Abstract
Purpose of Review
Albumin is a colloid used in fluid resuscitation, with intrinsic physiologic properties that make it ideal to use for certain hypotensive patients. Despite this, its indications for use in this context are the source of much debate. This review aims to provide an overview of the history of albumin, explain its rise and fall in popularity, and identify situations where use of albumin may be beneficial over other forms of fluid resuscitation.
Recent Findings
The use of albumin dropped significantly in 1998 after a review article was published suggesting that it was harmful to use in critically ill patients. It was not until 2004 and 2014 when the first large-scale randomized control trials were performed demonstrating that albumin administration in certain hypotensive critically ill patients was associated with decreased morbidity and mortality.
Summary
Compared to other fluids, albumin appears to be safe for most patient populations. Choice of resuscitation fluid is partly provider dependent; however, there is an increasing body of evidence supporting albumin use associated with improved patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the acutely ill patient, hypotension is typically one of the heralding signs that the body is progressing towards a state of shock: physiologic dysregulation marked by the decreased ability of the body to maintain end organ perfusion [1]. When this occurs, one of the measures by which clinicians can restore blood pressure is through the administration of fluids. Throughout medical history, many different types of fluids have been developed; however, there continues to be clinical equipoise regarding which fluid is ideal for this purpose. Human albumin, a serum protein synthesized by the liver and derived from blood, is a colloid solution that was developed in the 1940s as a means of fluid resuscitation in military casualties during World War II [2]. One of the qualities of albumin that theoretically make it an ideal fluid for use in resuscitating hypotensive patients is its ability to maintain intravascular oncotic pressure. This can improve blood pressure for longer periods of time relative to the amount of fluid used, while reducing the amount of fluid extravasation to the interstitium (e.g., “third spacing”). There have been numerous studies that have investigated the safety and efficacy of human albumin in fluid resuscitation, with mixed results. In this review, we seek to explore the role of albumin in the resuscitation of hypotensive patients, and define whether or not there is any demonstrated benefit in using human albumin for fluid resuscitation in hypotensive patients over other types of fluid.
History of Albumin
Albumin has a long history and has been one of the earliest studied proteins of the human body. It was first described by the Greek physician Hippocrates, when he implicated the protein albumin as the link between foamy urine and kidney disease, recorded in his Aphorisms [3]. Around 1500 AD, Swiss physician Paracelsus caused the precipitation of albumin by adding vinegar to a sample of human urine [4]. Scientist Frederick Dekkers was able to isolate albumin by heat fractionation in the late eighteenth century [5], and in 1837, Henry Ancell identified albumin as a key component to blood serum [6]. It was first utilized as a resuscitation fluid in the 1940s by a surgeon named I.S. Ravdin during the US Pearl Harbor attacks, when there arose a need to create a stable substitute for blood plasma [4]. Ravdin used albumin to resuscitate seven sailors who had been badly burned in the attacks, and all seven survived. This led to its popularity, production, and study of how albumin could be best utilized [4].
Properties of Albumin
Albumin, specifically human serum albumin, is a monomeric protein with a molecular mass of 66.5 kDa and a serum half-life of about 21 days. It is synthesized by the liver and is the most abundant protein type in the blood. Albumin has several functions, the most notable being a determinant of plasma colloid oncotic pressure. Once synthesized, it gets released into the bloodstream at a rate of about 10–15 g/day, where it functions to raise the colloid oncotic pressure and act as a transporter of both endogenous and exogenous ligands [7]. It also has antioxidant properties, since its molecular structure allows it to bind readily to ligands to scavenge reactive oxygen species [8].
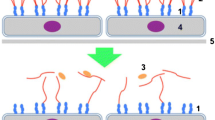
Albumin is one of several different colloid fluids that can be used in resuscitation. By definition, a colloid fluid is an electrolyte solution with an added homogenous high molecular weight substance that generates oncotic pressure by remaining in the intravascular space [9]. Both the rate and direction of fluid exchange between the intravascular space and interstitium is determined by the hydrostatic pressure inside the blood vessel, minus the colloid oncotic pressure [10]. When lying supine, the normal intravascular hydrostatic pressure is ~ 20 mmHg, whereas the colloid oncotic pressure of plasma is ~ 28 mmHg, which favors movement of fluid into the intravascular space in order to preserve plasma volume [10]. Iso-oncotic 5% albumin has a colloid oncotic pressure of 20 mmHg, whereas 25% albumin has a colloid oncotic pressure of 70 mmHg [11]. Both formulations have a duration of effect of approximately 12 h. Five percent albumin has a volume expansion effect of 80–100% of the initial infused volume, whereas 25% albumin has a volume expansion effect of 200–400% [11].
