Abstract
Purpose of the Review
In this narrative review, we focus on the latest updates on CA–AS diagnosis, the implementation of CMR, and CT in the diagnostic algorithm and their future prospectives.
Recent Findings
Aortic stenosis (AS) is the most common valvular heart disease (VHD) worldwide. In recent years, the association between Cardiac amyloidosis (CA) and AS has emerged as a not uncommon and sneaky association. Trans-thyretin (TTR) and immunoglobulin light chain (AL) are the two most common different types of misfolded amyloid proteins infiltrating the heart. AS–CA shares some anatomical features with CA, but the association leads to worse outcome. Nearly 30% of patients undergoing TAVR suffers from CA. Differentiating CA–AS from lone AS is of great importance to tailorize pharmaceutical therapy and/or surgery. Nowadays, bone scintigraphy and urine/serum analyses are crucial to assess which type of amyloid excess there is, but to represent anatomical changes of the myocardium cardiac magnetic resonance (CMR) and computed tomography cardiac angiography (CTCA), they are the best non-invasive tools. Moreover, extracellular expansion can be quantified via CMR, but new promising studies assessing extracellular volume (ECV) via CT are emerging. Furthermore, AS–CA is a sneaky pathology afflicting elderly patients. Seen the comorbidities of the typical patient, Transcatheter Aortic Valve Replacement (TAVR) should be the indicated procedure. CT is the best imaging modality for TAVR planning with its excellent anatomical resolution.
Summary
CMR and CT could be integrated in the CA algorithm. Both can assess myocardium anatomical changes. Moreover, ECV is a precious tool to suggest the presence of amyloid in the myocardium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aortic Stenosis (AS) is the most prevalent valvular heart disease (VHD). It is characterized by a reduction of the area of the aortic valve which leads to overload, hypertension and left ventricle (LV) concentric hypertrophy, reduction of LV, and diastolic and systolic function and, eventually, heart failure.
In recent years, the association between cardiac amyloidosis (CA) and AS has emerged as a frequent and sneaky condition [1]. There are different types of amyloidosis, depending on the type of misfolded protein—being immunoglobulin light chain (AL) and trans-thyretin (TTR) the most common ones—and the system involved (e.g., cardiovascular, nervous, hematopoietic).
TTR-amyloidosis is more prone to cardiac involvement, where misfolded amyloid fibrils deposit in the ECV of the myocardium and the other heart structures. Cardiac Amyloidosis can be present in up to 25% of the over 80-year-old patients [2], and it is even more present in patients undergoing TAVR with a prevalence of nearly 33% [3]. When combined, Cardiac amyloidosis and Aortic stenosis (CA–AS) have worse prognosis than AS alone [4]. However, Riley et al. demonstrated how risk of all-cause mortality was significantly lower in patients who underwent TAVR than those treated with conservative medical therapy alone [5].
AL–CA usually follows hemopoietic disorders such as myeloma. Plasma cells produce an excessive amount of monoclonal immunoglobulin light chains, which by misfolding themselves, can aggregate into amyloid fibrils and can deposit in the myocardium [6]. Moreover, light chains elevate natriuretic peptide production, thus, rendering AL–CA a “toxic and infiltrative” cardiomyopathy [7].
CA afflicts different cardiac structures, ranging from myocardium to the valves. Amyloid firstly accumulates from the base of the myocardium to the apex, leading to a concentric hypertrophy. Atria are also afflicted, and this explains the frequent association with atrial fibrillation. It is yet to be cleared what type of causation, there is between aortic valve infiltration and the stenosing process [8, 9••]. As proposed by Bonelli et al., probably the infiltration of amyloid within the myocardium leads to endothelium damage and consequently fibrosis and calcifications [9••].
CA–AS presents some overlaps in terms of morphologic cardiac alterations with AS; thus, it can be hard to distinguish between the two. Concentric hypertrophy, LV disfunction, and progressive impairment of the systolic function can be found in both, but CA–AS tends to be worse in each of these aspect [10, 11]. In addition, elderly patients present comorbidities such as coronary artery disease (CAD) and hypertension, making the diagnosis more challenging [3].
