Abstract
Point-of-care (POC) ultrasonography can be defined as ultrasonography brought to the patient and performed by the provider in real time. Anesthesiologists commonly use this modality to aid regional anesthesia and central vascular access. However, as POC ultrasonography has been further developed, utility of this technology has increased in the areas of hemodynamic monitoring, cardiopulmonary function, and other areas that are relevant for the perioperative physician. This manuscript seeks to provide a review of the literature of point-of-care ultrasound topics that are relevant for the anesthesiologist. These topics will include (I) assessment of preload and fluid responsiveness, (II) assessment of mechanisms of hypotension and shock, (III) evaluation of pulmonary function, (IV) advanced vascular access, and (V) additional areas of POC ultrasound for perioperative improvement. Finally, this manuscript will suggest a novel POC ultrasound curriculum that integrates the components of this review into a comprehensive perioperative ultrasound examination, abbreviated as FORESIGHT (focused, perioperative, risk, evaluation, sonography, involving, gastro-abdominal, hemodynamic, and trans-thoracic ultrasound) exam.









Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grocott MP, Pearse RM. Perioperative medicine: the future of anaesthesia? Br J Anaesth. 2012;108(5):723–6.
Alpert JS, Mladenovic J, Hellmann DB. Should a hand-carried ultrasound machine become standard equipment for every internist? Am J Med. 2009;122(1):1–3.
Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007;35(5 Suppl):S126–30.
•• Ramsingh D, R.J., Kain Z, Strom S, Canales C, Alexander B, Capatina A, Ma M, Le K, Cannesson M, Impact assessment of perioperative point of care ultrasound training anesthesiology (Forthcoming 2015). This upcoming publication highlights a perioperative “whole-body” point of care ultrasound curricuium for anesthesiologists and suggests the potential for its postivie clinical impact.
Bundgaard-Nielsen M, et al. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand. 2007;51(3):331–40.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774–81.
Ommen SR, et al. Assessment of right atrial pressure with 2-dimensional and Doppler echocardiography: a simultaneous catheterization and echocardiographic study. Mayo Clin Proc. 2000;75(1):24–9.
Prekker ME, et al. Point-of-care ultrasound to estimate central venous pressure: a comparison of three techniques. Crit Care Med. 2013;41(3):833–41.
Gillman LM, et al. Clinician performed resuscitative ultrasonography for the initial evaluation and resuscitation of trauma. Scand J Trauma Resusc Emerg Med. 2009;17:34.
Barbier C, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30(9):1740–6.
Cannesson M, et al. Prediction of fluid responsiveness using respiratory variations in left ventricular stroke area by transoesophageal echocardiographic automated border detection in mechanically ventilated patients. Crit Care. 2006;10(6):R171.
Scheuren K, et al. Left ventricular end-diastolic area is a measure of cardiac preload in patients with early septic shock. Eur J Anaesthesiol. 2009;26(9):759–65.
Subramaniam B, Talmor D. Echocardiography for management of hypotension in the intensive care unit. Crit Care Med. 2007;35(8 Suppl):S401–7.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134(1):172–8.
Gelman S. Venous function and central venous pressure: a physiologic story. Anesthesiology. 2008;108(4):735–48.
Howell MD, et al. Occult hypoperfusion and mortality in patients with suspected infection. Intensive Care Med. 2007;33(11):1892–9.
Sefidbakht S, et al. Sonographic measurement of the inferior vena cava as a predictor of shock in trauma patients. Emerg Radiol. 2007;14(3):181–5.
Broch O, et al. Variation of left ventricular outflow tract velocity and global end-diastolic volume index reliably predict fluid responsiveness in cardiac surgery patients. J Crit Care. 2012;27(3):325e7–13.
Charron C, et al. Echocardiographic measurement of fluid responsiveness. Curr Opin Crit Care. 2006;12(3):249–54.
Feissel M, et al. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest. 2001;119(3):867–73.
Monge Garcia MI, Gil Cano A, Diaz Monrove JC. Brachial artery peak velocity variation to predict fluid responsiveness in mechanically ventilated patients. Crit Care. 2009;13(5):R142.
Monnet X, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34(5):1402–7.
Lamia B, et al. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med. 2007;33(7):1125–32.
Maizel J, et al. Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med. 2007;33(7):1133–8.
Levitov A, Marik PE. Echocardiographic assessment of preload responsiveness in critically ill patients. Cardiol Res Pract. 2012;2012:819696.
Mahjoub Y, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med. 2010;38(9):1824–9.
Rozycki GS, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995;39(3):492–8.
Rodriguez A, DuPriest RW Jr, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457–9.
Perry JF Jr, DeMeules JE, Root HD. Diagnostic peritoneal lavage in blunt abdominal trauma. Surg Gynecol Obstet. 1970;131(4):742–4.
Scalea TM, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma. 1999;46(3):466–72.
Rose JS. Ultrasound in abdominal trauma. Emerg Med Clin North Am. 2004;22(3):581–599, vii.
