Abstract
Purpose of Review
Myocardial infarction in the absence of coronary artery disease is caused by a variety of clinical conditions, so it is important to detect the specific causes in order to perform a better prognostic stratification of these patients. The aim of this review is to summarize the most important findings that established the role of CMR (cardiovascular magnetic resonance) to detect the MINOCA (myocardial infarction with non-obstructive arteries) patients and the importance to differentiate them from myocardial infarction patients.
Recent Findings
The role of CMR is crucial to diagnose the principal diseases involved in MINOCA, as demonstrated. The several MR sequences used in all the MINOCA patients showed different results for all the different causes of MINOCA and, surely, high-resolution MR with gadolinium enhancement has been considered the best method to differentiate the transmural lesions.
Summary
Another fundamental aspect to be considered is the experience of CMR radiologists, which represent the most important element for the right diagnosis of MINOCA. Surely, in the future, CMR will be the most important technique of choice for MINOCA patients, playing a key role in their management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial infarction in the absence of obstructive coronary artery disease is found in 5% to 6% of all patients with acute infarction, who are referred for coronary angiography [1]. The term MINOCA indicates patients with evidence of atherosclerosis that is not hemodynamically compromising [2]. The management of patients with MINOCA is strictly dependent on the cause, so an evaluation should be mandatory in all these patients. The demographic and clinical characteristics of MINOCA patients differ from other patients with AMI (acute myocardial infarction). MINOCA patients are usually younger than patients with AMI−CAD (acute myocardial infarction−coronary artery disease). Women are disproportionately represented among individuals with MINOCA [3,4,5]; they make up close to 50% of the MINOCA population but only 25% of the population with AMI−CAD [5]. MINOCA patients have a lower prevalence of dyslipidemia than their counterparts with AMI−CAD [3,4,5,6]. Finally, other CAD risk factors, such as hypertension, diabetes mellitus, tobacco abuse, and family history of myocardial infarction, are less frequent in MINOCA patients [3,4,5,6].
MINOCA Classification
The European Society of Cardiology proposed the following MINOCA criteria [7]:
-
AMI criteria as defined by the “Third Universal Definition of Myocardial Infarction” [8]
-
Non-obstructive coronary arteries as per angiographic guidelines with no lesions >50% in a major epicardial vessel (plaque disruption) [9],
-
No other clinical specific cause that can be an alternative cause for the acute presentation [1].
Fundamental to the definition of MINOCA is the diagnosis of AMI with an elevated cardiac biomarker, typically a cardiac troponin > 99th percentile of the upper reference level on serial assessment [1]. To limit the diagnostic mistakes due to indiscriminate use of troponin, the “Fourth Universal Definition of Myocardial Infarction” redefined the concept of myocardial injury [10]. Similar to myocardial infarction, the myocardial injury is an elevated troponin beyond the 99th percentile of the upper reference level. The diagnostic challenge is to define these entities, because patients with myocardial injury can show symptoms that mimic myocardial infarction at the initial presentation. In the evaluation of patients with a suspected AMI, it is mandatory to exclude clinical causes for the elevated troponin (sepsis, pulmonary embolism), obstructive disease (complete occlusion of a small coronary artery), and non-ischemic mechanisms of myocyte injury that can mimic myocardial infarction (myocarditis). The elevation of troponin level and the elevation of ST segment, as expression of myocardial injury, are also found in Myocarditis and Takotsubo syndrome that are involved in MINOCA causes, despite the myocardial injury is not referable to a coronary obstruction [1]. Once these causes and pathologies have been considered, a diagnosis of MINOCA can be made (Table 1).
Diagnosis
Many studies have demonstrated the utility of cardiovascular magnetic resonance (CMR) in providing a reclassification of an AMI diagnosis. So CMR is considered a crucial multiparametric diagnostic tool by the European Society of Cardiology working group on MI (myocardial infarction) with non-obstructive coronary arteries [11∙]. Based on a meta-analysis of studies using CMR as a diagnostic tool in MINOCA, myocarditis is the leading diagnosis, and when CMR is performed early, it can secure a diagnosis in up to 87% of cases [1,2,3,4,5,6,7,8,9,10,11∙]. Other causes of MINOCA, as diagnosed by CMR, commonly include Takotsubo cardiomyopathy, acute MI, hypertrophic or dilated cardiomyopathy, and non-cardiac causes (such as pulmonary embolism). Although CMR can provide an evaluation of the myocardium in MINOCA, additional diagnostic testing of the coronary arteries, such as intravascular ultrasonography (IVUS) and optical coherence tomography (OCT), may elucidate the mechanism of MINOCA, including atherosclerotic plaque rupture, erosion, and spontaneous coronary dissection. Furthermore, provocative testing may support coronary vasospasm as a potential cause of MINOCA [1].
