Abstract
Purpose of Review
Review building of programs to eliminate Toxoplasma infections.
Recent Findings
Morbidity and mortality from toxoplasmosis led to programs in USA, Panama, and Colombia to facilitate understanding, treatment, prevention, and regional resources, incorporating student work.
Summary
Studies foundational for building recent, regional approaches/programs are reviewed. Introduction provides an overview/review of programs in Panamá, the United States, and other countries. High prevalence/risk of exposure led to laws mandating testing in gestation, reporting, and development of broad-based teaching materials about Toxoplasma. These were tested for efficacy as learning tools for high-school students, pregnant women, medical students, physicians, scientists, public health officials and general public. Digitized, free, smart phone application effectively taught pregnant women about toxoplasmosis prevention. Perinatal infection care programs, identifying true regional risk factors, and point-of-care gestational screening facilitate prevention and care. When implemented fully across all demographics, such programs present opportunities to save lives, sight, and cognition with considerable spillover benefits for individuals and societies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
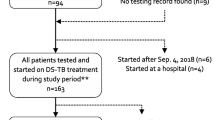
Herein, we present an introduction to, and an overview and review of work [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 51•, 52•, 53••, 54, 55••, 56••, 57•, 58••, 59•, 60••, 61, 62••, 63•, 64••, 65, 66••, 67••, 68••, 69, 70, 71••, 72••, 73••, 74••, 75••, 76,77,78, 79••, 80••, 81••, 82, 83, 84••, 85••, 86••, 87,88,89,90,91,92,93,94,95,96,97,98, 99••, 100••, 101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119, 120••, 121••, 122••, 123••, 124••, 125••, 126••, 127••, 128••, 129••, 130, 131, 132••, 133••, 134,135,136,137, 138••, 139, 140••, 141, 142••, 143,144,145,146,147,148,149,150,151] to provide a basis for public health programs addressing toxoplasmosis. Students began by reviewing pertinent, available literature which is summarized in part in Tables 1, 2, 3 and references [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 51•, 52•, 53••, 54, 55••, 56••, 57•, 58••, 59•, 60••, 61, 62••, 63•, 64••, 65, 66••, 67••, 68••, 69, 70, 71••, 72••, 73••, 74••, 75••, 76,77,78, 79••, 80••, 81••, 82, 83, 84••, 85••, 86••, 87,88,89,90,91,92,93,94,95,96,97,98, 99••, 100••, 101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119, 120••, 121••, 122••, 123••, 124••, 125••, 126••, 127••, 128••, 129••, 130, 131, 132••, 133••, 134,135,136,137, 138••, 139, 140••, 141, 142••, 143,144,145,146,147,148,149,150,151] with commentary about each manuscript for this Review. This initially was focused, as reviewed here, on work in France, Austria, the USA, Brazil, and Colombia (Fig. 1). Student-generated research then contributed to this initiative, which encompassed three different countries including Panama, Colombia and the USA, seven different educational levels (high school, university, medical school, residency, graduate school, post-graduate, practicing physicians and scientists), patients of all educational backgrounds, and more than a dozen institutions. Each individual research project generated useful data and discussions at poster sessions and presentations that utilized and then updated our body of research. In addition, each student’s work provided original information concerning a certain aspect of toxoplasmosis and its prevention and treatment, which could then be expanded upon by other groups in the USA, Panama, Colombia, and other countries (e.g., Brazil, France, Morocco). For example, there were six groups of US students and additional in-country students, scientists, and practitioners who, over the course of eight years, devised and updated spatial epidemiologic analyses of Toxoplasma seroprevalence and risk factors in Panama and Colombia. Some of this work provided a foundation for and part was incorporated into now published, relevant work [41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 52•, 53••, 54, 55••, 56••, 57•, 59•, 62••, 63•, 65]. As a fundamental part of our global initiative, students have established new routes of communication between multiple academic and medical institutions. Together, we have created a tradition of, and paradigm for, research contributions that can be passed down and modified by new generations who take an interest in our expanding toxoplasmosis initiative. This introduction is the first in a series of four papers, which describe work begun in Panama in 2014 to build a comprehensive public health program (Fig. 1). This initiative is structured to provide education, information, and improvements meant to benefit healthcare centered around eliminating toxoplasmosis. The importance of exposure to oocyst contaminated water sources and soil became apparent from this and other work (Fig. 2) [57•, 62••, 63•, 64••, 65, 77, 99••].
“Toxoplasmosis” refers to the disease caused by the protozoan parasite Toxoplasma gondii [138••]. The parasite can be acquired through a variety of pathways; while a common way of acquisition is ingestion of tissue cysts found in raw or undercooked meat, Figure 2 demonstrates how oocysts can also be transmitted via feces from cats, which are T. gondii’s natural host, as well as through water and soil cycles [64••, 138••].
Toxoplasma
is acquired congenitally when a pregnant woman contracts the parasite for the first time, which is marked by seroconversion including IgM and IgG antibodies. About 8 weeks after infection, serum IgM antibody levels usually decrease, while IgG levels become high and stable, as measured by the Sabin Feldman dye test. This pattern of test results signals subacute/chronic infection, indicating that the individual is now partially immune to subsequent infection. With established maternal seropositivity prior to pregnancy, the fetus usually is not at risk for congenital toxoplasmosis (CT). IgG antibodies persist for life, so their presence in serum is a marker of either acute or chronic infection with the parasite. Meanwhile, IgM antibodies might signify a case of recent infection, in which parasite tachyzoites may be vertically transmitted to the fetus. This can result in ocular and neurologic damage—such as chorioretinitis, loss of sight, psychomotor impediments, seizures, microcephaly, hydrocephalus, and intracranial calcifications, among other manifestations—as well as prematurity and pregnancy loss [71••, 79••, 137]. As multiple studies have observed, the best way to prevent these adverse effects is through prompt diagnosis and treatment of acutely infected mothers; this can greatly decrease risk of mother-to-child transmission and overall damage the parasite can do if it manages to cross the placenta [4••, 6••, 14••, 71••].
The devastating effects of toxoplasmosis—especially the congenital form—are well documented. However, despite decades of estimates of disease burden—such as a 2013 World Health Organization report on CT—the actual prevalence of toxoplasmosis is generally not well defined, even in countries with some of the highest estimated rates of infection [141]. The starting point for the present study described herein is Panama, one of many tropical and sub-tropical countries where high prevalence and severe overall disease burden have been noted. While there are few current published results on the seroprevalence of T. gondii in Panama, a previous study estimated that this country has one of the highest rates of Toxoplasma infection in Latin America, with a seroprevalence of 50% in 10-year-olds and 90% in 60-year-olds [142••]. Additionally, the neighboring countries of Colombia and Costa Rica have estimated seroprevalences of 43–67% and 49-61%, respectively [143,144,145,146,147]. When it comes to the congenital form of toxoplasmosis in Panama, estimated annual incidence is 1.8 cases per 1000 live births, and the estimated number of disability-adjusted life-years (DALYs), i.e., loss of the equivalent of one year of full health, resulting from congenital infection is 840 [141]. With this high seroprevalence and significant burden, Panama would be expected to have a significant risk for the development of congenital and ocular toxoplasmosis. Toxoplasmosis has traditionally been a neglected disease in Panama, despite significant morbidity and mortality. Given this need, a team of scientists, physicians, and students from Panama, Colombia, and the USA —known as “Team Panama” —made an effort to establish a healthcare program in Panama that could reduce the adverse impacts of this infection. In this paper, we describe the multiple facets of our public health project: building educational programs and understanding regional prevalence of toxoplasmosis, evaluating the efficacy of a mandate to screen for and report CT, studying risk factors for toxoplasmosis, building spatial epidemiology maps, creating mathematical models to predict risk, and improving availability of care for symptomatic illness, among other items. We also describe some of our parallel projects in neighboring Colombia, a country that has a more robust mandatory gestational screening program for CT, and in the United States, where a large part of our research is based. We conclude with an evaluation of our research and initiatives and comments on the next steps to take to improve care for toxoplasmosis (especially the congenital form) in all three countries.
Review of Foundational Studies and Updates Concerning Clinical Manifestations of Congenitally Infected Children and Treatment in Programs in France, Austria, the USA, Brazil, Colombia and Morocco
France, Austria
The important work from France [46•, 51•, 52•, 56••, 60••, 62••, 66••, 67••] and Austria [53••] with some data from the USA [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 51•, 52•, 53••, 54, 55••, 56••, 57•, 58••, 59•] has demonstrated that congenital toxoplasmosis is a treatable and preventable disease. Like other infectious diseases the sooner treatment is initiated the better the outcome.
The cost benefit analyses emphasize that treatment brings not only reduction in individual suffering but also brings substantial cost savings for countries (e.g., 14 fold in Austria [53••]). The major role France has had in developing this improved approach that saves life, sight, and cognition is represented also in Fig. 3. As this has been addressed in earlier publications [46•, 51•, 52•, 53••, 56••, 60••, 62••, 66••, 67••], it is not considered in more depth here. Many of the problems faced in the USA are avoided in France and Austria where prices for medicines are mandated by the government, social systems support medical care evenly for all those in the countries, and prenatal screening and reporting for toxoplasmosis are required by law.
United States
In the United States, an ongoing longitudinal study called the National Collaborative Chicago-based Congenital Toxoplasmosis Study (NCCCTS) was initiated in 1981 and continues into the present time. Methodology has been presented in ongoing reports throughout that time. Methodology has included obtaining information about this infection, its epidemiology, diagnosis, treatment and outcomes (Tables 1, 2 and 3) [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 51•, 52•, 53••, 54, 55••, 56••, 57•, 58••, 59•]. Results are compared with earlier studies [70, 71••]. Initially treatment dosing for infants were established in a phase 1 clinical trial, then with feasibility and safety and favorable outcomes identified, a randomized controlled trial compared higher and lower doses. In this context and with participants who missed treatment during the first year of life, all these families were then observed, carefully documenting outcomes across lifetimes. Methodology for treatment beginning in gestation also has been established with and extended by French colleagues making a model paradigm for care and prevention of sequalae by promptly treating the seroconverting pregnant woman and the fetus followed by treatment in the first year of life [33••].
Results from work in the United States have been published in individual manuscripts [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 52•, 55••, 56••] but not with a composite overview in some time. This data set is included herein in a not previously published composite form in a table with comments that summarize some of the major earlier and more recently updated findings in the context of others’ work (Tables 1, 2 and 3; Figs. 3-5, Part I Supplement) [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•, 51•]. Pyrimethamine, sulfadiazine, leucovorin, and spiramycin are essential for the treatment and prevention of congenital toxoplasmosis (CT) [17••, 33••, 46•, 48••, 53••, 60••, 65]. Through ongoing programs for care, the personal experience of the authors informed observations of availability of medicines in Panama and the United States. These observations were made in the context of building programs in each of these countries.
These studies demonstrate that in the United States most diagnoses are made at birth, or later, when significant clinical manifestations have already occurred (e.g., reference 33). Nonetheless, findings which should be sentinel markers of this disease often go unattributed to this infection resulting in unnecessary delays in diagnosis and treatment. As in the child in part B of Fig. 5, and others, prematurity, thrombocytopenia, small for gestational age, rule out sepsis, hepatocellular abnormalities, and meningitis often go undiagnosed as being caused by toxoplasmosis and the diagnosis is missed. This results in needed treatment not being given for months. This has resulted in irreparable damage that could have been prevented.
Prompt prenatal treatment in the United States, as in France and Austria, results in the best outcomes [17••, 33••, 46•, 48••, 53••, 60••, 65]. Outcomes with treatment postnatally also results in markedly better outcomes than earlier without treatment. Those data and analyses include an early phase 1 clinical trial (1981–1990), and later randomized trial (1990–present). Kaplan Meier analyses of the randomized trial with pre-specified endpoints in which a lower and a higher dosage of pyrimethamine were compared. Both treatments were predicted/selected to likely be efficacious based on the Phase 1 clinical study. Doses expected to be effective were utilized for equipoise, with the assumption that if differences from all past experience were found, efficacy would be proven, and perhaps a small dose response effect might be evident. There was not a significant difference in those outcomes for the higher and lower dose, but pre-specified outcomes for both were considerably better than prior studies where children were untreated or treated only for a month [88,89,90].
