Abstract
Introduction
Post-keratoplasty glaucoma (PKG) is a major complication following penetrating keratoplasty (PKP) for congenital corneal opacity (CCO). This study aims to assess the preoperative structural risk factors for PKG following PKP for CCO using ultrasound biomicroscopy (UBM).
Methods
Pediatric patients with CCO who underwent preoperative UBM and primary PKP were enrolled. Patients with anterior segment operation history or with a follow-up duration less than 12 months were excluded. The structural features of the anterior segment including central corneal thickness, anterior chamber depth, angle closure range (ACR), anterior synechia range, maximum iridocorneal adhesion length, abnormal iridocorneal synechia, and lens anomalies were identified on UBM images. The medical histories were reviewed to identify clinical features. The incidence of PKG was assessed to determine significant structural and clinical risk factors.
Results
Fifty-one eyes of 51 pediatric patients with CCO were included. The median age at surgery was 8.0 months, and the mean follow-up duration was 33 ± 9 months. Eleven (21.6%) eyes developed PKG. The main structural risk factors were abnormal iridocorneal synechia (P = 0.015), lens anomaly (P = 0.001), and larger ACR (P = 0.045). However, a larger range of normal anterior synechia without involvement of the angle was not a significant risk factor. Preoperative glaucoma (P < 0.001) and higher intraocular pressure (P = 0.015) were clinical risk factors. A shallow anterior chamber was a unique risk factor for sclerocornea (P = 0.019).
Conclusions
Detailed preoperative examination of iridocorneal synechia, lens, and angle closure using UBM is critical for PKG risk assessment, surgical prognosis evaluation, and postoperative management in patients with CCO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
Congenital corneal opacity (CCO) is a congenital eye disease with a very poor prognosis. Penetrating keratoplasty (PKP) is the only treatment option for severe CCO, but pediatric PKP faces significant challenges. |
Post-keratoplasty glaucoma (PKG) is a major complication following PKP, yet there is a lack of effective prognostic indicators. |
Ultrasound biomicroscopy (UBM) was used in this study to assess the anterior segment features of the eyes of children with CCO to identify structural risk factors for PKG. |
What was learned from the study? |
The main structural risk factors for PKG in CCO eyes were abnormal iridocorneal synechia (P = 0.015), lens anomaly (P = 0.001), and larger angle closure range (P = 0.045). Preoperative glaucoma (P < 0.001) and higher intraocular pressure (P = 0.015) were the main clinical risk factors. |
For pediatric patients with CCO, particularly those with clinical risk factors, a detailed preoperative examination using UBM to assess iridocorneal synechia, lens, and angle closure range is crucial for the risk assessment of PKG. |
Introduction
Congenital corneal opacity (CCO) is a congenital ocular abnormality caused by multiple factors. A clinico-epidemiological survey of congenital eye malformations in Spain and the United States reported that 2.20–3.11 per 100,000 children were born with CCO [1, 2]. Severe deprivation amblyopia and even childhood blindness caused by CCO may occur, so keratoplasty is needed as early as possible [3]. CCO is one of the most common indications for pediatric penetrating keratoplasty (PKP) [4,5,6,7]. Compared with that in adult eyes, the difficulty of keratoplasty in pediatric eyes is greater due to less scleral rigidity and a crowded anterior chamber [8]. In addition, pediatric keratoplasties have a higher rate of graft failure [3, 9, 10]. Many relevant complications may cause graft failure, including glaucoma, infection, and rejection [8, 11].
Post-keratoplasty glaucoma (PKG) has been identified as the major complication and leading cause of irreversible graft failure after PKP [4, 12,13,14]. The incidence of PKG in pediatric eyes is 17.6–45.7%, and 68.0–83.8% of PKG cases progress to graft failure [1, 2, 4, 5, 15,16,17,18]. Several preoperative risk factors for PKG in adults have been identified, including age, preexisting glaucoma, and peripheral anterior synechia (PAS), and the indications for keratoplasty contribute to the poor prognosis (including acquired traumatic and regraft cases) [11, 19,20,21,22,23]. However, the effect of lens status (aphakia or pseudophakia) on the occurrence of PKG remains a subject of discussion [22]. In congenital cases, the risk factors may be different from those in other cases due to their unique pathogenesis, and the structural risk factors for PKG require further study.
Ultrasound biomicroscopy (UBM), which provides high-resolution images, is the only noninvasive choice for anterior segment imaging of eyes with CCO [7]. It is a valuable imaging technique for examining the structure of the anterior segment, including the cornea, iris, anterior chamber angle, lens trabecular meshwork, and ciliary body. Compared with light-dependent techniques for examining the anterior segment such as optical coherence tomography, ultrasound can penetrate opaque tissue, making UBM more suitable for preoperative evaluation, diagnosis, and management of eyes with CCO [7, 24,25,26,27]. Therefore, UBM has great potential for identifying the structural features of the anterior segment of eyes with CCO.
