Abstract
The use of ex vivo machine preservation/perfusion (MP) remains investigational in clinical liver transplantation. MP is a platform that provides continuous circulation of nutrients and metabolic substrates and oxygen during the ex vivo period. Over the last few years, several groups worldwide have been actively translating MP into the clinical arena for liver transplantation. Groups are investigating ex vivo MP at various temperatures and with various perfusates and devices. There have been several promising preliminary clinical series of liver hypothermic MP (HMP) published over the last 5 years. Normothermic MP (NMP) is currently undergoing clinical investigation in Europe with promising clinical reports. There has been excellent clinical experience with HMP in small series including those recovered from extended criteria donors and donation after cardiac death donors. While some variability exists in technique, all clinical HMP series to date have reported improved outcomes with reductions in early allograft dysfunction, biliary complications, and reduced hospital length of stay. These benefits, together with the development of innovative portable MP devices and further adoption by more centers worldwide, have “broken the ice” for more widespread use of HMP and subsequent expanded elucidation of the benefits of MP in liver transplantation. Optimal temperatures and protocols are still a topic of debate.

Similar content being viewed by others
Abbreviations
- DCD:
-
Donation after cardiac death
- ECD:
-
Extended criteria donor
- ECMO:
-
Extracorporeal membrane oxygenation
- HMP:
-
Hypothermic machine perfusion
- IRI:
-
Ischemia/reperfusion injury
- LOS:
-
Length of stay
- MP:
-
Machine perfusion
- NMP:
-
Normothermic machine perfusion
- ROS:
-
Reactive oxygen species
- SCS:
-
Static cold storage
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
http://optn.transplant.hrsa.gov/converge/latestData/rptData.asp;Pages.
https://www.eurotransplant.org/cms/index.php?page=annual_reports;Pages.
Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, Napieralski BP, et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 2009;360(1):7–19.
Steen S, Ingemansson R, Eriksson L, Pierre L, Algotsson L, Wierup P, et al. First human transplantation of a nonacceptable donor lung after reconditioning ex vivo. Ann Thorac Surg. 2007;83(6):2191–4.
Wierup P, Haraldsson A, Nilsson F, Pierre L, Schersten H, Silverborn M, et al. Ex vivo evaluation of nonacceptable donor lungs. Ann Thorac Surg. 2006;81(2):460–6.
Ravikumar R, Leuvenink H, Friend PJ. Normothermic liver preservation: a new paradigm? Transpl Int. 2015;28(6):690–9.
•• Guarrera JV, Henry SD, Samstein B, Reznik E, Musat C, Lukose TI, et al. Hypothermic machine preservation facilitates successful transplantation of “orphan” extended criteria donor livers. Am J Transpl. 2015;15(1):161–9. Largest clinical series to date employing HMP demonstrating the safe use and excellent outcomes in ECD livers that were rejected by multiple transplant centers.
Butler AJ, Rees MA, Wight DG, Casey ND, Alexander G, White DJ, et al. Successful extracorporeal porcine liver perfusion for 72 hr. Transplantation. 2002;73(8):1212–8.
Schon MR, Kollmar O, Wolf S, Schrem H, Matthes M, Akkoc N, et al. Liver transplantation after organ preservation with normothermic extracorporeal perfusion. Ann Surg. 2001;233(1):114–23.
St Peter SD, Imber CJ, Lopez I, Hughes D, Friend PJ. Extended preservation of non-heart-beating donor livers with normothermic machine perfusion. Br J Surg. 2002;89(5):609–16.
Reddy SP, Bhattacharjya S, Maniakin N, Greenwood J, Guerreiro D, Hughes D, et al. Preservation of porcine non-heart-beating donor livers by sequential cold storage and warm perfusion. Transplantation. 2004;77(9):1328–32.
Reddy S, Greenwood J, Maniakin N, Bhattacharjya S, Zilvetti M, Brockmann J, et al. Non-heart-beating donor porcine livers: the adverse effect of cooling. Liver Transpl. 2005;11(1):35–8.
Brockmann J, Reddy S, Coussios C, Pigott D, Guirriero D, Hughes D, et al. Normothermic perfusion: a new paradigm for organ preservation. Ann Surg. 2009;250(1):1–6.
Xu H, Berendsen T, Kim K, Soto-Gutierrez A, Bertheium F, Yarmush ML, et al. Excorporeal normothermic machine perfusion resuscitates pig DCD livers with extended warm ischemia. J Surg Res. 2012;173(2):e83–8.