There is no pathognomonic aspect for CA–AS. Electrocardiogram and echo-cardiography can be valuable, but their sensitivity is feeble. In clinical practice, RAISE (Remodeling, Age, Injury, Systemic involvement, and Electric abnormalities) multiparametric score has been proposed to distinguish lone AS from CA–AS. Such score comprehends the following criteria: the presence of carpal tunnel, disproportionate electrical remodeling, disproportionate myocardial remodeling, chronic myocardial injury, and age. The presence of one of the parameters adds different points. A score equal or higher than six has a 100% specifity [10].
In this review, we will focus on the role of cardiac magnetic resonance (CMR) and computed tomography (CT) in the identification of the patients affected by AS and CA.
Cardiac Magnetic Resonance
Why CMR
CMR is a non-ionizing imaging modality that represents the gold standard in assessing volumes, mass, and kinetic of the myocardium. It is the current reference standard for the evaluation of left and right ventricle ejection fraction, for the relative stroke volume and to picture valve changes [12]. Moreover, it has the unique ability to characterize myocardial tissue through the late gadolinium enhancement (LGE) sequences and the parametric techniques of T1 and T2 mapping.
Cardiac CMR can identify patients with CA, with a specificity of 92% and sensitivity of 85% [13]. CMR can also monitors response to CA’s therapy [14].
Through steady-state-free-precession cine sequences, CMR can easily detect and measure the typical changes of the AS-affected myocardium, such as left ventricular myocardial mass thickening, atrial dilatation, LV diastolic and systolic dysfunction.
However, these changes are not exclusive of AS, as patients with CA can also present these morpho-functional changes. Therefore it is necessary to pay particular attention to suspicious criteria for CA–AS, the so-called “red flags”: discordance between low-voltage and LV wall thickness, disproportionate LV wall thickening (> 15 mm) relative to AS severity, LV global longitudinal strain ≥ 12%, apex/basal longitudinal strain ratio > 2, right ventricle (RV) wall thickening (> 5 mm), predominant right ventricular heart failure with ascites, atrial septal thickening and biatrial dilatation, and the presence of pericardial effusion [15].
Moreover, cardiac tissue abnormalities, consequential to amyloid substances deposits, can be identified with late gadolinium enhancement (LGE), native myocardial T1 mapping, myocardial extracellular space volume calculations, myocardial-blood inversion time rate analysis, and myocardial edema investigation.
Normal myocardial T1 values are usually between 950 and 1050 ms. T1 values are prolonged in patients with isolated CA or AS and AS–CA [16•].
Moreover, tissue characterization with T1 mapping allows not only the assessment of cardiac involvement in cases of CA but has also proven to be a good marker to discover early stages of the disease [17] and for monitoring the response of the treatment [18].
Tavoosi et al. showed that an abnormal nulling pattern on Look Locker Inversion Time in post-contrast T1 mapping is highly suggestive of CA [19]. The abnormal nulling pattern could be related in these subjects to the amplification of ECV of the body leading to a faster clearance of gadolinium.
CA usually has basal–apical distribution of late enhancement while apical segments are frequently spared. LGE occurs in up to 40% of isolated AS cases, being present primarily in the LV with a focal mesocardiac pattern but with possible involvement of the right ventricle and atrial myocardium [20]. Different LGE patterns correlate with different etiologies. TTR-CA follows a basal–apical enhancement distribution where apex can be spared and a higher presence of RV involvement. On the contrary, AL–CA has a circumferential subendocardial involvement that can extend to transmural pattern (Fig. 1) [21].
The presence of distribution of LGE can be used to possibly exclude other cardiovascular diseases such as hypertrophic cardiomyopathy, Fabry disease, and cardiac hemochromatosis [1].
Furthermore, the presence of LGE was correlated to an increased relative risk of major cardiovascular events and residual left ventricular dysfunction after aortic valve replacement [22].