Radiological Features
CMR Study Protocol
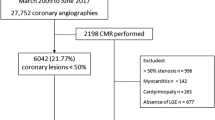
In MINOCA patients, the CMR study should be performed within 7 days from symptom onset. A CMR study protocol to evaluate MINOCA patients include the evaluation of cardiac structure and function of LV (left ventricle) with cine imaging, presence of myocardial edema with T2-weighted (T2w-STIR) image, and presence of myocardial injury with late gadolinium enhancement (LGE) imaging. Moreover, the use of new tissue characterization techniques, T1 and extracellular volume (ECV), and T2 mapping are recommended, due to their diagnostic accuracy in the detection of myocardial damage [12, 13]. Recently, Pierre Francoise Lintigre et al. had showed the diagnostic yield of CMR with high-resolution late gadolinium enhancement, in order to investigate the intramural myocardial lesions in MINOCA patients [14∙∙]. This retrospective study involved 229 patients categorized as MINOCA. The patients were evaluated after lab tests, electrocardiogram, echocardiogram, and conventional CMR, and were performed cine sequences, T2-weighted, first pass perfusion, conventional LGE at 10 min, and high-resolution LGE (HR LGE) free breathing. Was used CMR 1.5 T and the images were interpreted by two readers with 5 and 15 years of experience in a random order, months or years after the acquisitions, and they were blinded to the initial CMR report. Left ventricular volume and ejection fraction were quantified using Argus software (Siemens Medical System). Ventricular dilatation and systolic dysfunction were defined on the basis of previously reported normal values [15]. Cine images were used to look for the abnormality of wall motion or pericardial effusion. T2 weighted were analyzed to look for myocardial edema. LGE imaging was analyzed to look for myocardial perfusion defects and the HR LGE imaging volume could be reviewed in multiplanar reformation of any orientation, depending on LGE location. In each patient, the distribution of LGE was described as subendocardial, subepicardial, and midwall. The criterion to diagnose the myocardial infarction on CMR was the presence of subendocardial or transmural LGE [16]. Myocarditis was instead diagnosed with the presence of definite midwall or subepicardial LGE in the absence of subendocardial LGE [12]. Takotsubo syndrome was diagnosed when wall motion abnormality was found evolving in the apical or basal in the absence of myocardial LGE [17]. In these patients were performed a follow-up at 3 months using CMR or TTE. A total of 229 patients were recruited for MINOCA. Electrocardiography showed ST elevation for myocardial infarction in 85 patients, and TTE were negative in 124 patients, coronary angiography showed normal arteries in 125 patients, and non-obstructive CAD in 104. All patients underwent CMR, and a subpopulation of 172 patients had HR LGE as added protocols when diagnosis remained inconclusive. These patients (86) had a definite diagnosis: myocardial infarction in 39, acute myocarditis in 32, Takotsubo cardiomyopathy in 13, and other diagnosis in 2. In this study, HR LGE could reveal the infarction in 14% and rule out the diagnosis of infarction in 12%. The interpretation of myocardial injury with HR LGE led to a modification of diagnosis in 45 of 172 patients, with a modification of prognosis, and a different decision making on therapy [14∙∙]. HR LGE had showed in this study how it could be more incisive for the outcome of MINOCA patients when conventional CMR is negative.