•• Fondevila C, Hessheimer AJ, Maathuis MH, Munoz J, Taura P, Calatayud D, et al. Superior preservation of DCD livers with continuous normothermic perfusion. Ann Surg. 2011;254(6):1000–7. This study expands on a previous landmark study by the same group demonstrating the use of ECMO to maintain graft viability in unexpected DCD donors. They demonstrate the addition of NMP to ECMO as being further protective in grafts subject to extended warm ischemia.
Liu Q, Nassar A, Farias K, Buccini L, Baldwin W, Mangino M, et al. Sanguineous normothermic machine perfusion improves hemodynamics and biliary epithelial regeneration in donation after cardiac death porcine livers. Liver Transpl. 2014;20(8):987–99.
Banan B, Xiao Z, Watson R, Xu M, Jia J, Upadhya GA, et al. Novel strategy to decrease reperfusion injuries and improve function of cold preserved livers using normothermic ex-vivo liver perfusion machine. Liver Transpl. 2015;. doi:10.1002/lt.24352.
Fondevila C, Hessheimer AJ, Ruiz A, Calatayud D, Ferrer J, Charco R, et al. Liver transplant using donors after unexpected cardiac death: novel preservation protocol and acceptance criteria. Am J Transpl. 2007;7(7):1849–55.
• op den Dries S, Karimian N, Sutton ME, Westerkamp AC, Nijsten MW, Gouw AS, et al. Ex vivo normothermic machine perfusion and viability testing of discarded human donor livers. Am J Transpl. 2013;13(5):1327–35. The study demonstrated that NMP of human livers is feasible and demonstrated the protective effect in an ex-vivo model without transplantation.
•• Watson CJ, Kosmoliaptsis V, Randle LV, Russell NK, Griffiths WJ, Davies S, et al. Preimplant normothermic liver perfusion of a suboptimal liver donated after circulatory death. Am J Transpl. 2015. doi:10.1111/ajt.13448. First report of the use of NMP prior to transplant in a human. It reports survival and absence of cholangiopathy at 6 months post transplant from a donor subject to an arrest period of 150 mins.
Caldwell-Kenkel JC, Currin RT, Tanaka Y, Thurman RG, Lemasters JJ. Reperfusion injury to endothelial cells following cold ischemic storage of rat livers. Hepatology. 1989;10(3):292–9.
McKeown CM, Edwards V, Phillips MJ, Harvey PR, Petrunka CN, Strasberg SM. Sinusoidal lining cell damage: the critical injury in cold preservation of liver allografts in the rat. Transplantation. 1988;46(2):178–91.
• Bruinsma BG, Yeh H, Ozer S, Martins PN, Farmer A, Wu W, et al. Subnormothermic machine perfusion for ex vivo preservation and recovery of the human liver for transplantation. Am J Transpl. 2014;14(6):1400–9. This study demonstrated the feasibility of subnormothermic machine perfusion and the ability of the technology to support discarded grafts while maintaining their metabolic activity. The group hypothesize that an intermediate perfusate temperature prevents rapid rewarming at the same time maintaining some metabolic activity in the graft.
van Golen RF, van Gulik TM, Heger M. Mechanistic overview of reactive species-induced degradation of the endothelial glycocalyx during hepatic ischemia/reperfusion injury. Free Radic Biol Med. 2012;52(8):1382–402.
Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischaemia-reperfusion injury in liver transplantation: from bench to bedside. Nat Rev Gastroenterol Hepatol. 2013;10(2):79–89.
Land WG. Emerging role of innate immunity in organ transplantation part II: potential of damage-associated molecular patterns to generate immunostimulatory dendritic cells. Transpl Rev (Orlando). 2012;26(2):73–87.
• Tulipan JE, Stone J, Samstein B, Kato T, Emond JC, Henry SD, et al. Molecular expression of acute phase mediators is attenuated by machine preservation in human liver transplantation: preliminary analysis of effluent, serum, and liver biopsies. Surgery. 2011;150(2):352–60. By measuring levels of key mediators of inflammation in IRI this study demonstrated the molecular mechanisms of the protective effect of HMP.
Guarrera JV, Henry SD, Chen SW, Brown T, Nachber E, Arrington B, et al. Hypothermic machine preservation attenuates ischemia/reperfusion markers after liver transplantation: preliminary results. J Surg Res. 2011;167(2):e365–73.