Cardiac magnetic resonance ECV (ECVCMR) analysis is based on native myocardial T1 time and on post-contrast T1 time and on the hematocrit value assessed through blood sample. The ECV is calculated according to the following formula:
Normally, ECV value ranges are < 25–27%. In CA–AS, it is increased (Fig. 2) [23].
In amyloidosis, T1 relaxation time values are typically increased as a result of the extracellular deposition of the amyloid protein. The T1 mapping (A) displays on a color scale the T1 values of the myocard, blood, and surrounding structures. On the polar map, (B) a diffuse increase of the T1 values is reported (in this case normal values < 1250 ms on a 3 T CMR). The resulting ECV values (normal values < 30%) are consequently also increased (C, D)
ECV has excellent prognostic value in patients with CA–AS since it is correlated with mortality. An ECV < 25% is a protective factor regardless of exclusive clinical treatment or valve replacement, with no reports of cardiovascular death within 1 year [24].
When CMR
Nitsche et al. in 2021 demonstrated that CA-associated AS is more common in older patients, especially males, and can be predicted clinically evaluating the presence of history of carpal tunnel syndrome, LV remodeling and increased septal thickness, RBBB, low Sokolow voltage, increased E/A ratio, and elevated troponin levels. [10]
Ecocardiography is the first imaging tool to assess CA–AS but has limited sensitivity and specificity to identify both conditions simultaneously [20].
The 2021 ESC guidelines on the management of VHD give no specific indication for when to perform cardiac MRI in suspected CA-associated AS, but CMR is increasingly emerging as the technique of choice when echocardiographic findings are not diriment [25].
CMR represents a unique tool for the diagnosis and the monitoring of therapeutic response and prognostication in patients with aortic stenosis and cardiac amyloidosis.
However, data obtained by CMR should always be integrated with clinical, laboratory, and imaging data to obtain a more accurate diagnosis.
If imaging assessment with CMR raises suspicion of CA–AS, further investigations are necessary to confirm the diagnostic assumption. Bone scintigraphy with 99 m technetium-labeled bisphosphonates in association with research for monoclonal light chain in blood and urine is able to discriminate TTR-CA and AL–CA with high sensitivity and specificity. TTR-CA is diagnosed by the presence of cardiac uptake and absence of monoclonal protein in serum/urine analysis [26].
Computed Tomography
Why CT
Nowadays, Computed Tomography Cardiac Angiography (CTCA) is a widely diffused and available imagine technique. Even if CMR remains the gold standard, some cardiac changes due to CA–AS can be visualized, such as RV and LV hypertrophy, atria calcifications, and chamber dilatation. Furthermore, CTCA has the capability to exclude the presence of coronary artery disease and to enable the evaluation of LV volumes and function when an ECG-gated scan encompassing the entire cardiac cycle is performed.
Moreover, CTCA is the pivotal examination for the transcatheter aortic valve replacement (TAVR) planning. In a single, contrast-enhanced acquisition, CTCA offers a valid overview of the aorta, the iliac arteries, and the femoral arteries [27]. Moreover, it allows to depict anatomy of the aortic annulus (AoA), aortic root, and the height of coronary ostia providing crucial information for the interventional cardiologist [28].
Usually, TAVR-planning scan acquisition comprehends 2 acquisitions: one unenhanced CT and one after contrast media injection. However, in the last few years, new studies suggested how CTCA could be used for ECV measurement [29•] in order to identify patients with CA.
In the setting of TAVR planning, CTCA can be employed as a method to screen the presence of CA–AS measuring ECV. This is readily obtainable through three different acquisitions: an unenhanced CT, a retrospective, contrast-enhanced acquisition of the heart plus a whole body acquisition (to assess the thoraco-abdominal vessels), and a 3-min acquisition for measuring ECV (ECVCT) [29•].
Two methods can be used for calculating the myocardial ECV fraction: one requires blood sampling to determine the serum hematocrit; the other, called synthetic ECV, is derived by using unenhanced attenuation of blood.
In the first case, ECVCT relies upon the same principle as ECVCMR and is calculated using the following formula:
where ΔHU is the change in Hounsfield unit attenuation pre- and post-contrast (e.g., HUpost-contrast − HUpre-contrast).
