Abstract
Introduction
The phase 3, randomized, vehicle-controlled, 14-day VIRGO study evaluated the efficacy and safety of twice-daily dosing of pilocarpine hydrochloride ophthalmic solution 1.25% (Pilo) in presbyopia. On VIRGO exit, a companion study was conducted to assess the patient experience with presbyopia and satisfaction with Pilo.
Methods
Recruited individuals completed the Presbyopia Patient Satisfaction Questionnaire (PPSQ) plus a three-part exit survey, or a live interview. The PPSQ evaluated respondents’ experience with Pilo. Survey parts 1 and 2 evaluated experience managing presbyopia before and during VIRGO, respectively; part 3 assessed future possibilities of using Pilo in real-world situations. The interview further informed the interviewees’ experience with presbyopia and Pilo. The primary endpoint was responders (%) in each rating category of the PPSQ items 1–7; the secondary endpoints were summary of categorical (survey) and qualitative (interviews) responses.
Results
The PPSQ and survey included 62 participants who received Pilo (N = 28) or vehicle (N = 34) in VIRGO; the interview included ten participants (Pilo, N = 4; vehicle, N = 6). Per the PPSQ, 64.3% of Pilo users reported vision improvement, including 17.9% with complete improvement; ≥ 46.4% were satisfied/very satisfied with their ability to perform daily activities, see up close unaided, and read in dim light. Among vehicle users, these percentages were 35.3%, 0%, and ≤ 23.5%, respectively. In both subgroups, ≥ 67.9% were interested in using Pilo or Pilo and eyeglasses/contact lenses in the future. Per the interview, vehicle users (n = 6/6) found the eyedrop easy to use but none experienced meaningful near-vision improvements, stopped using other correction method(s) part of the day, were satisfied with the eyedrop, preferred it over their previous correction method(s), or would continue using it if prescribed. Conversely, 75% (n = 3/4) of Pilo users responded positively to each of these six criteria.
Conclusions
Findings validate the VIRGO results and improve our understanding of the patient experience, demonstrating improved vision and satisfaction with Pilo (vs. vehicle) when performing daily activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pilocarpine hydrochloride ophthalmic solution 1.25% is to date the only pharmacologic therapy approved by the U.S. Food and Drug Administration to manage presbyopia. |
The current study aimed to assess the patient experience with presbyopia before enrollment in the randomized, vehicle-controlled, phase 3 VIRGO study of pilocarpine hydrochloride ophthalmic solution 1.25%, and to evaluate satisfaction with treatment during the VIRGO study. |
What was learned from the study? |
Most participants in the current study described their pre-VIRGO uncorrected near vision as moderately to severely impacted, and generally characterized their pre-VIRGO presbyopia as frustrating and bothersome. |
The Presbyopia Patient Satisfaction Questionnaire, exit survey, and live interview used in the current study consistently demonstrated a better patient experience with pilocarpine hydrochloride ophthalmic solution 1.25% than with the vehicle. |
The current study findings improve our understanding of the patient experience with pilocarpine hydrochloride ophthalmic solution 1.25%, demonstrating improved vision and satisfaction when performing daily activities (compared with the vehicle). |
Introduction
Presbyopia results from age-related changes of the crystalline lens and, as a consequence, an inevitable, progressive decline in near vision that usually begins to manifest itself at age 40 years [1,2,3]. Per findings from the Global Burden of Disease Study, between 1990 and 2020, the number of cases of visual impairment due to uncorrected presbyopia increased by 124.4% globally, corresponding to a 6.3% increase in age-standardized prevalence for the same period [4] and making presbyopia an important public health issue.
