Abstract
Purpose of Review
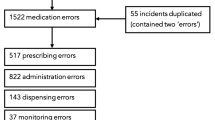
Computerized patient safety reporting systems are used to improve the safety of the medication use process. The objective of our analysis was to determine whether differences exist in the accuracy of reporter estimated incident severity level. This is a retrospective, quality assurance analysis of medication safety reports. Information collected included the total number of medication safety reports, reporter roles, reported severity level, and actual severity level. Accuracy of reporter severity was determined based on the difference between reported compared to the actual severity scored for each incident.
Recent Findings
Four hundred forty-nine were included in the analysis. Reports were most commonly entered by nurses (71.3%) followed by pharmacists (16.9%), physicians (7.6%), and physician extenders (nurse practitioners, physician assistants) (4.2%). The overall accuracy rate of severity level was 77.5%.
Summary
No difference was found between nurses, pharmacists, and physicians in regard to reporting accuracy.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016;353:i2139. This article summarizes the impact of medical errors on outcomes and discussses the importance of improving health care systems and reporting to better understand deaths due to medical care.
• Kennedy Sheldon L. 2016: creating a culture of safety in oncology. Clin J Oncol Nurs. 2016;20(2):115–6. This article discusses the role of nurses on patient safety and reporting systems.
Hwang JI, Ahn J. Teamwork and clinical error reporting among nurses in Korean hospitals. Asian Nurs Res. 2015;9(1):14–20.
Weant KA, Humphries RL, Hite K, Armitstead JA. Effect of emergency medicine pharmacists on medication-error reporting in an emergency department. American journal of health-system pharmacy : AJHP : official journal of the Am J Health Syst Pharm. 2010;67(21):1851–5.
Westbrook JI, Li L, Lehnbom EC, Baysari MT, Braithwaite J, Burke R, et al. What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. International journal for quality in health care : journal of the Int J Qual Health Care / ISQua. 2015;27(1):1–9.
• Patterson ME, Pace HA. A cross-sectional analysis investigating organizational factors that influence near-miss error reporting among hospital pharmacists. Journal of Patient Safety. 2016;12(2):114–7. This article describes the factors that may influence safety reporting and suggest that reporting on near- miss events are vastly underestimated.
Guchelaar HJ, Colen HB, Kalmeijer MD, Hudson PT, Teepe-Twiss IM. Medication errors: hospital pharmacist perspective. Drugs. 2005;65(13):1735–46.
Hohenstein C, Fleischmann T, Rupp P, Hempel D, Wilk S, Winning J. German critical incident reporting system database of prehospital emergency medicine: analysis of reported communication and medication errors between 2005-2015. World J Emerg Med. 2016;7(2):90–6.
Tuttle D, Holloway R, Baird T, Sheehan B, Skelton WK. Electronic reporting to improve patient safety. Qual Saf Health Care. 2004;13(4):281–6.
•• Pitkanen A, Teuho S, Uusitalo M, Kaunonen M. Improving medication safety based on reports in computerized patient safety systems. Comput Inform Nurs : CIN. 2016;34(3):122–7. This study summarizes and suggests methods in which to report and track medication safety events, and described the role technology has in safety reporting.
•• Wagner C, Merten H, Zwaan L, Lubberding S, Timmermans D, Smits M. Unit-based incident reporting and root cause analysis: variation at three hospital unit types. BMJ Open. 2016;6(6):e011277. This article describes the value and importance of unit based reporting systems, and the role of nalyzing medication errors based on specific services, as this may lead to different causes and solutions.
Abbasi T, Adornetto-Garcia D, Johnston PA, Segovia JH, Summers B. Accuracy of harm scores entered into an event reporting system. The J Nurs Adm. 2015;45(4):218–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pharmacology of Acute Care
Rights and permissions
About this article
Cite this article
Kovacevic, M.P., Schurr, J.W. & Dell’Orfano, H. Accuracy of Medication Safety Report Severity Level Among Disciplines at a Tertiary Academic Medical Center. Curr Emerg Hosp Med Rep 6, 116–119 (2018). https://doi.org/10.1007/s40138-018-0165-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-018-0165-6