Abstract
Purpose of review
To identify lessons learned about maintaining confidentiality for adolescent telehealth care during the COVID-19 pandemic.
Recent findings
Adolescents, parents, and providers recognize benefits of telehealth for confidential care while also identifying potential risks for confidentiality breach unique to the telehealth care setting.
Summary
Rapid implementation of telehealth care during COVID-19 presented an opportunity to test strategies that protect confidentiality for adolescents accessing care through telehealth. Policy, practice, and provider-level interventions are needed to ensure that adolescents can access confidential care through telehealth
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“I need to talk to my doctor alone,” was scratched on a tiny, folded note that was handed to the nurse as the patient was checked in. The note came from one of my adolescent patients during her first in-person visit with me since the start of the COVID-19 pandemic and following the quick pivot among providers around the world to the delivery of healthcare via telehealth. I had seen her many times on a screen over the past several months discussing strategies to help her depression and chronic pain. Often, her mother sat beside her during the visits although we had time alone during these visits as well. We had tried medication changes as well as many other lifestyle habit changes to work on her symptoms, but like so many during that difficult time, her symptoms had worsened. In the exam room without anyone nearby to overhear, the patient disclosed emotional abuse and trauma experienced in her home, all of which had worsened during the pandemic.
In early 2020, as the COVID-19 pandemic took hold around the world, many healthcare providers pivoted to telehealth to preserve access to healthcare for their patients [1,2,3,4]. Adolescents have been considered ideal for telehealth practices being perceived as “digital natives” and being a particularly vulnerable population with issues of limited access to healthcare [5,6,7]. However, provision of telehealth care had been limited due largely to poor reimbursement and cumbersome regulatory issues [6]. The abrupt shift to telehealth care during the pandemic presented opportunities to learn more about how telehealth care should be delivered to adolescents, particularly to ensure that confidentiality is preserved [8•, 9•, 10•]. The patient scenario described above highlights that key health information may be missed when confidentiality during telehealth visits is impaired. This paper will review evidence gathered during the COVID-19 pandemic telehealth surge, with a spotlight on the pinnacle of adolescent healthcare — confidentiality.
Prior to the pandemic, there was increasing evidence supporting telehealth care for adults with positive outcomes as well as patient and provider satisfaction with the care provided, particularly for mental health and chronic condition care. Very little literature existed relating to adolescent telehealth experiences particularly in relation to the adolescent experience [11]. Early adopters during the pandemic shared their observations, describing a variety of methods used to preserve confidentiality in the telehealth setting, particularly when providers addressed sensitive topics, such as reproductive and sexual health, mental health and substance use [8•, 9•, 10•]. Based on these shared observations, an ideal care delivery model is presented here that aims to maintain confidentiality across the telehealth visit continuum.
Telehealth care is defined by the World Health Organization as “a broad range of technologies and services to provide client care remotely and improve health-care delivery and systems” [12]. For the purposes of this paper, telehealth includes synchronous healthcare visits conducted between a patient and healthcare provider via video or phone in lieu of in-person, office-based visits.
Rapid Implementation
Rapid implementation of telehealth with the onset of the COVID-19 pandemic allowed for access to healthcare providers when state governments had mandated “shelter in place” and/or “stay at home” policies during peak infection rates [1, 2, 4710•]. Previously, telehealth had been explored and utilized in similar circumstances, such as during H1N1 and Zika outbreaks [6], but in early 2020, healthcare providers around the world quickly developed telehealth practices to remain connected with their patients especially those at highest risk of medical decline [1, 2710•]. In 2016, 11.8% of US family physicians and pediatricians reported working in a practice with telehealth services and within 2 months of the COVID-19 pandemic, only 9% of primary care physicians reported working in a practice that did not offer these services [7]. Adolescent medicine providers were on the front line during this time developing protocols and mechanisms that facilitated telehealth with adolescents for multiple aspects of care [2, 8•, 9•, 10•]. Published literature sharing experiences of rapid telehealth expansion in March 2020 describes increases from an average of 2.5 telehealth visits weekly to 220 telehealth visits weekly [2]. Within 1 month of the shelter in place order, Barney et al. (2020) describe an increase in percent of encounters that were conducted through telehealth from 0 to 97% and Carlson et al. (2020) report a 600% increase in telehealth visits at their institution [8•, 10•]. As we move into the post-pandemic era, lessons learned from this rapid implementation can guide future innovative approaches to health care delivery. However, providing increased access must include what decades of research in adolescent health has demonstrated — that adolescents require confidentiality as an element of their healthcare to ensure that all needs are met [13,14,15,16].