The treatment or correction of presbyopia poses challenges, as no surgical procedure can provide flawless vision at all distances without inherent risks [5], and the use of contact lenses (multifocal or monovision) or eyeglasses is associated with various compromises and/or negative impacts on daily life [5,6,7], despite recent advancements [8, 9]. The U.S. Food and Drug Administration’s approval of the first pharmacologic therapy for presbyopia, an ophthalmic solution of pilocarpine hydrochloride 1.25% in a proprietary vehicle (Pilo 1.25%; Vuity™; Allergan, an AbbVie company, Irvine, CA, USA) for once-daily (QD) or twice-daily (BID) administration [10], has introduced another approach for presbyopia management. Approval of QD administration of Pilo 1.25% was based on results of the randomized, double-masked, vehicle-controlled, phase 3 GEMINI 1 [11] and GEMINI 2 (ClinicalTrials.gov identifier: NCT03857542) studies of Pilo 1.25% dosed bilaterally, QD for 30 days, in individuals with presbyopia. Approval of BID administration was based on results of the randomized, double-masked, vehicle-controlled, phase 3 VIRGO study [12] of Pilo 1.25% administered bilaterally, BID for 14 days, and the underlying premise that some users may benefit from prolonging their near-vision improvements. All three studies met their primary endpoint, showing proportions of participants gaining ≥ 3 lines in mesopic, high-contrast, binocular distance-corrected near visual acuity (DCNVA) that were 3.8- and 4.5-fold greater (P < 0.01 for both) 3 h after administration of the single dose [11] (day 30) and second daily dose [12] (day 14) of Pilo 1.25%, respectively, compared with vehicle. Pilo 1.25% was well tolerated, with most treatment-emergent adverse events being mild in severity regardless of the dosing regimen [11, 12]. Moreover, minimal systemic accumulation was observed following use of Pilo 1.25% BID, as evidenced by accumulation indices of 1.11 (per the maximum observed plasma concentration) and 1.03 (per the area under the plasma concentration vs. time curve from time 0 to the end of the dosing interval) [12] that are close to 1.0 [13].
This present companion study was initiated to further comprehend the patient experience with presbyopia and to evaluate satisfaction with Pilo 1.25% compared with the vehicle in participants of the VIRGO study of BID dosing.
Methods
Study Design
Upon exiting (day 14) the phase 3 VIRGO study, participants were invited to enroll in this companion study, in which (1) the Presbyopia Patient Satisfaction Questionnaire (PPSQ, a validated patient-reported outcome instrument [14,15,16,17]) plus a 30-min, close-ended survey were self-administered via an online survey tool, or (2) a live interview was performed. Per protocol, the PPSQ/survey and interviews were to be completed within 14 days of the participants’ last VIRGO study visit (Fig. S1) [12].
The protocol was prospectively approved (on 17 December 2021) by the Western Copernicus Group Institutional Review Board (tracking number: 20216789) before any of the participants were contacted. The study was conducted in accordance with ethical principles of the Declaration of Helsinki and followed the guidelines of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use and applicable regulatory requirements. Individuals who agreed to participate provided written informed consent before initiating the companion study.
Participants
In the VIRGO study, adults aged 40–55 years with objective and subjective evidence of presbyopia impacting daily activities and mesopic, high-contrast, binocular DCNVA of 20/40 to 20/100 were randomized to bilateral administration of Pilo 1.25% BID or vehicle BID (6 h apart) for 14 days [12].
Eligible for participation in this study were individuals who completed the VIRGO study; signed the informed consent and Health Insurance Portability and Accountability Act forms; were able to speak, read, write, and comprehend English; had adequate communication skills to convey their experience with presbyopia and the VIRGO study (per the recruitment coordinator and/or recruiting clinician); and were willing/able to complete the PPSQ and survey or participate in a 60-min video interview within the aforementioned timeframe.
Excluded were participants who withdrew from the VIRGO study; were unable to understand the nature, scope, and possible consequences of the current study; or presented with evidence of uncooperativeness (per the recruitment coordinator/recruiting clinician’s judgment). Clinicians and/or their patient coordinators received training materials from Endpoint Outcomes, a Lumanity company (Boston, MA), the study administrator, on how to recruit/enroll participants.
Participants of this study were asked if they wanted to complete the PPSQ/exit survey or exit interview and received the recruitment flyer corresponding to their choice until ten interviews were completed. Subsequently, all participants were recruited to complete the PPSQ/exit survey. Upon completion of this study, respondents and interviewees were compensated for their time.
