Abstract
Introduction
The aim of this work is to identify patients at risk of limited access to healthcare through artificial intelligence using a name-ethnicity classifier (NEC) analyzing the clinical stage of cataract at diagnosis and preoperative visual acuity.
Methods
This retrospective, cross-sectional study includes patients seen in the cataract clinic of a tertiary care hospital between September 2017 and February 2020 with subsequent cataract surgery in at least one eye. We analyzed 4971 patients and 8542 eyes undergoing surgery.
Results
The NEC identified 360 patients with names classified as ‘non-German’ compared to 4611 classified as ‘German’. Advanced cataract (7 vs. 5%; p = 0.025) was significantly associated with group ‘non-German’. Mean best-corrected visual acuity in group ‘non-German’ was 0.464 ± 0.406 (LogMAR), and in group ‘German’ was 0.420 ± 0.334 (p = 0.009). This difference remained significant after exclusion of patients with non-lenticular ocular comorbidities. Surgical time and intraoperative complications did not differ between the groups. Retrobulbar or general anesthesia was chosen significantly more frequently over topical anesthesia in group ‘non-German’ compared to group ‘German’ (24 vs. 18% respectively; p < 0.001).
Conclusions
This study shows that artificial intelligence is able to uncover health disparities between people with German compared to non-German names using NECs. Patients with non-German names, possibly facing various social barriers to healthcare access such as language barriers, have more advanced cataracts and worse visual acuity upon presentation. Artificial intelligence may prove useful for healthcare providers to discover and counteract such inequalities and establish tailored preventive measures to decrease morbidity in vulnerable population subgroups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
For patients with an increased risk of limited access and utilization of healthcare services in the event of a cataract, a delay in proper diagnosis and therapeutic management can have serious consequences. |
Can artificial intelligence bring ‘color consciousness’ to our otherwise ethnically blind medical society and introduce tailored preventative measures to ensure that every patient has equal access to medical treatment? |
What was learned from the study? |
Patients identified with a potential immigrant background have more advanced cataracts and worse visual acuity upon presentation. |
Artificial intelligence may prove useful for healthcare providers to counteract inequalities and establish tailored preventive measures to decrease morbidity in vulnerable population subgroups. |
Introduction
Based in the heart of central Europe, Austria has always been a multiethnic society, shaped by historic events from the Roman Empire, the following Migration Period, to the Austrian-Hungarian Monarchy, with over nine different ethnic groups. Nowadays, out of its population of 8.969 million people, 26.4% have a migration background, and about 11.4% use a conversational language other than German [1]. However, since German is the administrative language of the public health service, language barriers pose a significant obstacle to health care access and patient care. This potentially increases the risk for serious health disadvantages. The medical census of 2014 showed that people with a migration background tend to visit ophthalmologists less frequently compared to the general population [2]. These reports suggest a delayed diagnosis and management of health conditions, including cataract formation and visual impairment in this population group.
The ‘International Code of Medical Ethics’ states that ‘the physicians need to practice medicine fairly and justly, providing care based on the patient’s health needs without bias [3]. Therefore, it is our responsibility as medical professionals to investigate potential ethnic disadvantages in our healthcare system and address inequalities. With more than 94 million people affected worldwide, cataract prevalence increases up to 92.6% at an age of 80 years and older [4]. Health risks arising are extensive, including dementia [5], traffic accidents [6], and falls [7], ultimately resulting in higher mortality [8]. Diagnostic and therapeutic delays may bring about severe consequences, especially in conditions that can be treated in a safe and minimally invasive way if diagnosed timely [4].
Unlike other countries, ethnicity of patients is not routinely documented at first patient registration at the University Hospital of the Medical University of Innsbruck, Austria. However, recent innovations in artificial intelligence have introduced new data analyzing techniques. Name-ethnicity classifiers (NECs) are capable of inferring people’s ethnicities from their names with an accuracy of over 88%, allowing researchers to investigate potential ethnic disparities in datasets where this was previously impossible due to data limitations [9]. Additionally, we believe that Austria, with its multiethnic society, could serve as a role model for detecting and improving ethical inequalities in other countries.