To date, there has been little discussion regarding the preoperative structural risk factors for PKG in eyes with CCO; such discussions may provide valuable guidance for surgery planning and management. Since 2008, we have performed approximately 40 pediatric keratoplasties each year. The significantly different surgical outcomes have raised concerns regarding the risk factors associated with a poor prognosis. In this study, UBM was used to detect the features of the anterior segments in eyes with opaque corneas, especially the anterior synechia, anterior chamber angle, and lens. The effects of the structural features on the development of PKG in eyes with CCO were evaluated.
Methods
Patients
This retrospective cohort study was conducted at Peking University Third Hospital, Beijing. The clinical data of patients with CCO, who were younger than 14 years, were studied retrospectively. These patients underwent preoperative UBM and primary PKP between November 2018 and June 2021 and were followed for more than 12 months. For patients who underwent bilateral PKP, only one eye was included randomly using a random number generator. Patients with a history of surgery that altered the anterior segment structure before PKP were excluded from this study. The study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2018244). The patients’ guardians provided consent at the time of treatment for their data to be used for future research purposes. Consent for publication was not applicable as our manuscript does not include identifiable information.
All patients’ medical histories were reviewed, and follow-up data were collected. The patients’ medical histories were reviewed for sex, age, surgery history, preoperative intraocular pressure (IOP), history of preexisting glaucoma, preoperative UBM images, preoperative slit-lamp microscopy images, preoperative axis length of the eye measured by B-scan, and operation notes. The patients’ medical records were also reviewed for follow-up data, including postoperative IOP and the features of both the graft and the graft bed.
Preoperative IOP was measured under anesthesia in the supine position using an iCare tonometer. For eyes with incomplete corneal opacities, IOP measurements were performed in the clear corneal area. The eye was diagnosed with preoperative ocular hypertension when the mean of three preoperative IOP measurements was higher than 21 mmHg. Preoperative glaucoma was diagnosed when an increase in ocular dimensions inconsistent with normal growth was observed with or without ocular hypertension [28]. Specifically, the increase in ocular dimensions included an abnormal corneal diameter (≥ 11 mm in newborns, ≥ 12 mm in pediatric patients younger than 1 year, and > 13 mm at any age) and an abnormal progression of axis length of the eye [28]. PKG was diagnosed as uncontrolled ocular hypertension after the withdrawal of steroid eye drops that required intervention with topical antiglaucoma drugs or surgical interventions.
UBM Examination Process
All patients included underwent UBM examinations before PKP. Sedation was induced with oral chloral hydrate (0.3–0.5 ml/kg) to maintain cooperation during the examination. An experienced technician conducted all the UBM examinations using an SW-3200L UBM (50 MHz; SUOER, Tianjin, China). The images were processed as described in our previous study [29]. In brief, oxybuprocaine hydrochloride was used for surface anesthesia, and a contact lens cup filled with multipurpose contact lens solution was placed in the conjunctival sac in the supine position. To ensure the completeness and accuracy of the UBM examinations, the technician conducted axial scans and radial scans to observe the position and morphology of the cornea, lens, and iris, respectively. Images of axial scanning, radial scanning (images at 3, 6, 9, and 12 o’clock), and specific anomalies were frozen and recorded. Ofloxacin eye drops were applied when the examination processes were finished.
Identification of Structural Features Using UBM
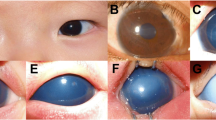
The following structural features were identified and recorded. (1) Central corneal thickness (CCT): The CCT was defined as the radial distance between the anterior and posterior central corneal surface (Fig. 1). (2) The anterior chamber depth (ACD) was defined as the radial distance between the central corneal endothelium and the anterior surface of the lens (Fig. 1). (3) Angle closure range (ACR): Angle closure was identified when the iris root was completely adherent to the posterior surface of the cornea from the anterior chamber angle to 500 μm anterior to the scleral spur, and the range of angle closure was recorded across quadrants. This feature was mainly identified and recorded by a technician under dynamic observation due to poor cooperation among pediatric patients. (4) Anterior synechia range (ASR): The anterior synechia was identified when the iris was adherent to the posterior surface of the cornea, and the range of the anterior synechia was recorded across quadrants. (5) Maximum iridocorneal adhesion length (MIAD): The MIAD was measured according to the method put forward by Hong et al. (Fig. 1) [30]. (6) Abnormal iridocorneal synechia: An abnormal iridocorneal synechia was identified when filamentous structures extended anteriorly from the thin iris to the posterior surface of the cornea (Fig. 2). (7) Lens anomaly: A lens anomaly was identified when lens dislocation, shape anomaly, or aphakia was observed. UBMScan, version 2.2.0.1 (SUOER, Tianjin, China), was used for measurement on the UBM examination images.
