Abstract
Introduction
Cataract surgery poses a risk to corneal endothelial cells. This study aimed to assess the protective effect of rho-associated kinase inhibitor eye drop (ripasudil) on corneal endothelial cells after cataract surgery over 12 months.
Methods
We conducted a prospective, non-randomized, non-blinded comparative study including 43 patients divided into two groups: the ripasudil group (22 patients, 23 eyes) and the control group (21 patients, 21 eyes). All patients had grade 3 nuclear cataract and underwent uneventful phacoemulsification with intraocular lens implantation. In the ripasudil group, one drop of ripasudil hydrochloride hydrate (Glanatec® ophthalmic solution 0.4%) was administered three times a day for 5 days. Outcome measures included central corneal thickness (CCT) and endothelial cell density (ECD), which were evaluated preoperatively and 12 months postoperatively.
Results
In the ripasudil group, the median ECD was 2398 (interquartile range [IQR] 410, 2201–2611) cells/mm2 at baseline and 2262 (IQR 298, 2195–2493) cells/mm2 at 12 months postoperatively. In the control group, the median ECD was 2503 (IQR 390, 2340–2730) cells/mm2 at baseline and 2170 (IQR 324, 2049–2373) cells/mm2 at 12 months postoperatively. Endothelial cell loss (ECL) was 12.8% in the control group, significantly reduced to 4.5% in the ripasudil group (p = 0.001*). CCT (p = 0.042), age (p = 0.383), sex (p = 0.944), and duration of surgery (p = 0.319) were not significant factors. No adverse effects were observed in either of the groups.
Conclusions
Incorporating ripasudil into postoperative management could help maintain corneal endothelial cell integrity and reduce cell loss after cataract surgery, potentially decreasing the need for endothelial transplantation in patients who have undergone intraocular surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cataract surgery is the most frequently performed surgical procedure globally, but it can negatively impact the corneal endothelium, which is crucial for corneal health. |
Unlike other tissues, the corneal endothelium lacks significant regenerative ability, making cell loss permanent, emphasizing the need to minimize endothelial cell loss during cataract surgery. |
Ripasudil, a medication, shows promise in significantly reducing endothelial cell loss after cataract surgery, with a regimen of one drop administered three times a day for 5 consecutive days starting on the day of surgery. |
The study aims to assess the protective effect of ripasudil on corneal endothelial cells after cataract surgery, addressing the unmet need for interventions to mitigate endothelial cell loss in this population. |
Findings demonstrate a significant reduction in endothelial cell loss in the ripasudil group compared to controls, suggesting its potential benefit in preserving corneal endothelial health following cataract surgery. |
Protecting the corneal endothelium during cataract surgery and exploring interventions like ripasudil could ultimately improve long-term corneal health and potentially decrease the need for corneal transplants. |
Introduction
Cataract surgery is one of the most frequently performed surgical procedures worldwide, and it has proven to be cost-effective [1, 2]. This procedure is known to improve patients’ quality of life, and with ongoing technological advancements, it is increasingly becoming a procedure aimed at achieving emmetropia [3]. Although cataract surgery has been demonstrated to be effective and safe, complications can occasionally arise. These complications range from mild, such as dry eye or discomfort, to more severe ones, including endophthalmitis, retinal detachment, suprachoroidal hemorrhage, and corneal decompensation [4,5,6]. Bullous keratopathy, in particular, can occur in patients with underlying Fuchs endothelial corneal dystrophy or after complicated cataract surgery. The current first line of treatment of such a complication is endothelial keratoplasty [7]. However, new approaches in the management of endothelial corneal failure are emerging [8].
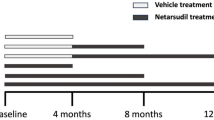
Rho kinase inhibitors (also known as ROCK inhibitors) have been utilized in the management of glaucoma and corneal endothelium diseases [9]. Studies have demonstrated that ROCK inhibitors enhance cell adhesion, growth, and antiapoptotic properties in both cultured monkey and human corneal endothelial cells [10]. Ripasudil and netarsudil are both ROCK inhibitors formulated as eye drops and approved for clinical use [11]. The safety of ripasudil has been well established, and it has been used in Japan for the treatment of glaucoma [11].