Two goals were defined for the present retrospective study: Firstly, to evaluate whether the application of artificial intelligence via NECs is capable of identifying patients at risk of facing social barriers limiting their access to health care services; secondly, to determine if these patients exhibit more advanced cataracts with worse visual acuity upon presentation.
Methods
Inclusion and Exclusion Criteria and Data Collection
This retrospective cross-sectional study includes patients seen in our specialized cataract screening clinic between September 2017 and February 2020 who had cataract surgery in at least one eye. We included 4971 patients and 8542 eyes undergoing surgery. Only patients with complete reports were considered. A total of 163 patients who were under 50 years of age were excluded from the study to evaluate age-related cataract formation. Data were recorded, stored, and analyzed locally on university equipment in strict compliance with data protection regulations.
This was a retrospective, non-interventional study that had no impact on the management or treatment of patients and was conducted according to the guidelines of the Declaration of Helsinki of the World Medical Association (WMA). The research on accessibility of cataract surgery was approved by the local ethics committee of the Medical University of Innsbruck, Austria (study number 1013/2021) and due to the retrospective nature of the study and the strict implementation of data protection, no consent was required for this study. Advanced cataract was defined as documented ‘mature’, ‘premature’, ‘brunescent’, or ‘advanced’ cataract. Intrasurgical complications were defined as deviation from standard surgical protocol, including vitreous prolapse, anterior or posterior capsular tear.
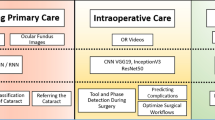
Name-Ethnicity Classifier—Model
To meet the needs of the present study, the original NEC machine learning model proposed by Hafner et al. [9] was customized. The original model analyzes the individual characters of names and classifies them into up to 49 nationalities and ethnic groups. It does so using a combination of a Convolutional Neural Network [10], a Long short-term memory (LSTM) Neural Network [11], and an optimization technique known as backpropagation [12]. To tailor the model to the Austrian health care context, it was then re-trained to classify names into one of two groups: ‘German’ (including Austrian names) and ‘non-German’ (representing other ethnicities).
Name-Ethnicity Classifier—Dataset
The dataset used for training the original model was sourced from the United Kingdom government’s CompaniesHouse business register [13], which consists of 7.3 million names from 49 different ethnicities. For the customized model, all German and Austrian names were extracted and combined into a group with 85,760 names, i.e., the ‘German’ class. Then a subset of the same size but containing only non-German names was extracted from the dataset, creating the ‘non-German’ class. The names in this subset were balanced across the 47 non-German ethnicities. This resulted in a final dataset of 171,520 names, with an equal distribution of 85,760 names for the ‘German’ and the ‘non-German’ class. Ensuring balance between the two classes is crucial to avoid biased results. Subsequently, each name consisting of a first name, optional middle names and a surname, was preprocessed. This involved removing name prefixes (e.g., ‘Mrs.’ and ‘Dr.’) and normalizing it to the Latin alphabet (e.g., replacing ô with o). Finally, the dataset was divided into three parts: 80% for training, 10% for validation during the training, and 10% for the final evaluation.
Name-Ethnicity Classifier—Training and Evaluation
The training was performed following the methodology described by Hafner et al. [9]. The remaining 10% of the dataset, i.e., 17,408 names, were then used to evaluate the model, resulting in an 88.09% accuracy score. To strengthen the validity of the results, the model was additionally tested on an independent dataset consisting of names of Olympic athletes [14], yielding a similar score of 88.07%. Furthermore, the evaluations showed a sensitivity (true-positive rate) of 78% for the class ‘non-German’ and 96% for the class ‘German’. This means that out of 100 non-German names, 78 were correctly classified as non-German, and out of 100 German names 96 were correctly classified as such. Given these results, the model was deemed to be sufficiently accurate to classify the patient data for this study.