Consent and Confidentiality
While there is variation by state, adolescents are legally able to consent to a variety of healthcare services that focus on sensitive areas, such as reproductive and sexual health, mental health and substance use, and with the right to consent comes privacy and confidentiality pertaining to these services [17, 18]. An abundance of research demonstrates that adolescents will forgo care if confidentiality is not part of their care and that they would not share details about their risky behaviors with their healthcare providers when confidentiality is not guaranteed [19,20,21,22,23]. With risky behaviors being key drivers of morbidity and mortality in adolescents, multiple organizations have developed evidence-based and expert opinion guidelines advising that adolescents have alone time with their providers to ensure these sensitive subject areas are thoroughly addressed. These recommendations are based on the importance of confidentiality as well as the developmental milestones of achieving independence and autonomy that are essential for adolescents to transition to adulthood [13,14,15,16].
Despite HIPPA regulations mandating privacy for services to which adolescents consent as well as professional organizations endorsing protection of adolescent confidentiality, there are many potential leaks in the healthcare system [18, 24]. Confidential information may be shared due to provider lack of knowledge about consent and confidentiality and/or discomfort with following these guidelines. In fact, only approximately 50% of adolescents report that they had time alone with their provider where there would be an opportunity to discuss confidential concerns [21, 25]. Even when providers do create opportunities for adolescents to consent to confidential services, direct billing by healthcare institutions and/or explanation of benefits from payors being sent to adolescents’ homes pose significant risk for breach of confidentiality [18]. With electronic health records (EHR) dominating healthcare delivery, additional numerous opportunities for leaks were created through patient portals listing diagnoses, medications and lab test results [24, 26]. While many institutions provide opportunities for adolescents and their parents to have separate portal access, there is accumulating evidence that parents are frequently able to access their adolescents’ accounts [27•, 28]. Professional organizations suggest mechanisms for protecting confidentiality in the era of EHR; however, these rely heavily on individual approaches from institutions as well as providers with minimal support from EHR corporations and legislation. These limitations create conflict between accessibility of patients to their healthcare data and protection of adolescent confidential services [24, 26, 29,30,31].
Confidential Telehealth Care: Advantages
Prior to the pandemic, telehealth for adolescents had been cited as a means to improve access to care particularly those in geographically remote areas or with transportation challenges. Pre-pandemic research suggested that adolescents, parents, and providers viewed telehealth as an acceptable form of care delivery with advantages including decreased time to travel, less missed work or school, and fewer expenses associated with travel, missed work or childcare for other children [32•]. Telehealth research had focused focusing on specific regions with infectious outbreaks or limited access and indicated that adolescents could develop therapeutic relationships with providers [33]. Furthermore, and that most adolescents, even those without stable housing, had access to a mobile device of some kind [34]. Specific visit types where telehealth was identified as ideal for confidential care included reproductive and sexual health, gender-affirming care, behavioral health, substance use and eating disorders [6]. However, existing electronic health and/or telehealth policy statements offered minimal guidance to providers to reliably facilitate confidentiality in the telehealth setting [8•].
Shortly after the world pivoted from in-person to telehealth visits, the American Academy of Pediatrics released a statement endorsing use of telehealth in the care of pediatric patients [35]. This was followed by release of a technical report in 2022 which provides guidance for pediatric telehealth visits but lacks substantive guidance on approaches that preserve access to confidential care [36]. Strategies used by early adopters during the pandemic as well as provider, parent and patient perspectives regarding telehealth care centered on confidentiality can help inform future revisions of telehealth care policies and guidelines.
The general utility of telehealth for adolescents was reconfirmed in the experiences described by the pandemic’s early adopters whereby patients and providers observed telehealth offering an alternative point of care that decreased travel, cost, and time. In fact, authors sharing these early experiences speculated that telehealth may have expanded the geographic footprint for adolescent confidential services in ways that were not possible prior to the pandemic [8•, 9•]. Rationale for telehealth implementation, in addition to following governmental shelter-in-place orders, also included the need for distancing to prevent infection transmission, to conserve personal protective equipment (PPE) and to protect the healthcare workforce [9•]. Providers further acknowledged some added benefit in seeing the adolescents’ home environment and having more family members able to participate in the visit [32•].