Research has shown that ripasudil may enhance wound healing of corneal endothelial cells in rabbits, suggesting its potential use in protecting corneal endothelium during intraocular surgery [12]. However, there remains a lack of consensus regarding the application of ripasudil in humans for protection after intraocular surgical procedures. A recent study indicated that ripasudil may help preserve the functional integrity of the corneal endothelium and minimize cell loss following cataract surgery in individuals with low corneal endothelial cell density (ECD) [13]. This finding suggests that the potential use of ripasudil could extend to safeguarding the corneal endothelium after intraocular procedures. The aim of this study is to evaluate the effectiveness of ripasudil in protecting corneal ECD following routine cataract surgery.
Methods
This prospective, non-randomized, non-blinded comparative study was conducted at King Saud University Medical City, Riyadh, Saudi Arabia. This study was conducted in accordance with the ethical standards outlined by the Helsinki Declaration and was approved by the Ethical Committee at King Saud University, Riyadh, Saudi Arabia. Informed consent was obtained from all patients who were enrolled in the ophthalmology outpatient clinic between October 2021 and March 2022. The study included 43 patients divided into two groups: the ripasudil group (22 patients, 23 eyes) and the control group (21 patients, 21 eyes). All patients had grade 3 nuclear cataracts, as identified using Pentacam Nucleus Staging Software and Pentacam’s Scheimpflug camera with a grading scale of 0–5, and no other anterior segment ocular disorders. Patients with healthy endothelium and an endothelial cell count of at least 1900 were included in the study. Those with complicated surgery, endothelial cell counts < 1900, or abnormal anterior segment structures were excluded. Outcome measures included central corneal thickness (CCT) and ECD, which were evaluated preoperatively and 12 months postoperatively.
The standard endocapsular stop-and-chop technique was performed by a single surgeon (M.K.) using the Centurion Vision System (Centurion) (Alcon Surgical, Fort Worth, TX, USA). In the ripasudil group, one drop of ripasudil hydrochloride hydrate (Glanatec® ophthalmic solution 0.4%) was administered three times a day on the day of surgery and continued to receive the same dosage for 5 days postoperatively. All participants were prescribed topical fluoroquinolone (ofloxacin 0.3%) four times a day for 1 week and 1% topical prednisolone acetate (initially administered four times a day and gradually tapered over a 4-week period).
Changes in ECD were evaluated using a non-contact specular microscope (SP 3000P, Topcon) before and 12 months after surgery. In our analysis of the ECD for both groups, we examined the central point as well as four paracentral points deviating from the center: superiorly, inferiorly, nasally, and temporally. The measured ECD values were then averaged. Changes in CCT were measured using the Pentacam Scheimpflug system. All measurements were performed by the same technician.
Statistical Analysis
Data were collected, stored, and managed on a spreadsheet using Microsoft Excel 2010® software. Subsequent analysis and figure preparation were carried out using SPSS® version 21.0 (IBM Inc. Chicago, IL, USA). Normality tests for continuous variables were conducted using the Shapiro–Wilk test and Q–Q plots. As the data were not normally distributed, they were reported as median (interquartile range) (IQR) and depicted using box-and-whisker plots. The Mann–Whitney U test was employed to assess differences between the two groups, while the Spearman correlation coefficient was calculated to determine the relationship between the duration of surgery and ECD loss. Categorical variables are presented as frequencies and percentages, and the chi-squared analysis was used to compare proportions between groups. Statistical significance was set at p < 0.05.