In the second case, synthetic ECV is based on synthetic blood hematocrit (Hct) whose value derives from blood attenuation on unenhanced CT:
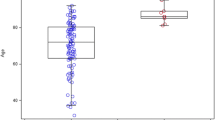
Treibel et al. demonstrated how synthetic ECV is a good surrogate for laboratory-derived ECV in the assessment of myocardial fibrosis or infiltration (Fig. 3) [30].
ECV with CT is measured through two acquisitions: an unenhanced scan and a post-contrast acquisition at 5–7 min from injection. Measurement of the HU values from the ROIs placed at the interventricular septum in unenhanced (A) and enhanced (B) CT. Unenhanced ROI value: 29 ± 29 HU; Post-contrast ROI value: 92 ± 12 HU
CT and CMR are both valid tools to estimate myocardial ECV, without the need for invasive endomyocardial biopsy. Indeed, it is possible to measure ECV by means of CT contrast agents to visualize diffuse myocardial fibrosis, tissue amyloid accumulation, or edema [29•]. While CMR is considered the non-invasive gold standard for ECV measurement, the evidence based on ECV quantification via CT is growing rapidly. Han et al. showed how ECVCT has an excellent correlation with ECVCMR [31]. Seen this, ECVCT still requires a tailored protocol with at least three acquisitions, it is not being implemented in diagnostic routine and it remains to this day in the realm of research.
As ECV is a marker of myocardial tissue remodeling, it could be useful as prognostic tool for patients who have undergone transcatheter or surgical aortic valve replacement. Suzuki et al. demonstrated how myocardial ECVCT in patients who underwent aortic valve intervention was an independent predictor of adverse outcomes after aortic valve replacement [32].
When CT
Between the non-invasive imaging technique, CTCA surely has the greatest special resolution. It offers a great description for every anatomical change that afflicts the CA–AS myocardium. It is also pivotal for vessels visualization before TAVR. To this day, the only usefulness of CTCA remains TAVR planning. Coronary artery visualization is a controversial topic as elderly patients tend to have diffuse-calcified coronaries, thus, increasing the blooming effect and reducing the diagnostic power of the machine. Further studies should concentrate on the correct framing of CTCA in the CA–AS diagnostic algorithm.
CTCA can also measure ECV. Hence, CTCA could become an alternative technique to CMR in patients undergoing TAVR to identify a concomitant CA and AS.
In particular, Scully et al. demonstrated how an ECVCT > 31% is linked to AS-amyloid. Hence, they proposed a diagnostic algorithm that orbits around CTCA. After TAVR-planning CTCA, if ECV is > 31% patient should be referred to further investigations (e.g., bone scintigraphy, urine and serum immunofixation, and serum-free light chains) [29•].
It is important to consider the higher ionizing radiation exposure associated with obtaining ECV measurements using CT, which involves multiple scans. However, the use of ECV CT could be considered primarily for elderly patients aged 80 and above, in which their potential radiation impact is minimal.
Conclusions
The real prevalence of CA in patients with SA is unknown to date, but considering the aging of the general population, we are facing a condition that we currently underestimate and may become even more prominent in the future.
The association between the two diseases severely worsens the patient's prognosis, and there is a need to facilitate the diagnostic and treatment pathways [33].
In addition, new therapies for amyloidosis are emerging and this could lead to changes in the therapeutic strategy in case of association between CA and AS [34].
Although CMR may not be an imaging modality that can be applied to all patients with AS due to the high incidence of the disease, costs, and availability in different hospital centers it represents to date the best tool to identify and evaluate the concomitant presence of CA.
CTCA remains crucial for TAVR planning and CAD assessment and could become a screening method for CA in these subsets of patients through the use of ECVCT. Indeed, ECVCT showed remarkable concordance with ECVCMR at the price of an additional ionizing acquisition. To this day, ECVCT is used only in the research field, but further studies and the incoming new low-dose scanners will help the transition to clinical practice.