In infants who had not been treated in utero. there was greater severity at birth and more prematurity in those infected with non II parasite serotypes. In contrast, for infants who were treated in utero those differences associated with parasite strain (genetics) were not present at birth [33••]. Later outcomes were not different for those treated children with differing serotypes of parasites reflecting infection with different strain in these treated children [33••]. A comment prepared for a grant application by one of the NCCCTS neurologists and R. McLeod is included as follows, as it describes, in a different format, observations in the NCCCTS during these past 4 decades:
“My goal as a contributor to this study is to understand the consequences of Toxoplasma infection across life, particularly as this infection affects the brain. I am an expert in Pediatrics, Child Neurology and Developmental Pediatrics. I have served as [one of] the primary neurologist [s] in this study for the evaluation of the neurologic status of the study patients since the inception of this study in 1981. I have evaluated most of the families involved in this study and I have enjoyed this work immensely. I have watched this symptomatic newborn disease transition from one that was assumed to always have a bleak prognosis at birth to one that many times is associated with good outcomes. It has also been fascinating to watch the development of understanding better management and pathogenesis of the infection. The many contributions our work has made to this understanding, and to define the next frontiers for both treatment and deciphering pathogenesis of this disease has been gratifying. It has been extremely rewarding to observe such children move on to University, to productive work and to beginning their own families, all unexpected outcomes at the outset of this work in 1981. (CNS)”
Examples of physician resistance to considering possible benefit from shunt placement and potential good outcomes are in Fig. 4 and in the Box). In some cases, the need for a ventriculoperitoneal shunt is clear with anatomy indicative of obstruction of the Aqueduct of Sylvius with a dilated third ventricle and lateral ventricles, head circumference crossing percentiles and a full anterior fontanelle, and even then there sometimes is resistance to shunt placement. Drainage made through creating a small orifice at lower surface of the third entricle so it drains in the basilar cistern called a third ventriculostomy work less well with risk from inflammatory cerebrospinal fluid after anti-parasitic medicines are discontinued. In some cases where there is less obvious, clear potential benefit, and anatomy associated with an inflammatory, fibrotic pathogenesis without aqueductal obstruction, the approach we have used is summarized in this paraphrased comment by one of the NCCCTS neurosurgeons. This experience is also presented in the manuscript by McLone et al [50•] and in Fig. 4 [50•] with permission:
“The shunt may help your child and one can only know by placing it and seeing if it does. No one can predict that and there are no guarantees but it is a hope that it will help him/her and we will all be fortunate if that happens. There are always risks but these are not uniquely worse for your child and not inevitable. Without the shunt your child will not have that chance. (DMc. DF, RP, RMc and more recently P. Das and J Ruge)”
Box Update: Some strengths, benefits, and problems in access to, implementation, and understanding of the importance of various treatment options identified and exemplified in the following recent patient experiences/cases below: Case 1: Infants who received treatment from large bottles of pyrimethamine and sulfadiazine stored for longer than one week developed severe and prolonged neutropenia. These are suspensions rather than solutions. They sediment and congeal resulting in under and overdosing. Medicines should be in 25ml bottles and made fresh each week adjusting dosages for the child’s weight. Case 2: Patient in USA was exposed to Toxoplasma in utero. The patient was treated in the first year of life and has done well. At the age of 16 years she developed a peripapillary lesion medial and superior to the optic disc with considerable fluid, cells and loss of visual acuity. Treatment with pyrimethamine and sulfadiazine with leucovorin led to resolution. Duration of treatment was for many months. Treatment is continued until lesions become quiet and resolve and then for several more weeks. It is not a disease where duration can be specified as a consistent, uniform length of time but rather depends on the patient’s clinical status. See Figure 5e and also Supplemental Figure 5. Azithromycin is used for suppression after complete resolution of active disease when frequent recurrences are in areas that are vision threatening, especially for patients whose vision is significantly impaired in one or both eyes. Azithromycin obviates the problem of hypersensitivity to sulfonamides that occurs from less effective trimethoprim/sulfamethoxazole. Failures of treatment of active disease with trimethoprim/sulfamethoxazole are not infrequent. Trimethoprim/sulfamethoxazole plus clindamycin has been used a few times when pyrimethamine was unavailable. Sulfadiazine has now been made available in Canada after a prolonged time when it could not be obtained there. Case 3: Patient from US developed congenital toxoplasmosis in utero. The disease advanced and resulted in significant cerebral edema. Neurosurgery was consulted for placement of a shunt but did not intervene until the disease was advanced. This case highlights that the problems in toxoplasmosis treatment are solvable. Greater interdisciplinary collaboration is needed across pediatricians, infectious disease providers, and neurosurgeons in order to improve patient care outcomes. A photo of the patient years after successful surgical intervention can be seen in Fig. 5. Case 4: 40-year-old body builder, took corticosteroids, presented with extensive encephalitis. He had steroid treatment and was found to have very low or no IgG, IgM, or IgA with this immunodeficiency a contributing cause. He developed sulfadiazine hypersensitivity, He initially responded to de-sensitization. But then developed a marked increase in liver function tests, some biliary sludge on ERCP, liver functions returned to near normal but then became elevated again. He was experiencing a slow neurologic rehabilitation when he developed inanition, and seizures and a cardiac arrest with unsuccessful attempts at resuscitation... Some severe illness due to Toxoplasma is associated with not previously recognized immune deficiency, genetic mutations or allelic variations in genes which confer susceptibility [47••, 117, 123••, 124••, 125••]. |
Examples of resolution of a large symptomatic retinal lesion in a teenager in the United States are shown in Figure 5. Treatment was continued beyond the time the lesion was fully resolved. The approach to treatment of recurrences is to promptly utilize pyrimethamine, sulfadiazine and leucovorin (PSL) (or with azithromycin instead of sulfadiazine if there is hypersensitivity to sulfonamides). These medicines (PSL) have demonstrated better efficacy in animal models, a correct ratio of constituents for synergy and a higher trough level of the anti-Dihydrofolate reductase component of the combination than trimethoprim sulfamethoxazole which has resulted in treatment failures.
If there is monocular vision and lesions in the better seeing eye near to the fovea, or with multiple recurrences, after complete resolution of activity, suppression with azithromycin has been used without further recurrences. Duration for such suppression is not established.
Azithromycin is used only when QT interval is normal, i.e., not prolonged. Trimethoprim sulfamethoxazole is not used for suppression because of the high frequency of hypersensitivity to sulfonamides which then precludes further use of the better sulfadiazine with pyrimethamine combination if there is another recurrence (please see above). A school aged child responded to clindamycin TMP/SMx but an older patient relapsed quickly [McLeod et al unpublished observations, 2022]. These medicines were used because of difficulty in obtaining pyrimethamine initially and are not the treatment of first choice.
Additional examples of ocular manifestations of Toxoplasmosis are presented in Supplement to Part 1 (Fatima Clouser Atlas, Part I, Supplemental) and at Toxoplasmosis.org. Others were presented earlier in other manuscripts and Atlases and book chapters [1••, 2, 3••, 4••, 5••, 6••, 7••, 8••, 9••, 10••, 11••, 12, 13, 14••, 15••, 16••, 17••, 18•, 19•, 20•, 21•, 22•, 23, 24••, 25, 26, 27•, 28•, 29, 30, 31•, 32•, 33••, 34•, 35•, 36, 37•, 38•, 39••, 40•, 41•, 42••, 43••, 44••, 45, 46•, 47••, 48••, 49, 50•].
Brazil and Colombia
The extensive well-organized work in Brazil and Colombia has been summarized recently [57•, 74••] and follows the same pattern of markedly improved outcomes in those who are treated. There have been comprehensive scholarly summaries of the programs for Brazil, that were completed earlier and recently [62••, 74••, 77, 151]. Brazil has played an important role both in clinical care on a large scale and in understanding parasite genetics as well as in basic and translational studies. Education programs in Brazil have included physician/scientists from Brazil, Europe, the United States, and Colombia with government sponsorship of programs for care. Collaborative work particularly in genetics and immunology/vaccines is included among the references herein and addressed in more depth in Part IV.
Morocco
Morocco has utilized gestational screening for decades according to the French model but not with monthly testing. A robust program to eliminate congenital toxoplasmosis has also been initiated with more frequent serologic screening [57•]. A thousand women have now been tested. Educational programs have been initiated. Epidemiologic studies like those described for Panama and Colombia have also been performed recently. There is an ongoing study of screening of thousands of pregnant women in two practice settings and a program to screen twenty thousand women in the poorer, high prevalence agricultural areas are under consideration as part of a government initiative.
Anti-parasitic treatments using medicines currently available in clinical practice: What is working and where are there problems?
As mentioned above, in France, Austria, and Brazil medicines are easily available and price is not an issue because of the countries’ policies on pricing and availability of medicines. In all the United States currently accessing medicines presents challenges. The recent history concerning the availability of medicines has influenced care for toxoplasmosis in the United States. In the United States in 2015, Turing Pharmaceuticals (now rebranded as Vyera Pharmaceuticals) acquired Daraprim (pyrimethamine), a medicine used to treat toxoplasmosis, and hiked the price by over 5000%, from $13.50 a pill to $750 for commercially insured patients. This caused substantial concern with broad criticism from the press and in senate hearings. The company defended the increase by stating that only a small percentage of patients had commercial insurance and for those uninsured medicine would have no charge (“penny pricing”), and that the profits gained from the price hike would be used to develop better treatments for toxoplasmosis and that patient co-pay would not be affected. Six years later, the cost of Daraprim has remained at $750 per pill with no public news of Vyera’s alternative toxoplasmosis medicine(s) since its approval to initiate a phase 1 study of a DHFR inhibitor in 2018. There are two candidate molecules with earlier phase studies but no public news as yet of their advancing for clinical use. The current pace of progressing medicines into clinical use for SARS-CoV-2 provides a stark contrast.
The history of pyrimethamine as a medicine is relevant: Pyrimethamine was discovered in the 1950s and has remained a major component of the treatment for toxoplasmosis throughout the subsequent decades. However, with only about 2000–8000 Americans recognized to be in need of this treatment annually, there was little incentive for other pharmaceutical companies to develop generic versions. As such, despite costing pennies to manufacture, companies like Turing/Vyera were able to increase the price by also enacting anti-competitive practices including tightly controlled distribution. As of October 2020, there are two additional generic versions of pyrimethamine, but the pricing has not been lowered significantly. Without insurance, this medicine is provided without charge. Only a relatively small percentage of the pyrimethamine is paid for by indemnity insurance and pre-approval can now involve substantial delays. Initially insurance coverage seemed to occur with relatively little difficulty and there was a robust assistance program and prompt distribution of medicines was possible. More recently, insurance company delays and refusals have made obtaining this medicine challenging for physicians, this has presented considerable difficulties in promptly providing emergent medicines for those who do not have 340B pharmacies. Such 340B pharmacies that can provide medicine at nominal or no cost while waiting for insurance coverage to be clarified (bridging the provision of medicines while waiting for medicines to be delivered) and for uninsured patients with no delays. These delays and difficulties can be harmful for patients. Bridging programs may help to remedy this in some instances. Hospitals with pharmacies that can provide medicines at low costs to patients who are medically indigent (340B pharmacies) can help with bridging when patients are registered there and some of these have obtained approvals to ship to patients in other states. For example, The University of Chicago is authorized to ship to California, New York, Georgia and Florida for patients registered at the University which can be accomplished following a telehealth appointment. Thus, they can assist patients in those locations. There are also pharmacy assistance phone numbers physicians can contact for assistance with obtaining medicines for the different companies with affiliated pharmacies. There is a charity that can assist patients also (phone numbers are available from Vyera “Daraprim Direct”). Unfortunately, as the charity provides support for many medicines, it is often depleted and runs out of resources early in each year. Therefore, it does not fulfill the desired goal throughout the year. Thus, obtaining medicines is feasible, even if substantial extra work for physicians, but has elements that currently do not function well. This information can allow patients and their physicians to know that proven treatments can be available to them, but it can be cumbersome, time consuming and result in delays or denials with insurance pre-approvals. There has been a recent anti-monopoly settlement with the FCC for multiple states and a patient class action lawsuit is pending.
While Vyera Pharmaceuticals has introduced programs, called “Daraprim Direct,” to help patients with financing their treatment plans, the price hike has clearly inflicted delays in obtaining medicines in urgent circumstances and suffering for Americans with toxoplasmosis. As described above, Daraprim Direct currently offers free medication to those uninsured and under 500 percent of the federal poverty level. Company coupons providing $10 monthly treatment regimens are also available for commercially insured patients whose insurance continues to deny coverage for this medicine when an appeal for a pre-authorization is submitted, as long as physicians continue the time-consuming appeal process. The limited distribution of Daraprim due to its cost creates other problems for patients, namely the lengthy wait times as physicians negotiate with insurance providers. Where treatment of emergent infection requires immediate attention, these delays can cause irremediable damage, such as loss of sight and death due to difficulty from diminished access. 340B pharmacies have provided medicines in emergencies, to be replenished when insurance allows so no patient suffers.
Finally, those under Medicare Part D face 31% copay due to Daraprim’s placement as a Tier V drug based on cost. Such patients, often under standard triple therapies such as prescriptions of Daraprim, Leucovorin, and sulfadiazine, face monthly fees of over $4000 for multi-month regimens that must often be repeated for reemergence of toxoplasmosis symptoms. Without the price hike, monthly fees would be merely $80 due to the comparatively lower prices of Leucovorin and sulfadiazine. As a result of these issues facing Daraprim prescription, some physicians choose to fall back to cheaper and less effective alternatives such as trimethoprim sulfamethoxazole or clindamycin, with two physicians recently trying the two together without any data to support this.
More recently, two additional companies gained approval for generic pyrimethamine but for a longwhile had chosen to continue to list the drug at prices nearly as high as the initial high price by Vyera Pharmaceuticals, rather than offering an affordable alternative. This has made access more complex with prior approvals, taking time and substantial delays.
As above at the University of Chicago, a system that permits prompt access for 340B pharmacies while providing bridge medicines, obviates some of these problems but it remains cumbersome and difficult to deal with pharmaceutical company preapprovals. Further problems with access and delays have become more pronounced with limitations in access to care during the SARS-CoV-2 pandemic (see representative cases, tabulated data in Tab 4, Box 1).
Very recently a pharmaceutical company called Oakrum began to sell pyrimethamine at ~$0.30 per 25 mg tablet which could mean that this resolves the problems associated with cost in the United States. It has not been possible at present to learn where this is manufactured or if there is any problem with quality or safety, or where the starting material (API) originates. If this is really a low-price tablet of high quality from a reliable source it could mean the treatment of this disease with optimal medicines will be feasible, straightforward and convenient again. It could lead competitor company prices to become comparable, and easily affordable
In Tables 4, 5, Box and Figs. 4, 5, we present approaches that have worked effectively where problems have arisen. These problems include loss of sight, inadequate access to neurosurgical shunt procedures, lack of recognition of well-known presenting manifestations of CT in neonatal Intensive Care Units, complications with laboratory access, and limited availability of prenatal care during the COVID-19 pandemic further complicating healthcare.
Spiramycin, used in the first trimester to prevent infections of the fetus, has been provided since the 1990s at no charge in the United States when it was cleared by Dr. McLeod, or the Remington Specialty Laboratory, and then the FDA. IRB approval is needed after the first emergency use for a practitioner. Benefit from this medicine particularly in the first 14 weeks of gestation recently was noted in a meta-analysis [68••]. This medicine has been available in Panama and Colombia commercially, as it is in Europe, Brazil, Argentina, and Guyana.
The National Collaborative Toxoplasmosis Study (NCCCTS) and other published materials provide guidelines for treatment which also are outlined in the manuscripts and book chapters on Management of congenital toxoplasmosis [60••, 65, 70, 71••, 72••, 73••] and updated and summarized herein (Fig. 1). The work of Mandelbrot et al [60••] indicates that prompt use of pyrimethamine and sulfadiazine can result in better outcomes after 15-weeks’ gestation for a small subset of infected fetuses [60••].
A. Model of Toxoplasma gondii transmission between domestic and wild felids, freshwater runoff, livestock, predatory and scavenger animals, marine mammals, bivalves and other invertebrates, and humans. This model is subject to change depending on the setting, but it presents a general overview of how Toxoplasma circulates through an ecosystem and suggests ways in which transmission to humans can be stopped or limited. Adapted from Van Wormer et al. B. Relationship of Toxoplasma transmission patterns to water and soil; designed by Jorge Gómez-Marin and Lilian Bahia Oliveira, also in McLeod et al. 2022.
Early studies in France, the United States, and Brazil demonstrated efficacy of treatment and shaped understanding of this disease. The images from France, those in the NCCCTS in the USA, and in Brazil represent the early chronology of this work, and show some of the investigators who worked on some of these studies. Special accomplishments of colleagues are noteworthy and have not been mentioned specifically. Since a number of those working on this study in the early years have died in the past two years with some posthumous authors they are mentioned specifically as follows: Paul Meier designed the first Toxoplasma RCT for congenital toxoplasmosis with colleagues in the NCCCTS. Michael Gottlieb’s guidance as a Program officer at NIAID was instrumental in the establishment of the NCCCTS and many aspects of development of treatments and vaccines to prevent this disease along with others continuing in this in the NIAID DMID program. Jean Hickman worked with them within NIAID. Eileen Stillwaggon worked on cost benefit analyses demonstrating predicted cost savings when there was diagnosis and treatment of congenital toxoplasmosis in the United States. In Austria she found fourteen-fold cost savings occurred. In France, early treatment in gestation has been found to be superior to treatment started after delays (Wallon, Stillwaggon, Sawyer et al 2022, In submission). Charles N Swisher was one of the primary neurologists in the NCCCTS working with this study from 1981 until his passing in 2020. Jack S Remington and his laboratory performed the serologic tests for this study and included findings from the NCCCTS in co-authored book chapters, with the work of his laboratory continuing with the study. Lazlo Stein developed the hearing testing protocols. The contributions of others either as authors or acknowledged are substantial as well. Each of these scientists, physicians, and others had an important role in the understanding and improvement in outcomes for this disease.