Results
This study included 44 eyes of 43 patients who underwent uncomplicated phacoemulsification and intraocular lens implantation. Among the participants, 23 eyes from 22 patients (14 males and nine females) were prescribed ripasudil. In the ripasudil group, the median age was 65 years (IQR 9, 60–69), while in the control group, the median age was 61 years (IQR 7, 60–67). The preoperative median best-corrected visual acuity (BCVA) was 0.70 (IQR 0.10; 0.60–1.30) LogMAR in the ripasudil group and 0.70 (IQR 0.10; 0.60–1.00) LogMAR in the control group. The postoperative median BCVA was 0.15 (IQR 0.30; 0.00–0.30) LogMAR in the ripasudil group and 0.15 (IQR 0.19; 0.05–0.24) LogMAR in the control group. In the ripasudil group, the median ECD was 2398 (IQR 410; 2201–2611) cells/mm2 at baseline and 2262 (IQR 298; 2195–2493) cells/mm2 at 12 months postoperatively. Conversely, in the control group, the median ECD was 2503 (IQR 390; 2340–2730) cells/mm2 at baseline and 2170 (IQR 324; 2049–2373) cells/mm2 at 12 months postoperatively (Table 1). Endothelial cell loss (ECL) was 12.8% in the control group, significantly reduced to 4.5% in the ripasudil group (p = 0.001*) (Fig. 1). In the ripasudil group, the median CCT values were 509 (IQR 35; 489–524) µm at baseline and 511 (IQR 56; 477–533) µm at 12 months postoperatively. In the control group, the median CCT was 509 (IQR 49; 490–539) µm at baseline and 528 (IQR 54; 494–548) µm at 12 months postoperatively (Fig. 2). The median duration of surgery was 21 min (IQR 7, 20–27) in the ripasudil group and 24 min (IQR 9, 20–29) in the control group (p = 0.319). Age (p = 0.383), sex (p = 0.944), and duration of surgery (p = 0.319) were not significant factors. Notably, throughout the study period, no Guttae were observed. No adverse effects were observed in either of the groups.
Discussion
Cataract surgery is both safe and effective; however, intraocular surgery can also result in the loss of corneal endothelial cells [14]. Techniques such as employing ophthalmic viscoelastic devices, utilizing certain surgical approaches, or leveraging femtosecond lasers have been developed with the goal of reducing ECL [15, 16]. Recently, new drugs such as ROCK inhibitors have entered the market. Rho kinase is a protein kinase that contributes to the regulation of cell size and shape via cytoskeleton structure [17]. Initially released as a glaucoma drug, ROCK inhibitors were later recognized for their potential to protect the corneal endothelium due to their ability to enhance cell adhesion, promote cell migration and growth, and exhibit antiapoptotic properties [8, 18]. It has been demonstrated that endothelial cells possess proliferative activity in vitro, suggesting that the corneal endothelium might proliferate under certain conditions [19]. The protective and pro-proliferative effects of ROCK inhibitors on the corneal endothelium could play a crucial role in regenerative medicine and may be utilized in the future management of corneal endothelial pathologies [8, 13]. In line with these observations, Schlötzer-Schrehardt et al. showed that a single dose of ripasudil significantly upregulated genes and proteins associated with cell cycle progression, cell–matrix adhesion, cell migration, as well as endothelial barrier and pump function, for up to 72 h [20]. Various authors have also demonstrated that ROCK inhibitors can enhance cellular proliferation in animals. Okumura et al. showed that the ROCK inhibitor Y-27632 increased cellular proliferation in vitro in primates [21]. Subsequently, Koizumi et al. and Okumura et al. demonstrated its application in in vivo corneal endothelial dysfunction models in rabbits and primates, and its usage has been demonstrated in humans with endothelial dysfunction due to various cause [12, 22]. Additionally, Kinoshita et al. revealed the benefits of ROCK inhibitors in cultured cells [23]. Other combinations, such as Descemet’s stripping only (DSO), also known as descemetorhexis without endothelial keratoplasty (DWEK), in conjunction with ROCK inhibitors, have also been demonstrated [24]. Alkharashi et al. reported on a series of three cases, aiming to evaluate the impact of perioperative ROCK inhibitors on corneal endothelial cells following phacoemulsification surgery. Employing a prospective design, three patients underwent administration of ROCK inhibitors both before and after surgery, with preoperative and 3-month postoperative assessments conducted using specular microscopy and Pentacam. The study findings revealed a significant decrease in ECD in eyes without ROCK inhibitors compared to those with, suggesting a potential protective effect of ROCK inhibitors on corneal endothelium [25]. Furthermore, Achiron et al. found compelling evidence suggesting that prophylactic exposure of corneal endothelial cells to a selective ROCK inhibitor could significantly reduce apoptosis rates following phacoemulsification. In their experimental ex vivo study, they observed a noteworthy decrease in both early and late apoptosis rates in corneal endothelial cells pre-treated with the ROCK inhibitor compared to controls. Specifically, a reduction of 37.06% in early apoptosis and 45.27% in late apoptosis rates was demonstrated. Additionally, the levels of ROCK in apoptotic corneal endothelial cells were markedly lower in the group treated with the ROCK inhibitor. These findings indicate a promising protective effect of the ROCK inhibitor against apoptosis induced by phacoemulsification energy [26].