Abbreviations
- AL:
-
Immuglobulin light chain
- AS:
-
Aortic Stenosis
- CA:
-
Cardiac amiloydosis
- CAD:
-
Coronary artery disease
- CMR:
-
Cardiac magnetic resonance
- CTCA:
-
Computed tomography cardiac angiography
- CT:
-
Computed tomography
- ECV:
-
Extracellular volume
- ECVCMR :
-
ECV assessed through CMR
- ECVCT :
-
ECV assessed through CT
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- TTR:
-
Trans-thyretin
- VHD:
-
Valvular heart disease
References
Papers of particular interest, published recently have been highlighted as: • Of importance •• Of major importance
Cavalcante JL, Rijal S, Abdelkarim I, Althouse AD, Sharbaugh MS, Fridman Y, Soman P, Forman DE, Schindler JT, Gleason TG, Lee JS, Schelbert EB. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2017;19:98. https://doi.org/10.1186/s12968-017-0415-x.
Tanskanen M, Peuralinna T, Polvikoski T, Notkola I-L, Sulkava R, Hardy J, Singleton A, Kiuru-Enari S, Paetau A, Tienari PJ, Myllykangas L. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med. 2008;40:232–9. https://doi.org/10.1080/07853890701842988.
Balciunaite G, Rimkus A, Zurauskas E, Zaremba T, Palionis D, Valeviciene N, Aidietis A, Serpytis P, Rucinskas K, Sogaard P, Glaveckaite S, Zorinas A, Janusauskas V. Transthyretin cardiac amyloidosis in aortic stenosis: prevalence, diagnostic challenges, and clinical implications. Hell J Cardiol HJC Hell Kardiologike Epitheorese. 2020;61:92–8. https://doi.org/10.1016/j.hjc.2019.10.004.
d’Humières T, Fard D, Damy T, Roubille F, Galat A, Doan H-L, Oliver L, Dubois-Randé J-L, Squara P, Lim P, Ternacle J. Outcome of patients with cardiac amyloidosis admitted to an intensive care unit for acute heart failure. Arch Cardiovasc Dis. 2018;111:582–90. https://doi.org/10.1016/j.acvd.2018.03.004.
Bauernschmitt R, Schreiber C, Bleiziffer S, Ruge H, Mazzitelli D, Hutter A, Tassani P, Lange R. Transcatheter aortic valve implantation through the ascending aorta: an alternative option for no-access patients. Heart Surg Forum. 2009;12:E63-64. https://doi.org/10.1532/HSF98.20081112.
Rubin J, Maurer MS. Cardiac amyloidosis: overlooked, underappreciated, and treatable. Annu Rev Med. 2020;71:203–19. https://doi.org/10.1146/annurev-med-052918-020140.
Brenner DA, Jain M, Pimentel DR, Wang B, Connors LH, Skinner M, Apstein CS, Liao R. Human amyloidogenic light chains directly impair cardiomyocyte function through an increase in cellular oxidant stress. Circ Res. 2004;94:1008–10. https://doi.org/10.1161/01.RES.0000126569.75419.74.
Audet A, Côté N, Couture C, Bossé Y, Després J-P, Pibarot P, Mathieu P. Amyloid substance within stenotic aortic valves promotes mineralization. Histopathology. 2012;61:610–9. https://doi.org/10.1111/j.1365-2559.2012.04265.x.
••Bonelli A, Paris S, Nardi M, Henein MY, Agricola E, Troise G, Faggiano P. Aortic valve stenosis and cardiac amyloidosis: a misleading association. J Clin Med. 2021;10:4234. https://doi.org/10.3390/jcm10184234. Bonelli et al. was a good quality paper to understand the CA-AS diagnostic and therapeutic algorithm and the new perspectives for CMR and CTCA.