Ultrasound biomicroscopy and intraoperative findings of abnormal iridocorneal synechia. A Extensive filamentous structures extending anteriorly from the iris were observed. A strong echo was observed on the posterior surface of the cornea. B During penetrating keratoplasty, a large area of the iris was found to adhere tightly to the posterior surface of the cornea
Surgical Techniques
All PKP procedures were performed by the same experienced surgeon under general anesthesia, and some were combined with cataract extraction, goniosynechialysis, or limbal stem cell transplantation when necessary.
A Flieringa ring was used for global stabilization. Peripheral iridectomy was performed for most patients. The trephination diameter of the recipient cornea was adjusted according to the extent of the leukoplakia and diameter of the cornea. A tag line was incised along the estimated trephined zone into two-thirds the thickness of the cornea. A small amount of viscoelastic material was injected into the anterior chamber through the tag line to maintain the stability of the anterior chamber and the IOP, preventing the loss of intraocular contents. The opaque cornea was cut off along the tag line using corneal scissors. The iridocorneal adhesions and closed anterior chamber angle were separated using viscoelastic material if necessary. Then the viscoelastic material was rinsed out. A 0.5 mm oversized donor cornea was sutured to the plant bed using interrupted 10-0 nylon sutures. The incision was sutured watertight. In the end, dexamethasone and tobramycin were injected subconjunctivally, and TobraDex eye ointment was used.
Statistical Methods
IBM SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY, USA) was used for data analysis except for survival analysis. Quantitative variables are presented as the means ± standard deviations or medians (n, maximum, minimum) if not normally distributed, while categorical variables are presented as numbers and percentages. The Kolmogorov‒Smirnov test was used to assess the distribution of the data. The Mann‒Whitney U test was used to analyze ranked data and non-normally distributed data, while the t test was used for normally distributed data. The chi-square test was used for comparisons between categorical data.
Survival analyses were performed using GraphPad Prism version 9.3.0 for Windows (64-bit; GraphPad Software, San Diego, CA, USA). The Kaplan‒Meier method was used to construct survival curves. The log-rank test was performed and hazard rations (HRs) were calculated for statistical comparisons. P values < 0.05 were considered to indicate statistical significance.
Results
Demographic Data and Baseline Characteristics
Fifty-one eyes with CCO, comprising 27 (52.9%) right eyes and 24 (47.1%) left eyes, were included in the study. There were 22 (43.1%) male patients and 29 (56.9%) female patients. The median age at surgery was 8.00 (n = 51, 2.00, 127.00) months. Thirty (58.8%) of the patients had bilateral CCO, five of whom had systemic diseases, including cardiovascular anomalies (n = 3), duodenal stenosis (n = 1), and cheiloschisis (n = 1). The clinical diagnoses for the 51 eyes with CCO included Peters anomaly (n = 34, 66.7%) and sclerocornea (n = 17, 33.3%).
Nine (17.6%) eyes had preoperative glaucoma, of which seven had Peters anomaly and two had sclerocornea. The median corneal diameter of the eyes with preoperative glaucoma was 10.00 mm (n = 9, 5.00, 12.50; P = 0.012, U = 288.50, 95% confidence interval (CI) [−3.50, −0.50]). Only one of the nine eyes underwent antiglaucoma therapy (diode cyclophotocoagulation) before keratoplasty.
Two hundred and eighty preoperative UBM images of the 51 eyes were reviewed. The average central corneal thickness was 728 ± 215 (n = 51) μm. The average anterior chamber depth was 1377 ± 491 (n = 47) μm. The anterior chamber angles were open in 12 (23.5%) eyes, closed in less than two quadrants in 25 (49.0%) eyes, and closed in two or more quadrants in 12 (23.5%) eyes. The angle structure was not observed in two (3.9%) eyes due to poor cooperation. The iridocorneal synechiae involved less than two quadrants in 18 (35.3%) eyes and two or more quadrants in 30 eyes. Two (3.9%) eyes had no anterior adhesion. The average maximum iridocorneal adhesion length was 1513 ± 731 (n = 46) μm. Abnormal iridocorneal synechia was found in nine (17.6%) eyes, and lens anomalies were found in 11 (21.6%) eyes.
The average preoperative IOP was 19.5 ± 10.0 mmHg. PKP was accomplished in all eyes. Eleven (21.6%) of the patients underwent limbal stem cell transplantation, and seven (13.7%) underwent cataract surgery. None of the patients underwent combined glaucoma filtering surgery or diode cyclophotocoagulation. The median graft diameter was 6.25 (n = 51, 4.00, 11.00) mm.
Follow-Up of Patients with Post-keratoplasty Glaucoma
During the postoperative follow-up period (33 ± 9 months, ranging from 13 to 53 months), 11 (21.6%) eyes developed postoperative glaucoma (Table 1). Seven eyes developed postoperative glaucoma within 3 months after surgery. Filtering surgeries were performed on six eyes, diode cyclophotocoagulation was performed on two eyes, and an antiglaucoma drug therapy longer than 3 months was needed for three eyes.