Adolescents endorsed that telehealth provided opportunities for confidential care [37•], some appearing more engaged when discussing sensitive topics via telehealth as compared to in-person visits [38,39,40]. The stigma associated with receiving care for mental health, sexual health and substance use may be removed when able to attend visits in the privacy of one’s own home [41, 42]. Several institutions shared visit data suggesting increased or similar engagement and show rates with telehealth compared to in-person visits [8•, 9•]. Barney et al. (2020) noted that visits were well-received by patients but did encounter some difficulty when patients attempted to find private, quiet space to complete the confidential aspects of the visit. Of the 332 visits they studied, 7 visits were completed without confidential elements due to inability for the patient to identify a private space [8•]. Wood et al. (2020) reported that the no-show rates were lower for telehealth visits compared to in-person visits with clinical needs including eating disorders (39%), contraception and menstrual issues (22%), gender-affirming care (17%), general adolescent medicine (15%), HIV treatment (6%) and substance use (1%). While they expected confidentiality to potentially be compromised, there were no breaches identified for the 392 visits studied and adolescents were able to have confidential time with their providers when needed [9•].
Confidential Telehealth Care: Challenges
While the early adopters noted that telehealth care was well-suited for addressing sensitive topics and were able to maintain confidentiality for most visits, they also identified many ways in which privacy and confidentiality can be uniquely challenged with this mode of care delivery. Even though adolescents voiced increased comfort discussing sensitive issues via telehealth, they also indicated concerns about privacy and confidentiality [37•, 4344•]. The reliability of the telehealth platforms in maintaining privacy and confidentiality was called into question by patients and parents, particularly early on in the telehealth surge [10•]. WHO guidelines further cited concerns for privacy being compromised for adolescents if they are using someone else’s device or if spyware has been installed on the devices they use [12]. Providers were the most consistent in expressing skepticism about the security of the various telehealth platforms used [10•, 45]; yet there were no reports of major platform security failures.
As much as apprehension existed regarding the technological reliability of telehealth platform privacy, concerns about the adolescents’ surroundings limiting privacy and confidentiality were more substantial. Adolescents and their parents shared reservations about others’ nearby overhearing confidential discussions [44•]. Identifying a private space for the telehealth visit was more challenging for homeless adolescents or those living in crowded housing [8•, 9•]. When comparing sense of privacy between telehealth and in-person visits, parents and patients reported a perceived lower privacy level for telehealth visits compared to in-person visits (77% vs. 96%, respectively). Parents and adolescents in this same study conducted by Allison et al. (2022) confirmed that they would be able to identify a private space if needed and acknowledged the important implications of the adolescent having time alone with a provider. However, only 31% of adolescents in that study reported having time alone with their provider [44•].
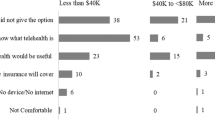
Primary care providers described similar frequency of time alone with patients, reporting that 28% requested alone time to speak with adolescent always or often, 38% sometimes, and 33% rarely or never during telehealth visits [46•]. This is substantially lower than an already less than optimal reported percentage of alone time with in-person visits [21, 25]. Time alone during telehealth visits may be lower due to provider concerns about others’ overhearing as evidenced through a survey of primary care providers where advantages of adolescent telehealth care were acknowledged but, one in three cited a lack of privacy as a major disadvantage. Most (89%) surveyed reported use of telehealth to see adolescent patients for a variety of care concerns including chronic disease management, acute care, mental and behavioral health, vaccine consultation and sexual health or contraceptive counseling, many of which would typically require time alone with the provider [46•].
The heightened complexity of not knowing who is in the room or who is nearby with telehealth visits has been cited by telehealth experts as raising concerns that responses to particularly sensitive questions may be limited or that there may be more risk for coerced responses [7]. Even when adolescents share a 360-degree view at the onset of the telehealth visit, providers might not know if individuals come into the room during the telehealth visit or if an individual is in a separate but nearby space and can overhear. In addition, physical examination already very limited through telehealth, was cited as particularly challenging with adolescents, especially for sensitive symptoms, such as genital lesions [8•].
Provider discomfort with negotiating the time alone with the adolescent patient has been one explanation for the existing gap in reported time alone [21]; a discomfort that appears to be heightened in the telehealth setting. Interestingly, the patients’ therapeutic alliance with their provider was positively correlated with the perceived level of privacy and the therapeutic alliance was higher when the patients had seen the provider in person prior to the telehealth visit [44•]. These findings suggest that telehealth care may be more advantageous after at least one in-person visit and/or that training in telehealth-based rapport building skills and methods to negotiate alone time is needed.