Nitsche C, Scully PR, Patel KP, Kammerlander AA, Koschutnik M, Dona C, Wollenweber T, Ahmed N, Thornton GD, Kelion AD, Sabharwal N, Newton JD, Ozkor M, Kennon S, Mullen M, Lloyd G, Fontana M, Hawkins PN, Pugliese F, Menezes LJ, Moon JC, Mascherbauer J, Treibel TA. Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J Am Coll Cardiol. 2021;77:128–39. https://doi.org/10.1016/j.jacc.2020.11.006.
Rosenblum H, Masri A, Narotsky DL, Goldsmith J, Hamid N, Hahn RT, Kodali S, Vahl T, Nazif T, Khalique OK, Bokhari S, Soman P, Cavalcante JL, Maurer MS, Castaño A. Unveiling outcomes in coexisting severe aortic stenosis and transthyretin cardiac amyloidosis. Eur J Heart Fail. 2021;23:250–8. https://doi.org/10.1002/ejhf.1974.
Costantini P, Perone F, Siani A, Groenhoff L, Muscogiuri G, Sironi S, Marra P, Carriero S, Pavon AG, Guglielmo M. Multimodality imaging of the neglected valve: role of echocardiography, cardiac magnetic resonance and cardiac computed tomography in pulmonary stenosis and regurgitation. J Imaging. 2022. https://doi.org/10.3390/jimaging8100278.
Kupfahl C, Honold M, Meinhardt G, Vogelsberg H, Wagner A, Mahrholdt H, Sechtem U. Evaluation of aortic stenosis by cardiovascular magnetic resonance imaging: comparison with established routine clinical techniques. Heart Br Card Soc. 2004;90:893–901. https://doi.org/10.1136/hrt.2003.022376.
Martinez-Naharro A, Patel R, Kotecha T, Karia N, Ioannou A, Petrie A, Chacko LA, Razvi Y, Ravichandran S, Brown J, Law S, Quarta C, Mahmood S, Wisniowski B, Pica S, Sachchithanantham S, Lachmann HJ, Moon JC, Knight DS, Whelan C, Venneri L, Xue H, Kellman P, Gillmore JD, Hawkins PN, Wechalekar AD, Fontana M. Cardiovascular magnetic resonance in light-chain amyloidosis to guide treatment. Eur Heart J. 2022;43:4722–35. https://doi.org/10.1093/eurheartj/ehac363.
Ternacle J, Krapf L, Mohty D, Magne J, Nguyen A, Galat A, Gallet R, Teiger E, Côté N, Clavel M-A, Tournoux F, Pibarot P, Damy T. Aortic stenosis and cardiac amyloidosis: JACC review topic of the week. J Am Coll Cardiol. 2019;74:2638–51. https://doi.org/10.1016/j.jacc.2019.09.056.
•Balciunaite G, Rimkus A, Zurauskas E, Zaremba T, Palionis D, Valeviciene N, Aidietis A, Serpytis P, Rucinskas K, Sogaard P, Glaveckaite S, Zorinas A, Janusauskas V. Transthyretin cardiac amyloidosis in aortic stenosis: prevalence, diagnostic challenges, and clinical implications. Hellenic J Cardiol. 2020;61:92–8. https://doi.org/10.1016/j.hjc.2019.10.004. Balciunaite et al. was useful for the introduction of the paper.
Fontana M, Banypersad SM, Treibel TA, Maestrini V, Sado DM, White SK, Pica S, Castelletti S, Piechnik SK, Robson MD, Gilbertson JA, Rowczenio D, Hutt DF, Lachmann HJ, Wechalekar AD, Whelan CJ, Gillmore JD, Hawkins PN, Moon JC. Native T1 mapping in transthyretin amyloidosis. JACC Cardiovasc Imaging. 2014;7:157–65. https://doi.org/10.1016/j.jcmg.2013.10.008.
Izumiya Y, Takashio S, Oda S, Yamashita Y, Tsujita K. Recent advances in diagnosis and treatment of cardiac amyloidosis. J Cardiol. 2018;71:135–43. https://doi.org/10.1016/j.jjcc.2017.10.003.