Restoration of anatomy and clinical improvement can occur with prompt treatment and placement of VP shunt. Third ventriculostomies often fail in this infection. A. Shows a recent photo (with permission) of a child whose first neurosurgeon was adamant about not shunting this child when he was an infant. The family sought care elsewhere had a ventriculoperitoneal shunt placed quickly and the child has done well. In just the first months of 2021 this scenario has repeated itself 5 times. Each time, except one infant in Guam, the children were shunted and all improved. B. Another example of an infant with a delay in shunting with a good response shown when an entricular peritoneal shunt was placed. His spinal cord lesions and associated signs are also resolving slowly although with developmental delays. C Figures from McLone et al reproduced with permission show the restoration of anatomy and better outcomes when needed shunts are placed without delay. Each aspect of care for this disease is urgent and emergent and should be treated as expectant for favorable outcome, recognizing this does not always occur but can and does on many occasions. Images reproduced with permission.
Retinal photographs and Optical Coherence Tomographic studies showing large active lesion with substantial edema (top) and then gradual near complete resolution with treatment with pyrimethamine, sulfadiazine and leucovorin and initially prednisone eye drops. This demonstrates that treatment should be initiated promptly, treatment should continue beyond resolution of the lesion, even large lesions can resolve almost entirely leaving only a small area of pigment, and no permanent detrimental change in visual acuity. An Atlas of retinal lesions is in the Supplemental, and also at toxoplasmosis.org, included herein with permission. The examples in the Atlas show the variability in appearance of lesions of toxoplasmic chorioretinitis.
There is an important distinction that is often overlooked in comparing data concerning prevention of CT in the literature in studies from France and work in the United States. In the United States, conception is dated from two weeks after the last menstrual period. Whereas in France, gestational week is counted from the onset of amenorrhea. Thus, in the literature from France, gestational age at which amniocentesis is performed is written as 17 weeks amenorrhea, this would be 15-weeks gestation in the United States. When dating of gestational age is considered the date of conception would be 2 weeks later than the onset of amenorrhea.
Parasite and Host Genetics
Serotyping assays have previously allowed us to distinguish infections caused by Type 2 strains from all other strains, collectively referred to as NE-II within the NCCCTS cohort [33••]. A new assay utilizing additional polymorphic peptides expands the utility of the earlier assay, and now resolves infection caused by Type 1, 2, 3, haplogroup 12 and non-archetypal parasites [148, 149]. This expands the utility of the earlier methodology used in the NCCCTS cohort and makes it possible to determine the strains causing infections in regions of the world where Toxoplasma genotypes are more heterogenous, as found in Colombia and Panama. Furthermore, limited genotyping studies performed on a few clinical samples within the USA by Pomares et al [150] suggest that type 1, 2, 3, and haplogroup 12 parasites dominate and cause illness in patients in the United States, providing the impetus to re-serotype the NCCCTS cohort with the new assay. Additional host susceptibility genes have also been identified (Tables 1, 2 and 3) [47••, 123••, 124••].
Conclusions
As reviewed herein, a great deal has been learned about optimal diagnosis and management from work in France, Austria and the USA Work in Brazil [152, 153••, 154], Colombia, and Morocco added substantially to this in recent decades (as also reviewed elsewhere comprehensively recently [57•,65, 74••]. In some cases, the need for a ventriculoperitoneal shunt is clear with anatomy indicative of obstruction of the Aqueduct of Sylvius with a dilated third ventricle and lateral ventricles, head circumference crossing percentiles and a full anterior fontanelle, and even then there sometimes is resistance to shunt placement. However, benefits of ventriculoperitoneal shunt to treat ventricular dilatation are considerable, as are benefits from using available medicines promptly to treat active disease for pregnant women, those immunocompromised, and for those with ocular disease.
Recent data and updated clinical experiences demonstrate that treatment for this disease when it is active should be considered to be emergent with outcomes expectant to be favorable at the outset. Recent progress to make screening easier and less expensive in France, Austria, and the United States, to detect Toxoplasma infection acquired in gestation and to facilitate prompt emergent treatment, is considered in depth in part IV of this series of manuscripts. Some solutions concerning costs and current conditions concerning medicines are also considered. Parts II, III, and IV of this series address individual topics in building these programs, the role of contamination of water sources and the environment. They provide detail concerning educational interventions (II), risk factors (III), and public health (IV).
Change history
06 November 2022
Open Access funding information has been added in the Funding Note.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Mcleod R, Mack DG, Boyer K, Mets M, Roizen N, Swisher C, Patel D, Beckmann E, Vitullo D, Johnson D, et al. Phenotypes and functions of lymphocytes in congenital toxoplasmosis. J Lab Clin Med. 1990;116(5):623–35 Parasite specific unresponsiveness in tests of cell mediated immunity in US children with congenital toxoplasmosis.
McGee T, Wolters C, Stein L, Kraus N, Johnson D, Boyer K, Mets M, Roizen N, Beckman J, Meier P, Swisher C, Holfels E, Withers S, McLeod R. Absence of sensorineural hearing loss in treated infants and children with congenital toxoplasmosis. Otolaryngol Head Neck Surg. 1992;106(1):75–80 Identifies that in the US in treated children sensorineural hearing loss is very rare.
•• Mcleod R, Mack D, Foss R, Boyer K, Withers S, Levin S, Hubbell J. Levels of pyrimethamine in sera and cerebrospinal and ventricular fluids from infants treated for congenital toxoplasmosis. Toxoplasmosis Study Group. Antimicrob Agents Chemother. 1992;36(5):1040–8 Presents pyrimethamine pharmacokinetics in infants and children and that treatment can be used safely in the first year of life. Outcomes for some children were markedly better than for comparable children in prior literature.
•• McAuley J, Boyer KM, Patel D, Mets M, Swisher C, Roizen N, Wolters C, Stein L, Stein M, Schey W, Remington J, Meier P, Johnson D, Heydemann P, Holfels E, Withers S, Mack D, Brown C, Patton D, McLeod R. Early and longitudinal evaluations of treated infants and children and untreated historical patients with congenital toxoplasmosis: the Chicago Collaborative Treatment Trial. Clin Infect Dis. 1994;18(1):38–72 Systematic diagnosis and follow up of treated and untreated children and the beginning of a randomized treatment study.
•• Swisher CN, Boyer K, McLeod R. Congenital toxoplasmosis. In JB Bodensteiner, Ed. Semin Pediatr Neurol. 1994;1:4–25 Describes neurologic findings of congenital toxoplasmosis in the United States.
•• Roizen N, Swisher CN, Stein MA, Hopkins J, Boyer KM, Holfels E, Mets MB, Stein L, Patel D, Meier P, Withers S, Remington J, Mack D, Heydemann P, Patton D, McLeod R. Neurologic and developmental outcome in treated congenital toxoplasmosis. Pediatrics. 1995;95(1):11–20 Demonstrates better neurologic outcomes and the importance of recognizing that what may be interpreted as developmental delays may really be related to visual impairment. This emphasizes the importance of compensatory educational strategies.
•• Patel DV, Holfels EM, Vogel NP, Boyer KM, Mets MB, Swisher CN, Roizen NJ, Stein LK, Stein MA, Hopkins J, Withers SE, Mack DG, Luciano RA, Meier P, Remington JS, McLeod RL. Resolution of intracranial calcifications in infants with treated congenital toxoplasmosis. Radiology. 1996;199(2):433–40 Identifies that intracranial calcifications in infants with congenital toxoplasmosis resolve or diminish in size with treatment.
•• Vogel N, Kirisits M, Michael E, Bach H, Hostetter M, Boyer K, Simpson R, Holfels E, Hopkins J, Mack D, Mets MB, Swisher CN, Patel D, Roizen N, Stein L, Stein M, Withers S, Mui E, Egwuagu C, et al. Congenital toxoplasmosis transmitted from an immunologically competent mother infected before conception. Clin Infect Dis. 1996;23:1055–60 Identifies that occasionally preconception infection can be transmitted to a fetus even when the pregnant women did not have known immunocompromise.
•• Mets MB, Holfels E, Boyer KM, Swisher CN, Roizen N, Stein L, Stein M, Hopkins J, Withers S, Mack D, Luciano R, Patel D, Remington JS, Meier P, McLeod R. Eye manifestations of congenital toxoplasmosis. Am J Ophthalmol. 1996;122:309–24 Characterizes ocular toxoplasmosis with congenital infection, that it can be treated effectively without loss of vision in recurrences, and the timing of recurrences especially at school age entry, adolescence, and with significant stress.
•• Roberts F, McLeod R. Pathogenesis of toxoplasmic retinochoroiditis. Parasitol Today. 1999;15:51–7 Identifies pathogenic mechanisms in toxoplasmic retinochoroiditis.
•• Mack DG, Johnson JJ, Roberts F, Roberts CW, Estes RG, David C, Grumet FC, Mcleod R. HLA-class II genes modify outcome of Toxoplasma gondii infection. Int J Parasitol. 1999;29:1351–8 Identifies HLA Class II susceptibility alleles.
Lyons RE, Lyons K, McLeod R, Roberts CW. Construction and validation of a polycompetitor construct (SWITCH) for use in competitive RT-PCR to assess tachyzoite-bradyzoite interconversion in Toxoplasma gondii. Parasitology. 2001;123:433–9 Quantitating parasite tachyzoite and bradyzoite burden by PCR.
Brezin AP, Thulliez P, Couvreur J, Nobre R, McLeod R, Mets MB. Ophthalmic outcomes after prenatal and postnatal treatment of congenital toxoplasmosis. Am J Ophthalmol. 2003;135:779–84 Contrasts retinal disease in French and US children.
•• Boyer KM, Holfels E, Roizen N, Swisher C, Mack D, Remington J, Withers S, Meier P, McLeod R. Risk factors for Toxoplasma gondii infection in mothers of infants with congenital toxoplasmosis: Implications for prenatal management and screening. Am J Obstet Gynecol. 2005;192:564–71 Identifies risk factors and lack of recognition of these factors by mothers with infants with congenital toxoplasmosis in the US.
•• McLeod R, Khan AR, Noble GA, Latkany P, Jalbrzikowski J, Boyer K. Severe sulfadiazine hypersensitivity in a child with reactivated congenital toxoplasmic chorioretinitis. Pediatr Infect Dis J. 2006;25:270–2 Emphasizes that severe hypersensitivity with sulfonamides can occur with treatment of ocular toxoplasmosis, in this case DRESS syndrome which can be lethal.
•• Roizen N, Kasza K, Karrison T, Mets M, Noble AG, Boyer K, Swisher C, Meier P, Remington J, Jalbrzikowski J, McLeod R, Kipp M, Rabiah P, Chamot D, Estes R, Cezar S, Mack D, Pfiffner L, Stein M, et al. Impact of visual impairment on measures of cognitive function for children with congenital toxoplasmosis: implications for compensatory intervention strategies. Pediatrics. 2006;118:e379–90 Emphasizes the effect of visual impairment on the measurement of cognition in congenital toxoplasmosis and the importance of compensatory strategies.
•• McLeod R, Boyer K, Karrison T, Kasza K, Swisher C, Roizen N, Jalbrzikowski J, Remington J, Heydemann P, Noble AG, Mets M, Holfels E, Withers S, Latkany P, Meier P. Outcome of treatment for congenital toxoplasmosis, 1981-2004: The National Collaborative Chicago-Based, Congenital Toxoplasmosis Study. Clin Infect Dis. 2006;42:1383–94 Presents data for the National Collaborative Toxoplasmosis study over 23 years considering pre-specified endpoints, comparing the results with two doses of pyrimethamine following randomization, calculating Kaplan Meier analyses of endpoints, and documenting substantially better outcomes than in earlier literature.
• Arun V, Noble AG, Latkany P, Troia RN, Jalbrzikowski J, Kasza K, Karrison T, Cezar S, Sautter M, Greenwald MJ, Mieler W, Mets MB, Alam A, Boyer K, Swisher CN, Roizen N, Rabiah P, Del Monte MA, McLeod R. Cataracts in congenital toxoplasmosis. J AAPOS. 2007;11:551–4 Identifies types of cataracts and their treatment in congenital toxoplasmosis.
• Benevento JD, Jager RD, Noble AG, Latkany P, Mieler WF, Sautter M, Meyers S, Mets M, Grassi MA, Rabiah P, Boyer K, Swisher C, McLeod R. Toxoplasmosis-associated neovascular lesions treated successfully with ranibizumab and antiparasitic therapy. Arch Ophthalmol. 2008;126:1152–6 Identifies toxoplasmosis as a cause of choroidal neovascular membranes and their successful treatment with ranibizumab and antiparasitic treatment.
• Phan L, Kasza K, Jalbrzikowski J, Noble AG, Latkany P, Kuo A, Mieler W, Meyers S, Rabiah P, Boyer K, Swisher C, Mets M, Roizen N, Cezar S, Remington J, Meier P, McLeod R. Longitudinal study of new eye lesions in treated congenital toxoplasmosis. Ophthalmology. 2008;115:553–59 e8 Follows longitudinal outcomes of ocular disease in congenital toxoplasmosis with less recurrence of retinal disease in treated children.
• Phan L, Kasza K, Jalbrzikowski J, Noble AG, Latkany P, Kuo A, Mieler W, Meyers S, Rabiah P, Boyer K, Swisher C, Mets M, Roizen N, Cezar S, Sautter M, Remington J, Meier P, McLeod R. Longitudinal study of new eye lesions in children with toxoplasmosis who were not treated during the first year of life. Am J Ophthalmol. 2008;146:375–84 Follows longitudinal outcomes of ocular disease in congenital. There were more recurrences in children who missed treatment in the first year of life.
• Jamieson SE, de Roubaix LA, Cortina-Borja M, Tan HK, Mui EJ, Cordell HJ, Kirisits MJ, Miller EN, Peacock CS, Hargrave AC, Coyne JJ, Boyer K, Bessieres MH, Buffolano W, Ferret N, Franck J, Kieffer F, Meier P, Nowakowska DE, et al. Genetic and epigenetic factors at COL2A1 and ABCA4 influence clinical outcome in congenital toxoplasmosis. PLoS One. 2008;3:e2285 Discusses epigenetic influences on the development of congenital toxoplasmosis.
Jamieson SE, Cordell H, Petersen E, McLeod R, Gilbert RE, Blackwell JM. Host genetic and epigenetic factors in toxoplasmosis. Mem Inst Oswaldo Cruz. 2009;104:162–9 Discusses discovery of susceptibility genes that indicate imprinting and epigenetic influences.