It is worth mentioning that Tseng et al. conducted a retrospective series involving five patients who experienced persistent corneal edema after undergoing various anterior segment surgeries. The study found that using topical ripasudil proved to be an effective management option, resulting in improved vision and reducing the need for endothelial transplantation in four out of five cases [27].
In this study, we prospectively assessed the role of ripasudil in protecting corneal endothelial cells in healthy patients undergoing cataract surgery. We observed that the group treated with ripasudil exhibited lower ECL (4.5%) compared to the group receiving standard treatment (12.8%). It is crucial to emphasize that both groups exhibited similar baseline demographic characteristics regarding age and degree of cataracts. All surgeries were performed by the same surgeon using a consistent surgical technique. Although the BCVA results of both groups were comparable, it is well established that substantial ECL can trigger corneal endothelial decompensation and ultimately necessitate a corneal transplant. Thus, ripasudil use may be beneficial in reducing ECL, which could potentially result in a decreased need for corneal transplantation. It is conceivable that its use could be indicated in patients with borderline or low ECD. Fujimoto et al. demonstrated that ripasudil might help maintain corneal endothelial functional integrity and reduce ECL after cataract surgery in patients with low corneal ECD [13]. Fujimoto showed that the ECL in the control group was 14.1 ± 10.3%, and this proportion was significantly reduced to – 4.5 ± 13.0% in the ripasudil group (p = 0.0003). In our study, we observed similar outcomes, as we found a reduction of 12.8% ECD in the control group and 4.5% in the ripasudil group. Fujimoto et al. investigated the application of ripasudil for diseased endothelial cells, specifically in patients with low corneal ECD. In contrast, our study focused on assessing the protective effect of ripasudil on normal endothelium in patients undergoing routine cataract surgery. This difference in patient populations underscores the varying clinical contexts in which ripasudil may be applied, from diseased to healthy endothelium. Moreover, while Fujimoto et al. explored the efficacy of ripasudil over a longer duration, we specifically targeted the immediate postoperative period characterized by inflammation and stressors following cataract surgery. By administering ripasudil during this critical phase, we aimed to evaluate its ability to mitigate endothelial cell loss during a period of heightened vulnerability. Although some adverse effects have been reported in the literature, no adverse effects were observed in our patients [28, 29].
Nonetheless, this study has several limitations. It should be noted that, although it was a prospective study, it lacked randomization and blinding. Additionally, the sample size was insufficient to draw robust conclusions, and further study is needed to identify the optimal dose and duration of ripasudil. However, our study supports the findings of a previous study by Fujimoto et al. [13], highlighting the promising future of this drug in patients undergoing intraocular surgery. Larger studies with more rigorous designs are required to confirm these findings.
Conclusions
Our study delved into the protective effects of ripasudil, a rho-associated kinase inhibitor, on corneal endothelial cells post-cataract surgery over a span of 12 months. Through a prospective, non-randomized, non-blinded comparative study involving 43 patients, we identified a notable reduction in ECL within the ripasudil group compared to the control group. These findings underscore the potential of ripasudil integration into postoperative care as an effective strategy for preserving corneal endothelial cell integrity following cataract surgery. While our study presents promising insights into the clinical applicability of ripasudil, it is imperative to acknowledge the inherent limitations of our study design, including the relatively small sample size and absence of randomization and blinding. Additionally, there is a critical need for future research to ascertain the optimal dosing, duration, and frequency of ripasudil administration, alongside an evaluation of its long-term safety and efficacy.
Data Availability
All data generated or analyzed during this study have been included in this published article for accessibility.
References
Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on global eye health: vision beyond 2020. Lancet Glob Heal. 2021;9(4):e489–551. https://doi.org/10.1016/S2214-109X(20)30488-5.