Albumin Compared to Other Colloids
While human albumin demonstrates one of the earliest uses of colloid, the other types of colloid fluids commonly used for intravascular volume expansion include fresh frozen plasma (FFP), dextrans, gelatin, and hydroxyethyl starch (HES) solutions. FFP and albumin are natural colloids, while dextrans and starches are synthetic colloids. The use of FFP as fluid resuscitation tends to be limited to situations in which there is massive hemorrhage, in trauma and burn victims, and to reverse coagulopathy [12]. It does not appear to be ideal to use as a primary resuscitation fluid owing to the fact that it is not shelf-stable (needs to be used within 24 h of thawing), and moreover has an increased risk of both immunogenic and non-immunogenic complications, such as transfusion-associated circulatory overload, hemolytic transfusion reactions due to failure of ABO matching, and transmission of infectious agents such as HIV, hepatitis B, and hepatitis C [12]. Dextrans comprise a group of single chain polymers of bacterial origin, prepared in 40 kD, 60 kD, and 70 kD formulations [13]. Use of dextrans has declined in recent years due to their association with osmotically mediated renal injury [14, 15], anaphylactoid reactions [16], and increased bleeding risk from impaired platelet aggregation and decreased levels of factor VIII and von Willebrand factor [17]. HES preparations are composed of natural polysaccharides that have been chemically modified by hydroxyethylation to stabilize the solution against alpha-amylase degradation in vivo [13]. Use of HES solutions have declined over the years due to reports of increased risk of renal injury [18,19,20] and altered hemostasis conferring increased bleeding risk [17, 21]. Gelatin is a degradation product of collagen and has been used as a plasma expander, however has a comparable risk of allergic reactions compared to dextrans [22], and may additionally confer an increased risk of coagulopathy compared to other colloids [23]. For these reasons, albumin has risen significantly in popularity as the colloid agent of preference for fluid resuscitation.
Colloid vs Crystalloid
The debate between whether crystalloid or colloid fluids are most appropriate for resuscitation has been long standing. The early use of large volume crystalloid fluid resuscitation, particularly balanced crystalloids, has proven mortality benefit in patients with severe sepsis and septic shock [24]. A multitude of randomized control trials (RCTs) have been published looking at the effects of crystalloid vs colloid in fluid resuscitation, and from these there have been several large-scale systematic reviews and meta-analyses.
In 2014, a systematic review and network meta-analysis by Rochwerg et al. identified 14 RCTs involving approximately 19,000 participants that investigated mortality benefit of fluid resuscitation with albumin, HES, gelatin, dextran, and crystalloid (both balanced and unbalanced) in critically ill patients with severe sepsis and septic shock. The result of the analysis suggested that both albumin and balanced crystalloid solutions conferred a mortality benefit when used for resuscitation of patients in this population, compared to the other fluid types analyzed [25].
Tseng et al. revisited the topic in 2020 with their own systematic review and network meta-analysis, which looked at 58 RCTs involving approximately 26,300 participants. In addition to including a larger pool of studies for analysis, the group reported on seven fluid types: balanced crystalloids, unbalanced crystalloids, dextran, gelatin, iso-oncotic albumin, hyperoncotic albumin, low molecular weight HES, and high molecular weight HES. Moreover, the study delineated patient subgroups, separating outcomes from sepsis, surgery, trauma, and traumatic brain injury (TBI). The results from this analysis demonstrated that balanced crystalloids and albumin (both hyperoncotic and iso-oncotic) are associated with increased survival, decreased risk of acute kidney injury, and less red blood cell transfusion volume in septic and surgical patients when compared to the other fluids. Interestingly, the study outcomes differed for patients with TBI, as there was a greater mortality benefit with use of normal saline and low molecular weight HES compared to isotonic solutions, including albumin and balanced crystalloid solutions [26].
In 2019, Martin and Bassett published a systematic review and meta-analysis that sought to identify whether crystalloid fluid resuscitation alone is sufficient for critically ill patients in the ICU, or whether the addition of colloids conferred improved outcomes, focusing on hemodynamic endpoints such as central venous pressure (CVP), mean arterial pressure (MAP), and cardiac index, as well as patient-centered endpoints such as all-cause and 90-day mortality. Fifty-five RCTs involving about 27,000 participants were identified and analyzed. The results of this analysis demonstrated that the use of albumin was associated with a higher cardiac index, CVP, and MAP. In addition, the results demonstrated that using crystalloid resuscitation alone was associated with higher volumes of fluid administered and a greater positive fluid balance compared with albumin [27], a metric associated with adverse patient outcomes [28].