PPSQ and 3-Part Exit Survey
The PPSQ, also used as a secondary outcome measure in the GEMINI studies [16], consists of seven items/questions (listed in the Results section) assessing satisfaction with different aspects of presbyopia treatment with Pilo 1.25% vs. vehicle. Item 1 of the PPSQ was rated on a 0 (far worse) to 7 (complete improvement) scale; items 2–7 were rated on a 0 (very dissatisfied, far worse than expected, or extremely unlikely) to 4 (very satisfied, far better than expected, or extremely likely) scale. Higher scores indicated higher levels of satisfaction. Participants accessed the questionnaire via SurveyMonkey using a password-protected link sent to their email. Only one submission per respondent was allowed.
The three-part exit survey, comprising closed-ended questions (listed in the Results section), was available through the previously mentioned password-protected link. Only one submission per respondent was allowed.
Part 1 evaluated the respondents’ experience with presbyopia and its management before the VIRGO study, with questions regarding the onset of presbyopia, history of eyeglasses or contact lens use, and impact of near-vision blurriness, for example, as well as the types and level of satisfaction with the methods used to correct their near vision. Part 2 evaluated the respondents’ experience with and management of presbyopia during the VIRGO study. For example, part 2 inquired about the respondents’ ability to stop using/relying on their eyeglasses or contact lenses, their ability to see objects and text at near and intermediate distances, how the eyedrops did or did not benefit their daily life, and the level of satisfaction with Pilo 1.25% vs. other presbyopia correction methods. Part 3 inquired about future possibilities of using the investigational eyedrops vs. other vision correction methods in real-world situations (e.g., at work, in restaurants, and during weekends), and how frequently the respondent would consider using Pilo 1.25%.
Exit Interview
The exit interviews (audio-recorded with the participants’ consent) were conducted via Zoom video conferencing by experienced interviewers who were trained in the protection of human research participants, internal data protection, and the interviewing process, and masked to the treatment received during the VIRGO study. The interviewers used a guide that consisted of open-ended questions to encourage spontaneous responses and good qualitative data. The topics, questions, and probes were designed to provide information on the interviewees’ signs, symptoms, and impacts of presbyopia, as well as their experience with the VIRGO study.
Audio recordings of the exit interviews were processed as previously described [6]. Briefly, all audio recordings were transcribed verbatim and anonymized. Each transcript was considered to be a unit of analysis, and data from all transcripts were aggregated after coding (including demographics and health-related information), without imputation of missing data. The initial coding scheme was developed using terms from the exit interview guide and research objectives, but was updated as necessary to reflect the actual terminology used by interviewees and allow the incorporation of recoded/reclassified data, cataloging concepts that were reported spontaneously (without prompting from the interviewer) or probed (following explicit probing from the interviewer).
The coding process was guided by a hybrid approach that involved established qualitative research methods for open-ended questions, and a more targeted approach for probed questions. Details of this hybrid approach have been previously published [6]. Unique concepts were identified and merged into broader categories when appropriate, which helped identify and explain patterns and relationships within the data set [18, 19].
Because open-ended questions do not always yield the data needed to answer all research questions, more specific probes and codes were incorporated into the interview and coding process as well, to ensure that the objectives of the research were accomplished. Frequencies of unique concepts (based on the interviewees’ responses) were reported [6].
The coding scheme was applied and operationalized using ATLAS.ti software version 8.4 or higher (ATLAS.ti GmbH, Berlin, Germany), which is designed specifically for qualitative data analysis [6]. Intercoder reliability (extent to which independent coders are concordant in coding) was evaluated using percentage agreement (i.e., [total number of concordant codes]/[total number of codes used] × 100). Intercoder reliability was considered acceptable if ≥ 90%, based on benchmarks outlined in the literature (70–94%) [20].