Acute Myocarditis
Inflammation of the myocardium may occur as a result of exposure to antigens such as viruses, bacteria, protozoa, drugs, toxins, or as an autoimmune condition. CMR is indicated for patients with new presentation or persisting of symptoms suggestive of myocarditis (dyspnea, orthopnea, palpitations, chest pain, effort intolerance), if viral etiology is suspected with no evidence of coronary stenosis. According to the European Society of Cardiology Working group and to the last guidelines, myocarditis diagnosis is performed by CMR as a Class I procedure for the identification of myocarditis [18]. The CMR protocol used for these patients consisted in evaluation of: Presence and pattern of myocardial edema with T2w-STIR images: Patchy areas of high signal intensity; Subepicardial or septal high signal intensity; Transmural high signal intensity (not specific for myocardial inflammation); Global high signal intensity evaluated through the T2-ratio technique; Evaluation of myocardial early gadolinium enhancement ratio that explore the regional vasodilation as a feature of tissue inflammation. The presence and pattern of necrosis and fibrosis with LGE imaging: Patchy areas of enhancement; Subepicardial enhancement; and transmural enhancement. These criteria are evaluated in parallel to the cardiac structure and function with cine imaging due to the evaluation of the presence of LV dysfunction with regional or global systolic dysfunction or pericardial effusion which were considered supportive criteria. According to LLC (Lake Louise criteria) CMR findings of T2 STIR sequences for myocardial edema and early gadolinium sequences for hyperemia are predictive of myocarditis, if at least 2 of 3 of the previous criteria are present. The mapping techniques can derive T1 and T2 relaxation time and permit ECV (extracellular volume) calculation. These techniques provide better diagnosis than traditional sequences in the diagnosis of acute myocarditis, in particular the reported AUC (area under the curve) for T1 mapping was 0.95, for T2 mapping was 0.88, and for ECV (extracellular volume) 0.81 [18] (Fig. 1). To assess the role of CMR and to detect the non-obstructive causes of Minoca, Heidecker Bettina et al., in a study of 2019, had investigated the myocarditis patients in a population of 556 MINOCA patients with high levels of Troponin and angina-like symptoms, without significant coronary artery obstruction [19]. The study was a retrospective chart review between 2011 and 2017. CAD was excluded using a coronary angiography or a coronary CT in all the patients with a rise in Troponin level and angina-like symptoms. All the patients with an obstruction < 50% had a CMR to exclude other causes of MINOCA. CMR 1.5 T was used and all the images were performed under the supervision of the head of cardiac imaging, who had several years of experience. Were performed, with this purpose, cine-images, T2-weighted imaging and LGE (Late Gadolinium Enhancement) images evaluated in 10 min. Myocarditis was considered when there was an epicardial or midwall distribution of LGE, associated with a patchy pattern and non-coronary distribution [20, 21]. 556 patients were admitted, and CMR was able to diagnose 76 (13.7%) myocarditis, 34 (6.1%) dilated cardiomyopathy, 41 ischemia during stress, 15 hypertrophic, 13 pericarditis, 8 amyloidosis, 7 Takotsubo, 5 sarcoidosis, 3 Fabry’s disease, others 22, and 332 normal heart. For these reasons, a great number of myocarditis was investigated, and this study had showed the central role of CMR to detect another important cause of MINOCA, often unremarkable by systematic work up of the patients with angina-like symptoms, rise of troponin, and no significant coronary artery disease [22].
30-year-old patient with myocarditis symptoms. The diagnosis was made with these significant images according to Lake Louise Criteria: a T2 STIR 3-chamber view with subepicardial hyperintensity of inferior and inferolateral walls and edema. b Delayed enhancement in short-axis view with subepicardial hyperintensity of inferior and inferolateral walls and edema of LV. c Delayed enhancement in 3-chamber view with subepicardial hyperintensity of inferolateral wall with edema
Takotsubo Syndrome