Outside of the actual visit, challenges to preserve confidentiality had been previously identified and appear to persist with telehealth visits. One area of concern associated with telehealth visits surrounds appointment notification. Many EHR systems send automated text or email appointment reminders. This is particularly important for telehealth visits as often the appointment reminders guide patients through the process of signing on to the telehealth visits. However, if automated notification of the appointment occurs and is delivered to a caregiver phone or email address, confidentiality may be compromised. In addition, caregivers may be able to view upcoming appointments through the caregiver/proxy EHR portal account or through inappropriate access to their adolescent’s EHR portal [10•]. With the Cures Act mandating increased access for all healthcare consumers to their records, concern is higher that adolescent confidentiality may be jeopardized through the inappropriate access by parents to adolescent portals or unfiltered parental portal access revealing medications, diagnoses, open notes and after-visit summaries that contain information that when shared with parents could jeopardize the safety and well-being of the adolescent [31].
Confidential Telehealth Care: Solutions
The conflict between the benefit of improved access to care for adolescents and risk of compromised confidentiality can be addressed at many levels including public policy as well as institutional, practice and/or provider-level interventions. Multiple action steps to protect adolescent confidentiality can occur prior to, during and after the telehealth visit as illustrated in the care delivery model in Fig. 1. First, institutional and practice policies regarding adolescent consent and confidentiality during all types of visits should be clearly posted and easily shared with patients and families. Next, institutions should ensure that a secure telehealth platform is used with the ideal being a platform embedded in the institution’s highly secure electronic medical record system [10•, 26]. The institution’s information technology (IT) group in collaboration with adolescent medicine experts should be involved in the selection of the platform as well as development of an infrastructure within EHR that supports a workflow honoring consent and confidentiality policies.
Developing a tiered system of appointments within the EHR system can prevent confidential appointments from being viewed in the portal and block automated appointment notification [9•, 10•]. More ideal would be the use of adolescent confidential contact information for these appointments to allow appointment reminders and use of the reminder to guide access to the telehealth visit. Other IT solutions have included blocking specific diagnoses, tests and medications from view in the patient portal [9•, 24]. However, adolescents need access to all of their relevent health information in their own patient portal that is not accessed by parents or others. Training in adolescent rights to consent and confidentiality along with portal access as well as scheduling appointments is essential for staff and providers to protect adolescent confidentiality [8•]. Many providers report being aware of ways to improve confidentiality in electronic health systems but only 22% report receiving any training on it [47]; While there are no data regarding staff training, this is likely even lower given other skills are often prioritized with training. In addition to training in the technical aspects of telehealth confidentiality, providers would benefit from skill-building around rapport and trust during a telehealth visit [44•], and this should be a routine part of medical school and residency training programs.
Setting expectations for parents and patients prior to and at the start of the telehealth visit can assist with negotiating time alone with the adolescent. Some authors suggest having parents log on to the visit with a different device in a different room, making it easier and more natural for the parent to log off when the portion including them is completed [32•, 44•]. Written expectations explicitly reviewing confidentiality and time alone with the provider could be sent electronically or via mail prior to the visit and could also include reassurance about the security of the electronic platform used.
At the start of the adolescent telehealth visit, providers should revisit expectations with patients and their caregivers and explicitly state that the telehealth platform being used protects their health information. Some patients access their telehealth visits at school, local libraries or in other public places; therefore, providers should ask the patients where they are at the start of the telehealth visit. Asking the patient for a 360-degree view of the space they are in can help providers verify who else may be in the space. Once the adolescent is alone with the provider, questions about their degree of privacy should be further explored and some authors suggest these questions be repeated several times during the visit. Patients may need assistance with identifying more private spaces, such as going to another room, outside or to a nonmoving car. If patients are on a computer or other device that cannot be moved, the visit could be transitioned to phone with or without video to allow for more mobility. If unable to confirm the adolescent is in a private space for confidential care, providers can utilize privacy-enhancing strategies such as asking patients to wear headphones while the provider asks yes/no questions or using the secure chat feature within the EHR platform to review confidential information. Providers should ensure that the chat is not visible to others and is deleted prior to return of patient’s parent if private/confidential information is disclosed that way. Finally, asynchronous communication via the patient’s EHR patient portal can be used for sharing private/confidential information including sending questionnaires that ask confidential questions as long as the patient portal is only accessed by the adolescent [6, 8•, 9•, 10•, 32•].