•• Henry SD, Nachber E, Tulipan J, Stone J, Bae C, Reznik L, et al. Hypothermic machine preservation reduces molecular markers of ischemia/reperfusion injury in human liver transplantation. Am J Transpl. 2012;12(9):2477–86. The study demonstrates reduction in IRI in HMP treated grafts by showing lower levels of pro-inflammatory cytokines thereby providing a molecular explanation of reduced preservation injury seen with HMP.
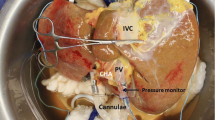
•• Guarrera JV, Henry SD, Samstein B, Odeh-Ramadan R, Kinkhabwala M, Goldstein MJ, et al. Hypothermic machine preservation in human liver transplantation: the first clinical series. Am J Transpl. 2010;10(2):372–81. Landmark study reporting the first use of machine perfusion in human liver transplantation. Human liver transplantation performed after HMP was compared with cold storage showing lower injury markers and shorter hospital stay in the perfused group. The study also demonstrated the safety and efficacy of the approach.
•• Dutkowski P, Schlegel A, de Oliveira M, Mullhaupt B, Neff F, Clavien PA. HOPE for human liver grafts obtained from donors after cardiac death. J Hepatol. 2014;60(4):765–72. First report of use of HMP in human DCD liver grafts suggesting a protective effect against reperfusion injury and ischemic cholangiopathy.
• Schlegel A, Rougemont O, Graf R, Clavien PA, Dutkowski P. Protective mechanisms of end-ischemic cold machine perfusion in DCD liver grafts. J Hepatol. 2013;58(2):278–86. The study elucidates the protective mechanisms underlying HMP using a reperfusion pig liver model. The report concluded that an hour of oxygenated perfusion with lower pressures at the end of ischemic period exerted maximum benefit.
Maluf DG, Stravitz RT, Cotterell AH, Posner MP, Nakatsuka M, Sterling RK, et al. Adult living donor versus deceased donor liver transplantation: a 6-year single center experience. Am J Transpl. 2005;5(1):149–56.
Pine JK, Aldouri A, Young AL, Davies MH, Attia M, Toogood GJ, et al. Liver transplantation following donation after cardiac death: an analysis using matched pairs. Liver Transpl. 2009;15(9):1072–82.
Brunner SM, Junger H, Ruemmele P, Schnitzbauer AA, Doenecke A, Kirchner GI, et al. Bile duct damage after cold storage of deceased donor livers predicts biliary complications after liver transplantation. J Hepatol. 2013;58(6):1133–9.
• op den Dries S, Sutton ME, Karimian N, de Boer MT, Wiersema-Buist J, Gouw AS, et al. Hypothermic oxygenated machine perfusion prevents arteriolonecrosis of the peribiliary plexus in pig livers donated after circulatory death. PLoS One. 2014;9(2):e88521. This study demonstrated the protective of HMP on biliary microvasculature. In a DCD pig liver model, histology of bile ducts after reperfusion were compared between the perfused and statically stored livers.
Jochmans I, Moers C, Smits JM, Leuvenink HG, Treckmann J, Paul A, et al. The prognostic value of renal resistance during hypothermic machine perfusion of deceased donor kidneys. Am J Transpl. 2011;11(10):2214–20.
Busuttil RW, Lipshutz GS, Kupiec-Weglinski JW, Ponthieux S, Gjertson DW, Cheadle C, et al. rPSGL-Ig for improvement of early liver allograft function: a double-blind, placebo-controlled, single-center phase II study. Am J Transpl. 2011;11(4):786–97.
Dulkanchainun TS, Goss JA, Imagawa DK, Shaw GD, Anselmo DM, Kaldas F, et al. Reduction of hepatic ischemia/reperfusion injury by a soluble P-selectin glycoprotein ligand-1. Ann Surg. 1998;227(6):832–40.
Nativ NI, Maguire TJ, Yarmush G, Brasaemle DL, Henry SD, Guarrera JV, et al. Liver defatting: an alternative approach to enable steatotic liver transplantation. Am J Transpl. 2012;12(12):3176–83.
Nagrath D, Xu H, Tanimura Y, Zuo R, Berthiaume F, Avila M, et al. Metabolic preconditioning of donor organs: defatting fatty livers by normothermic perfusion ex vivo. Metab Eng. 2009;11(4–5):274–83.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Solid Organ Transplantation.
Rights and permissions
About this article
Cite this article
Klair, T.S., Guarrera, J.V. Machine Perfusion and Innovations in Liver Transplant Preservation. Curr Surg Rep 4, 2 (2016). https://doi.org/10.1007/s40137-015-0125-y
Published:
DOI: https://doi.org/10.1007/s40137-015-0125-y