Endpoints and Statistical Analysis
The primary endpoint was the proportion of respondents in each of the rating categories associated with questions 1–7 of the PPSQ. The secondary endpoints were the summary of categorical responses to the exit survey and summary of the qualitative, semi-structured exit interviews. All data were analyzed descriptively in terms of frequency, mean, standard deviation (SD), median, quartiles (Q), and range, among others, for the respondents/interviewees overall, as well as for subgroups of interest (Pilo 1.25% vs. vehicle) when applicable. No inferential statistics were calculated.
Before proceeding with data analysis, Endpoint Outcomes, a Lumanity company, confirmed that the PPSQ and exit survey were operating correctly on SurveyMonkey.
Sample Size
Based on the overall VIRGO study sample (estimated at N = 200 since this study protocol was developed before completion of the VIRGO study) and minimum sample sizes recommended by Endpoint Outcomes (based on their overall experience in conducting/analyzing questionnaires and surveys) for data collection, the proposed enrollment target was 25–50% (i.e., 50–100) of the VIRGO study participants for the PPSQ/exit survey and eight to ten participants for the exit interview [21, 22] (including ≥ 5 with a history of current or prior use of corrective lenses to treat presbyopia).
Results
Enrollment, Demographics, and Health-Related Information
Following an expansion of the study period from 14 to 175 days after the last VIRGO study visit (due to recruitment challenges), the clinicians had reached out to 110 individuals who had completed the VIRGO study. Of those, 20 were excluded because they declined to participate, were deemed ineligible by the clinicians, or could not be contacted. Ninety individuals were recruited, and although 18 were lost to follow-up, the enrollment targets were met: 62 participants completed the PPSQ and exit survey, and ten completed the exit interview (all of whom had a history of use of corrective eyeglasses or contact lenses for presbyopia).
The mean (SD) time to study completion from the last VIRGO study visit was 61.2 (49.0) days in the overall population (N = 72), 64.3 (51.4) days in the PPSQ/exit survey population (N = 62), and 42.1 (22.6) days in the exit interview population (N = 10). The median time (Q1, Q3) to study completion was 52.5 (18.0, 97.3) days in the overall population (N = 72), 55.0 (15.8, 102.3) days in the PPSQ/exit survey population (N = 62), and 36.0 (33.8, 52.3) days in the exit interview population (N = 10).
Mean age and race distribution were similar in the present study (Table 1) and the VIRGO study [12], while the proportion of females was numerically higher in the present study (66.7%), compared with the VIRGO study (57.4% [12]). Notably, demographics and health-related information were generally similar in the PPSQ/exit survey and exit interview populations (Table 1).
Overall, 39% of the study participants had experienced difficulty with their near vision for > 5 years; 79% had previously used or were currently using over-the-counter glasses; ≥ 65% had previously used or were currently using presbyopia coping behaviors (e.g., adjusting brightness and/or increasing font size on electronic devices, holding materials farther out to read, increasing room lighting, squinting, and relying on others to read materials); 49% had previously used or were currently using prescription reading glasses; 35% had used or were currently using bifocal/trifocal/multifocal prescription glasses; and 18% had used or were currently using monovision contact lenses (Table 1).
PPSQ and Exit Survey
PPSQ
As shown in Table 2, the proportion of respondents reporting far better vision or complete improvement (i.e., no difficulties seeing up close) was 21.4% with Pilo 1.25% and 2.9% with vehicle. The proportions of respondents who were satisfied or very satisfied with their ability to perform daily activities, see up close without assistance, and read in dim light were 50.0%, 53.6%, and 46.5% with Pilo 1.25% and 20.6%, 14.7%, and 23.5% with vehicle, respectively. The proportion of respondents for whom the eyedrop performed better or far better than expected was 39.3% (Pilo 1.25%) and 14.7% (vehicle). The proportions of respondents who were satisfied/very satisfied with the eyedrop’s ease of use and were likely/very likely to use the eyedrop over previous forms of near-vision correction were 53.6% and 57.2% with Pilo 1.25% vs. 35.3% and 38.2% with vehicle.