The unique challenge of physical examination, especially when addressing sensitive symptoms has been managed via several strategies including uploading photos to the secure patient portal or sending images or confidential messages to the provider that are encrypted in some way. Patients requiring more evaluation or testing could be referred to local labs for testing or to a closer provider for visual examination [6, 8•]. The option to mail testing kits to adolescents for pregnancy or STI screening has also been proposed as an option [8•] although confidentiality may be challenging if mail delivery is accessible to all household members. If patients require confidential prescriptions, providers need to ask about transportation to the pharmacy as well as be mindful that the automated pharmacy notification system may be defaulted to the parents phone or email. Alternatively, referral to nearby Title X facilities, school based health centers, local health department clinics, a different pharmacy or home delivery of medications may be necessary. Identifying the means by which the adolescent can reach the provider for follow-up confidential questions after the visit also requires attention prior to disconnecting from the telehealth visit.
After the telehealth visit, closing the confidentiality loop is critical. This includes ensuring visit notes containing confidential information are marked as “sensitive” or “confidential” and are blocked from release to the patient portal if viewing by individuals other than the patient is a risk. Filtering information by diagnosis, medication or lab testing has been used by institutions to prevent release of confidential information [24, 26, 31]. Given the evolving regulatory landscape surrounding telehealth visits, reimbursement mechanisms for confidential telehealth visits should be verified prior to the visit to avoid direct billing if the visit is not covered by insurance or if explanation of benefits pose a risk for confidentiality breach.
Increasing access to confidential care through telehealth has been cited as a means to improve equity in health care. However, the expanded use during the pandemic also introduced equity issues unique to telehealth. While most adolescents appear to have access to a mobile device, their access to a high-quality telehealth experience may be diminished by insufficient wifi access, crowded home environments, language barriers, and limited technological literacy [32•]. These issues require institutional and community support to be adequately addressed. Parents surveyed about their experience also recommended adolescent and parental involvement in developing workflows and educational opportunities about telehealth use that can be offered in clinics, libraries, schools, and other public spaces [48]. The American Academy of Pediatrics provides educational videos for patients and parents that demonstrate telehealth use and specifically how privacy and confidentiality can be preserved; although they are currently only offered in English [49]. More innovative approaches to telehealth access such as soundproof telehealth kiosks located in reachable community locations [6] may also narrow the gap in equitable access to care that the pandemic accentuated.
Conclusion
While access to confidential care for adolescents is challenged by multiple barriers, widespread use of telehealth during the pandemic demonstrated that telehealth access may improve access. Adolescents and parents endorse the importance of confidentiality as a routine part of adolescent healthcare and can help inform best practices in this area. Multiple strategies to protect adolescent confidentiality in the telehealth setting were explored and evaluated during the pandemic. However, implementation of these strategies designed to preserve confidentiality across the telehealth visit continuum requires institutional, practice, and provider investment and engagement. Providers and staff would benefit from increased institutional and IT support as well as training in skills essential to the provision of confidential care and specifically the unique dynamics of the telehealth visit. Organizational and public policies should incorporate the elements needed to maintain confidentiality across the telehealth visit continuum to enable equitable access to high quality, comprehensive healthcare for all adolescents.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly Converting to "Virtual Practices": Outpatient Care in the Era of COVID-19. In: NEJM Catalyst. 2020. https://catalyst.nejm.org/doi/abs/10.1056/CAT.20.0091. Accessed 10 Mar 2023.
Patel PD, et al. Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: barriers, solutions, results. J Am Med Inform Assoc. 2020;27(7):1116–20. https://doi.org/10.1093/jamia/ocaa065.
Omboni S, et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health. 2022;1:7–35. https://doi.org/10.20517/ch.2021.03.
Demeke HB, et al. Trends in use of Telehealth among health centers during the COVID-19 pandemic - United States June 26-November 6 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):240–4. https://doi.org/10.15585/mmwr.mm7007a3.
Villanti AC, Johnson AL, Ilakkuvan V, Jacobs MA, Graham AL, Rath JM. Social media use and access to digital technology in US young adults in 2016. J Med Internet Res. 2017;19(6):e196. https://doi.org/10.2196/jmir.7303.
Evans YN, Golub S, Sequeira GM, Eisenstein E, North S. Using telemedicine to reach adolescents during the COVID-19 pandemic. J Adolesc Health. 2020;67(4):469–71. https://doi.org/10.1016/j.jadohealth.2020.07.015.