Ginel J, Burguera N, Rocha-de-Lossada C, Piñero D, Sáez-Martín A, Fernández J. Economic evaluation of cataract: a systematic mapping review. Ophthalmol Ther. 2023;12(2):789–807. https://doi.org/10.1007/S40123-023-00678-0/TABLES/9.
Akpolat C, Demir M, Cevher S, Ozturk SZ, Yesiltas S. The impact of phacoemulsification surgery on vision-related quality of life in senile cataract patients. Ther Adv Ophthalmol. 2022;14:251584142110632. https://doi.org/10.1177/25158414211063293.
Levin HJ, Mehta MS, Storey PP, et al. Endophthalmitis following cataract surgery: visual outcomes, microbial spectrum and complications. Curr Opin Ophthalmol. 2023;34(3):237–42. https://doi.org/10.1097/ICU.0000000000000951.
Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification—a review of the literature. Eye (Lond). 2020;34(4):616–31. https://doi.org/10.1038/S41433-019-0575-Z.
Márquez AF, Urbinati F, Rocha-de-Lossada C, et al. Management of suprachoroidal hemorrhage during phacoemulsification: a comprehensive review. Medicina (B Aires). 2023;59(3):583. https://doi.org/10.3390/MEDICINA59030583.
Borroni D, Rocha-De-Lossada C, Parekh M, et al. Tips, tricks, and guides in Descemet membrane endothelial keratoplasty learning curve. J Ophthalmol. 2021. https://doi.org/10.1155/2021/1819454.
Rocha-De-Lossada C, Rachwani-Anil R, Borroni D, et al. New horizons in the treatment of corneal endothelial dysfunction. J Ophthalmol. 2021;2021:6644114. https://doi.org/10.1155/2021/6644114.
Novack GD. RHO kinase inhibitors for the treatment of glaucoma. Drugs Future. 2013;38(2):107–13. https://doi.org/10.1358/DOF.2013.038.02.1924778.
Pipparelli A, Arsenijevic Y, Thuret G, Gain P, Nicolas M, Majo F. ROCK inhibitor enhances adhesion and wound healing of human corneal endothelial cells. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0062095.
Tanihara H, Kakuda T, Sano T, Kanno T, Gunji R. Safety and efficacy of ripasudil in Japanese patients with glaucoma or ocular hypertension: 12-month interim analysis of ROCK-J, a post-marketing surveillance study. BMC Ophthalmol. 2020. https://doi.org/10.1186/S12886-020-01490-1.
Okumura N, Koizumi N, Ueno M, et al. ROCK inhibitor converts corneal endothelial cells into a phenotype capable of regenerating in vivo endothelial tissue. Am J Pathol. 2012;181(1):268–77. https://doi.org/10.1016/J.AJPATH.2012.03.033.
Fujimoto H, Setoguchi Y, Kiryu J. The ROCK inhibitor ripasudil shows an endothelial protective effect in patients with low corneal endothelial cell density after cataract surgery. Transl Vis Sci Technol. 2021. https://doi.org/10.1167/TVST.10.4.18.
Ho JW, Afshari NA. Advances in cataract surgery: preserving the corneal endothelium. Curr Opin Ophthalmol. 2015;26(1):22–7. https://doi.org/10.1097/ICU.0000000000000121.
Van Den Bruel A, Gailly J, Devriese S, Welton NJ, Shortt AJ, Vrijens F. The protective effect of ophthalmic viscoelastic devices on endothelial cell loss during cataract surgery: a meta-analysis using mixed treatment comparisons. Br J Ophthalmol. 2011;95(1):5–10. https://doi.org/10.1136/BJO.2009.158360.
Abell RG, Kerr NM, Howie AR, Kamal MAAM, Allen PL, Vote BJ. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg. 2014;40(11):1777–83. https://doi.org/10.1016/J.JCRS.2014.05.031.
Moshirfar M, Parker L, Birdsong OC, et al. Use of rho kinase inhibitors in ophthalmology: a review of the literature. Med Hypothesis, Discov Innov Ophthalmol. 2018;7(3):101.