Tavoosi A, Yu B, Aghel N, Karur GR, Pakkal M, Wald R, Wintersperger BJ, Delgado DH, Hanneman K. Diagnostic performance of abnormal nulling on cardiac magnetic resonance imaging look locker inversion time sequence in differentiating cardiac amyloidosis types. J Thorac Imaging. 2020;35:334–9. https://doi.org/10.1097/RTI.0000000000000493.
Barbosa PME, Magalhães TA. The role of cardiac magnetic resonance in patients with amyloidosis and aortic stenosis. Arq Bras Cardiol Imagem Cardiovasc. 2022. https://doi.org/10.47593/2675-312X/20223503eabc320i.
Dungu JN, Valencia O, Pinney JH, Gibbs SDJ, Rowczenio D, Gilbertson JA, Lachmann HJ, Wechalekar A, Gillmore JD, Whelan CJ, Hawkins PN, Anderson LJ. CMR-based differentiation of AL and ATTR cardiac amyloidosis. JACC Cardiovasc Imaging. 2014;7:133–42. https://doi.org/10.1016/j.jcmg.2013.08.015.
Bohbot Y, Renard C, Manrique A, Levy F, Maréchaux S, Gerber BL, Tribouilloy C. Usefulness of cardiac magnetic resonance imaging in aortic stenosis. Circ Cardiovasc Imaging. 2020;13:e010356. https://doi.org/10.1161/CIRCIMAGING.119.010356.
Sado DM, Flett AS, Banypersad SM, White SK, Maestrini V, Quarta G, Lachmann RH, Murphy E, Mehta A, Hughes DA, McKenna WJ, Taylor AM, Hausenloy DJ, Hawkins PN, Elliott PM, Moon JC. Cardiovascular magnetic resonance measurement of myocardial extracellular volume in health and disease. Heart Br Card Soc. 2012;98:1436–41. https://doi.org/10.1136/heartjnl-2012-302346.
Cavalcante JL, Rijal S, Abdelkarim I, Althouse AD, Sharbaugh MS, Fridman Y, Soman P, Forman DE, Schindler JT, Gleason TG, Lee JS, Schelbert EB. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis. J Cardiovasc Magn Reson. 2017;19:98. https://doi.org/10.1186/s12968-017-0415-x.
Vahanian A, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, Bonis MD, Paulis RD, Delgado V, Freemantle N, Haugaa K, Jeppsson A, Jüni P, Pierard L, Prendergast B, Sádaba J, Tribouilloy C, Wojakowski W, Beyersdorf F. ESC/EACTS guidelines for the management of valvular heart disease. EuroIntervention. 2021. https://doi.org/10.4244/EIJ-E-21-00009.
Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A, Wechalekar AD, Berk JL, Quarta CC, Grogan M, Lachmann HJ, Bokhari S, Castano A, Dorbala S, Johnson GB, Glaudemans AWJM, Rezk T, Fontana M, Palladini G, Milani P, Guidalotti PL, Flatman K, Lane T, Vonberg FW, Whelan CJ, Moon JC, Ruberg FL, Miller EJ, Hutt DF, Hazenberg BP, Rapezzi C, Hawkins PN. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133:2404–12. https://doi.org/10.1161/CIRCULATIONAHA.116.021612.
Marano R, Pontone G, Agricola E, Alushi B, Bartorelli A, Cameli M, Carrabba N, Esposito A, Faletti R, Francone M, Galea N, Golino P, Guglielmo M, Palmisano A, Petronio S, Petullà M, Pradella S, Ribichini F, Romeo F, Russo V, Scandura S, Schicchi N, Spaccarotella C, Tomai F, Indolfi C, Centonze M. Recommendations in pre-procedural imaging assessment for TAVI intervention: SIC-SIRM position paper part 2 (CT and MR angiography, standard medical reporting, future perspectives). Radiol Med (Torino). 2022;127:277–93. https://doi.org/10.1007/s11547-021-01434-9.