Exit Survey Part 1: Experience with Presbyopia Before VIRGO
Respondents were asked to classify their pre-VIRGO uncorrected near vision on an impact scale ranging from barely to severely. “Barely impacted” meant being able to read without squinting; “mildly impacted” meant being able to read when squinting; “moderately impacted” was described as letters being blurry but clearing up if the materials are held farther away or font size is increased on a phone or tablet; “severely impacted” was being unable to read even when holding the materials at arms’ length, increasing font size by > 2 on a phone/tablet, or zooming in on text. Of the 62 respondents, 51 (82.3%) classified their pre-VIRGO uncorrected near vision as moderately to severely impacted, and 11 (17.7%) classified it as mildly/barely impacted. Consistent with this finding, the overall mean (SD) level of frustration with presbyopia was 6.7 (2.8) on a 0 (no frustration) to 10 (highest level of frustration) scale.
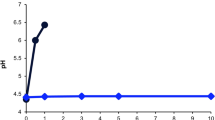
When respondents were asked to indicate all accommodations/procedures that they previously tried to correct their presbyopia (Fig. 1), “over-the-counter reading glasses” (72.6%) was most commonly selected, followed by “coping behaviors” (53.2%). The mean (SD) age at which over-the-counter reading glasses were first used was 45.4 (3.8) years, compared with 45.5 (4.0) years for coping behaviors. Of respondents who were using over-the-counter reading glasses before VIRGO, the most common prescription strength of the last pair purchased was + 1.5 D (24%), followed by + 2.0 D (16%) (Fig. 2).
Exit survey part 1: presbyopia correction methods/behaviors used by the exit survey participants (N = 62) before the VIRGO study. The question was: “Which of the following accommodations or procedures did you try for your presbyopia before the VIRGO study?” Participants could choose all applicable methods/behaviors. If they selected “Other,” they were asked to provide details
Exit survey part 1: strength of reading glasses last purchased. Data reflect the subgroup of exit survey participants who used over-the-counter reading glasses before enrolling in the VIRGO study (N = 45). The question was: “Which of the following is the correction strength or magnification of the last pair of reading glasses you purchased?”
Exit Survey Part 2: Experience with Presbyopia and Pilo 1.25% During VIRGO
Among respondents who received Pilo 1.25% BID (N = 28) during the VIRGO study, 54.2% (n = 13/24) indicated that they were able to stop using their eyeglasses at least part of day, compared with 11.1% (n = 3/27) of respondents who received the vehicle BID (Fig. 3). Among respondents who had used near-vision coping behaviors before the VIRGO study (n = 33; Fig. 1), 64.3% (n = 9/14) reported needing them less often while using Pilo 1.25% BID, compared with 21.1% (n = 4/19) in the vehicle BID subgroup (Fig. 4).
Exit survey part 2: ability to stop using eyeglasses during the VIRGO study. Data reflect the subgroup of exit survey participants who used eyeglasses before enrolling in the VIRGO study (N = 51). The question was: “During the clinical study, were you able to stop using store-bought or prescription glasses for at least part of the day?” aFour respondents did not use eyeglasses before the VIRGO study and were not included in this analysis. bSeven respondents did not use eyeglasses before the VIRGO study and were not included in this analysis. BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Exit survey part 2: change in use of coping behaviors during the VIRGO study. Data reflect the subgroup of exit survey participants who used coping behaviors before enrolling in the VIRGO study (N = 33). The question was: “How did your use of near-vision coping behaviors (such as squinting, holding items farther away, or increasing font size) change from before the VIRGO to during the VIRGO study?” BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
When prompted to rate their level of satisfaction with the VIRGO study eyedrops on a 0 (very dissatisfied) to 4 (very satisfied) scale, 57.1% (n = 16/28) of Pilo 1.25% BID users were satisfied or very satisfied, while 23.5% (n = 8/34) of vehicle BID users were satisfied or very satisfied (Fig. 5). Overall, satisfaction with the VIRGO study eyedrops over previously used presbyopia correction methods was also consistently higher among Pilo 1.25% users (49.1%; n = 28/57) than vehicle users (25.0%; n = 18/72; Fig. 6).