Statistical Analysis
Statistical analysis was performed using Jamovi 2.3.21 (www.jamovi.org), Excel (Microsoft, Redmond, WA, USA) and graphs were drawn with the additional JJStatsPlot Module. Student’s t test or Welch’s t test (for unequal variances, if Levene’s test was significant p < 0.05) was used for parametric analysis with unequal variances. When assessing nominal data, the χ2 test of independence was utilized. For all statistical analysis, the level of significance was p < 0.05.
Results
Demographics
The study included 4971 patients and 8542 eyes. The name-ethnicity classifier divided all patients into two groups as discussed in the Methods section. The group whose names were classified as likely non-German consisted of 360 patients and 618 eyes undergoing cataract surgery amounting to 7.2% of the total study patient population. In contrast, the group classified as having ‘German’ names consisted of 4611 patients and 7924 eyes undergoing surgery (Fig. 1A). Group ‘non-German’ was significantly younger (p < 0.001) than group ‘German’ with a mean age of 71.4 ± 8.91 vs. 74.1 ± 8.71 and showed significantly less preoperative refractive error with a mean spherical equivalent of − 0.204 ± 3.73 versus − 0.624 ± 3.81 (p < 0.011; Fig. 1B).
A Table of demographic characteristics. Group ‘non-German’ identified 360 patients and 618 eyes undergoing cataract surgery, making up 7% of the total 4971 patients and 8542 eyes. With a mean age of 71.4 ± 8.91 for the group ‘non-German’ vs. 74.1 ± 8.71 for group ‘German’ a significant effect was found (p < 0.001) and illustrated in the box-violin plots of (B). Additionally, preoperative spherical equivalent was significantly (p = 0.011) less in group ‘non-German’ than group ‘German’
Comparing both groups regarding the documented need for a translator shows a strong and significant correlation (p < 0.001) between the use of a translator and being classified as belonging to the group ‘non-German’ by the NEC. While 5% of patients of group ‘non-German’ were accompanied on their clinic visit by a translator, this proportion was only 0.002% (respectively 0%) in the group ‘German’ (Fig. 2).
Ocular Comorbidities
Corneal opacities were documented in 4% of group ‘non-German’ and 2% of group ‘German’ (p = 0.001; Fig. 3A). Similarly, the prevalence of advanced cataract was a significantly different between the two groups (7 vs. 5%; p = 0.025; Fig. 3B). In contrast, analysis of both glaucoma (10 vs. 10%; p = 0.708; Fig. 3C) and advanced macular disease (8 vs. 8%; p = 0.818) revealed no significant difference (Fig. 3D).
A Bar chart showing the percentage of corneal opacities found in group ‘non-German’ with 4% and in group ‘German’ with 2% with a significant difference of p = 0.001. B Bar chart showing the percentage of advanced cataract found in group ‘non-German’ with 7% and in group ‘German’ with 7% with a significant difference of p = 0.025. C Bar chart showing the percentage of glaucoma found in group ‘non-German’ with 10% and in group ‘German’ with 10% with no significant difference of p = 0.708 and D bar chart showing the percentage of advanced macular disease found in group ‘non-German’ with 8% and in group ‘German’ with 8% with no significant difference of p = 0.818
Visual Acuity
Visual acuity (LogMAR) was compared between both groups, first for all patients (Fig. 4A) and secondly for patients without corneal opacities, glaucoma, or advanced macular disease (Fig. 4B). For all patients, group ‘non-German’ had a mean visual acuity 0.464 ± 0.406 and group ‘German’ 0.420 ± 0.334 with a significant difference of p = 0.009. After excluding 135 patients in group ‘non-German’ and 1464 in group ‘German’ due to reported central or paracentral corneal opacities, glaucoma or advanced macular disease (‘atrophic, fibrotic, microcystic edema, or subretinal fluid’) the observed difference remained significant with p = 0.008 with a mean visual acuity of 0.465 ± 0.411 for group ‘non-German’ and of 0.414 ± 0.326 for group ‘German’ (p = 0.008).