The 1998 Cochrane Review and its Effects on Albumin Use
Since its inception in the 1940s until the late 1990s, interest in the use of human albumin solutions over other fluid types has increased substantially [29]; however, more widespread use had been limited by the lack of high-quality clinical trials demonstrating clear benefit in safety and efficacy of albumin over other types of fluid resuscitation. In 1998, a review article by the Cochrane Injuries Group was published by the British Medical Journal, with the aim of quantifying the effect on mortality of administering human albumin for fluid resuscitation in management of critically ill patients [30•]. The review analyzed 30 randomized controlled trials that included a total of 1419 patients, with the primary outcome measure being all-cause mortality at the end of follow-up from each trial. Of the initial 32 trials that met inclusion criteria, albumin was primarily used for burns, hypoproteinemia, and hypotension associated with trauma, sepsis, post-surgical, preterm infant, and vascular leak syndrome patients. The results of this review suggested that there was no evidence that albumin reduced mortality, and that there was in fact an associated increased risk of death in patients administered albumin, compared to patients not administered albumin.
In the years following the publication of the Cochrane review, use of human albumin in the UK dropped by 40% [32]. Several responses sent to and published by the British Medical Journal supported the conclusions drawn from the review, further propagating the notion that albumin was indeed harmful and should be avoided [33, 34]. Moreover, the United States Food and Drug Administration issued a warning statement agreeing with the results of the Cochrane review and urging physicians to use discretion when administering albumin [35]. Conversely, critics of the Cochrane review have pointed out the flaws in its study design—specifically, the small number of trials analyzed, with a similarly small number of patients observed, confers insufficient power to the study to support its sweeping assertion that albumin may actually be dangerous [36]. A subsequent meta-analysis by Wilkes and Navickis published in 2001 sought to identify the outcomes of patient survival after human albumin administration. The analysis looked at the results of 55 trials involving 3504 patients and concluded that there was no statistically significant increase in mortality of patients who received albumin-containing fluid [37]. Ultimately, the controversy sparked by the Cochrane review highlighted the need for more high-quality randomized control trials to further characterize the harm vs benefit of albumin as fluid resuscitation in critically ill patients.
Studies Investigating Use of Albumin for Resuscitation
Following the Cochrane review, one of the first large-scale, multi-center, double-blinded, randomized control trials that investigated the safety and efficacy of albumin in critically ill patients was the Saline versus Albumin Fluid Evaluation (SAFE) Study [38••]. Investigators performed the study across 16 intensive care units in Australia and New Zealand, testing the hypothesis that there was no difference in 28-day all-cause mortality when using 4% albumin vs 0.9% normal saline for intravascular fluid resuscitation. The study recruited adults aged 18 or older, of which 6997 were included in the data analysis: 3497 patients were assigned to the albumin group, 3500 patients were assigned to the saline group. Patients were further stratified into six predefined subgroups based on presence or absence of trauma, severe sepsis, or acute respiratory distress syndrome (ARDS). The primary outcome measure was all-cause mortality 28 days after randomization, and secondary endpoints included survival time within the first 28 days, proportion of patients who had developed new organ failure, the duration of mechanical ventilation, the duration of renal replacement therapy (RRT), and the duration of the ICU and hospital stay.
The results of the trial demonstrated that between the two groups, there was no difference in 28-day all-cause mortality, and that the secondary outcomes at day 4 were equivalent in both groups. The study authors highlighted that there was a greater volume of packed red blood cell (PRBC) transfusions required in the patients assigned to the albumin group within the first 2 days of the trial (an average of 71 mL of PRBCs per patient), an effect speculated to be due to possible increased effects of hemodilution and transient alterations in coagulation with albumin compared to saline. In addition, there was concern of an increased incidence of mortality in trauma patients when administered albumin compared to normal saline, since there was noted to be an increased relative risk of death in trauma patients, specifically patients with traumatic brain injury (TBI). To address this concern, the SAFE study investigators conducted a post hoc follow-up study investigating use of saline versus albumin in patients with TBI, identifying 460 patients included in the original SAFE trial who also had severe TBI (Glasgow Coma Scale score of 3–8) [39]. They found that mortality rates within 28 days were significantly higher in patients with TBI who received albumin compared to saline.