Exit survey part 2: satisfaction with Pilo 1.25% BID and vehicle BID during the VIRGO study. Data reflect the overall exit survey population (N = 62). The question was: “Overall, how satisfied were you with the eyedrops that you received as part of the clinical study?” Participants were to rate their satisfaction on a 0 (very dissatisfied) to 4 (very satisfied) scale. BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Exit survey part 2: satisfaction with Pilo 1.25% BID and vehicle BID vs. previous correction methods. Data reflect the overall exit survey population (N = 62). The question was: “Were you more satisfied with the clinical study eyedrop or your previous correction method(s)?” Participants were asked to rate their satisfaction on a 1 (much more satisfied with the clinical study eyedrops) to 5 (much more satisfied with my previous correction method) scale. BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Among respondents who received Pilo 1.25% BID in the VIRGO study, 46.4% (n = 13/28) were satisfied/very satisfied with their near vision. Importantly, 50.0% (n = 14/28) were also satisfied/very satisfied with their intermediate vision (Fig. 7). In comparison, in the vehicle subgroup, 23.5% (n = 8/34) were satisfied/very satisfied with their near vision and 20.6% (n = 7/34) were satisfied/very satisfied with their intermediate vision in (Fig. 7). In addition, 46.4% (n = 13/28) of respondents indicated that their near-vision changes lasted 3–6 h with Pilo 1.25% BID, compared with 23.5% (n = 8/34) with vehicle BID (Fig. 8).
Exit survey part 2: satisfaction with near and intermediate vision with Pilo 1.25% BID vs. vehicle BID. Data reflect the overall exit survey population (N = 62). The questions were: “During the VIRGO study, how satisfied were you with your ability to see near objects (such as text on a cell phone or labels on items) for the entire day?” “During the VIRGO study, how satisfied were you with your ability to see intermediate objects (such as a computer screen) for the entire day?” BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Exit survey part 2: duration of near-vision improvements with the eyedrop used during the VIRGO study. Data reflect the overall exit survey population (N = 62). The question was: “For approximately how long were you able to focus on objects or read up close after applying the eyedrops during the clinical study?” Participants were to choose between < 3, 3–4, 5–6, 7–8, 9–10, 11–12, or > 12 h. BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Exit Survey Part 3: Future Use of Pilo 1.25%
It is notable that 71.4% (n = 20/28) of respondents in the Pilo 1.25% subgroup indicated that they would use the eyedrop once (17.9%; n = 5/28) or twice (53.6%; n = 15/28) daily if prescribed by their doctor. Interestingly, despite large differences in satisfaction favoring Pilo 1.25% over vehicle, 82.3% of respondents in the vehicle subgroup would use the investigational eyedrop once (20.6%) or twice (61.8%) daily if prescribed by their doctor (Fig. 9).
Exit survey part 3: number of times respondents would use the investigational eyedrop if prescribed by their doctor. Data reflect the overall exit survey population (N = 62). The question was: “If your eye doctor said you could use the clinical study eyedrops once or twice per day, how many times would you apply the presbyopia eyedrops per day when they are available for purchase based on your clinical study experience?” BID twice daily, Pilo pilocarpine hydrochloride ophthalmic solution
Exit Interview
When asked about the impacts of presbyopia on their daily life, interviewees reported 30 negative impacts across four domains, including 20 impacts that were reported by > 1 participant (Electronic Supplementary Material [ESM] Table 1). Among those negative impacts, difficulty reading from a cell phone or computer, text up close, menus in dimly lit restaurants, or small text on labels, and presbyopia being aggravating/irritating/frustrating were the most frequently reported (≥ 90% each). In addition, 14 negative impacts of reading glasses were reported across three domains, and 16 negative impacts of prescription bifocal/trifocal/multifocal glasses were reported across seven domains (ESM Table 2). The most common were inconvenience (of reading glasses, 87.5%), as well as reliance on and glare (of prescription bifocal/trifocal/multifocal glasses, 100% each).