•• Tan T, Mui E, Cong H, Witola W, Montpetit A, Muench S, Sidney J, Alexander J, Sette A, Grigg M, Reed S, Maewal A, Kim S, Boothroyd J, McLeod R. Identification of T. gondii epitopes, adjuvants, & host genetic factors that influence protection of mice & humans. Vaccine. 2010;28:3977–89 Identification of susceptibility gene in NCCCTS cohort, establishing MHC Class I pathway processing by ERAAP. Parts of the initial steps in development of a vaccine to prevent toxoplasmosis in humans which is ongoing with expanded approaches. Demonstration of powerful adjuvant effects of GLA-SE in HLA transgenic mice.
•• Lees MP, Fuller SJ, McLeod R, Boulter NR, Miller CM, Zakrzewski AM, Mui EJ, Witola WH, Coyne JJ, Hargrave AC, Jamieson SE, Blackwell JM, Wiley JS, Smith NC. P2X7 receptor-mediated killing of an intracellular parasite, Toxoplasma gondii, by human and murine macrophages. J Immunol. 2010;184:7040–6 Susceptibility gene for congenital toxoplasmosis which influences outcomes, affecting cytokines and cell death.
Jamieson SE, Peixoto-Rangel AL,Hargrave AC,Roubaix LA,Mui EJ,Boulter NR,Miller EN,Fuller SJ,Wiley JS,Castellucci L, Boyer K, Peixe RG,Kirisits MJ,Elias Lde S,Coyne JJ,Correa-Oliveira R,Sautter M,Smith NC,Lees MP,Swisher CN,Heydemann P,Noble AG,Patel D,Bardo D,Burrowes D,McLone D,Roizen N,Withers S,Bahia-Oliveira LM, McLeod R,Blackwell JM. Evidence for associations between the purinergic receptor P2X(7) (P2RX7) and toxoplasmosis. Genes Immun. 2010;11:374-383. Susceptibility gene for congenital toxoplasmosis which influences outcomes, affecting cytokines and cell death.
•• Noble G, Latkany P, Kusmierczyk J, Mets M, Rabiah P, Boyer K, Jalbrzikowski J, Wroblewski K, Karrison T, Swisher C, Mieler W, Meier P, McLeod R. Chorioretinal lesions in mothers of children with congenital toxoplasmosis in the National Collaborative Chicago-based, Congenital Toxoplasmosis Study. Scientia Medica. 2010;20:20–6 Finds that ten percent of mothers of infants in the US who have congenital toxoplasmosis have retinal lesions, emphasizing the importance of performing eye examinations of mothers of children with congenital toxoplasmosis.
•• Witola WH, Mui E, Hargrave A, Liu S, Hypolite M, Montpetit A, Cavailles P, Bisanz C, Cesbron-Delauw MF, Fournié GJ, McLeod R. NALP1 influences susceptibility to human congenital toxoplasmosis, proinflammatory cytokine response, and fate of Toxoplasma gondii-infected monocytic cells. Infect Immun. 2011;79:756–66 Identifies susceptibility gene to congenital toxoplasmosis determining functioning of the inflammasome.
Delair E, Latkany P, Noble AG, Rabiah R, McLeod R, Brezin A. Clinical Manifestations of Ocular Toxoplasmosis. Ocul Immunol Inflamm. 2011;2:91–102 Collates and presents clinical manifestations of ocular toxoplasmosis in a pictorial collection.
Hill D, Coss C, Dubey JP, Wroblewski K, Sautter M, Hosten T, Munoz-Zanzi C, Mui E, Withers S, Boyer K, Hermes G, Coyne J, Jagdis F, Burnett A, McLeod P, Morton H, Robinson D, McLeod R, Toxoplasmosis Study Group. Identification of a sporozoite-specific antigen from Toxoplasma gondii. J Parasitol. 2011;97:328-37 Identifies antigens in sporozoites in oocysts that elicit an antibody response present for about 8 months following exposure consistent with the half-life of that antibody, allowing exposure. Also identifies high prevalence of Toxoplasma infection in Lancaster Pennsylvania Amish persons.
•• Stillwaggon E, Carrier CS, Sautter M, McLeod R. Maternal serologic screening to prevent congenital toxoplasmosis: a decision-analytic economic model. PLoS Negl Trop Dis. 2011:5–e1333 Demonstrates parameters that lead to cost effective screening for Toxoplasma infection acquired in gestation. This suggests strategies important in this model for lowering costs for diagnosis and treatment to facilitate programs for screening.
•• Boyer K, Hill D, Mui E, Wroblewski K, Karrison T, Dubey JP, Sautter M, Noble AG, Withers S, Swisher C, Heydemann P, Hosten T, Babiarz J, Lee D, Meier P, McLeod R. Toxoplasmosis Study Group. Unrecognized ingestion of Toxoplasma gondii oocysts leads to congenital toxoplasmosis and causes epidemics in North America. Clin Infect Dis. 2011;53:1081–9 Identifies epidemics of acute acquired Toxoplasma infection in North America and that ingestion of oocysts may go unrecognized.
•• McLeod R, Boyer K, Lee D, Mui E, Wroblewski K, Karrison T, Noble AG, Withers S, Swisher CN, Heydemann PT, Sautter M, Babiarz J, Rabiah P, Meier P, Grigg M. Prematurity & Severity Associate with T. gondii Alleles (NCCCTS, 1981-2009). Clin Infect Dis. 2012;54:1595–605 Defines serotypes of T .gondii and their distribution in the United States, and associations of Toxoplasma genotypes with phenotypes of illness including prematurity and severity of illness.
•• Lai BS, Witola WH, El Bissati K, Zhou Y, Mui E, Fomovska A, McLeod R. Molecular target validation, antimicrobial delivery, and potential treatment of Toxoplasma gondii infections. Proc Natl Acad Sci U S A. 2012;109:14182–7 Identification or validation of molecular targets in Toxoplasma and that they can be targeted with antisense as an approach to medicines.
•• Burrowes D, Boyer K, Swisher CN, Noble AG, Sautter M, Heydemann P, Rabiah P, Lee D, McLeod R. Toxoplasmosis Study Group. Spinal Cord Lesions in Congenital Toxoplasmosis Demonstrated with Neuroimaging, Including Their Successful Treatment in an Adult. J Neuroparasitology. 2012;3:1–8 Chronic active toxoplasmosis in an adult and its effective treatment proves that this can occur in the brain and spinal cord, not only the eye, and that it can resolve with treatment.
•• Béla SR, Dutra MS, Mui E, Montpetit A, Oliveira FS, Oliveira SC, Arantes RM, Antonelli LR, McLeod R, Gazzinelli RT. Impaired Innate Immunity in Mice Deficient in Interleukin-1 Receptor-Associated Kinase 4 Leads to Defective Type 1 T Cell Responses, B Cell Expansion, and Enhanced Susceptibility to Infection with Toxoplasma gondii. Infect Immun. 2012;80:4298–308 Susceptibility gene and its mechanism in congenital toxoplasmosis.
•• Witola W, Liu S, Montpetit A, Hypolite M, Zhou Y, Mui E, Cesbron-Delauw MF, Fournie G, Cavailles P, Bisanz C, Boyer K, Withers S, Noble AG, Swisher C, Heydemann P, Rabiah P, McLeod R. ALOX12 In Human Toxoplasmosis. Infect Immun. 2014;82(7):2670–9 Susceptibility genes and their mechanisms in congenital toxoplasmosis.
• McLeod R. Utility and limitations of T. gondii-specific IgM serum antibodies in the diagnosis of congenital toxoplasmosis in Porto Alegre. J Pediatr. 2014;90(4):329–31 Emphasizes utility and limitation of testing for T.gondii specific IgM serum antibodies in infants.
•• McLeod R, Lykins J, Noble AG, Rabiah P, Swisher C, Heydemann P, McLone D, Frim D, Withers S, Clouser F, Boyer K. Management of Congenital Toxoplasmosis. Current Pediatrics Reports. 2014;2(3):166–94 Provides guidelines and an overview of the supporting evidence for the management of congenital toxoplasmosis based on the US experience.
•• Hutson SL, Wheeler KM, McLone D, Frim D, Penn R, Swisher CN, Heydemann PT, Boyer KM, Noble AG, Rabiah P, Withers S, Montoya JG, Wroblewski K, Karrison T, Grigg ME, McLeod R. Patterns of Hydrocephalus Caused by Congenital Toxoplasma gondii Infection and Association with Parasite Strain. Cli48, 58,61n Infect Dis. 2015. Pattern of hydrocephalus associated with parasite serotype suggesting different epitopes may be critical or that there may be multifactorial influences.
•• Contopoulos-Ioannidis D, Wheeler KM, Ramirez R, Press C, Mui E, Zhou Y, Van Tubbergen C, Prasad S, Maldonado Y, Withers S, Boyer KM, Noble AG, Rabiah P, Swisher CN, Heydemann P, Wroblewski K, Karrison T, Grigg ME, Montoya JG, McLeod R. Clustering of Toxoplasma gondii Infections Within Families of Congenitally Infected Infants. Clin Infect Dis. 2015;61(12):1815–24 Emphasizes that toxoplasmosis occurs in families, living groups likely exposed to the same risk factors.
•• McLeod R, Wheeler KM, Boyer K. Reply to Wallon and Peyron. Clin Infect Dis. 2016;62(6):812–4 Emphasizes that favorable outcomes in treated toxoplasmosis are due to treatment.
•• Begeman IJ, Lykins J, Zhou Y, Lai BS, Levigne P, El Bissati K, Boyer K, Withers S, Clouser F, Noble AG, Rabiah P, Swisher CN, Heydemann PT, Contopoulos-Ioannidis DG, Montoya JG, Maldonado Y, Ramirez R, Press C, Stillwaggon E, et al. Point-of-care testing for Toxoplasma gondii IgG/IgM using Toxoplasma ICT IgG-IgM test with sera from the United States and implications for developing countries. PLoS Negl Trop Dis. 2017;11:e0005670 All sera from persons in the NCCCTS including all serotypes and acute, subacute and chronic, could be detected with 100% sensitivity and specificity. A consideration of spillover benefit and clinical benefit is included.
•• Lykins J, Li X, Levigne P, Zhou Y, El Bissati K, Clouser F, Wallon M, Morel F, Leahy K, El Mansouri B, Siddiqui M, Leong N, Michalowski M, Irwin E, Goodall P, Ismail M, Christmas M, Adlaoui EB, Rhajaoui M, et al. Rapid, inexpensive, fingerstick, whole-blood, sensitive, specific, point-of-care test for antiToxoplasma antibodies. PLoS Negl Trop Dis. 2018;12(8):e0006536 Whole blood obtained by fingerstick is an efficient and accurate way to screen for Toxoplasma seropositivity with 100% sensitivity and specificity.
Lykins J, Wang K, Wheeler K, Clouser F, Dixon A, El Bissati K, Zhou Y, Lyttle C, Rzhetsky A, McLeod R. Understanding Toxoplasmosis in the United States through “Large Data” Analyses. Clin Infect Dis. 2016;63(4):468–75 Initial effort to understand the magnitude and implications of Toxoplasma infection of humans in the United States. Editors choice and Editorial.
• Soberon-Felin M, Grose A, Castro C, Moreira A, AShi K, Li X, McLeod et al. Building Programs to Eliminate Toxoplasmosis: Part II Education. Current Pediatrics Reports 2022. In Press Considers and presents many aspects of contrasts in gestational screening in France facilitating early treatment with delays that are the norm in the United States inxlusing Peyron (2017 see Ref 52).
•• Ngô HM, Zhou Y, Lorenzi H, Wang K, Kim TK, Zhou Y, El Bissati K, Mui E, Fraczek L, Rajagopala SV, Roberts CW, Henriquez FL, Montpetit A, Blackwell JM, Jamieson SE, Wheeler K, Begeman IJ, Naranjo-Galvis C, Alliey-Rodriguez N, Davis RG, Soroceanu L, Cobbs C, Steindler DA, Boyer K, Noble AG, Swisher CN, Heydemann PT, Rabiah P, Withers S, Soteropoulos P, Hood L, Mcleod R. Toxoplasma Modulates Signature Pathways of Human Epilepsy, Neurodegeneration & Cancer. Sci Rep (Nature). 2017;7(1):11496. https://doi.org/10.1038/s41598-017-10675-6.Using a systems biology analysis of genetics, transcriptomics, proteomics, serum and miR biomarkers, upstream regulators, protein association string, immunohistochemistry, and human MM6 (myeloid) and primary human brain neuronal stem cells, disease association analyses, it was found that Toxoplasma modulates signature pathways of human epilepsy, neurodegeneration and cancer. This has important implications for the 2 billion people who have this parasite in their brains across lifetimes, including in Panama, Colombia and the United States, making the seroprevalence of 85% in Panama adults over the age of 65 years potentially of considerable significance for those later in life.
•• El Bissati K, Levigne P, Lykins J, Adlaoui EB, Barkat A, Berraho A, Laboudi M, El Mansouri B, Ibrahimi A, Rhajaoui M, Quinn F, Murugesan M, Seghrouchni F, Gómez Marín JE, Peyron F, and McLeod R. Global initiative for congenital toxoplasmosis: an observational and international comparative clinical analysis. Emerging Microbes & Infections (2018) 7:165 Emerging Microbes & Infections 10.1038/s41426-018-0164-4. Introduces the concept of the ongoing global initiative to eliminate toxoplasmosis.
Aguirre AA,Longcore T, Barbieri M, Dabritz H, Hill D, Klein PN,Lepczyk C, Lilly EL, McLeod R, Milcarsky J, Murphy CE, Su C, VanWormer E, Yolken R,Sizemore GC. The One Health Approach to Toxoplasmosis: Epidemiology, Control, and Prevention Strategies. Ecohealth. 2019 10.1007/s10393-019-01405-7. [Epub ahead of print]. Considers Toxoplasma as part of a “One Health” initiative including cat excrement exposure and what could be done to improve water systems and eliminate contamination due to oocysts.
• McLone D, Frim D, Penn R, Swisher CN, Heydemann P, Boyer K, Noble AG, Rabiah P, Withers S, Wroblewski K, Karrison T, Hutson S, Wheeler K, Cohen W, Lykins J, McLeod R. Outcomes of hydrocephalus secondary to congenital toxoplasmosis. J Pediatric Neurosurgery, I doi: 10.3171/2019.6. PEDS18684. 2019. Documents that prompt treatment including needed neurosurgery placement of ventriculoperitoneal shunts can result in favorable outcomes.
• Wallon M, Peyron F, Cornu C, Vinault S, Abrahamowicz M, Kopp CB, Binquet C. Congenital toxoplasma infection: monthly prenatal screening decreases transmission rate and improves clinical outcome at age 3 years. Clin Infect Dis. 2013;56(9):1223–31 Improved outcomes with screening and treatment in utero.