A Box-violin plot highlighting the significant difference of p = 0.009 between both groups with a mean visual acuity of 0.464 ± 0.406 LogMAR and of group ‘German’ 0.420 ± 0.334 LogMAR. B Box-violin plot showing the significant difference of p = 0.008 with a mean visual acuity of 0.465 ± 0.411 for group ‘non-German’ and of 0.414 ± 0.326 for group German ± 0.334 LogMAR after excluding all patients with significant corneal opacities, glaucoma, and advanced macular disease
Surgical Analysis
Comparison of surgical time between both groups (‘non-German’: 14.4 ± 9.07 min vs. ‘German’: 14.5 ± 9.11) revealed no significant difference with p = 0.733. Similarly, occurrence of intraoperative complications was equally distributed, occurring in 1% vs. 2% patients of either group as seen in Fig. 5B with p = 0.362. However, surgeons less frequently chose topical anesthesia in group ‘non-German’ compared to group ‘German’ (74 vs. 81%, respectively; p < 0.00; Fig. 5A).
A Box plot illustrating the percentage of topical anesthesia accounting 74% in group ‘non-German’ and 81% in group ‘German’, and other types of anesthesia (retrobulbar or general anesthesia) making up of 24% for group ‘non-German’ and 18% for group ‘German’ showing a significant difference of p < 0.001 of used anesthesia. B Showing no difference (p = 0.362) in the percentage of surgical complications with 1% in group ‘non-German’ and 2% in group ‘German’
Discussion
In this large retrospective study, patients with non-German names, as classified by an NEC, exhibited worse cataract outcomes using a variety of different indicators, including more advanced cataract formation and worse visual acuity at presentation. To our knowledge, this is the first study in ophthalmology using this methodology to identify and analyze a specific patient subpopulation. As a higher proportion of patients who were classified as non-German had requested a translator to help them navigate the Austrian healthcare system, language barriers present one possible cause for these disparities. As patients with non-German names that did not require a translator exhibited similar patterns, however, other causes such as lack of financial resources, lack of knowledge about the health care system, or social prejudices might likewise contribute to such inequalities [15, 16]. By ‘bringing color-consciousness’ into our otherwise ethnically blind medical society, these findings can serve as a basis to establish more-tailored preventive measures to ensure that every patient gets the same access to medical treatment.
The Austrian healthcare system offers universal and equal access for all population groups, including people with an immigrant background. Potential earlier diagnoses and treatments would therefore theoretically be available for all patients under the public healthcare system, with private health insurance only playing a subordinate role. Schober et al. [17] therefore came to the conclusion that differences in the utilization of the healthcare system are likely caused by social instead of institutional factors. Among such social factors, language barriers have been linked to several disadvantages in medicine. Not only restricted to Austria or Europe, this challenge involves every country [18, 19]. Similar to Austria, about 21% of the US American population speak a language other than English at home and 8.6% report that they speak English less than ‘very well’ [20]. This population with limited English proficiency (LEP) is affected by reduced utilization of health [21] and preventive services [22], such as the regular use of optometry services or eye clinic visits [23]. Similarly, Zheng et al. reported that in the English-dominated society of Singapore, Tamil-speaking Indians were more likely to have type 2 diabetes and diabetic retinopathy [24].
Similar to our study, Gill et al. found significantly more mature cataracts and worse preoperative visual acuity in patients with LEP. They defined patients as LEP, who self-identified as needing or preferring an interpreter in medical encounters [25]. However, as ethnicity and language proficiency are not documented routinely, the effect of these factors may remain undetected. In those cases, such as in our study, name-ethnicity classifiers are a promising tool for identification hidden disparities in health care.