Structural and Clinical Risk Factors for Post-keratoplasty Glaucoma in Congenital Corneal Opacity
Eyes with lens anomaly (P = 0.001, odds ratio (OR) = 6.37, 95% CI [2.27, 17.86]), abnormal iridocorneal synechia (P = 0.015, OR = 3.89, 95% CI [1.51, 10.00]), and PAS were likely to develop PKG (Table 2). All eyes with lens shape anomalies developed PKG (n = 4, P = 0.001). Interestingly, rather than range of anterior synechia (P = 0.624 in ASR and P = 0.978 in MIAD), larger range of angle closure (P = 0.045, U = 121.00, 95% CI [0.00, 1.00]) was the more important risk factor.
As to clinical features, preoperative glaucoma (P < 0.001, OR = 8.20, 95% CI [3.02, 22.22]) and higher IOP (P = 0.015, t = 2.522, 95% CI [1.64, 14.60]) were main risk factors. Peters anomaly and sclerocornea eyes had similar incidence rates (23.5% vs. 17.6%, P = 0.731, OR = 1.33, 95% CI [0.41, 4.39]).
Log-rank survival analysis revealed that lens anomaly (P < 0.001, HR = 10.41, 95% CI [2.10, 51.66]), abnormal iridocorneal synechia (P < 0.001, HR = 6.534, 95% CI [1.10, 38.72]), larger angle closure range [P = 0.043, for eyes with angle closure range ≥ 2 quadrants (P = 0.012, HR = 4.226, 95% CI [0.70, 25.74])] and preoperative glaucoma history (P < 0.001, HR = 11.51, 95% CI [2.01, 65.95]) contributed to PKG (Fig. 3).
Structural Risk Factors for Post-keratoplasty Glaucoma in Eyes with Clinical Risk Factors
Compared with eyes without preoperative glaucoma, 55.6% of eyes with preoperative glaucoma had lens anomalies (P = 0.015, OR = 4.55, 95% CI [1.46, 14.08]) or abnormal iridocorneal synechia (P = 0.005, OR = 5.85, 95% CI [1.94, 17.54]). However, other structural features showed no significant differences (P > 0.050). All eyes with lens anomalies (P = 0.167, OR = 2.00, 95% CI [0.75, 5.32]) and all eyes with angle closures larger than two quadrants among the preoperative glaucomatous eyes developed PKG (P = 0.105, U = 2.00, 95% CI [−1.00, 2.00]), although the difference was not statistically significant (Table 3). Similarly, both the eyes with a lens anomaly among those with preoperative ocular hypertension developed PKG (P = 0.058, OR = 5.68, 95% CI [2.03, 15.87]) (Table 4).
Eight eyes with Peters anomaly developed PKG, and abnormal iridocorneal synechia was found to be a risk factor (P = 0.037, OR = 3.86, 95% CI [1.27, 11.63]) (Table 5). A shallow anterior chamber (P = 0.019, T = −2.687, 95% CI [−1.85, −0.20]), larger range of angle closure (P = 0.025, U = 36.00, 95% CI [−2.00, 0.00]), and lens anomaly (P = 0.006, all eyes with lens anomaly developed PKG) were risk factors for PKG development in sclerocorneal eyes (Table 6). All eyes with lens shape anomalies developed PKG (P = 0.050 for Peters anomaly and P = 0.022 for sclerocornea).
Discussion
Potentially causing irreversible graft failure and loss of vision, PKG is a major complication of PKP in the eyes of children with CCO. Compared with adult PKP, pediatric PKP has an additional risk of poor graft survival due to the structure of the anterior segment in eyes with CCO. Therefore, these patients should undergo more detailed preoperative evaluation and prognostic risk identification. Currently, risk factors for PKG in adult eyes have been identified. However, both structural and clinical risk factors for PKG in eyes with CCO remain to be identified, which makes prognosis evaluation, operation design, and postoperative management difficult. In this study, the preoperative anterior segment structural features evaluated using UBM were reviewed and analyzed along with the incidence of PKG.
Abnormal iridocorneal synechia is a leading risk factor for PKG. Intraoperative exploration of these eyes revealed a large area of anterior synechia and a thin iris (Fig. 2). Pre-existing extensive angle closure with anterior synechia may be further compromised by additional intraocular manipulation that can cause postoperative inflammation. Elevated cytokine levels are associated with iris damage, which may be excessive in eyes with abnormal iridocorneal synechia [31]. Specifically, increased cytokines in the aqueous humor are linked to the formation of PAS and glaucoma following surgery [32]. Therefore, abnormal iridocorneal synechia may eventually lead to PKG by inducing PAS.