In 2014, investigators in Italy conducted the ALBIOS trial: a multicenter, open-label, randomized control trial designed to observe the effects of fluid resuscitation with crystalloid combined with albumin, versus crystalloid alone, in patients with severe sepsis or septic shock [40••]. In this study, albumin was supplemented along with crystalloid to obtain a target serum albumin level of 30 g/L in 1800 patients across 100 ICUs. The primary outcome measure was all-cause mortality 28 days after randomization; secondary outcomes included 90-day all-cause mortality, degree of organ dysfunction, and length of stay in the ICU and in the hospital. Tertiary outcomes were also measured in post hoc analysis and included incidence of use of RRT, incidence of acute kidney injury, duration of mechanical ventilation, and duration of use of vasopressor or inotropic agents. The results of the study demonstrated that there was no difference in either the primary or secondary outcome measures between the two groups. Despite this, patients in the albumin supplementation group achieved higher targeted MAPs, lower positive net fluid balance, and decreased time to suspension of catecholamines. These physiologic and hemodynamic benefits were especially evident in the post hoc analysis resulting in the findings that in patients with septic shock, mortality in the albumin group was significantly lower at 90 days compared to the crystalloid group.
Discussion
In choosing which fluid to administer to patients with hypotension, healthcare providers need to consider a multitude of factors: disease state, presence of end organ dysfunction, and hemodynamic parameters, all of which can potentially affect outcomes such as morbidity and mortality, as well as length of ICU and hospital stay. Intravascular volume resuscitation is an important intervention to maintain circulatory function and end organ perfusion. Crystalloid fluids are better studied and more commonly used over colloids given they are cheaper to produce, and natural colloids are a resource limited by the availability of human blood donors. Synthetic colloids have in recent years fallen out of favor due to the incidence of adverse side effects, without demonstrating superiority to human serum albumin. The debate as to whether use of albumin confers harm or benefit when used for fluid resuscitation is one that has proven to be divisive. Nonetheless, there is data to support the assertion that albumin is at least non-inferior to crystalloid fluid when used in hypotensive states, and that albumin may in fact even confer certain benefits over crystalloid, such as improved MAP and CVP, decreased catecholamine duration, and decreased positive fluid balance [41].
Conclusion
The above review of the current body of literature suggests that albumin can be a safe and effective fluid to use in the resuscitation of select hypotensive patients, especially in those with septic shock and/or hypoalbuminemia. The issue of albumin use as a mainstay of fluid resuscitation in the hospital now is one wherein cost-effectiveness and resource availability becomes a major consideration. Further studies are needed to elucidate specific clinical scenarios where albumin is best used for resuscitation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sharma S, Hashmi MF, Bhattacharya PT. Hypotension. In: StatPearls. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK499961/. Accessed August 28, 2022.
McClelland DB. ABC of transfusion. Human albumin solutions BMJ. 1990;300(6716):35–7.
Scholtz M. Hippocrates’ aphorisms Calif West Med. 1940;53(6):272.
Peters Jr, T. All about albumin: biochemistry, genetics, and medical applications. Academic Press; 1995.
Dekkers F. Exercitationes Practicae circa Medendi Methodum. Boutensteyn and Luchtmans; 1694.
Course of lectures on the physiology and pathology of the blood, and the other animal fluids. The Lancet. 1840;34(872):257–264.
Moman RN, Gupta N, Varacallo M. Physiology, albumin. In: StatPearls. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK459198/. Accessed September 11, 2022.
Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E. The antioxidant properties of serum albumin. FEBS Lett. 2008;582(13):1783–7.
Hahn RG. Colloid fluids. In: Hahn RG, editor. Clinical fluid therapy in the perioperative setting. 2nd ed. Cambridge University Press; 2016. p. 10–9.
Guyton A, Hall J. Textbook of medical physiology. 10th ed. Co: W.B. Saunders; 2000.
MI Griffel, Kaufman B. Pharmacology of colloids and crystalloids. Crit Care Clin. 8:235–254.
Khawar H, Kelley W, Stevens JB, Guzman N. Fresh frozen plasma (FFP). In: StatPearls. StatPearls Publishing; 2022. http://www.ncbi.nlm.nih.gov/books/NBK513347/. Accessed September 10, 2022.
Baron JF. Crystalloids or colloids for the treatment of hypovolemia? Transfus Altern Transfus Med. 1999;1(4):12–26.