Within the Austrian healthcare system, cataract surgery is only performed in hospital-based ophthalmic referral centers and not in ophthalmologist offices. Thus, our results apply to healthcare services offered in centers rather than outpatient facilities. The necessary two-step referral process is more challenging than one-step access to primary care facilities. This might present an additional challenge for patients facing language barriers, who have to communicate their needs to at least two medical professionals separately in order to obtain necessary treatment.
Furthermore, our results are obtained from an ophthalmic patient database with questionable applicability to other specialties or general medicine. However, medical referral processes are highly comparable between specialties within national healthcare systems. We therefore believe that further research might reveal similar health disparities also in other medical sectors.
One of the main limitations of this study is the assessment of visual acuity among patients facing various barriers in a routine clinical setting. It is possible, for example, that the language barrier itself affected the quality of visual acuity testing. However, to date, there are no clinical studies investigating this effect. Additionally, as a retrospective analysis, several key outcome parameters including cataract grading and documented presence of a translator were assessed from the medical charts and therefore highly dependent on the examiner’s documentation diligence. Thus, underreporting is a possible biasing factor.
It is difficult to establish causality between delayed cataract diagnosis and patient’s names being labeled as non-German using NEC. Patients with non-German names might face a variety of barriers in the Austrian medical system, ranging from prejudice treatment by medical professionals to language barriers. As significantly more patients in the non-German sample required a translator, and as there exists extensive literature supporting the claim that language barriers can lead to worse medical outcomes, we suggest that this factor likely also causes some of the disparities uncovered in the present study. However, further research is needed to investigate the exact extent to which this as well as other potential causal factors influence health disparities in Austria. Lastly, the NEC used in this study exhibits higher sensitivity than specificity when classifying names into ‘German’ or ‘non-German’. Therefore, a significant proportion of patients labeled as ‘non-German’ might not face any language or social barriers when accessing the Austrian healthcare system. Conversely, among those labeled ‘German’, there may also be some who are, for example, not proficient in the German language.
Conclusions
This study highlights that artificial intelligence is able to uncover delayed cataract diagnosis using name-ethnicity classification algorithms. These findings argue for the use of NECs in healthcare to raise awareness of inequalities and implement tailored counteractive measures to protect vulnerable population groups.
Data Availability
The datasets analyzed during the current study is available from the corresponding author on reasonable request.
References
Historische Volkszählungen. Stat. AUSTRIA. Available from: https://www.statistik.at/statistiken/bevoelkerung-und-soziales/bevoelkerung/bevoelkerungsstand/historische-volkszaehlungen
Österreichische Gesundheitsbefragung 2014. Stat. AUSTRIA. 2014. Available from: https://www.statistik.at/fileadmin/publications/OEsterreichische_Gesundheitsbefragung_2014.pdf
Parsa-Parsi RW. The International Code of Medical Ethics of the World Medical Association. JAMA. 2022;328:2018–21.
Liu Y-C, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. The Lancet. 2017;390:600–12.
Lee CS, Gibbons LE, Lee AY, Yanagihara RT, Blazes MS, Lee ML, et al. Association between cataract extraction and development of dementia. JAMA Intern Med. 2022;182:134–41.
Desapriya E. Association of cataract surgery with driving safety and falls. JAMA Ophthalmol. 2019;137:585.
Keay L, Ho KC, Rogers K, McCluskey P, White AJ, Morlet N, et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study. Med J Aust. 2022;217:94–9.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9:e489-551.
Hafner L, Peifer TP, Hafner FS. Equal accuracy for Andrew and Abubakar—detecting and mitigating bias in name-ethnicity classification algorithms. AI Soc. 2023. https://doi.org/10.1007/s00146-022-01619-4.
Lecun Y, Bottou L, Bengio Y, Haffner P. Gradient-based learning applied to document recognition. Proc IEEE. 1998;86:2278–324.