However, the extent of involvement was not significantly associated with PKG in eyes with normal iridocorneal synechia in our study. Therefore, congenital dysplasia may play an important role in the development of PKG in eyes with abnormal iridocorneal synechia. At the seventh week of gestation, neural crest cells from the third wave of migration form a layer between the cornea and the anterior surface of the iris, a part of which becomes the iris stroma [33, 34]. The neural crest cells located in the tissues anterior to the chamber angle differentiate into endothelial cells in the trabecular meshwork as well as in Schlemm’s canal afterward [34]. Therefore, a thin iris might indicate aberrant migration or abnormal differentiation of neural crest cells [34, 35]. In addition, extensive synechiae suggest abnormal iris separation at the seventh month of gestation [36]. Dysgenesis of these anterior segments indicates dysplasia of the drainage pathway of the aqueous humor. Thus, the development of postoperative PAS and dysgenesis of the aqueous drainage pathway may jointly contribute to the progression of PKG in eyes with abnormal iridocorneal synechia.
In addition to abnormal iridocorneal synechia, a larger range of angle closure was also identified as a major risk factor. Previous studies have confirmed that eyes with preoperative PAS are significantly associated with PKG [19]. However, by further assessing the anterior chamber angle in detail, the range of angle closure was found to be an important risk factor compared to the extent of PAS in this study. One possible reason is that, unlike in previous studies, UBM was used to assess the extent of PAS instead of gonioscopy or intraoperative exploration [21, 22]. Recently, UBM has been widely used for anterior segment imaging in glaucomatous eyes [37]. The UBM examination images that were reviewed showed that in some eyes with PAS, gaps remained in the anterior angle. These potential gaps may provide access for aqueous humor drainage. Although angle closures and iridocorneal adhesions are separated during surgery, patients might also develop postoperative glaucoma. Considering the particularity of the congenital diseases in the included population, a possible explanation is that congenital trabecular meshwork dysplasia leads to PKG. Aqueous humor circulation could be imbalanced as a result of anatomical changes involving the trabecular meshwork, anterior chamber angle, iris, and ciliary body, leading to a greater than 50% incidence of secondary glaucoma in patients with anterior segment dysgenesis [38, 39]. During embryonic development, an intercellular gap was observed between the endothelial cells differentiated from the neural crest cells, which extended from the developing intertrabecular space. A gap was commonly found by the 18–22th weeks. At the 7th months of gestation, the trabecular meshwork separates from the anterior chamber with angle recession [36]. Therefore, the underlying etiology might be abnormal formation of the intercellular gap, resulting in blockage of the trabecular meshwork and the appearance of PKG.
Lens anomaly is another major risk factor, and shape anomaly may have a greater effect. Lenses without a normal shape were found to be thin sheet-like structures, some of which were attached to the posterior surface of the cornea during surgery. Similarly, developmental abnormalities may be an important reason. Aqueous drainage begins at the 17th–18th week of gestation, and lens vesicles are formed during the fifth week [33, 36]. Therefore, aberrant embryonic development of an eye with a lens anomaly might begin earlier, leading to higher risk of PKG. The results of previous studies on PKG in aphakic eyes are controversial [22]. Our findings suggested that aphakia was an important risk factor for PKG in patients with congenital diseases due to the developmental abnormalities it may represent.
Preoperative glaucoma and higher IOP were identified as clinical risk factors in this study. And eyes with these clinical risk factors exhibit a higher prevalence of anterior segment structural abnormalities including abnormal iridocorneal synechia, lens anomaly, and larger range of both ACR and ASR. The structural findings indicated that the preoperative glaucoma and ocular hypertension may be caused by the structural anomalies.
Interestingly, eyes diagnosed with preoperative glaucoma developed PKG in a relatively early time after PKP. In a previous study, preoperative glaucoma was considered to be associated with early postoperative elevation of IOP after PKP [40]. Goldberg et al. suggested that this is related to more manipulation in the anterior chamber in these eyes. Our research found that patients with preoperative glaucoma have more severe anterior segment structural abnormalities, which of course introduces more manipulation in the anterior chamber. In particular, for patients with CCO, the dysgenesis of the aqueous drainage pathways in patients with preoperative glaucoma may make them more susceptible to the effects of surgical manipulation inducing inflammation and PAS. However, patients 7 and 9 were the exceptions. Patient 7 was not diagnosed with preoperative glaucoma but developed elevated IOP early after surgery, while patient 9 developed PKG at 14 months postoperatively despite being diagnosed with preoperative glaucoma. For these exceptions, our hypotheses were as follows. Patient 7’s preoperative corneal diameter and axial length examination results did not suggest abnormal ocular dimensions. However, preoperative UBM indicated that the patient had lens abnormalities, abnormal iridocorneal adhesions, and a large range of ACR and ASR. In addition, the patient had high IOP preoperatively. Therefore, it may be that due to the young age at the time of surgery (9 months), the patient's eye dimensions had not yet been affected by the IOP, and thus preoperative glaucoma was not diagnosed. However, the patient had all the structural risk factors, and hence early PKG occurred. Patient 9 had preoperative glaucoma, abnormal iridocorneal adhesions, and a large range of ACR and ASR. However, the preoperative anterior segment structural examination and intraoperative exploration found that the abnormal iridocorneal adhesions were limited to the mid-peripheral area (see Figure S1 in the electronic supplementary material for details). Therefore, the peripheral adhesions may be caused by the traction of the mid-peripheral adhesions, and the angle structure may retain normal drainage function. After the release of the mid-peripheral adhesions, this child’s angle closure may have been greatly resolved. These exceptions highlighted the importance of utilizing UBM to determine anterior segment structural abnormalities before PKP surgery in infants and young children.