CMR is able to identify LV (left ventricle) wall motion abnormalities, and provides the evaluation of right ventricle (RV) motility [17, 23]. The most common presentation of TS (Takotsubo) is LV apical akinesia with preserved function of the remaining segments, which causes the typical “apical ballooning” appearance. Mid-ventricular type, basal or inverted type, focal variants, and isolated or concomitant RV (right ventricle) akinesia have also been described but with lower frequency [24]. Wall motion abnormalities are reversible and complete recovery of systolic function has been demonstrated at 3 months of follow-up [25]. CMR represents a widely established method to non-invasively assess myocardial tissue, within a scanning time of 30 min [26]. CMR myocardial edema can be detected by means of T2w-STIR images or assessed either on T1- or T2-mapping sequences, with increased values in both ballooning and non-ballooning segments [27]. Usually, no LGE (late gadolinium enhancement) is seen in Takotsubo patients. In conclusion, wall motion abnormalities and absence of LGE represent the findings that permit CMR for providing a diagnosis of Takotsubo in patients with high serum troponin levels, and for differentiating this entity from myocardial infarction and myocarditis [27]. The epidemiological data of MINOCA showed that women were disproportionately represented among MINOCA patients, in fact Harmony R. Reynolds et al., in a recent prospective study of November 2020, had involved 301 women at 16 sites, with a clinical diagnosis of myocardial infarction [28∙]. When coronary angiography showed a < 50% stenosis in all major artery, an OCT was performed, followed by CMR. CMR was performed one week after the symptoms, and the images were interpreted by different laboratories blinded to the results of other laboratories. OCT was performed using an OCT ILUMIEN OPTIS, and CMR was 1.5 T or 3.0 T and T2-weighted, fat-suppressed, fast-spin echo, LGE at 10 or 15 min, and T1 mapping were performed [29]. Although patients involved were 301, only 147 had an OCT evaluation and 67 had a culprit lesion (rupture plaque, intraplaque cavity, and thrombus without rupture plaque). Three patients had coronary spasm. CMR was interpretative in 116 of the 147 participants with an interpretable OCT and showed regional injury in 24 women, myocarditis in 17, Takotsubo cardiomyopathy in 4, non-ischemic cardiomyopathy in 3, and normal heart in 30 patients [30]. Furthermore, this study had demonstrated that among 116 women who had OCT and CMR evaluation, 98 had an abnormality on one or both methodic, and surely the prevalence of abnormalities indicating a cause of MINOCA presentation after the combination of OCT and CMR was 84.5%, significantly higher than OCT alone or CMR alone.
Ischemic Causes of MINOCA
CMR imaging is a diagnostic tool to be employed in MINOCA patients with suspected acute myocardial infarction. Myocardial edema is evaluated on T2w-STIR images and LGE that permit the evaluation of myocardial damage and gives information about the mechanisms. Transmural LGE indicates an ischemic cause of injury, but it does not specify the particular mechanism of ischemia, while a non-ischemic appearance of LGE (mesocardial or subepicardial localization) is indicative of other myocardial disorders such as myocarditis and other cardiomyopathies [30] (Figs. 2, 3). To this purpose, Amerdeep Gosh Dastidar et al., in a study of 2018, investigated the prognostic impact of CMR in these patients [31] in a retrospectively study of 388 MINOCA. The protocols provided the use of 1.5 T CMR and included cine imaging, T2 weighted for myocardial edema, and early and late gadolinium enhancement imaging [32]. Patients were grouped in 4 categories: myocardial Infarction, myocarditis, cardiomyopathies, and normal CMR. CMR was performed with a median of 37 days from clinical presentations, and the images were analyzed by radiologists with 15 years of experiences, all with an ESC CMR level 3 certification. The cases of myocarditis were diagnosed by LLC: T2 STIR sequences for myocardial edema and early gadolinium sequences for hyperemia [19]. Myocardial infarction was diagnosed by territorial subendocardial and transmural LGE. Cardiomyopathies, in particular Takotsubo, were diagnosed by T2 STIR for myocardial edema and regional wall motion in mid-cavity or apical distribution with no myocardial LGE [24]. Normal heart was defined based on no regional wall motion abnormality, no myocardial edema, and no myocardial LGE. In this study, CMR was able to identify the causes of troponin rise in 74% of patients, which were so distributed: 25% myocarditis, 25% patients with myocardial infarction, 25% cardiomyopathy, and 26% normal heart. The cardiomyopathy group, represented by Takotsubo syndrome, had showed a worst prognosis over a median of follow-up of 3.5 years with a 15% of death. In particular, in these patients, CMR could better identify the cases by delineating the myocardial edema, RV involvement, presence of thrombus caused by the stunning of apical wall, and LV outflow tract obstruction. The study had also showed the importance of CMR and ST elevation on ECG, as best predictors of mortality. All these data had led a better stratification of all the MINOCA patients involved in order to assess the right treatment and change the clinical history of the patients.