Guglielmo M, Fusini L, Muratori M, Tamborini G, Mantegazza V, Andreini D, Annoni A, Babbaro M, Baggiano A, Conte E, Carriero S, Formenti A, Guaricci AI, Mancini E, Mollace R, Muscogiuri G, Mushtaq S, Ricci F, Rossi A, Scafuri S, Alushi B, Cau C, Cau R, Cesarano M, Saba L, Rabbat M, Pepi M, Pontone G. Computed tomography predictors of structural valve degeneration in patients undergoing transcatheter aortic valve implantation with balloon-expandable prostheses. Eur Radiol. 2022;32:6017–27. https://doi.org/10.1007/s00330-022-08747-x.
•Scully PR, Patel KP, Saberwal B, Klotz E, Augusto JB, Thornton GD, Hughes RK, Manisty C, Lloyd G, Newton JD, Sabharwal N, Kelion A, Kennon S, Ozkor M, Mullen M, Hartman N, Cavalcante JL, Menezes LJ, Hawkins PN, Treibel TA, Moon JC, Pugliese F. Identifying cardiac amyloid in aortic stenosis: ECV quantification by CT in TAVR patients. JACC Cardiovasc Imaging. 2020;13:2177–89. https://doi.org/10.1016/j.jcmg.2020.05.029. Scully et al. present a proper study about ECV via CT, a new topic in cardiac imaging.
Treibel TA, Fontana M, Steeden JA, Nasis A, Yeung J, White SK, Sivarajan S, Punwani S, Pugliese F, Taylor SA, Moon JC, Bandula S. Automatic quantification of the myocardial extracellular volume by cardiac computed tomography: synthetic ECV by CCT. J Cardiovasc Comput Tomogr. 2017;11:221–6. https://doi.org/10.1016/j.jcct.2017.02.006.
Han D, Lin A, Kuronuma K, Gransar H, Dey D, Friedman JD, Berman DS, Tamarappoo BK. Cardiac computed tomography for quantification of myocardial extracellular volume fraction: a systematic review and meta-analysis. JACC Cardiovasc Imaging. 2023. https://doi.org/10.1016/j.jcmg.2023.03.021.
Suzuki M, Toba T, Izawa Y, Fujita H, Miwa K, Takahashi Y, Toh H, Kawamori H, Otake H, Tanaka H, Fujiwara S, Watanabe Y, Kono AK, Okada K, Hirata K-I. Prognostic impact of myocardial extracellular volume fraction assessment using dual-energy computed tomography in patients treated with aortic valve replacement for severe aortic stenosis. J Am Heart Assoc. 2021;10:e020655. https://doi.org/10.1161/JAHA.120.020655.
Treibel TA, Fontana M, Gilbertson JA, Castelletti S, White SK, Scully PR, Roberts N, Hutt DF, Rowczenio DM, Whelan CJ, Ashworth MA, Gillmore JD, Hawkins PN, Moon JC. Occult transthyretin cardiac amyloid in severe calcific aortic stenosis: prevalence and prognosis in patients undergoing surgical aortic valve replacement. Circ Cardiovasc Imaging. 2016;9:e005066. https://doi.org/10.1161/CIRCIMAGING.116.005066.
Tschöpe C, Elsanhoury A. Treatment of transthyretin amyloid cardiomyopathy: the current options, the future, and the challenges. J Clin Med. 2022;11:2148. https://doi.org/10.3390/jcm11082148.
Funding
Open access funding provided by Università degli Studi del Piemonte Orientale Amedeo Avogrado within the CRUI-CARE Agreement. This study was funded by “Fondo di Ateneo per la Ricerca” of Università del Piemonte Orientale.
Author information
Authors and Affiliations
Contributions
MG had the idea for the article. All authors performed the literature search. GDZ did the imagine research. PC contributed and coordinated the first draft. MG and PC revised the last draft. All authors agreed on the submission of the last draft.
Corresponding author
Ethics declarations
Competing Interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Research Involving Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Costantini, P., Ostillio, E., Groenhoff, L. et al. Aortic Stenosis and Amyloidosis: Role of MRI and CT in the Diagnosis of a Sneaky Association. Curr Radiol Rep 11, 153–159 (2023). https://doi.org/10.1007/s40134-023-00419-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40134-023-00419-y