Structural risk factors for eyes with clinical risk factors were also identified. Anomalies of the lens and iris in eyes with preoperative glaucoma and Peters anomaly indicate the important effect of congenital dysplasia on poor prognosis. Eyes with preoperative glaucoma and larger ACRs or lens anomalies tend to develop PKG, which may imply a smaller range for normal aqueous humor drainage. Moreover, a shallow anterior chamber is a unique risk factor for sclerocornea. On the one hand, the shallowness may be associated with lens anomalies. On the other hand, concerning the flat corneal morphology of sclerocornea, a crowded anterior chamber may induce severe surgical injuries and flatter corneal grafting, which can lead to a higher risk of postoperative PAS formation. To avoid this situation, the introduction of a donor graft oversized by 1 mm may be helpful [41].
PKP in pediatric patients, especially patients with congenital cases, is challenging, and the prognosis may be poor. Therefore, detailed preoperative evaluations of both the structural and clinical features of eyes with CCO should be conducted. UBM shows great potential for the examination of the anterior segment in severely opaqued corneas and should be widely used in preoperative evaluations of eyes with CCO. Our study successfully identified several structural risk factors for PKG in eyes with CCO as well high-risk factors in eyes with clinical risk factors. An explanation of the risk factors should be included when patients are counseled about the risk of poor prognosis if they choose the proposed surgical procedure. High-risk patients should undergo frequent postoperative follow-up examinations and careful management of IOP. PKP should be performed with caution in these patients, and the timing of antiglaucoma surgery should be evaluated.
However, potential limitations should be noted. First, this study is limited by the small sample size, which is common in studies involving pediatric keratoplasties [5]. Therefore, the statistical power may be lower, and some variables may not be statistically significant. Second, only eyes with Peters anomaly and sclerocornea were included, which is related to the disease spectrum of our hospital. The addition of other cases of CCO may improve the reliability of the conclusions. However, due to the rareness of the disease, statistical analysis may be difficult. Moreover, this cohort should undergo long-term follow-up so the effects of structural risk factors on graft survival can be observed. Postoperative structural evaluations of these eyes should be conducted to explore the potential effects of dysplasia and the inflammatory response on the mechanisms of PKG.
There has been little focus on eyes with CCO in previous studies of PKG, and the risk factors for PKG in adult eyes are limited to PAS and lens anomalies, with no consideration of other structural details. Our study revealed the detailed structural risk factors for PKG in eyes with CCO using UBM, which has great implications for decision-making and postoperative management of complicated pediatric keratoplasties and provides a theoretical basis for the prevention and treatment of congenital blindness.
Conclusion
This is the largest clinical observational study of structural risk factors for PKG in pediatric patients to date. Our findings highlight the critical importance of a thorough preoperative assessment of the anterior segment structure, including iridocorneal synechia, lens status, and angle closure, in the PKG risk assessment, surgical prognosis, and postoperative management of pediatric patients with CCO. Particularly for patients presenting with clinical risk factors such as preoperative glaucoma and higher IOP, structural examinations are indispensable for clinical decision-making.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Bermejo E, Martínez-Frías ML. Congenital eye malformations: clinical-epidemiological analysis of 1,124,654 consecutive births in Spain. Am J Med Genet. 1998;75(5):497–504.
Kurilec JM, Zaidman GW. Incidence of Peters anomaly and congenital corneal opacities interfering with vision in the United States. Cornea. 2014;33(8):848–50.
Vanathi M, Panda A, Vengayil S, Chaudhuri Z, Dada T. Pediatric keratoplasty. Surv Ophthalmol. 2009;54(2):245–71.
Xavier Dos Santos Araújo ME, Santos NC, Souza LBD, Sato EH, de Freitas D. Primary pediatric keratoplasty: etiology, graft survival, and visual outcome. Am J Ophthalmol. 2020;212:162–8.
Karadag R, Chan TCY, Azari AA, Nagra PK, Hammersmith KM, Rapuano CJ. Survival of primary penetrating keratoplasty in children. Am J Ophthalmol. 2016;171:95–100.