• Peyron F, McLeod R, Ajzenberg D, Contopoulos-Ioannidis DG, Kieffer F, Mandelbrot L, Sibley LD, Pelloux H, Villena I, Wallon M, Montoya JG. Congenital toxoplasmosis in France and the United States: one parasite, two diverging approaches. 2017;11(2):e0005222. France has a strong prenatal diagnosis and treatment program using currently available medicines. This has been initiated but is not yet developed for widespread use in the United States. Currently attempts are initiated to build such programs modeled on the French experience.
•• Prusa AR, Kasper DC, Sawers L, Walter E, Hayde M, Stillwaggon E. Congenital toxoplasmosis in Austria: prenatal screening for prevention is cost saving. PLoS Negl Trop Dis. 2017;11(7):e0005648 Fourteen-fold cost savings, with efficacy that has transformed outcomes of congenital infection in Austria with use of pre-natal screening. Goal herein is to scale up such programs worldwide to benefit individual patients and societies with spill over benefit for maternal and child health.
Kosack CS, Pasge AL, Klatser PR. A guide to aid the selection of diagnostic tests. Bull World Health Organ. 2017;95(9):639–45 Guide to diagnostic tests prepared by WHO.
•• Gomez CA, Budvytyte LN, Press C, Zhou L, McLeod R, Maldonado Y, Montoya JG, Contopoulos-Ioannidis DG. Evaluation of three point-of-care (POC) tests for detection of Toxoplasma immunoglobulin IgG and IgM in the United States: proof of concept and challenges. Open For Inf Dis. 2018; 10.1093/ofid/ofy215. High sensitivity and specificity of LDBio used with sera.
•• Stillwaggon E, Carrier CS, Sautter M, McLeod R. Maternal serologic screening to prevent congenital toxoplasmosis: a decision-analytic economic model. PLoS Negl Trop Dis. 2011 ;5(9):e1333. Dec 10(1):1675-1682. doi: 10.1080/22221751.2021.1948359.Supplement. Equations for determining cost efficacy of gestational screening for acquisition of Toxoplasma during gestation. This is to facilitate prompt treatment to prevent congenital infection and/or its sequelae.
• El Mansouri B, Amarir F, Peyron F, Adlaoui EB, Piarroux R, El Abassi M, Lykins J, Nekkal N, Bouhlal N, Makkaoui M, Barkat A, Lyaghfouri A, Zhou Y, Rais S, Daoudi F, Ismail Elkoraichi I, Zekri M, Nezha B, Hajar M, et al. El Bissati K. Performance of a novel point-of-care blood test for Toxoplasma infection in women from diverse regions of Morocco. Microbes Infect. 2021;10(1):1675–82. https://doi.org/10.1080/22221751.2021.1948359High prevalence of Toxoplasma infection in Morocco: LDBio can be used for diagnosis with high sensitivity and specificity, infection was associated with poverty, well water, not washing fruits and vegetables.
•• Grose A, Wallon M, Chapey E, LeahyK, ZhouY, Siddiqui M, Leong N, Goodall P, Tesic V, Beavis C, Jouze S, Abraham S, Limonne D, Piarroux R, McLeod R. Eliminating Confounding False Positive IGM tests by Using a Lateral Immunochromatography Test that meets WHO ASSURED Criteria In submission, 2022. Demonstrates that LDBio can eliminate problems from false positive IgMs in serologic screening programs for congenital toxoplasmosis for those who are seronegative.
• Flores C, Villalobos-Cerrud D, Borace J, Mcleod R, Fábrega L, Norero X, Sáez-Llorens X, Moreno MT, Restrepo CM, Llanes A, Mario Quijada RM, Ladrón De Guevara M, Guzmán G, de la Guardia V, García A, Wong D, Reyes O, Soberon M, Caballero EZ. Prevalence and risk factors associated with T. gondii infection in pregnant women and newborns from Panama. Pathogens. 2021;10(6):764. https://doi.org/10.3390/pathogens10060764Identifies areas of high risk in Panama, high frequency of infections, and role of exposure to pet animals.
•• Mandelbrot L, Kieffer F, Sitta R, Laurichesse-Delmas H, Winer N, Mesnard, Berrebi A, Le Bouar G, Bory J-P, Cordier A-G, Ville Y, Perrotin F, Jouannic J-M, Biquard F, d’ErcoleC, Houfflin-Debarge V, Villena I, Thiébaut R, Prenatal therapy with pyrimethamine + sulfadiazine versus spiramycin to reduce placental transmission of toxoplasmosis: A multicenter, randomized trial, American Journal of Obstetrics and Gynecology (2018), 10.1016/j.ajog.2018.05.031. Demonstrates that outcomes can be highly favorable with serologic screening in gestation and prompt treatment, with slight improvement in outcomes with pyrimethamine and sulfadiazine treatment after 16 weeks gestation defined as 16 weeks of amenorrhea.
McLeod R., Sautter M, Rooney T, Morel J, Taub L, Taub D, Taub V, Taub JW, Tirado S, Latkany P, Boyer K, Hotez P, Lin E, McLone D, and Friends et al Submission to the Committee on Public Health Illinois State Senate. Regarding: Prenatal and Neonatal Congenital Toxoplasmosis Prevention and Treatment Act, SB3667 in the context of the National Collaborative Chicago Based Congenital Toxoplasmosis Study. April 13, 2010. Introduction of a bill to have a law that obstetricians in Illinois offer their patients the opportunity to have serologic testing in gestation, in Illinois. This provided information from patients, families, physicians, scientists. Recommended law.
•• Dubey JP, Murata FHA, Cerqueira-Cézar CK, Kwok OCH, Villena I. Congenital toxoplasmosis in humans: an update of worldwide rate of congenital infections. Parasitology. 2021;148:1406–16. https://doi.org/10.1017/S0031182021001013Up to date review of prevalence and findings of congenital toxoplasmosis around the world.
• Gomez-Marín JE, Munoz-Ortiz J, Mejía-Oquendo M, Arteaga-Rivera JY, Nicolas Rivera-Valdivia N, Bohorquez-Granado MC, Velasco-Velasquez S, Castano-de-la-Torre G, Acosta-Davila JA, García-Lopez LL, Torres-Morale ES, Vargas M, Valencia JD, Celis-Giraldo D, de-la-Torre A. High frequency of ocular toxoplasmosis in Quindío, Colombia and risk factors related to the infection. Heliyon. 2021;7:e06659 Identifies high prevalence of ocular toxoplasmosis in Quindio, Colombia and associated risk factors. Importance of water purification (drinking bottled water) associated with prevention was identified.
•• McLeod R.,Cohen W, Dovgin S, Finkelstein L, Boyer K. Human Toxoplasmosis. Weiss, LM, Kim, K. (Editors). The Model apicomplexan: Perspectives and Methods Third Edition. Chapter 4. Elsevier.2020 pp.117-228. Comprehensive up to date consideration of human toxoplasmosis, including clinical aspects, treatment, prevention, other considerations of pathogenesis, unifying concepts and toward the future.
Mejia-Oquendo M, Marulanda-Ibarra E, Gomez-Marin JE, Evaluation of the impact of the first evidence-based guidelines for congenital toxoplasmosis in Armenia (Quindío) Colombia: An observational retrospective analysis The Lancet Regional Health - Americas.2021;1:100010. Between 2001 and 2019, national guideline has had a positive impact by improv-ing early diagnosis and treatment of prenatal toxoplasmosis and reducing severity.'.
•• Kieffer F, Wallon M, Garcia P, Thulliez P, Peyron F, Franck J. Risk factors for retinochoroiditis During the firat 2 years of life in infants with treated Congenital toxoplasmosis. J Pediatr Infect Dis J. 2008;27(1):27–32. https://doi.org/10.1097/INF.0b013e318134286dDefines risk factors for active disease in the first two years of life in children with treated congenital disease. “3 factors were significantly associated with first retinochoroiditis before the age of 2 years: a delay of >8 weeks between maternal seroconversion and first treatment [hazard ratio, 2.54; 95% confidence interval (CI), 1.14-5.65], female gender (hazard ratio, 2.02; 95% CI, 1.01-4.1), and cerebral calcifications at birth (hazard ratio, 4.3; 95% CI, 1.9-10). There was no correlation between gestational age at the time of maternal infection and risk for retinochoroiditis.”.
•• Soberon-Felin, McLeod et al. Building Programs to eradicate Toxoplasmosis. Part IV:: Understanding and Development of Public Health Strategies and Advances “Takea Village”. Current Pediatrics Reports. 2022 In Press Considers needed next stesps in a global initiative to eradicate Toxoplasosis. Considers Wallon (51).
•• Montoya JG, Laessig K, Fazeli MS, Siliman G, Yoon SS, Drake-Shanahan E, Zhu C, Akbary A, Mcleod R. A fresh look at the role of spiramycin in preventing a neglected disease: meta-analyses of observational studies. Eur J Med Res. 2021;26(1):1–0 Meta-analysis shows contribution of spiramycin to prevention and improved outcomes of congenital toxoplasmosis. Recent work by Mandelbrot et al suggests its most important role is in the first 14 weeks of gestation trimester when pyrimethamine may be teratogenic.
McLeod R, Lee D, Clouser F, Boyer K. Toxoplasmosis in the Fetus and Newborn Infant. In: Stevenson D and Sunshine P, Neonatology: Clinical Practice and Procedures. 1st, New York: McGraw Hill; 2015. p. 821–76. Comprehensive review of data concerning toxoplasmosis in the fetus and newborn infant with images.
McLeod R, Lee D, Clouser F, Boyer K. Diagnosis of Congenital Toxoplasmosis. In: Stevenson D and Sunshine P, Neonatology: Clinical Practice and Procedures. 1st, New York: McGraw Hill; 2015. p. 1297–310. Atlas of images of congenital toxoplasmosis and its diagnosis and treatment.
•• McLeod R, Boyer K. Toxoplasmosis. In Nelson’s Textbook of Pediatrics, 22ndt Ed. Behrman RL, Kliegman R, Arvin AM (Eds.). Philadelphia, WB Saunders, 2021. In Press. Most current chapter summarizing newer aspects of Toxoplasmosis in 2021.
•• Remington JS, McLeod R, Thulliez P, Desmonts G, Toxoplasmosis. Infectious Diseases of the Fetus and Newborn Infant. Ch 31. Elsevier. 6th edition. 2006. pp.947-1091. Detailed, thorough chapter that presents data and images of toxoplasmosis in the fetus and newborn infant.
•• Hotez PJ. Neglected Infections of Poverty in the United States of America P. June 2008 | Volume 2 | Issue 6 | e2 PLoS Neglected Tropical Diseses 2008. Demonstrates and emphasizes that the diseases noted to occur in developing countries also occur in the United States, especially in areas of poverty. These include toxoplasmosis, which affects persons of all demographics.
•• Lago EG, Endres MM, MFDC S, Fiori HH. Ocular Outcome of Brazilian Patients with Congenital Toxoplasmosis. Pediatr Infect Dis J. 2021;40(1):e21–7. https://doi.org/10.1097/INF.0000000000002931Part of a series of papers by Lago et al, demonstrating the severity of congenital toxoplasmosis in Brazil, manifestations, and efficacy associated with the high incidence of new retinochoroidal lesions during the follow-up period indicates the importance of long-term follow-up of patients with congenital toxoplasmosis. Initiating treatment within the first 4 months of life, especially within the first 2 months, was a protective factor against the later development of retinochoroiditis.
•• Silva Machado A et al. Biomarker Analysis Revealed Distinct Profiles of Innate and Adaptive immunity in Infants with ocular lesions of Congenital toxoplasmosis Scientific Reports, vol 2014, 2020. Active retinal lesions associated with leukocytosis with monocytes and NK cells CD8+ T cells, possibly predicting morbidity.
Guerina NG, Hsu HW, Meissner HC, et al. Neonatal serologic screening and early treatment for congenital Toxoplasma gondii infection. The New England Regional Toxoplasma Working Group. N Engl J Med. 1994:330–1858 Newborn screening program in Massachusetts, New Hampshire and Vermont detects congenital toxoplasmosis not otherwise recognized at birth with approximately half with retinal or central nervous system signs with careful evaluation.
Dubey JP, Lago EG, Gennari SM Su, Jones JL. Toxoplasmosis in humans and animals in Brazil: high prevalence, high burden of disease, and epidemiology. Parasitology. 10 July 2012. Comprehensive review of toxoplasmosis in Brazil.
Chapey, E., Wallon, M., Peyron, F., 2017. Evaluation of the LDBIO point of care test for the combined detection of toxoplasmic IgG and IgM. Clin. Chim. Acta 464,200-201. Available from: https://doi.org/10.1016/j.cca.2016.10.023. Lateral immunochromatography test for IgG and IgM sensitive and specific in France when testing serum.
•• Pomares C, Zhang B, Arulkumar S, Gonfrier G, Marty P, Zhao S, Cheng S, Tang M, Dai H, Montoya JG. Validation of IgG, IgM multiplex plasmonic gold platform in French clinical cohorts for the serodiagnosis and follow-up of Toxoplasma gondii infection. Diagn Microbiol Infect Dis. 2017;87(3):213–8. https://doi.org/10.1016/j.diagmicrobio.2016.09.001Inexpensive serum and saliva nanotest diagnoses Toxoplasma infection.
•• Li X, Pomares C, Peyron F, Press CJ, Ramirez R, Gonfrier G, Cannavo I, Chapey E, Levigne P, Wallon M, Montoya JG, Hongjie Dai H. Plasmonic gold chips for the diagnosis of Toxoplasma gondii, CMV, and rubella infections using saliva with serum detection precision. Eur J Clin Microbiol Infect Dis. 2019;38(5):883–90. https://doi.org/10.1007/s10096-019-03487-1Nanogold test can be multiplexed for perinatal infections with high sensitivity and specificity.
•• Abraham S, McLeod R, Houhou-Fidouh, Nicaise-Rolland P, Landraud L, Houze S. Performances of Toxoplasma ICT IgG-IgM in comparison with Vidas Toxo Competition and Toxoscreen, Lyon France European meeting. 2022. In submission. Lateral Chromatography test highly sensitive and specific when testing sera from persons in France and the USA.
Ben-Abdallah R et al. Contribution of the Toxoplasma ICT IgG IGM test in determining the immune status of pregnant women against toxoplasmosis. 10.1002/jcla 23749 2021. Lyon France European meeting. ICT Lateral immunochromatography test sensitive and specific with sera in Algeria.
Cardosa L, Piarroux R, Lopes APInterest du test Toxoplasma ICT IgG-IgM dans le diagnostic serologique de l’infection a Toxoplasma gondi chez le chat. 2022. In Press. POC test also of use for detection of infection in cats although not as sensitive and specific as for human infections.