North S. Telemedicine in the time of COVID and beyond. J Adolesc Health. 2020;67(2):145–6. https://doi.org/10.1016/j.jadohealth.2020.05.024.
• Barney A, Buckelew S, Mesheriakova V, Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. 2020;67(2):164–71. https://doi.org/10.1016/j.jadohealth.2020.05.006. Barney et al were among the first to publish and share their experiences with rapid implementation of telehealth early on during the COVID-19 pandemic. They shared pitfalls and strategies that helped guide future research and implementation as practices worldwide initiated telehealth visits to preserve patient access during critical times throughout the pandemic.
• Wood SM, et al. Outcomes of a rapid adolescent Telehealth scale-up during the COVID-19 pandemic. J Adolesc Health. 2020;67(2):172–8. https://doi.org/10.1016/j.jadohealth.2020.05.025. Wood et al provide one of the first descriptive analyses of the experience with implementation of telehealthcare in an adolescent medicine specialty clinic. They provide data relating to show rates as well as demographics and diagnoses of patients seen using telehealth. They also provide a detailed table with specific examples of patient encounters sharing the challenges they faced, the problem-solving strategies used to address these challenges and the clinical outcome following these visits.
• Carlson JL, Goldstein R. Using the electronic health record to conduct adolescent Telehealth visits in the time of COVID-19. J Adolesc Health. 2020;67(2):157–8. https://doi.org/10.1016/j.jadohealth.2020.05.022. This commentary by Carlson and Goldstein describes their experience with implementation of telehealth visits with a lens on the limitations and challenges the electronic health record systems present. They specificially discuss the confidential visit and some of the solutions to allow providers to be able to deliver confidential care.
Totten AM, Womack DM, Eden KB, McDonagh MS, Griffin JC, Grusing S, Hersh WR. Telehealth: mapping the evidence for patient outcomes from systematic reviews. technical brief no. 26. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2015-00009-I.) AHRQ Publication No.16-EHC034-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2016. www.effectivehealthcare.ahrq.gov/reports/final.cfm.
How to plan and conduct telehealth consultations with children and adolescents and their families. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO.
Confidentiality in Adolescent Health Care: ACOG Committee Opinion, Number 803. Obstet Gynecol. 2020;135(4):e171–e177. https://doi.org/10.1097/AOG.0000000000003770.
Ford CA, English A, Sigman G. Confidential health care for adolescents: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2004;35(2):160–7. https://doi.org/10.1016/j.jadohealth.2004.03.002.
Coble YD, Estes EH, Head CA, et al. Confidential Health Services for Adolescents. JAMA. 1993;269(11):1420–4. https://doi.org/10.1001/jama.1993.03500110088042.
Marcell AV, Burstein GR, AAP Committee on Adolescence. Sexual and Reproductive Health Care Services in the Pediatric Setting. Pediatrics. 2017;140(5):e20172858.
English A, Bass L, Dame BA, Eshragh F. State Minor Consent Laws: A Summary. 3rd ed. Chapel Hill, NC: Center for Adolescent Health and the Law; 2010.
English A, Ford CA. The HIPAA privacy rule and adolescents: legal questions and clinical challenges. Perspect Sex Reprod Health. 2004;36(2):80. https://doi.org/10.1363/psrh.36.80.04.
Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CEJ. Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized controlled trial. JAMA. 1997;12:1029–34.
Fuentes L, Ingerick M, Jones R, Lindberg L. Adolescents’ and young adults’ reports of barriers to confidential health care and receipt of contraceptive services. J Adolesc Health. 2018;62(1):36–43. https://doi.org/10.1016/j.jadohealth.2017.10.011.
Grilo SA, et al. Confidentiality discussions and private time with a health-care provider for youth, United States, 2016. J Adolesc Health. 2019;64(3):311–8. https://doi.org/10.1016/j.jadohealth.2018.10.301.
Jones RK, Purcell A, Singh S, Finer LB. Adolescents’ reports of parental knowledge of adolescents’ use of sexual health services and their reactions to mandated parental notification for prescription contraception. JAMA. 2005;293(3):340–8. https://doi.org/10.1001/jama.293.3.340.
Gilbert AL, Rickert VI, Aalsma MC. Clinical conversations about health: the impact of confidentiality in preventive adolescent care. J Adolesc Health. 2014;55(5):672–7. https://doi.org/10.1016/j.jadohealth.2014.05.016.