Zhang Y, Liu Y, Liang Q, Miao S, Lin Q, Zhang J, et al. Indications and outcomes of penetrating keratoplasty in infants and children of Beijing, China. Cornea. 2018;37(10):1243–8.
Alexander JL, Wei L, Palmer J, Darras A, Levin MR, Berry JL, et al. A systematic review of ultrasound biomicroscopy use in pediatric ophthalmology. Eye (Lond). 2021;35(1):265–76.
Patil M, Soh YQ, Yu HCU, Nischal KK, Mehta JS. Recent advances in pediatric endothelial keratoplasty. Int Ophthalmol Clin. 2021;61(1):57–75.
Hwang DG, Hwang PH. Pediatric penetrating keratoplasty. Semin Ophthalmol. 1991;6(4):212–8.
Trief D, Marquezan MC, Rapuano CJ, Prescott CR. Pediatric corneal transplants. Curr Opin Ophthalmol. 2017;28(5):477–84.
Haddadin RI, Chodosh J. Corneal transplantation and glaucoma. Semin Ophthalmol. 2014;29(5–6):380–96.
Baltaziak M, Chew HF, Podbielski DW, Ahmed IIK. Glaucoma after corneal replacement. Surv Ophthalmol. 2018;63(2):135–48.
Anders L-M, Gatzioufas Z, Grieshaber MC. Challenges in the complex management of post-keratoplasty glaucoma. Ther Adv Ophthalmol. 2021;13:25158414211031396.
Anshu A, Li L, Htoon HM, de Benito-Llopis L, Shuang LS, Singh MJ, et al. Long-term review of penetrating keratoplasty: a 20-year review in Asian eyes. Am J Ophthalmol. 2021;224:254–66.
Chanbour W, Ayoub MH, Towair E, Darwish M, Fakhoury H, Warhekar P, et al. Incidence, risk factors and treatment outcomes of intraocular hypertension and/or glaucoma post-penetrating keratoplasty: a 5-year Lebanese retrospective descriptive study. Clin Ophthalmol. 2020;14:2497–505.
Al-Ghamdi A, Al-Rajhi A, Wagoner MD. Primary pediatric keratoplasty: indications, graft survival, and visual outcome. J AAPOS. 2007;11(1):41–7.
Huang C, O’Hara M, Mannis MJ. Primary pediatric keratoplasty: indications and outcomes. Cornea. 2009;28(9):1003–8.
Low JR, Anshu A, Tan ACS, Htoon HM, Tan DTH. The outcomes of primary pediatric keratoplasty in Singapore. Am J Ophthalmol. 2014;158(3):496–502.
Karadag O, Kugu S, Erdogan G, Kandemir B, Eraslan Ozdil S, Dogan OK. Incidence of and risk factors for increased intraocular pressure after penetrating keratoplasty. Cornea. 2010;29(3):278–82.
Hovlykke M, Hjortdal J, Ehlers N, Nielsen K. Clinical results of 40 years of paediatric keratoplasty in a single university eye clinic. Acta Ophthalmol. 2014;92(4):370–7.
González-Pérez LM, Ortiz-Arismendi GE, Moreno CJ. Prevalence and risk factors to develop ocular hypertension and glaucoma after penetrating keratoplasty. Archivos de la Sociedad Espanola de Oftalmologia. 2021;96(8):415–21.
Shree N, Gandhi M, Dave A, Mathur U. Incidence and risk factors for post-penetrating keratoplasty glaucoma. Indian J Ophthalmol. 2022;70(4):1239–45.
Wu S, Xu J. Incidence and risk factors for post-penetrating keratoplasty glaucoma: a systematic review and meta-analysis. PLoS ONE. 2017;12(4): e0176261.
Nischal KK, Naor J, Jay V, MacKeen LD, Rootman DS. Clinicopathological correlation of congenital corneal opacification using ultrasound biomicroscopy. J Br J Ophthalmol. 2002;86(1):62–9.
Janssens K, Mertens M, Lauwers N, de Keizer RJW, Mathysen DGP, De Groot V. To study and determine the role of anterior segment optical coherence tomography and ultrasound biomicroscopy in corneal and conjunctival tumors. J Ophthalmol. 2016;2016:1048760.
Yangzes S, Kaushik S, Malhotra C, Thakur A, Gupta A, Jain AK, et al. Correlation of anterior segment optical coherence tomography and ultrasound biomicroscopy in congenital corneal opacity. J AAPOS. 2024;28:103863.
Sharma N, Priyadarshini K, Agarwal R, Bafna RK, Nagpal R, Sinha R, et al. Role of microscope-intraoperative optical coherence tomography in pediatric keratoplasty: acomparative study. Am J Ophthalmol. 2021;221:190–8.