•• McPhillie M, Zhou Y, El Bissati K, Dubey J, Lorenzi H, Capper M, Lukens AK, Hickman M, Muench S, Verma SK, Weber CR, Wheeler K, Gordon J, Sanders J, Moulton H, Wang K, Kim TK, He Y, Santos T, et al. New paradigms for understanding and step changes in treating active and chronic, persistent apicomplexan infections. Sci Rep. 2016;6:29179. https://doi.org/10.1038/srep29179Brazilian strain of Toxoplasma, EGS, grows as a slowly replicating encysted organism in tisuue culture identifying cytochrome b qi domain as critical for this lifecycle stage. This is used to develop an inhibitor of this molecular target in Toxoplasma amd Plasmodia.
•• McPhillie M, Zhou Y, Hickman M, Gordon J, Weber C, Li Q, Lee P, Amporndanai K, Johnson RH, Darby H, Woods S, Li ZH, Priestley R, Ristroph K, Biering GC, El Bissati K, Hwang S, Hakim FE, Dovgin S, et al. Potent Tetrahydroquinolone Eliminates Apicomplexan Parasites. Front. Cell Infect Microbiol. 2020;10:203. https://doi.org/10.3389/fcimb.2020.00203JAG21 is potent against tachyzoites, bradyzoites of toxoplasma, completely curative with prompt treatment. If begun in vivo after 15 days in vivo a small proportion of cysts (<50%) remain. Effective at low nM amounts in single oral dose also against P berghei three life cycle stages. “Persister” of a model parasite rps 13 delta that has exited the cell cycle shows overlapping molecular targets with P. cynomogoli hypnozoites single cell RNA seq providing insight into and model system to test which genes are transcribed in the small numbers of persisters.
•• E book, Research Topic editorial: Front. Cell. Infect. Microbiol. McPhillie M, Zhou Y, Hickman M, Gordon J, Weber C, Li Q, Lee P, Amporndanai K, Johnson RH, Darby H, Woods S, Li ZH, Priestley R, Ristroph K, Biering GC, El Bissati K, Hwang S, Hakim FE, Dovgin S, Lykins J, Roberts L, Hargrave K, Cong H, Sinai A, Muench SP, Dubey JP, Prud’homme R, Lorenzi, H Biagini GC, Moreno S, Roberts CW, Atonyuk S, Fishwick CW and McLeod R (2020) Potent Tetrahydroquinolone Eliminates Apicomplexan Parasites. Front. Cell. Infect. Microbiol Ebook with editorial by de-la-Torre A and Gomez-Marin JE that states: “Finally, one major finding reported in this Research Topic is the development of a powerful tetrahydroquinolone, JAG21, which can eliminate apicomplexan parasites in tissues (McPhillie et al.). This is an extraordinary achievement in in vivo models because, until now, there are no drugs that can eliminate tissue cysts of the parasite responsible for reactivations during the host’s period of life. The authors created a next generation lead compound with high in vitro and in vivo efficacy against T. gondii tachyzoites, bradyzoites, and established encysted organisms (McPhillie et al). This compound is promising and deserves further development through preparation of advanced formulations and testing in further studies of pharmacokinetics, efficacy, and safety. In summary, this Research Topic shows significant advances made in the study of T. gondii using in-vitro, in-vivo and animal models. The results presented here will illuminate the pathway to create an effective clinical response to this public health key issue.”
Lykins JD, Filippova EV, Halavaty AS, Minasov G, Zhou Y, Dubrovska I, Flores KJ, Shuvalova LA, Ruan J, El Bissati K, Dovgin S, Roberts CW, Woods S, Moulton JD, Moulton H, McPhillie MJ, Muench SP, Fishwick CWG, Sabini E, et al. CSGID Solves Structures and Identifies Phenotypes for Five Enzymes in Toxoplasma gondii. Front Cell Infect Microbiol. 2018;8:352. https://doi.org/10.3389/fcimb.2018.00352. eCollection 2018 Crystalography pipeline identifies potential molecular targets (enzymes) in Toxoplasma gondii; Vivo morpholinos and CRISPR/Cas9 screen together demonstrate which is essential in tachyzoites.
Eichenwald HF. A study of congenital toxoplasmosis with particular emphasis on clinical manifestations, sequelae and therapy. In: Human Toxoplasmosis, Siim JC (Ed), Munksgaard, Copenhagen 1959. Congenital toxoplasmosis with generalized or neurologic presentation in the US if untreated or treated only one month causes substantial neurologic and eye disease by the age of 4 years with significant morbidity.
Koppe JG, Loewer-Sieger DH, de Roever-Bonnet H. Results of 20-year follow-up of congenital toxoplasmosis. Lancet. 1986;1:254 Apparently asymptomatic infants develop adverse visual sequelae of congenital toxoplasmosis by teensge years.
Wilson CB, Remington JS, Stagno S, Reynolds DW. Development of adverse sequelae in children born with subclinical congenital Toxoplasma infection. Pediatrics. 1980;66:767 Apparently asymptomatic infants develop adverse retinal and central nervous system sequelae of congenital toxoplasmosis.
Rostami A, et al. Acute Toxoplasma infection in pregnant women worldwide: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2019;13(10):e0007807. https://doi.org/10.1371/journal.pntd.0007807Prevalence of antibodies to T. gondii in pregnant women worldwide.
Ryning FW, Mcleod R, Maddox JC, Hunt S, Remington JS. Probable transmission of Toxoplasma gondii by organ transplantation. Ann Intern Med. 1979;90(1):47–9 Patient who received a cardiac transplant donated from a person who died in a motorcycle accident who had acute toxoplasmosis. The recipient of this infected donor organ developed brain abscesses and encephalitis due to Toxoplasma gondii. His toxoplasmic brain disease responded to many months of treatment with pyrimethamine, sulfadiazine and leucovorin demonstrating this infection could be treated in such immune compromised persons when treatment was continued throughout the immune compromise until resolution of brain involvement.
Levin M, Mcleod R, Young Q, Abrahams C, Chambliss M, Walzer P, Kabins SA. Pneumocystis pneumonia: importance of gallium scan for early diagnosis and description of a new immunoperoxidase technique to demonstrate Pneumocystis carinii. Am Rev Respir Dis. 1983;128(1):182–5 Initial patient with toxoplasmosis encephalitis in the Midwest and eleventh in the United States with multiple opportunistic infections at the outset of the AIDS epidemic. His toxoplasmic encephalitis responded to treatment with pyrimethamine sulfadizine given with leucovorin.
Dubey JP. Schizogony and gametogony of oocyst-deficient T-263 strain of Toxoplasma gondi. Vet Parasitol. 2017;245:160–2. https://doi.org/10.1016/j.vetpar.2017.05.024T-263 cannot make life cycle stages beyond schizonts, male and female gametes. This chemically mutagenized parasite clone is an effective accine when administered orally in separate study eliminating endemic toxoplasmic infections on a pig farm in southern Illinois when administered to cats on this farm. Subsequent analysis of this clone provides a rosetta stone to merozoite development and capacitation preparing for Conception of Toxoplasma gondii.
Ramakrishnan C, Maier S, Walker R et al. An experimental genetically attenuated live vaccine to prevent transmission of Toxoplasma gondii by cats. Scientific Reports vol 9, No.: 1474 (2019) “RNA-Seq analysis of cat enteric stages of T. gondii uncovered genes expressed uniquely in microgametes and macrogametes. A CRISPR/Cas9 strategy was used to create a T. gondii strain that exhibits defective fertilization, decreased fecundity and generates oocysts that fail to produce sporozoites. Inoculation of cats with this engineered parasite strain totally prevented oocyst excretion following infection with wild-type T. gondii, demonstrating that this mutant is an attenuated, live, transmission-blocking vaccine.”
Alvarez C, de-la-Torre A, Vargas M, Herrera C, Uribe-Huertas LD, Lora F, and Gómez-Marín JE Striking Divergence in Toxoplasma ROP16 Nucleotide Sequences From Human and Meat Samples. JID 2015:211 (15 June). p2006. Association of Rop 16 type 1/3 variant with ocular toxoplasmosis in Colombia demonstrated by sequence and peptide elisa testing of sera is not the predominant organism found in meat samples. Variation in storage processes and hygenic factors differed in stores selling meat in Quindio, Armenia Colombia.
Hutson SL, Mui E, Kinsley K, Witola WH, Behnke MS, El Bissati K, Muench SP, Rohrman B, Liu SR, Wollmann R, Ogata Y, Sarkeshik A, Yates JR 3rd, McLeod RT. T. gondii RP promoters & knockdown reveal molecular pathways associated with proliferation and cell-cycle arrest. PLoS One. 2010;5:e14057 Gi arrested tetracycline regulated mutant RH strain parasite is a dormant persisting parasite when tetracycline regulating and leading to transcription of the the small ribosomal protein 13 (RPS13) gene is absent. This organism can recrudesce after very long times in tissue culture exceeding 6-months demonstrating effect of ribosomal stress secondary to protein starvation. This mutated parasite is a highly effective vaccine for mice.
Chu K-B, Quan F-S. Advances in Toxoplasma gondii Vaccines: Current Strategies and Challenges for Vaccine Development. Vaccines. 2021;9:413. https://doi.org/10.3390/vaccines9050413Excellent review of many current vaccine studies.
•• De Mourn L, Garcia Bahia-Oliveira, Lilian Maria. Wada MY, Jeffrey L. Jones, Suely H. Tuboi, Eduardo H. Carmo, Walter Massa Ramalho, Natal J. Camargo, Ronaldo Trevisan, Regina M. T. Graça, Alexandre J. da Silva, Iaci Moura, J.P. Dubey, and Denise O. Garrett. Waterborne Toxoplasmosis, Brazil, from Field to Gene. Emerg Infect Dis 2006 Feb; 12(2): 326–329. doi: 10.3201/eid1202.041115 . Waterborn epidemics of toxoplasmosis in Brazil.
•• McLeod R, Frenkel JK, Estes RG, Cohen H, Mack DG, Eisenhauer PB, Gibori G. Subcutaneous and intestinal vaccination with tachyzoites of Toxoplasma gondii and acquisition of immunity to peroral and congenital toxoplasma challenge. J Immunol. 1988;140(5):1632–7 Live vaccine and model to protect against Toxoplasma infection in mice.
El Bissati K, Zhou Y, Paulillo S, Raman SK, Karch C, Roberts CW, Burkhard P, McLeod R. Novel protein nanovaccine confers robust immunity against Toxoplasma. Nature (NPJ) Vaccines. 2017;2:24. https://doi.org/10.1038/s41541-017-0024-6Self-assembling nanoparticle vaccine created using immunosense priciples creates a powerful vaccine tailored to protect humans but the principles can also incorporated full length proteins effective for immunizing other species.
Zhou Y. Melo M, Weiss R, El Bissati K, Irvine D, McLeod R, RNA replicon vaccines protect against toxoplasmosis. Immunosense and SAG1 in a noel SAPN vaccine with a new Toxoplasma CD4 eliciting peptide. 2022. In preparation. RNA replicons created using immunosense principles effectively immunize against T. gondii but SAG1 is most critical when combined with RNA encoding the peptides, emphasizing importance of SAG1 as an immunogen in future vaccines.
Zhou Y, El Bissati K, Reed S, Fox C, Alexander J, Sidney J, Sette A, Burkhard P, McLeod R. Adjuvanting designer SAPN vaccines with conventional adjvuants demonstrates superiority of GLA-SE and inability to combine the adjuvant CPG and GLA-SE. Designer vaccines to protect humans against toxoplasmosis cannot be adjuvanted with cpg and gla-se together but are effective with one or the other adjuvants.
Waldman, B.S., Schwarz, D., Wadsworth, M.H., Saeij, J.P. Shalek, A.K., Lourido, S., 2019. Identification of a master regulator of differentiation in Toxoplasma. BioRxiv660753. Available from: https://doi.org/10.1101/660753. Regulator of bradyzoite stage switch discovered.
Elbissati K, Raczy M, ZhouY, Weber C, Solaki A, Reed S, Fox C, Alexander J, Sidney J, Sette A, Burkhard P, Hubbel J, McLeod R. In preparation 2022. Creation of a “plug and play” strategy to create designer vaccines to protect humans and other species. GLA-se and immunosense SAPN create a potent vaccine against toxoplasmosis in HLA transgenic mice.
Chalal JS, et al Dendrimer-RNA nanoparticles generate protective immunity against lethal Ebola, H1N1 influenza, and Toxoplasma gondiichallenges with a single dose 2016 Jul 5. https://doi.org/10.1073/pnas.1600299113 PMCID: PMC4961123 PMID: 27382155. Venezuelan Equine Virus (VEEV)-based modified dendrimer nanoparticle RNA (MDNP RNA) vaccine protects against death due to Pru with HGXPRT strain Toxoplasma gondii. RNA replicons encoding full length SAG1, SAG2A, AMA1, GRA6, ROP2A, and ROP18, protect C57Bl6 mice for 175 days post challenge against this strain when replicon is incorporated in polyethylene glycol lipid nanoparticle.
Lai B-S, Witola WH, Bissati K, El Zhou Y, Mui E, et al. Molecular target validation, antimicrobial delivery, and potential treatment of Toxoplasma gondii infections. Proc Natl Acad Sci U S A. 2012;109(35):1418214187 Peptide or vivo morpholinos targeting essential parasite molecules such as DHFR, ENR, and Apetela 2 transcription factors can treat toxoplasma infection.
Tipparaju SK, Muench SP, Mui EJ, Ruzheinikov SN, Lu JZ, Hutson SL, Kirisits MJ, Prigge ST, Roberts CW, Henriquez FL, Kozikowski AP, Rice DW, Mcleod RL. Identification and development of novel inhibitors of Toxoplasma gondii enoyl reductase. J Med Chem. 2010;53:6287–300 Novel inhibitors of toxoplasma type ii fatty acid synthesis can treat toxoplasmosis.
Mazumdar JH, Wilson E, Masek KA, Hunter C, Striepen B. Apicoplast fatty acid synthesis is essential for organelle biogenesis and parasite survival in Toxoplasma gondii. Proc Natl Acad Sci U S A. 2006;103:13192–7 Type 2 fatty acid synthesis (fas) is essential for parasite survival and organelle biogenesis.
Welsch ME, Zhou J, Gao Y, Yan Y, Porter G, Gautam Agnihotri G, Yingjie Li YM, Lu H, Chen Z, Thomas SB. Discovery of Potent and Selective Leads against Toxoplasma gondii Dihydrofolate Reductase via Structure-Based Design. ACS Med Chem Lett. 2016, 7(12):1124–9. https://doi.org/10.1021/acsmedchemlett.6b00328Targeting Toxoplasma DHFR creates a potent inhibitor of T. gondii tachyzoites currently held by Vyera.
Mui EJ, Schiehser GA, Milhous WK, Hsu H, Roberts CW, Kirisits M, Muench S, Rice D, Dubey JP, Fowble JW, Rathod PK, Queener SF, Liu SR, Jacobus DP, McLeod R. Novel Triazine JPC-2067-B Inhibits Toxoplasma gondii In Vitro and In Vivo. PLoS Negl Trop Dis. 2008;2:e190 Novel triazine is a potent inhibitor nanomolar inhibitor of T. gondii tachyzoites as effective as a single anti-parasitic ompound as pyrimethamine and sulfadiazine acting synergistically together.
