. Whole blood mitigates the acute coagulopathy of trauma and avoids the coagulopathy of crystalloid resuscitation. J Trauma Acute Care Surg. 2018;85:1055–62.
Shea SM, Staudt AM, Thomas KA, Schuerer D, Mielke JE, Folkerts D, et al. The use of low-titer group O whole blood is independently associated with improved survival compared to component therapy in adults with severe traumatic hemorrhage. Transfusion. 2020;60(Suppl 3):S2-9 This study shows that whole blood use is associated with improved survival in trauma patients.
Spinella PC, Cap AP. Whole blood: back to the future. Curr Opin Hematol. 2016;23:536–42.
McCoy CC, Cotton BA, Brenner M, Roberts D, Ferrada P, Horer T, et al. Back to the future: whole blood resuscitation of the severely injured trauma patient. Shock. 2021;56:9–15.
Seheult JN, Anto V, Alarcon LH, Sperry JL, Triulzi DJ, Yazer MH. Clinical outcomes among low-titer group O whole blood recipients compared to recipients of conventional components in civilian trauma resuscitation. Transfusion. 2018;58:1838–45.
Wade CE, Cardenas JC, Cap AP. Reply to: Is “thrombin burst” now the worst option in trauma? Shock. 2017;47:781–2.
O’Connell KA, Wood JJ, Wise RP, Lozier JN, Braun MM. Thromboembolic adverse events after use of recombinant human coagulation factor VIIa. JAMA. 2006;295:293–8.
Mamtani R, Nascimento B, Rizoli S, Pinto R, Lin Y, Tien H. The utility of recombinant factor VIIa as a last resort in trauma. World J Emerg Surg. 2012;7(Suppl 1):S7.
Palmason R, Vidarsson B, Sigvaldason K, Ingimarsson JP, Gudbjartsson T, Sigurdsson GH, et al. Recombinant factor VIIa as last-resort treatment of desperate haemorrhage. Acta Anaesthesiol Scand. 2012;56:636–44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alexander Y. Mitrophanov declares that he has no conflict of interest. Kofi Vandyck declares that he has no conflict of interest. Kenichi A. Tanaka has served on an advisory board for Octapharma relating to the clinical study of prothrombin complex concentrate, but did not receive any input from the company relating to the preparation of this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Blood Management
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mitrophanov, A.Y., Vandyck, K. & Tanaka, K.A. Thrombin Generation in Trauma Patients: How Do we Navigate Through Scylla and Charybdis?. Curr Anesthesiol Rep 12, 308–319 (2022). https://doi.org/10.1007/s40140-021-00502-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00502-0