Nearman HS, Herman ML. Toxic effects of colloids in the intensive care unit. Crit Care Clin. 1991;7(3):713–23.
Drumi W, Polzleitner D, Laggner A, et al. Dextran-40, acutre renal failure, and elevated plasma oncotic pressure. N Engl J Med. 1988;318:252–4.
Richter AW. Immune complex anaphylaxis induced by dextran and its elimination by hapten inhibition. In: Ring J, Burg G, editors. New trends in allergy II. Springer; 1986. p. 272–83.
de Jonge E, Levi M. Effects of different plasma substitutes on blood coagulation: a comparative review. Crit Care Med. 2001;29(6):1261–7.
Brunkkorst FM, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367(2):124–134.
Magder S, Potter BJ, DeVarennes B, Doucette S, Fergusson D. Fluids after cardiac surgery: a pilot study of the use of colloids versus crystalloids. Crit Care Med. 2010;38(11):2117–24.
Muller L, Lefrant JY. Metabolic effects of plasma expanders. Transfus Altern Transfus Med. 2010;11(s3):10–21.
Laxenaire MC, Charpentier C, Feldman L. Anaphylactoid reactions to colloid plasma substitutes: incidence, risk factors, mechanisms. A French multicenter prospective study. Ann Fr Anesth Réanimation. 1994;13(3):301–310.
Evans PA, Glenn JR, Heptinstall S, Madira W. Effects of gelatin-based resuscitation fluids on platelet aggregation. Br J Anaesth. 1998;81(2):198–202.
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063.
Rochwerg B, et al. Fluid resuscitation in sepsis: a systematic review and network meta-analysis. Ann Intern Med. 2014;161:347–55.
Tseng CH, Chen TT, Wu MY, Chan MC, Shih MC, Tu YK. Resuscitation fluid types in sepsis, surgical, and trauma patients: a systematic review and sequential network meta-analyses. Crit Care. 2020;24(1):693.
Martin GS, Bassett P. Crystalloids vs. colloids for fluid resuscitation in the intensive care unit: a systematic review and meta-analysis. J Crit Care. 2019;50:144–154.
Boyd JH, Forbes J, Nakada T, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39(2):259–65.
Matejtschuk P, Dash CH, Gascoigne EW. Production of human albumin solution: a continually developing colloid. Br J Anaesth. 2000;85(6):887–95.
• Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: systematic review of randomised controlled trials. BMJ. 1998;317(7153):235–240. Review of literature that suggested that albumin administration in critically ill patients was non-superior to other fluids and that albumin may confer increased morbidity and mortality.
McClelland B. Albumin: don’t confuse us with the facts. BMJ. 1998;317(7162):829–30.
Roberts I, Edwards P, McLelland B. Use of human albumin in the UK fell substantially when systematic review was published. BMJ. 1999;318(7192):1214.
Petros A, Schindler M, Pierce C, Jacobe S, Mok Q. Human albumin administration in critically ill patients. BMJ. 1998;317(7162):882.
Watts J. Fluid resuscitation with colloid or crystalloid solutions. BMJ. 1998;317(7153):277.
Fergal, D. Letter to doctors. Washington, DC: Food and Drug Administration, Center for Biologics Evaluation and Research https://scholar.google.com/scholar_lookup?title=Letter+to+doctors.&author=D+Fergal&publication_year=1998. Accessed 22 Sept 2022.
Horsey PJ. The Cochrane 1998 albumin review – not all it was cracked up to be. Eur J Anaesthesiol. 2002;19(10):701.
Wilkes MM, Navickis RJ. Patient survival after human albumin administration. Ann Intern Med. 2001;135(3):149–64.
•• The SAFE Study Investigators. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350(22):2247–2256. First major clinical trial that compared albumin vs saline for fluid resuscitation in ICU patients. Demonstrated no increased mortality with albumin, and even some improved outcomes compared to saline.
The SAFE Study Investigators. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84.
•• Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412–1421. Second major clinical trial that demonstrated benefit in giving albumin with crystalloid fluids in critically ill patients with severe sepsis and septic shock.
Vincent JL, De Backer D, Wiedermann CJ. Fluid management in sepsis: the potential beneficial effects of albumin. J Crit Care. 2016;35:161–7.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raynor, B., Huang, A., Udrea, D. et al. The Role of Albumin in the Resuscitation of Hypotensive Patients. Curr Emerg Hosp Med Rep 11, 89–94 (2023). https://doi.org/10.1007/s40138-023-00268-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-023-00268-1