Gray SH, Pasternak RH, Gooding HC, Woodward K, Hawkins K, Sawyer S, Anoshiravani A, Medicine, et al. Recommendations for electronic health record use for delivery of adolescent health care. J Adolesc Health. 2014;54(4):487–90. https://doi.org/10.1016/j.jadohealth.2014.01.011.
Bravender T, et al. Physicians’ assurances of confidentiality and time spent alone with adolescents during primary care visits. Clin Pediatr (Phila). 2014;53(11):1094–7. https://doi.org/10.1177/0009922813512022.
Committee on Adolescence; Council on Clinical and Information Technology; Blythe MJ, Del Beccaro MA. Standards for health information technology to ensure adolescent privacy. Pediatrics. 2012;130(5):987–90. https://doi.org/10.1542/peds.2012-2580.
• Xie J, et al. Ensuring adolescent patient portal confidentiality in the age of the Cures Act Final Rule. J Adolesc Health. 2021;69(6):933–9. https://doi.org/10.1016/j.jadohealth.2021.09.009. Xie at al describe an elegant quality improvement initiative at their institution aimed at identifying patient portal access for adolescents that may be compromised due to parents or others having access to the patient portal. The study shows how pervasive inappropriate access to adolescent patient portals is and presents a model for addressing this problem at an institutional level.
Sharko M, Wilcox L, Hong MK, Ancker JS. Variability in adolescent portal privacy features: how the unique privacy needs of the adolescent patient create a complex decision-making process. J Am Med Inform Assoc. 2018;25(8):1008–17. https://doi.org/10.1093/jamia/ocy042.
Bourgeois FC, DesRoches CM, Bell SK. Ethical challenges raised by OpenNotes for pediatric and adolescent patients. Pediatrics. 2018;141(6):20172745–12236.
Stablein T, Loud KJ, DiCapua C, Anthony DL. The catch to confidentiality: the use of electronic health records in adolescent health care. J Adolesc Health. 2018;62(5):577–82. https://doi.org/10.1016/j.jadohealth.2017.11.296.
Carlson J, Goldstein R, Hoover K, Tyson N. NASPAG/SAHM statement: the 21st Century Cures Act and Adolescent Confidentiality. J Pediatr Adolesc Gynecol. 2021;34(1):3–5. https://doi.org/10.1016/j.jpag.2020.12.015.
• Davidson SK, Sanci L, de Nicolas Izquierdo C, Watson CJ, Baltag V, Sawyer SM. Best practice during teleconsultations with adolescents: a scoping review. J Adolesc Health. 2022;70(5):714–28. https://doi.org/10.1016/j.jadohealth.2021.11.012. This review examined exisiting literature describing and/or evaluating telehealth use with adolescents. The review describes all aspects of telehealth care, including some discussion of confidentiality and more importantly viable solutions for preserving this essential part of the adolescent visit when delivering care via telehealth.
Goldstein F, Glueck D. Developing rapport and therapeutic alliance during telemental health sessions with children and adolescents. J Child Adolesc Psychopharmacol. 2016;26(3):204–11. https://doi.org/10.1089/cap.2015.0022.
VonHoltz LAH, Frasso R, Golinkoff JM, Lozano AJ, Hanlon A, Dowshen N. Internet and social media access among youth experiencing homelessness: mixed-methods study. J Med Internet Res. 2018;20(5):e184. https://doi.org/10.2196/jmir.9306.
American Academy of Pediatrics. Guidance on providing pediatric ambulatory services via telehealth during COVID-19. In: Critical Updates on COVID. 2020. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections2/guidance-on-providing-pediatric-ambulatory-services-via-telehealth-during-covid-19/. Accessed 10 March 2023.
Curfman A, et al. Telehealth: opportunities to improve access, quality, and cost in pediatric care. Pediatrics. 2022;149(3):e2021056035. https://doi.org/10.1542/peds.2021-056035.
• Wood SM, et al. Acceptability, feasibility, and quality of telehealth for adolescent health care delivery during the COVID-19 pandemic: cross-sectional study of patient and family experiences. JMIR Pediatr Parent. 2021;4(4):e32708. https://doi.org/10.2196/32708. Wood et al expand on their previous publication of telehealth implementation by evaluating the patient experience through a survey and interviews of adolescents and caregivers. This was the first study of this size specifically examining adolescent and caregiver acceptance of telehealth as well as challenges, such as technical difficulties or concerns about privacy. Adolescent and caregiver responses endorse telehealth as an acceptive care delivery option but also highlight limitations particularly adolescents' concerns about privacy. The authors offer some creative solutions to further optimize this care delivery model.