Samuel BU, Hearn B, Mack D, Wender P, Rothbard J, Kirisits MJ, Mui E, Wernimont S, Roberts CW, Muench SP, Rice DW, Prigge ST, Law AB, McLeod R. Delivery of antimicrobials into parasites. Proc Natl Acad Sci U S A. 2003;100:14281–6 Transductive peptides can deliver small molecules into tachyzoites and encysted bradyzoites creating potent inhibitors of T. gondii.
Zhou Y, Fomovska A, Muench S, Lai BS, Mui E, Mcleod R. Spiroindolone that inhibits PfATPase4 is a Potent, Cidal Inhibitor of Toxoplasma gondii tachyzoites in vitro and in vivo. Antimicrob Agents Chemother. 2014;58(3):1789-92. Spiroindolone that inhibits ATPase 4 is a cidal inhibitor of T. gondii tachyzoites. VivoPMO also is effective.
Fomovska A, Huang Q, El Bissati K, Mui EJ, Witola WH, Cheng G, Zhou Y, Sommerville C, Roberts CW, Bettis S, Prigge ST, Afanador GA, Hickman MR, Lee PJ, Leed SE, Auschwitz JM, Pieroni M, Stec J, Muench SP, et al. Novel N-benzoyl-2-hydroxybenzamide disrupts unique parasite secretory pathway. Antimicrob Agents Chemother. 2012;56:2666–82. https://doi.org/10.1128/AAC.06450-11Small molecule screen identifies a hydroxybenzamide that disrupts the T. gondii secretory pathway creating a potent inhibitor.
Smith D et al Toxoplasma TgATG9 is critical for autophagy and long-term persistence in tissue cysts eLife Apr 27, 2021. Autophagy protein TgATG9 is critical for long term persistence of T. gondii cysts.
Khan I, Huang et al. CD8 T cells cry for help. Front Cell Infect Microbiol. 2019;9:136. https://doi.org/10.3389/fcimb.2019.00136 BLIMP regulates 41BB mediated exhaustion of T cells that can be corrected by agonist antibody to 41BB. This eliminates encysted organisms which could make it possible to eliminate remaining tahyzoites by waking up protective immunologic mechanisms and targeting tachyzoites.
•• Souza SP, Splitt SD, Alvarez JA, Wizzard S, Wilson JN, Luo Z, Baumgarth N, Jensen, KDC NFkBid is required 1 for immunity and antibody responses to Toxoplasma gondii bioRxiv preprint https://doi.org/10.1101/2020.06.26.174151. A “collaborative cross” of mice demonstrates that hypervirulent South American parasite escapes protective immunological mechanisms effective against Type I, II, III parasites. Bumble mice with a difference in NFkBid also are not protected. These studies demonstrate the importance of NKcells and specific isotypes of antibody in protection against toxoplasmosis.
Borrmann S, Peter G. Kremsner PG et al. Fosmidomycin plus Clindamycin for Treatment of Pediatric Patients Aged 1 to 14 Years with Plasmodium falciparum Malaria. Antimicrobial Agents and ChemotherapyVolume 50, Issue 8, August 2006, Pages 2713-2718 https://doi.org/10.1128/AAC.00392-06. Inhibitor of mevalonate pathway discovered by Jomaa and Soldati inhibits Toxoplasma and Plasmodia. When administered with clindamycin, a delayed acting inhibitor is effective but has hematologic toxicity in humans.
Ismael AB, Dimier-Poisson I, Lebrun M, Dubremetz JF, Bout D, Mévélec MN. Mic1-3 knockout of Toxoplasma gondii is a successful vaccine against chronic and congenital toxoplasmosis in mice. J Infect Dis. 2006;194(8):1176–83 Knockout of microneme proteins creates live attenuate organism that functions well to protect mice against toxoplasmosis including congenital infection.
•• Dimier-Poisson I, Carpentier R, Nguyen T, Dahmani F, Ducournau C, Betbeder D. Porous nanoparticle as delivery system of complex antigens for an effective vaccine against acute and chronic Toxoplasma gondii infection. Biomaterials. Remarkable formulation of RH parasite lysate in a nanoparticle administered intranasally protects mice, sheep and primates in a zoo ending an epidemic of deaths due to toxoplasmosis in susceptible new world primate colonies in zoos across France. Creation of a vaccine capable of protecting multiple species of mammals. Remarkable protection with practical proof in French zoos for primates.
•• El Bissati K, Roberts CW, McLeod R. Adjuvanted multi-epitope vaccines protect HLA-A*11:01 transgenic mice against Toxoplasma gondii. JCI Insight. 2016;1(15):e85955. https://doi.org/10.1172/jci.insight.85955Combining T. gondii peptides mapped as important in immunosense system studies against toxoplasmosis in HLA Class I transgenic mice are potent as a polypeptide vaccine when admistered to these mice combined with a universal peptide eliciting CD4+T cells and GLA-SE a nanoemulsion adjuvant now in clinical use that stimulates TLR4.
•• Lourido, S., Jeschke, G.R., Turk, B.E., Sibley, L.D., 2013.Exploiting the unique ATP-binding pocket of toxoplasmacalcium-dependent protein kinase 1 to identifyits substrates. ACS Chem Biol. 8 (6), 1155-1162. Available from: https://doi.org/10.1021/cb400115y. Calcium dependent protein kinases are molecular targets in tachyzoite and encysted bradyzoites leading to development of small molecule inhibitor “lead compound” currently held by Vyera.
•• Karanovic D, Michelow IC, Hayward AR, DeRavin SS, Delmonte OM, Grigg ME, Dobbs AK, Niemela JE, Stoddard J, Alhinai Z, Rybak N, Hernandez N, Pittaluga S, Rosenzweig SD, Uzel G, Notarangelo LD. Disseminated and Congenital Toxoplasmosis in a Motherand Child with Toxoplasma Infections in Primary Immunodeficiencies. Front Immunol. 2019;10:77. https://doi.org/10.3389/fimmu.2019.0007Summarizes and identifies genes and pathways in which they function where mutations confer susceptibility to human toxoplasmosis.
•• Naranjo-Galvis CA, de-la-Torre A, Mantilla-Muriel LE, Beltrán-Angarita L, Elcoroaristizabal-Martín X, McLeod R, Alliey-Rodriguez N, Begeman IJ, López de Mesa C, Gómez-Marín JE, Sepúlveda-Arias JC. Genetic Polymorphisms in Cytokine Genes in Colombian Patients with Ocular Toxoplasmosis. Infect Immun. 2018;86(4):e00597-17. https://doi.org/10.1128/IAI.00597-17Identifies the importance of cytokine genes in protection against toxoplasmosis in Colombia.
•• Perce-da-Silva, D de Souza, Thays Euzebio J; Aleixo, Quintella do CoutoAL; Motta J; Ribeiro-Alves, M; Oliveira Ferreira, J de; Porto, Cristóvão de Moraes Sobrino L; Banic DM; Reis Amendoeira MR Influence of Activating and Inhibitory Killer Immunoglobulin-Like Receptors (KIR) genes on the recurrence rate of ocular toxoplasmosis in Brazil. BioRx. https://doi.org/10.1101/2020.09.16.299446; Identifies natural killer cell receptors in protection against recurrence of ocular toxoplasmosis in humans in Brazil.
•• Roberts F, Roberts CW, Johnson JJ, Kyle DE, Krell T, Coggins JR, Coombs GH, Milhous WK, Tzipori S, Ferguson DJ, Chakrabarti D, McLeod R. Evidence for the shikimate pathway in apicomplexan parasites. Nature. 1998;393:801–5 Plant-like metabolic pathways in apicomplexan parasites can be targeted. Apicomplexan parasites are mosaics of metabolic pathways identifying unique ways to target organellar and cytoplasmic pathways.
•• Zuther E, Johnson JJ, Haselkorn R, McLeod R, Gornicki P. Growth of Toxoplasma gondii is inhibited by aryloxyphenoxypropionate herbicides targeting acetyl-CoA carboxylase. Proc Natl Acad Sci U S A. 1999;96:13387–92 Targetting the plant-like acetyl-CoA carboxylase with herbicides known to inhibit this enzyme in weeds identifies two classes of small molecules capable of inhibiting apicomplexan parasites through targeting enzymes stored in the chloroplast like organelle inherited from an ancient progenitor Copydelia demonstrating this plant-like endosymbiotic organelle can be targeted. This suggests the possibility of targeting other unique organellar constituents and phylogenetically genetically distinct molecules including plant-like transcription factors as in McPhillie reference above as “Achilles heels” where these parasites are susceptible to unique methods of inhibiting these parasites.
•• Doggett JS, Nilsen A, Forquer I, Wegmann KW, Jones-Brando L, Yolken RH, Bordón C, Charman SA, Katneni K, Schultz T, Burrows JN, Hinrichs DJ, Meunier B, Carruthers VB, Riscoe MK. Endochin-like quinolones are highly efficacious against acute and latent experimental toxoplasmosis. Proc Natl Acad Sci U S A. 2012;109:15936–41. https://doi.org/10.1073/pnas.1208069109Effect of endochin-like quinolomes against cytochrome bc in Toxoplasma inhibits encysted bradyzoites in mouse models although inhibition is not complete.
•• Kortagere S, Mui E, McLeod R, Welsh WJ. Rapid discovery of inhibitors of Toxoplasma gondii using hybrid structure-based computational approach. J Comput Aided Mol Des. 2011;25:403–11. https://doi.org/10.1007/s10822-011-9420-6Targeting Myosin in Toxoplasma and using a computational approach with medicinal chemistry creates an inhibitor of Toxoplasma tachyzoites.
Yang S, Parmley SF. Toxoplasma gondii expresses two distinct lactate dehydrogenase homologous genes during its life cycle in intermediate hosts. Gene. 1997;184:1–12. https://doi.org/10.1016/S0378-1119(96)00566-5Chatcterization of stage specific lactic dehydrogenases in Toxoplasma gondii.
•• Dando C, Schroeder ER, Hunsaker LA, Deck LM, Royer RE, Zhou X, Parmley SF, Vander Jagt DL. The kinetic properties and sensitivities to inhibitors of lactate dehydrogenases (LDH1 and LDH2) from Toxoplasma gondii: comparisons with pLDH from Plasmodium falciparum. Mol Biochem Parasitol. 2001;118:23–32. https://doi.org/10.1016/S0166-6851(01)00360-7Targeting Lactate dehydrogenases of apicomplexan parasites.
•• El Bissati K, Zhou Y, Paulillo SM, Raman SK, Karch CP, Reed S, Estes A, Estes A, Lykins J, Burkhard P, & McLeod R. Engineering and characterization of a novel Self Assembling Protein for Toxoplasma peptide vaccine in HLA-A*11:01, HLA-A*02:01 and HLA-B*07:02 transgenic mice. Scientific Reports (Nature) September 2020. Potent imunosense protein self-assembling nanoaccine adjuvanted with GLA-SE protects HLA transgenic mice demonstrating effect of peptides where genetic restriction demonstrates protection is operative for three HLA Class I supermotifs.
Del Valle Mojica, C. McLeod, R. et al. Late diagnosis of congenital toxoplasmosis with macrocephaly in two dizygotic twins after incidental detection of leukocoria: a case report. J Peds Infectious Diseases. 2021. Late symptomatic infection is treated medically in dizygotic twins.
•• Mack DG, McLeod R, Stark B. RNAse P of T. gondii. Characterization of ribonuclease P from Toxoplasma gondii European Journal of Protistology. 32: 96-103. https://doi.org/10.1016/S0932-4739(96)80044-7. RNA enzymatic activity in Toxoplasma.
Cong H, Mui EJ, Witola WH, Sidney J, Alexander J, Sette A, Maewal A, El Bissati K, Zhou Y, Suzuki Y, Lee D, Woods S, Sommerville C, Henriquez FL, Roberts CW, McLeod R. Toxoplasma gondii HLA-B*0702-restricted GRA7(20-28) peptide with adjuvants and a universal helper T cell epitope elicits CD8(+) T cells producing interferon-γ and reduces parasite burden in HLA-B*0702 mice. Hum Immunol. 2012;73:1–10.
•• Cong H, Mui EJ, Witola WH, Sidney J, Alexander J, Sette A, Maewal A, McLeod R. Human immunome, bioinformatic analyses using HLA supermotifs and the parasite genome, binding assays, studies of human T cell responses, and immunization of HLA-A*1101 transgenic mice including novel adjuvants provide a foundation for HLA-A03 restricted CD8+T cell epitope based, adjuvanted vaccine protective against Toxoplasma gondii. Immunome Res. 2010;6:12.
•• Cong H, Mui EJ, Witola WH, Sidney J, Alexander J, Sette A, Maewal A, McLeod R. Towards an immunosense vaccine to prevent toxoplasmosis: protective Toxoplasma gondii epitopes restricted by HLAA*0201. Vaccine. 2011;29:754–62.
•• McLeod R, Lykins J, Noble AG, Rabiah P, Swisher C, Heydemann P, McLone D, Frim D, Withers S, Clouser F, Boyer K. Management of congenital toxoplasmosis. Curr Ped Rep. 2014;2(3):166–94 Review of management of congenital toxoplasmosis prior to 2014.
Van Wormer E, Fritz H, Shapiro K, Mazet JA, Conrad PA. Molecules to modeling: Toxoplasma gondii ooxyts at the human-animal-environment interface. Comp Immunol Microbiol Infect Dis. 2013;36(3):217–31 One health importance.
•• McLeod R, Kieffer F, Sautter M, Hosten T, Pelloux H. Why prevent, diagnose and treat congenital toxoplasmosis? Mem Inst Oswaldo Cruz. 2009;104:320–44 Importance of diagnosis, prevention, and treatment.
Olariu TR, Remington JS, McLeod R, Alam A, Montoya JG. Severe congenital toxoplasmosis in the United States: clinical and serologic findings in untreated infants. Pediatr Infect Dis J. 2011;30:1056–61 Reemphasizes severity of congenital toxoplasmosis in USA.
•• Torgerson PR, Mastroiacovo P. The global burden of congenital toxoplasmosis: a systematic review. Bull World Health Organ. 2013;91(7):501–8. Emphasizes frequency and burden of congenital toxoplasmosis in the world and its considerable cost and suffering it causes. Early Panama study.
Sousa OE, Saenz RE, Frenkel JK. Toxoplasmosis in Panama: a 10-year study. Am J Trop Med Hyg. 1988;38(2):315–22.
Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol. 2009;39:1385–94 Prevalence data globally in earlier decades.
Rosso F, Les JT, Agudelo A, Villalobos C, Chaves JA, Tunubala GA, Messa A, Remington JS, Montoya JG. Prevalence of infection with Toxoplasma gondii among pregnant women in Cali, Colombia, South America. Am J Trop Med Hyg. 2008;78(3):504–8 Prevalence in Cali Colombia 2008.