World Glaucoma Association Weinreb R, Grajewski, AL, Papadopoulos, M., Grigg, J., Freedman, SE, Eds. Childhood glaucoma: the 9th consensus report of the World Glaucoma Association. 2013.
Hong J, Xie Z, Wang X, Yu T, Ma S, Ben H, et al. Classifications of anterior segment structure of congenital corneal opacity in infants and toddlers by ultrasound biomicroscopy and slit-lamp microscopic photographs: an observational study. BMC Ophthalmol. 2024;24(1):34.
Hong J, Yang Y, Cursiefen C, Mashaghi A, Wu D, Liu Z, et al. Optimising keratoplasty for Peters’ anomaly in infants using spectral-domain optical coherence tomography. Br J Ophthalmol. 2017;101(6):820–7.
Aketa N, Yamaguchi T, Suzuki T, Higa K, Yagi-Yaguchi Y, Satake Y, et al. Iris damage is associated with elevated cytokine levels in aqueous humor. Investig Ophthalmol Vis Sci. 2017;58(6):BIO42-Bio51.
Kusano Y, Yamaguchi T, Nishisako S, Matsumura T, Fukui M, Higa K, et al. Elevated cytokine levels in aqueous humor are associated with peripheral anterior synechiae after penetrating keratoplasty. Int J Mol Sci. 2021;22(22):12268.
Barishak YR. Embryology of the eye and its adnexae. Dev Ophthalmol. 1992;24:1–142.
Williams AL, Bohnsack BL. Neural crest derivatives in ocular development: discerning the eye of the storm. Birth Defects Res C Embryo Today. 2015;105(2):87–95.
Idrees F, Vaideanu D, Fraser SG, Sowden JC, Khaw PT. A review of anterior segment dysgeneses. Surv Ophthalmol. 2006;51(3):213–31.
McMenamin PG. Human fetal iridocorneal angle: a light and scanning electron microscopic study. Br J Ophthalmol. 1989;73(11):871–9.
Gong H, Dong X, Zheng B, Gao X, Chen L, Zhang S, et al. Ultrasound biomicroscopy might predict the outcome of phacoemulsification-visco dissection in medically controlled primary angle-closure glaucoma eye with extensive peripheral anterior synechia. Front Med. 2021;8: 705864.
Ma AS, Grigg JR, Jamieson RV. Phenotype-genotype correlations and emerging pathways in ocular anterior segment dysgenesis. Hum Genet. 2019;138(8–9):899–915.
Gould DB, John SWM. Anterior segment dysgenesis and the developmental glaucomas are complex traits. Hum Mol Genet. 2002;11(10):1185–93.
Goldberg DB, Schanzlin DJ, Brown SI. Incidence of increased intraocular pressure after keratoplasty. Am J Ophthalmol. 1981;92(3):372–7.
Vajpayee RB, Dada T, Ray M, Tandon R, Sethi A, Turaka K. Oversized corneal grafts for corneal opacities with iridocorneal adhesions. Ophthalmology. 2001;108(11):2026–8.
Acknowledgements
We thank the participants of the study.
Medical Writing/Editorial Assistance
This manuscript was edited for proper English language, grammar, punctuation, spelling, and overall style by one or more of the highly qualified native English speaking editors at AJE (verification code: 23E7-662A-96E2-E9B9-5B5P). The assistance was funded by the National Natural Science Foundation of China (82371027).
Funding
This study was supported by grants from the National Natural Science Foundation of China (81970768). The journal’s Rapid Service Fee was funded by the National Natural Science Foundation of China (82371027).
Author information
Authors and Affiliations
Contributions
Zi-jun Xie is the first author. Jing Hong obtained funding. Zi-jun Xie and Jing Hong designed the study. Zi-jun Xie, Xin Wang and Ting Yu collected the data. Zi-jun Xie and Ting Yu were involved in data cleaning, follow-up, and data analysis. Zi-jun Xie drafted the manuscript. Zi-jun Xie, Jing-hao Qu, and Ling-ling Wu contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content and approved the final version of the manuscript. All authors have read and approved the final manuscript. Jing Hong is the study guarantor.
Corresponding author
Ethics declarations
Conflict of Interest
Zi-jun Xie, Xin Wang, Ting Yu, Jing-hao Qu, Ling-ling Wu and Jing Hong have nothing to disclose.
Ethic Approval
The study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee (IRB00006761-M2018244) and conducted in compliance with the principles of the Declaration of Helsinki. The patients’ guardians provided consent at the time of treatment for their data to be used for future research purposes. Consent for publication was not applicable as our manuscript does not include identifiable information.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xie, Zj., Wang, X., Yu, T. et al. Preoperative Structural Risk Factors for Glaucoma After Penetrating Keratoplasty for Congenital Corneal Opacity: An Observational Study. Ophthalmol Ther (2024). https://doi.org/10.1007/s40123-024-01027-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40123-024-01027-5