Gers FA, Schmidhuber J, Cummins F. Learning to forget: continual prediction with LSTM. Neural Comput. 2000;12:2451–71.
LeCun Y, Boser B, Denker JS, Henderson D, Howard RE, Hubbard W, et al. Backpropagation applied to handwritten zip code recognition. Neural Comput. 1989;1:541–51.
Companies House. GOV.UK. 2022. Available from: https://www.gov.uk/government/organisations/companies-house
Lee J, Kim H, Ko M, Choi D, Choi J, Kang J. Name Nationality Classification with Recurrent Neural Networks. Proc Twenty-Sixth Int Jt Conf Artif Intell. Melbourne, Australia: International Joint Conferences on Artificial Intelligence Organization; 2017. p. 2081–7. Available from: https://www.ijcai.org/proceedings/2017/289
Santalahti M, Sumit K, Perkiö M. Barriers to accessing health care services: a qualitative study of migrant construction workers in a southwestern Indian city. BMC Health Serv Res. 2020;20:1–7.
Czapka EA, Sagbakken M. “Where to find those doctors?” A qualitative study on barriers and facilitators in access to and utilization of health care services by Polish migrants in Norway. BMC Health Serv Res. 2016;16:460.
Schober T, Zocher K. Health-care utilization of refugees: evidence from Austria. Int Migr Rev. 2022;56:810–42.
Al Shamsi H, Almutairi AG, Al Mashrafi S, Al KT. Implications of language barriers for healthcare: a systematic review. Oman Med J. 2020;35: e122.
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A systematic review of the impact of patient-physician non-English language concordance on quality of care and outcomes. J Gen Intern Med. 2019;34:1591–606.
Bureau UC. Detailed Languages Spoken at Home and Ability to Speak English for the Population 5 Years and Over: 2009-2013. Census.gov. Available from: https://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html
Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80:11–9.
Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? J Gen Intern Med. 1997;12:472–7.
Wilson FA, Wang Y, Stimpson JP. Do immigrants underutilize optometry services? Optom Vis Sci Off Publ Am Acad Optom. 2015;92:1113–9.
Zheng Y, Lamoureux EL, Chiang P-CP, Anuar AR, Ding J, Wang JJ, et al. Language barrier and its relationship to diabetes and diabetic retinopathy. BMC Public Health. 2012;12:781.
Gill ZS, Caldwell AS, Patnaik JL, Marin AI, Mudie LI, Grove N, et al. Comparison of cataract surgery outcomes in English proficient and limited English proficiency patients. J Cataract Refract Surg. 2023;49(6):595–601.
Funding
The authors received no additional funding for this study. The journal’s Rapid Service Fee was funded by the Medical University of Innsbruck, Austria.
Author information
Authors and Affiliations
Contributions
Anna Lena Huber and Christoph Palme collected patient data. Franziska Sofia Hafner, Lena Hafner, and Theodor Peter Peifer developed, trained, and analyzed the names with the name-ethnicity classifier (NEC). Christoph Palme and Bernhard Steger analyzed the patient data. All authors were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors Christoph Palme, Franziska Sofia Hafner, Lena Hafner, Theodor Peter Peifer, Anna Lena Huber, and Bernhard Steger have no relevant financial or non-financial interests to disclose.
Ethical Approval
This was a retrospective, non-interventional study that had no impact on the management or treatment of patients and conducted according to the guidelines of the Declaration of Helsinki of the WMA. The research on accessibility of cataract surgery was approved by the local ethics committee of the Medical University of Innsbruck, Austria (study number 1013/2021) and due to the retrospective nature of the study and the strict implementation of data protection, no consent was required for this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Palme, C., Hafner, F.S., Hafner, L. et al. Artificial Intelligence (AI) Reveals Ethnic Disparities in Cataract Detection and Treatment. Ophthalmol Ther 13, 1683–1692 (2024). https://doi.org/10.1007/s40123-024-00945-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00945-8