Castro AT, Congora A, Gonzalez ME. Toxoplasma gondii antibody seroprevalence in pregnant women from Villavicencio, Colombia. Orinoquia. 2008;12:91–100 Prevalence Colombia.
Barrera AM, Castiblanco P, Gomez-Marin JE, Lopez MC, Ruiz A, Moncada L, Reyes P, Corredor A. Toxoplasmosis adquirida durante el embarazo, en el Instituto Materno Infantil en Bogotá. Rev Sal Púb. 2002;4(3):286–93 Prevalence Colombia.
Zapata M, Reyes L, Holst I. Disminución en la prevalencia de anticuerpos contra Toxoplasma gondii en adultos del valle central de Costa Rica. Parasitol Latinoam. 2005;60:32–7. Prevalence.
Arranz-Solís D, Cordeiro C, Young LH, Dardé ML, Commodaro AG, Grigg ME, Saeij JPJ. Serotyping of Toxoplasma gondii Infection Using Peptide Membrane Arrays. Front Cell Infect Microbiol. 2019;9:408. https://doi.org/10.3389/fcimb.2019.00408 Serotyping.
•• Arranz-Solís D, Carvalheiro CG, Zhang ER, Grigg ME, Saeij JPJ. Toxoplasma GRA peptide-specific serologic fingerprints discriminate among major strains causing toxoplasmosis. Front Cell Infect Microbiol. 2021;11:621738 Advanced serotyping.
Pomares C, Devillard S, Holmes TH, Olariu TR, Press CJ, Ramirez R, Talucod J, Estran R, Su C, Dubey JP, Ajzenberg D. Genetic characterization of Toxoplasma gondii DNA samples isolated from humans living in North America: an unexpected high prevalence of atypical genotypes. J Infect Dis. 2018;218(11):1783–91 Genotype snapshot varied in US.
•• Vasconcelos-Santos DV, Azevedo DO, Campos WR, Oréfice F, Queiroz-Andrade GM, Carellos ÉV, Romanelli RM, Januário JN, Resende LM, Martins-Filho OA, Carneiro AC. Congenital toxoplasmosis in southeastern Brazil: results of early ophthalmologic examination of a large cohort of neonates. Ophthalmology. 2009;116(11):2199–205 High prevalence of congenital toxoplasmosis and retinal disease in Brazil. Epidemics occur associated with water.
••Lago EG. Risk factors for congenital toxoplasmosis are not always obvious. ACOG. 2006;194(3):907–8. https://doi.org/10.1016/j.ajog.2005.07.021Risk factors not always clear.
Endres MM, Scheeren MFDC, Fiori HH. Ocular Outcome of Brazilian Patients With Congenital Toxoplasmosis. Pediatr Infect Dis J. 2021;40(1):e21–7. https://doi.org/10.1097/INF.0000000000002931Part of a series of papers by Lago et al, Lago and Dubey demonstrating severity of congenital Toxoplasmosis in Brazil, manifestations, and efficacy of treatment.
Acknowledgments
We gratefully acknowledge the following organizations and people for their financial, logistical, and/or technical support during our work on this project.
Panama: Thanks to the Secretaría Nacional de Ciencia, Tecnología e Innovación (SENACYT), the Sistema Nacional de Investigación (SNI), the Institute for Scientific Research and High Technology Services of Panama (INDICASAT), Hospital del Niño, Hospital Santo Tomás, and Roche Diagnostics International Ltd. Special thanks to the medical staff of the high-risk pregnancy and infectious disease wings of Hospital Santo Tomás, especially Aris Caballero de Mendieta, Susana Frías, Dario Beneditto, Edwin Ortiz, Carlos Moreno, Ana Belen Arauz, Monica Pachar, Eyra Garcia, as well as to the nurses for all their logistical support.
We thank little Henry Arosemena, who was the impetus for starting the program in Panama, and the Arosemena family for their support of educational initiatives in Panama.
Colombia: Thanks to the Grupo de Investigación en Parasitología Molecular (GEPAMOL) at the University of Quindío, to Richard James Orozco González, and to Hospital del Sur and Hospital San Juan de Dios in Armenia, Colombia.
United States: Thanks to Dr. Brian Callender, Dr. Jeanne Farnan, Dr. Olofunmilayo Olopade, Absera Melaku, MPH, Kristyna Hulland, MS, Dr. Susan Duncan, and Dr. John Schneider for facilitating summer research through the Summer Research Program at the Pritzker School of Medicine at the University of Chicago.
We appreciate Aaron Ponsler’s suggestion at a Thrasher Foundation site visit at Stanford University that the LDBio could do the most good if it were cleared by the FDA and waived by CLIA.
We thank all those in the National Collaborative Chicago-Based Congenital Toxoplasmosis Study (NCCCTS) who helped build and sustain programs in the United States.
We especially thank the many families who participated in and/or encouraged these initiatives, and their primary care physicians. We give special thanks to these participant families and their physicians without whom this NCCCTS could not have been performed.
We thank all those who traveled to Springfield IL to begin gestational screening in the United States, recognizing the importance this would have had for their families.
We thank those who worked with the NCCCTS in the earlier years including Marilyn Mets, William Mieler, Michael Grassi, Michael Kip, Hassan Shah, Diane Patton, Vicky Aithchison, Holly McGinnis, Randee Estes, Douglas Mack, Michael Kirisits, Adrian Esquivel, Toria Trendler, Joseph MCammon, Simone Cezar, Jessica Coyne, Daniel Lee, Diana Chamot, Jane Babiarz, Veena Arun, Laura Phan, as well as Daniel Johnson, Adil Javed and others as reflected in the author lists in references 3-50. Their contributions to the initial phases of this work were substantial and valuable.
We thank additional authors and members of the NCCCTS group Barbara Danis, Mark Stein, Linda Pfiffner, Jeanne Perkins, Sanford Meyers, Balaji Gupta, Ahmed Abdelsalam, Huiyuan Zhang, John Marcinak, Saeid Mojatahedi, Dianna Bardo, Marisha Humphries, Douglas Mack, Michael J. Kirisits, Diana Chamot, Ronald Thisted, Carina Yang, Delilah Burrowes, and John Collins (University of Chicago, Chicago, IL); Lazlo Stein (Northwestern University, Chicago; deceased); Andrew Suth (Argosy University, Chicago); Audrey Cameron (Mount Sinai Hospital, Chicago); Marie Weissbourd (Northwestern University Hospital, Chicago); Joyce Hopkins (Illinois Institute of Technology, Chicago); Dushyant Patel (Michael Reese Medical Center, Chicago); and others.
We thank Jack Remington and those in the Remington serology laboratory who performed the serologic testing for participants in the NCCCTS establishing the diagnosis for each participant as part of their clinical care, allowing the NCCCTS to be based on rigorous, meticulous diagnostic criteria.
We thank the Data Safety Monitoring Board members, John Flagherty, Richard Chappell, David Mittelmam, Dana Bradzunias.
We thank those working with us to establish gestational screening for perinatal infections and to develop and test WHO-compatible POC tests in the United States, France, and Morocco, Mohamed Rhajaoui, Amina Barkat, Hua Cong, and Bo Shiun Lai.
Additionally, we thank Shaun Carey, James Lynch, Millie Malekar, others in the IRB office, Jim Rago and Sam Campbell for photography, David G Goodwin, Colin Shephard, Ribhi M. Shawar, Matthew Macgilvray, and Steven Gitterman for their guidance with FDA processes, NIH DMID Program, Officers Michael Gottlieb, F. Lee Hall, Stephanie James, and John Rogers for many suggestions, Jean Hickman for assistance, additional Morocco Group colleagues including Mohamed Rhajaoui working alongside and with us, for their help and support in implementing prenatal screening for toxoplasmosis in Morocco. We thank Iris Ramirez for her contribution to screening. We thank Tom Lint for assistance with many aspects of the study.
France/Austria: Many thanks to our French and Austrian colleagues, who paved the way and worked with us in understanding the importance of prompt gestational screening, treatment, and prevention of congenital toxoplasmosis.
Funding
Additional thanks for funding from the Jeff Metcalf Internship Program, the Margaret P Thorp Scholarship Fund, the American College of Obstetricians and Gynecologists for their Medical Student Award, the National Institute of Diabetes and Digestive and Kidney Diseases for their Grant #T35DK062719-30, the American Society of Tropical Medicine and Hygiene for their Benjamin H. Kean Fellowship, the National Institutes of Health for their Division of Microbiology and Infectious Diseases Grants to RMc #R01 AI2753,RO1 16945, AI08749-01A1 BIOL-3 , U01 AI77887, U01 AI082180, TMP R01-AI071319, the Thrasher Research Fund for their E.W. “Al” Thrasher Award, the Kiphardt Global-Local Health Seed Fund Award of the University of Chicago, SENACYT, the Research to Prevent Blindness Foundation, March of Dimes (6-528), the FDA , the Pillsbury Foundation, Michael Reese, Physicians Research and Education Foundation, the Fulbright Scholar Awards (Craig Roberts, Kamal ElBissati, Dorota Nowakowska), the Pathological Society of Great Britain and Northern Ireland Travel Award, (Fiona Roberts) the WHO DIF, and the Stanley Foundation. This work was supported in part by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, NIH (Michael Grigg).
We are grateful to Toxoplasmosis Research Institute, Taking out Toxo, Network for Good, the Cornwell Mann Family Foundation, The Rodriguez family, The Samuel family and Running for Fin, the Buchanan Family Foundation, the Morel, Rooney, Mussalami, Kapnick, Taub, Engel, Harris, Quinn, and Drago families, Pritzker, the Hyatt Hotels Foundation, United Friendly Skies, American, Southwest, Braniff, Angel Flight, Pan Am, Horizon Britt Canada, and other airlines for complimentary transportation for NCCCTS participants.
We gratefully acknowledge the Susan and Richard Kiphart Family Foundation for providing funding for open access charges.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Denis Limonne Pharm D, PhD and Raphael Piarroux Pharm D, PhD, are the owner and Scientists at LDBio. A patent application was submitted in the United States for the development of the whole blood point of care test with the scientists at the University of Chicago to insure its continued high-quality performance and reproducibility of the results described herein. In the United States and Panama in the more recent studies the LDBio kit was provided for the studies without charge by D Limonne. The Roche kit was provided without charge in Panama. For the predicate test costs for the comparison test for 70 consecutive persons for the feasibility clinical trial the cost of performing the Biorad IgG and IgM tests was provided by Kiphard Foundation. Kamal El Bissati is heading the initiatives to prevent toxoplasmosis in Morocco. Patents have been obtained for the medicine, anti-sense, vaccine, biomarker development work to facilitate their development toward clinical use and sustain availability if/when they are used in clinical practice. RMcLeod was reimbursed for time in performing a literature review concerning Spiramycin by Sanofi Pasteur in accordance with Sunshine laws. RMcLeod (with her colleagues) shared first prize merit award in the Alzgerm initiative to identify the highest quality and rigorously developed and described work demonstrating that a pathogen can initiate, progress and contribute to neurodegenerative diseases, and that there can be effect of this chronic active infection on cognition, motor function and other disease processes. This monetary prize was used to further this ongoing work.
Competing Interests
There are no other disclosures and no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mariangela Soberón Felín, Kanix Wang, Andrew Grose, Aliya Moreira, Karen Leahy, Ying Zhou, Fatima Alibana Clouser, Maryam Siddiqui, Nicole Leong, Perpetua Goodall, Mahmoud Ismail, Monica Christmas, Stephen Schrantz, Zuleima Caballero, Ximena Norero, Dora Estripeaut, David Ellis, Catalina Raggi, Catherine Castro, Davina Moossazadeh, Margarita Ramirez, Abhinav Pandey, Kevin Ashi, Samantha Dovgin, Ashtyn Dixon, Xuan Li, Ian Begeman, Sharon Heichman, Joseph Lykins, Delba Villalobos-Cerrud, Lorena Fabrega, José Luis Sanchez Montalvo, Connie Mendivil, Mario R. Quijada, Silvia Fernández-Pirla, Digna Wong, Mayrene Ladrón de Guevara, Carlos Flores, Jovanna Borace, Anabel García, Natividad Caballero, Claudia Rengifo-Herrera, Maria Theresa Moreno de Saez, Michael Politis, Kristen Wroblewski, Theodore Karrison, Stephanie Ross, Mimansa Dogra, Vishan Dhamsania, Nicholas Graves, Marci Kirchberg, Kopal Mathur, Ashley Aue, Carlos M. Restrepo, Alejandro Llanes, German Guzman, Arturo Rebellon, Kenneth Boyer, Peter Heydemann, A. Gwendolyn Noble, Charles Swisher, Peter Rabiah, Shawn Withers, Teri Hull, Chunlei Su, Paul Latkany, Ernest Mui, Daniel Vitor Vasconcelos-Santos, Alcibiades Villareal, Ambar Perez, Carlos Andrés Naranjo Galvis, Mónica Vargas Montes, Nestor Ivan Cardona Perez, Morgan Ramirez, Cy Chittenden, Edward Wang, Laura Lorena Garcia-López, Juliana Muñoz-Ortiz, Nicolás Rivera-Valdivia, María Cristina Bohorquez-Granados, Gabriela Castaño de-la-Torre, Guillermo Padrieu, Daniel Celis-Giraldo, John Alejandro Acosta Dávila, Elizabeth Torres, Manuela Mejia Oquendo, José Y. Arteaga-Rivera, Dan L. Nicolae, Andrey Rzhetsky, Nancy Roizen, Eileen Stillwaggon, Larry Sawers, Francois Peyron, Martine Wallon, Emanuelle Chapey, Pauline Levigne, Carmen Charter, Migdalia De Frias, Jose Montoya, Cindy Press, Raymund Ramirez, Despina Contopoulos-Ioannidis, Yvonne Maldonado, Oliver Liesenfeld, Carlos Gomez, Kelsey Wheeler, Samantha Zehar, James McAuley, Denis Limonne, Raphael Piarroux, Vera Tesic, Kathleen Beavis, Ana Abeleda, Mari Sautter, Bouchra El Mansouri, Adlaoui El Bachir, Fatima Amarir, Kamal El Bissati, Alejandra de-la-Torre, Gabrielle Britton, Jorge Motta, Eduardo Ortega-Barria, Isabel Luz Romero, Michael Grigg, Jagannatha Rao Kosagisharaf, Xavier Sáez Llorens, Osvaldo Reyes and Rima McLeod contributed uniquely, differently to this work as did those acknowledged, some in major ways in critical, foundational studies
This article is part of the Topical Collection on International Health
Supplementary Information
ESM 1
(PDF 9974 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Felín, M.S., Wang, K., Moreira, A. et al. Building Programs to Eradicate Toxoplasmosis Part I: Introduction and Overview. Curr Pediatr Rep 10, 57–92 (2022). https://doi.org/10.1007/s40124-022-00269-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-022-00269-w