Kirkpatrick AW, et al. Prospective evaluation of hand-held focused abdominal sonography for trauma (FAST) in blunt abdominal trauma. Can J Surg. 2005;48(6):453–60.
Andersen GN, et al. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr. 2011;12(9):665–70.
Gunst M, et al. Accuracy of cardiac function and volume status estimates using the bedside echocardiographic assessment in trauma/critical care. J Trauma. 2008;65(3):509–16.
Beaulieu Y. Bedside echocardiography in the assessment of the critically ill. Crit Care Med. 2007;35(5 Suppl):S235–49.
Joseph MX, et al. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest. 2004;126(5):1592–7.
Manasia AR, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth. 2005;19(2):155–9.
Mazraeshahi RM, Farmer JC, Porembka DT. A suggested curriculum in echocardiography for critical care physicians. Crit Care Med. 2007;35(8 Suppl):S431–3.
Lichtenstein D, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9–15.
Vignon P, et al. Quantitative assessment of pleural effusion in critically ill patients by means of ultrasonography. Crit Care Med. 2005;33(8):1757–63.
Bedetti G, et al. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound. 2006;4:34.
Eibenberger KL, et al. Quantification of pleural effusions: sonography versus radiography. Radiology. 1994;191(3):681–4.
Bouhemad B, et al. Clinical review: bedside lung ultrasound in critical care practice. Crit Care. 2007;11(1):205.
Ueda K, Ahmed W, Ross AF. Intraoperative pneumothorax identified with transthoracic ultrasound. Anesthesiology. 2011;115(3):653–5.
Monti JD, Younggren B, Blankenship R. Ultrasound detection of pneumothorax with minimally trained sonographers: a preliminary study. J Spec Oper Med. 2009;9(1):43–6.
Lichtenstein D, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999;25(9):955–8.
Doust BD, et al. Ultrasonic evaluation of pleural opacities. Radiology. 1975;114(1):135–40.
Agricola E, et al. “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest. 2005;127(5):1690–5.
Gargani L, et al. Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: a comparison with natriuretic peptides. Eur J Heart Fail. 2008;10(1):70–7.
Costantino TG, et al. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456–61.
Keyes LE, et al. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34(6):711–4.
Ashworth A, Arrowsmith JE. Ultrasound-guided arterial cannulation. Eur J Anaesthesiol. 2010;27(3):307.
Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound-guided and blindly placed radial arterial catheters. Acad Emerg Med. 2006;13(12):1275–9.
Stolz LA, et al. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. J Vasc Access. 2015;16(4):321–6.
Wu SY, et al. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology. 2013;118(2):361–75.
Troianos CA, et al. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg. 2012;114(1):46–72.
Nazerian P, et al. Accuracy of point-of-care multiorgan ultrasonography for the diagnosis of pulmonary embolism. Chest. 2014;145(5):950–7.
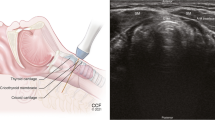
Muslu B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30(5):671–6.
Ramsingh D, Haughton FE, Schilling J, Gimenez K, Banh E, Rinehart J, Cannesson M. Auscultation vs. point of care ultrasound to determine endotracheal versus bronchial intubation: a diagnostic accuracy study. Anesthesiology 2015.
Perlas A, et al. Ultrasound assessment of gastric content and volume. Anesthesiology. 2009;111(1):82–9.
Perlas A, et al. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg. 2011;113(1):93–7.
Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87(1):34–40.
Tayal VS, et al. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49(4):508–14.
• Manno E et al. Deep impact of ultrasound in the intensive care unit: the “ICU-sound” protocol. Anesthesiology 2012;117(4):801–9. This study demonstrated the use of a comprehensive point of care ultrasound examination upon admission to the intensive care unit results in a high prevalence of unsuspected clinical abnormalities.
•• Botker MT et al. Routine pre-operative focused ultrasonography by anesthesiologists in patients undergoing urgent surgical procedures. Acta Anaesthesiol Scand 2014;58(7):807–14. This study demonstrated that pre-operative focused cardiopulmonary ultrasonography disclosed unexpected pathology in patients undergoing urgent surgical procedures and induced changes in the anesthesia management.
•• Killu K et al. Model point-of-care ultrasound curriculum in an intensive care unit fellowship program and its impact on patient management. Crit Care Res Pract 2014;2014:934796. This study assessed the clinical impact of establishing a Point-of-Care (POC) ultrasound curriculum into an intensive care unit (ICU) fellowship program and was associated with an increase in new diagnosis in about 2/3 and change in management in over 1/3 of ICU patients studied.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Davinder Ramsingh, Sumit Singh, Mike Ross, Wendell Williams, and Maxime Cannesson declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cardiovascular Anesthesia.
Appendix
Appendix
See Fig. 10.
Rights and permissions
About this article
Cite this article
Ramsingh, D., Singh, S., Ross, M. et al. Review of Point-of-Care (POC) Ultrasound for the 21st Century Perioperative Physician. Curr Anesthesiol Rep 5, 452–464 (2015). https://doi.org/10.1007/s40140-015-0137-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-015-0137-2