47-year-old patient with known thrombophilia and typical myocardial infarction symptoms. The presentation was negative T wave in anterior and regression of symptoms. Angiography does not show significative stenosis and CMR was performed that showed a Delayed enhancement in 2-chamber view with transmural necrosis of the apex and anterior wall. b Delayed enhancement in 4-chamber view with transmural necrosis of apex, lateral wall, and inferior sept. c Delayed enhancement in 3-chamber view with transmural necrosis of apex, posterior wall, and anterior sept
63-year-old patient with non-obstructive stenosis of MO1 and atrial fibrillation with rapid ventricular response and subendocardial ischemia. a T2 STIR short-axis view of subendocardial hyperintensity of lateral wall with edema. b Delayed enhancement in 4-chamber view of subendocardial edema in lateral wall
Other Causes of MINOCA
Hypertrophic Cardiomyopathy
HCM (Hypertrophic cardiomyopathy) patients present with increased ventricular myocardial thickness and could have hyperintense myocardial areas at T2w-STIR images, altered first pass perfusion and presence of LGE. T1- and T2-mapping MR imaging techniques are able to identify myocardial injuries associated with HCM without gadolinium-based contrast agents [33,34,35,36,37]. Therefore, T1 mapping without contrast may identify myocardial scarring as well as interstitial fibrosis in HCM. The T2 alterations are associated with edema and may represent acute ischemic damage so hypertrophic cardiomyopathy could be the expression of MINOCA. Furthermore, the presence of LGE seems to be a marker of increased risk of non-sustained ventricular tachycardia episodes as a prognostic factor. Cine SSFP (steady-state free precession sequences) MR imaging is used for morphological assessment of HCM and evaluation of cardiac function. These sequences are able to define all phenotypes of HCM because of its no limited view. Using retrospective gating, cine SSFP is the most important method to quantify the myocardial thickness and mass, which are related to the prognosis of HCM [33,34,35,36,37].. Late gadolinium enhancement is the most valuable MR imaging sequence for HCM, because it identifies the myocardial fibrosis that contributes to risk stratification for HCM [37]. The myocardial fibrosis is strictly related to ventricular tachyarrhythmia and so late gadolinium enhancement is significantly related to ventricular tachyarrhythmia associated with HCM. Late gadolinium enhancement is also useful for differentiating HCM from other cardiomyopathies with similar symptoms and LVH [35, 36].
Conclusions
These studies highlight the potential benefit of using CMR to evaluate MINOCA patients for a better treatment based on the detected cause. CMR can confirm MI (myocardial infarction) for accurately categorizing patients according to the contemporary definition of MINOCA. Additional tests of the coronary arterial system could provide further insights into the cause of MINOCA in patients who have an MI (Figs. 2 and 3), and although invasive, remain the first step to diagnose MINOCA. CMR is non-invasive and can differentiate MI from myocarditis (Fig. 1) and various cardiomyopathies, led to personalized treatment pathways and led to a better prognostic stratification of these patients. A multi-parametric CMR protocol may include functional imaging and advanced tissue characterization techniques, such as T1 mapping, LGE imaging, and HR LGE, that if performed early within 1 week of the acute presentation could change statistically significant the outcome of MINOCA patients, changing clinical assessment, therapy, and prognosis. The advantages of using CMR to guide management in MINOCA patients include a true diagnosis of MI, to distinguish from non-ischemic causes, and evaluate the extent and functional impact of the acute myocardial injury. Different and combined methodical as OCT and CMR had showed the importance of this approach to detect the obstructive causes of MINOCA. CMR has demonstrated clinical utility in diagnosis and prognosis of MINOCA and this has led to insert CMR in the guidelines, as a first method to investigate MINOCA in all inconclusive diagnoses.
References
Papers of particular interest, published recently, have been highlighted as: ∙ Of importance ∙∙ Of major importance
Tamis-Holland JE, Brilakis ES, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139:e891–908. https://doi.org/10.1161/CIR.0000000000000670.
Beltrame JF. Assessing patients with myocardial infarction and nonobstructed coronary arteries (MINOCA). J Intern Med. 2013;273:182–5. https://doi.org/10.1111/j.1365-2796.2012.02591.x.
Barr PR, Harrison W, Smyth D, Flynn C, Lee M, Kerr AJ. Myocardial infarction without obstructive coronary artery disease is not a benign condition (ANZACS-QI 10). Heart Lung Circ. 2018;27:165–74. https://doi.org/10.1016/j.hlc.2017.02.023.
Safdar B, Spatz ES, Dreyer RP, Beltrame JF, Lichtman JH, Spertus JA, Reynolds HR, Geda M, Bueno H, Dziura JD, Krumholz HM, D’Onofrio G. Presentation, clinical profile, and prognosis of young patients with myocardial infarction with nonobstructive coronary arteries (MINOCA): results from the VIRGO study. J Am Heart Assoc. 2018;7:e009174. https://doi.org/10.1161/JAHA.118.009174.
Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131:861–70. https://doi.org/10.1161/CIRCULATIONAHA.114.011201.
Daniel M, Agewall S, Caidahl K, Collste O, Ekenbäck C, Frick M, Y-Hassan S, Henareh L, Jernberg T, Malmqvist K, Schenck-Gustafsson K, Sörensson P, Sundin Ö, Hofman-Bang C, Tornvall P. Effect of myocardial infarction with nonobstructive coronary arteries on physical capacity and quality-of-life. Am J Cardiol. 2017;120:341–6. https://doi.org/10.1016/j.amjcard.2017.05.001.
Agewall S, Beltrame JF, Reynolds HR, Niessner A, Rosano G, Caforio AL, De Caterina R, Zimarino M, Roffi M, Kjeldsen K, Atar D, Kaski JC, Sechtem U, Tornvall P, on behalf of the WG on Cardiovascular Pharmacotherapy. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017;38:143–53. https://doi.org/10.1093/eurheartj/ehw149.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, the Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35. https://doi.org/10.1161/CIR.0b013e31826e1058.
Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM. ACC/AHA guidelines for coronary angiography: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). J Am Coll Cardiol. 1999;33:1756–824.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, the Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138:e618–51. https://doi.org/10.1161/CIR.0000000000000617.
∙Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, Gilard M, Jobs A, Jüni P, Lambrinou E, Lewis BS, Mehilli J, Meliga E, Merkely B, Mueller C, Ro M, Rutten FH, Sibbing D, Siontis GCM, ESC Scientic Document Group. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020. https://doi.org/10.1093/eurheartj/ehaa575. It’s an important recent reference which allows to understand how to treat patients without persistent ST-segment elevation and how to manage them with suitable diagnostic exam.
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras A, Laissy JP, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P, International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol. 2009;2009(53):1475–87. https://doi.org/10.1016/j.jacc.2009.02.007.
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, Mascherbauer J, Nezafat R, Salerno M, Schelbert EB, Taylor AJ, Thompson R, Ugander M, van Heeswijk RB, Friedrich MG. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson. 2017;19:75. https://doi.org/10.1186/s12968-017-0389-8.
∙∙Lintingre P-F, Nivet H, Clément-Guinaudeau S, Camaioni C, et al. High-resolution late gadolinium enhancement magnetic resonance for the diagnosis of myocardial infarction with nonobstructed coronary arteries. JACC Cardiovasc Imag. 2020;13(5):1135–48. https://doi.org/10.1016/j.jcmg.2019.11.020. Very important and recent reference which allows to perform a great MRI, with great images for patients with MINOCA.
Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel ER, et al. Normal values for cardiovascular magnetic resonance in adults and children. J Cardiovasc Magn Reson. 2015;17:29.
Rajiah P, Desai MY, Kwon D, Flamm SD. MR imaging of myocardial infarction. Radiographics. 2013;33:1383–412.
Ferreira VM. CMR should be a mandatory test in the contemporary evaluation of “MINOCA.” JACC Cardiovasc Imaging. 2019;12:1983–6. https://doi.org/10.1016/j.jcmg.2019.05.011.
Pan JA, Lee YJ, Salerno M. Diagnostic performance of extracellular volume, native T1, and T2 mapping versus lake Louise criteria by cardiac magnetic resonance for detection of acute myocarditis: a meta-analysis. Circ Cardiovasc Imaging. 2018;11:e007598. https://doi.org/10.1161/CIRCIMAGING.118.007598.
Bettina H, Gianni R, Nora B, Eva G, et al. Systematic use of cardiac magnetic resonance imaging in MINOCA led to a five-fold increase in the detection rate of myocarditis: a retrospective study. Swiss Med Wkly. 2019;149:w20098. https://doi.org/10.4414/smw.2019.20098.
Patriki D, Gresser E, Manka R, Emmert MY, Lüscher TF, Heidecker B. Approximation of the incidence of myocarditis by systematic screening with cardiac magnetic resonance imaging. JACC Heart Fail. 2018;6(7):573–9.
Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, Friedrich MG, American College of Cardiology Foundation Task Force on Expert Consensus Documents, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;121(22):2462–508.
Kagiyama N, Okura H, Kume T, Hayashida A, Yoshida K. Isolated right ventricular takotsubo cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2015;16:285. https://doi.org/10.1093/ehjci/jeu207.
Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, Carbone I, Muellerleile K, Aldrovandi A, Francone M, Desch S, Gutberlet M, Strohm O, Schuler G, Schulz-Menger J, Thiele H, Friedrich MG. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306:277–86. https://doi.org/10.1001/jama.2011.992.
Perazzolo Marra M, Zorzi A, Corbetti F, De Lazzari M, Migliore F, Tona F, Tarantini G, Iliceto S, Corrado D. Apicobasal gradient of left ventricular myocardial edema underlies transient T-wave inversion and QT interval prolongation (Wellens’ ECG pattern) in Tako-Tsubo cardiomyopathy. Heart Rhythm. 2013;10:70–7. https://doi.org/10.1016/j.hrthm.2012.09.004.
D’Angelo T, Grigoratos C, Mazziotti S, Bratis K, Pathan F, Blandino A, Elen E, Puntmann VO, Nagel E. High-throughput gadobutrol-enhanced CMR: a time and dose optimization study. J Cardiovasc Magn Reson. 2017;19:83. https://doi.org/10.1186/s12968-017-0400-4.
Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, Crea F, Galiuto L, Desmet W, Yoshida T, Manfredini R, Eitel I, Kosuge M, Nef HM, Deshmukh A, Lerman A, Bossone E, Citro R, Ueyama T, Corrado D, Kurisu S, Ruschitzka F, Winchester D, Lyon AR, Omerovic E, Bax JJ, Meimoun P, Tarantini G, Rihal C, Y-Hassan S, Migliore F, Horowitz JD, Shimokawa H, Lüscher TF, Templin C. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J. 2018;39:2032–46. https://doi.org/10.1093/eurheartj/ehy076.
Gaikwad N, Butler T, Maxwell R, Shaw E, Strugnell WE, Chan J, Figtree GA, Slaughter RE, Hamilton-Craig C. Late gadolinium enhancement does occur in Tako-tsubo cardiomyopathy—a quantitative cardiac magnetic resonance and speckle tracking strain study. Int J Cardiol Heart Vasc. 2016;12:68–74. https://doi.org/10.1016/j.ijcha.2016.07.009.
∙Reynolds HR, Hochman JS. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of myocardial infarction with nonobstructive coronary arteries in women. Circulation. 2021;143:624–40. https://doi.org/10.1161/CIRCULATIONAHA.120.052008. An important comparison study between different techniques of imaging for MINOCA woman patient.
Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. https://doi.org/10.1161/01.cir.100.19.1992.
Update. Eur Heart J Acute Cardiovasc Care 2019;8:54–62. https://doi.org/10.1177/2048872618782414
Dastidar AG, Baritussio A, De Garate E, Drobni Z, Biglino G, et al. Prognostic role of CMR and conventional risk factors in myocardial infarction with nonobstructed coronary arteries. JACC Cardiovasc Imaging. 2019;12(10):1973–82. https://doi.org/10.1016/j.jcmg.2018.12.023.
Dastidar AG, Rodrigues JC, Baritussio A, Bucciarelli-Ducci C. MRI in the assessment of ischaemic heart disease. Heart. 2015;102:239–52.
Bois JP, Geske JB, Foley TA, Ommen SR, Pellikka PA. Comparison of maximal wall thickness in hypertrophic cardiomyopathy differs between magnetic resonance imaging and transthoracic echocardiography. Am J Cardiol. 2017;119:643–50.
Spirito P, Bellone P, Harris KM, Bernabo P, Bruzzi P, Maron BJ. Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med. 2000;342:1778–85.
Simonetti OP, Kim RJ, Fieno DS, et al. An improved MR imaging technique for the visualization of myocardial infarction. Radiology. 2001;218:215–23.
Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ. Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. J Am Coll Cardiol. 2003;41:1561–7.
Olivotto I, Maron BJ, Appelbaum E, et al. Spectrum and clinical significance of systolic function and myocardial fibrosis assessed by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Am J Cardiol. 2010;106:261–7.
Funding
Open access funding provided by Università di Foggia within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatrics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Michele, F., Guerra, F.S., Forte, V. et al. Cardiovascular Magnetic Resonance (CMR) for the Evaluation of Myocardial Infarction in Patients with Non-obstructive Coronary Artery Disease (MINOCA). Curr Radiol Rep 9, 9 (2021). https://doi.org/10.1007/s40134-021-00384-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s40134-021-00384-4