Moorman LK. COVID-19 pandemic-related transition to telehealth in child and adolescent mental health. Fam Relat. 2022;71(1):7–17. https://doi.org/10.1111/fare.12588.
Hurtado ACM, Crowley SM, Landry KM, Landry MS. Telehealth contraceptive care in 2018: a quality improvement study of barriers to access and patient satisfaction. Contraception. 2022;112:81–5. https://doi.org/10.1016/j.contraception.2022.02.011.
Gessner M, Seeland G, Gonzalez DA, Dietrich JE. Telehealth Care in a Pediatric and Adolescent Gynecology Clinic During the COVID-19 Pandemic. J Pediatr Adolesc Gynecol. 2023;36(3):280–3. https://doi.org/10.1016/j.jpag.2022.12.003.
Hubach RD, O’Neil AM, Stowe M, Hamrick J, Giano Z, Currin JM. Preferred methods of HIV and sexually transmissible infection screening delivery among a rural sample of men who have sex with men. AIDS Patient Care STDS. 2020;34(11):470–6. https://doi.org/10.1089/apc.2020.0170.
Damian AJ, Stinchfield K, Kearney RT. Telehealth and beyond: promoting the mental well-being of children and adolescents during COVID. Front Pediatr. 2022;10(793167):2022. https://doi.org/10.3389/fped.2022.793167.
Carretier E, Bastide M, Lachal J, et al. Evaluation of the rapid implementation of telehealth during the COVID-19 pandemic: a qualitative study among adolescents and their parents. Eur Child Adolesc Psychiatry. 2023;32:963–73. https://doi.org/10.1007/s00787-022-02108-1.
• Allison BA, Rea S, Mikesell L, Perry MF. Adolescent and parent perceptions of telehealth visits: a mixed-methods study. J Adolesc Health. 2022;70(3):403–13. https://doi.org/10.1016/j.jadohealth.2021.09.028. This mixed methods study examines the adolescent and parent experience with telehealth using surveys and interviews. The authors specifically examine how the therapeutic alliance with the provider impacts satisfaction with the visit and perceived privacy and confidentiality during the visit. The findings suggest that the therapeutic alliance mediates perceived privacy and confidentiality indicating that telehealth implementation requires provider-patient relationship building in addition to more than logistical strategies to ensure adolesents experience the level of privacy and confidentiality they need.
Diaz MF, et al. Providing contraceptive health services to adolescents and young adults by telemedicine: a scoping review of patient and provider perspectives. J Pediatr Adolesc Gynecol. 2022;35(5):575–84. https://doi.org/10.1016/j.jpag.2022.05.003.
• Gilkey MB, Kong WY, Huang Q, Grabert BK, Thompson P, Brewer NT. Using telehealth to deliver primary care to adolescents during and after the COVID-19 pandemic: national survey study of US primary care professionals. J Med Internet Res. 2021;23(9):31240. https://doi.org/10.2196/31240. This national survey is the largest of its kind to describe primary care provider experiences with delivery of telehealthcare to adolescents during and after the pandemic. Findings indicate that providers see telehealthcare as a viable option even after the pandemic and suggest that offering it as an option to adolescents can improve access and reduce elements of stress to patients and families when attending visits in-person.
Goldstein RL, Anoshiravani A, Svetaz MV, Carlson JL. Providers’ perspectives on adolescent confidentiality and the electronic health record: a state of transition. J Adolesc Health. 2020;66(3):296–300. https://doi.org/10.1016/j.jadohealth.2019.09.020.
Kodjebacheva GD, Tang C, Groesbeck F, Walker L, Woodworth J, Schindler-Ruwisch J. Telehealth use in pediatric care during the COVID-19 pandemic: a qualitative study on the perspectives of caregivers. Children Basel. 2023;10(2):311. https://doi.org/10.3390/children10020311.
American Academy of Pediatrics. Promoting telehealth campaign toolkit. In: Campaigns & Toolkits. 2023. https://www.aap.org/en/news-room/campaigns-and-toolkits/promoting-telehealth/. Accessed 10 Mar 2023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author did not receive support from any organization for the submitted work. The author has no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Perry, M.F. Confidential Telehealth Care for Adolescents: Challenges and Solutions Identified During the COVID-19 Pandemic. Curr Pediatr Rep 11, 78–85 (2023). https://doi.org/10.1007/s40124-023-00288-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-023-00288-1