Saha BC, Kumari R, Kushumesh R, Ambasta A, Sinha BP. Status of rho kinase inhibitors in glaucoma therapeutics—an overview. Int Ophthalmol. 2022;42(1):281–94. https://doi.org/10.1007/S10792-021-02002-W/METRICS.
Okumura N, Koizumi N, Ueno M, et al. Enhancement of corneal endothelium wound healing by Rho-associated kinase (ROCK) inhibitor eye drops. Br J Ophthalmol. 2011;95(7):1006–9. https://doi.org/10.1136/BJO.2010.194571.
Schlötzer-Schrehardt U, Zenkel M, Strunz M, et al. Potential functional restoration of corneal endothelial cells in Fuchs endothelial corneal dystrophy by ROCK inhibitor (ripasudil). Am J Ophthalmol. 2021;224:185–99. https://doi.org/10.1016/J.AJO.2020.12.006.
Okumura N, Ueno M, Koizumi N, et al. Enhancement on primate corneal endothelial cell survival in vitro by a ROCK inhibitor. Invest Ophthalmol Vis Sci. 2009;50(8):3680–7. https://doi.org/10.1167/IOVS.08-2634.
Syed ZA, Rapuano CJ. Rho kinase (ROCK) inhibitors in the management of corneal endothelial disease. Curr Opin Ophthalmol. 2021;32(3):268–74. https://doi.org/10.1097/ICU.0000000000000748.
Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N Engl J Med. 2018;378(11):995–1003. https://doi.org/10.1056/nejmoa1712770/suppl_file/nejmoa1712770_DISCLOSURES.PDF.
Moloney G, GarcerantCongote D, Hirnschall N, et al. Descemet stripping only supplemented with topical ripasudil for Fuchs endothelial dystrophy 12-month outcomes of the Sydney Eye Hospital Study. Cornea. 2021;40(3):320–6. https://doi.org/10.1097/ICO.0000000000002437.
Alkharashi M, AlAbbasi O. MMPU of R-KI has BE on CE after PMEAJO 2020 J 29;26(4):246–249. https://doi.org/10.4103/meajo.MP32153339.
Achiron A, Feldman A, Karmona L, Avizemer H, Barequet IS, Rosner M, Knyazer B, Bartov E. Burgansky Z V-DVP exposure of human corneal endothelial cells to R kinase inhibitor reduced apoptosis rate after phacoemulsification: E vivo study. JCRS. 2018. https://doi.org/10.1016/j.jcrs.2018.0.
Tseng MFRT. Topical ripasudil for the treatment of segmental corneal edema: a case series. Cornea. 2023. https://doi.org/10.1097/ICO.0000000000003282. (Epub ahead of print. PMID: 37098107).
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Araie M. Phase 2 randomized clinical study of a Rho kinase inhibitor, K-115, in primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol. 2013. https://doi.org/10.1016/J.AJO.2013.05.016.
Wisely CE, Liu KC, Gupta D, Carlson AN, Asrani SG, Kim T. Reticular bullous epithelial edema in corneas treated with netarsudil: a case series. Am J Ophthalmol. 2020;217:20–6. https://doi.org/10.1016/J.AJO.2020.04.002.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Conceptualization and design: Majed Alkharashi, Mohammed M Abusayf; manuscript drafting: Wael Otaif; review and editing: Majed Alkharasi, Mohammed M Abusayf, Wael Otaif, Abdullah Alkharashi.
Corresponding author
Ethics declarations
Conflict of Interest
Majed Alkharashi, Mohammed M Abusayf, Wael Otaif and Abdullah Alkharashi declare that they have no conflicts of interest to disclose.
Ethical Approval
This study was conducted in accordance with the ethical standards outlined by the Helsinki Declaration and was approved by the Ethical Committee at King Saud University, Riyadh, Saudi Arabia. Informed consent was obtained from all patients who were enrolled in the ophthalmology outpatient clinic between October 2021 and March 2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Alkharashi, M., Abusayf, M.M., Otaif, W. et al. The Protective Effect of Rho-Associated Kinase Inhibitor Eye Drops (Ripasudil) on Corneal Endothelial Cells After Cataract Surgery: A Prospective Comparative Study. Ophthalmol Ther 13, 1773–1781 (2024). https://doi.org/10.1007/s40123-024-00950-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00950-x