Based on the interviewees’ rating of the bothersomeness of their blurry near vision before the VIRGO study on a 0 (not bothersome) to 10 (extremely bothersome) scale, the mean (SD) bothersomeness score of the overall interview population was 8.3 (1.5). The most bothersome impact of presbyopia was being unable to read/see up close, cited by 62.5% (n = 5/8) of interviewees with available data, but difficulty reading menus in dimly lit restaurants, difficulty watching television/movies, and taking longer to complete tasks were also mentioned (each 12.5%, n = 1/8). Consistent with these findings, the inability to see up close was deemed the most important aspect of presbyopia to treat (88.9%, n = 8/9). The most bothersome impact of the interviewees’ previous presbyopia correction methods was having to rely on them (87.5%, n = 7/8), although inconvenience was also reported (12.5%, n = 1/8).
Among interviewees who received Pilo 1.25% BID during the VIRGO study, 75% (n = 3/4) experienced meaningful near-vision improvements; were able to stop using other correction methods for part of the day; deemed the eyedrop effective and easy to use overall; and were satisfied with the eyedrop overall and in terms of being able to perform daily activities, read/see objects up close without eyeglasses, squinting, or changing font size, read books/newspapers, and read on a cell phone/computer/tablet (Table 3). Additionally, 25% (n = 1/4) of Pilo 1.25% users reported improvements in their intermediate/distance vision. In contrast, none of the six interviewees who received the vehicle BID reported vision improvements (near or intermediate/distance); none were able to stop using their other correction method(s) for part of the day; all deemed the eyedrop ineffective despite being easy to use; and all were dissatisfied with the eyedrop (Table 3).
When asked whether they would continue using the eyedrop if given the option, 75% (n = 3/4) of interviewees who received Pilo 1.25% BID during the VIRGO study said they would, and 25% (n = 1/4) said “yes, if the eyedrop was effective.” Notably, the latter participant did not experience near-vision improvement in the VIRGO study. Otherwise, 75.0% (n = 3/4) preferred the eyedrop over their other near-vision correction method(s) in general, during the evening, and at work/throughout daily life (i.e., doing activities such as working, running errands, doing chores around the house, etc.). When asked if they liked or disliked taking a second dose later in the day, 50.0% (n = 2/4) liked it, one disliked it (stating “I had to set up an alarm… and it became annoying”), and one was neutral about it.
Discussion
Overall, our study results indicate that, before entering the VIRGO study, respondents and interviewees generally found presbyopia frustrating and bothersome, and disliked the inconvenience of eyeglasses and having to rely on them for near vision. These findings align with those of studies showing that individuals with presbyopia have a lower quality of life than younger, emmetropic individuals, even when presbyopia is corrected surgically (monovision) or with eyeglasses [23,24,25]. Together, these data also underscore the need for additional presbyopia treatment options [6].
All PPSQ-related findings highlighted a more positive experience with Pilo 1.25% than with vehicle. The proportions of respondents who reported at least moderately better near vision, who were satisfied or very satisfied with their ability to see up close without additional correction, and who indicated that the eyedrop was far better than expected were 3.6- to 8.6-fold greater with Pilo 1.25% than vehicle. Per the exit survey, the majority of respondents also reported more positive experiences with Pilo 1.25% than with vehicle during the VIRGO study and a preference for using this eyedrop in the future, either alone or in combination with other vision correction methods. Notably, the proportion of PPSQ/survey respondents with mild/moderate dry eye as a baseline co-condition was 4.9-fold higher among vehicle users than among Pilo 1.25% users. Since the vehicle could have provided some relief of dry eye symptoms and improved vision to some extent, the differences in outcomes between intervention groups may have been underestimated.
Per the exit interviews, 75% of Pilo 1.25% users found it effective (reporting meaningful near-vision improvements), were satisfied with it, preferred it over their other presbyopia correction methods, and were able to stop using their correction method at least part of the day.
The duration of near-vision improvements reported herein with Pilo 1.25% was ≥ 3 h in 57% (n = 16/28) of participants (including 3–6 h in 46% [n = 13/28] of participants), which is consistent with product information indicating that a second daily dose may be administered 3–6 h after the first dose [10]. It is also noteworthy that the proportion of participants satisfied with their intermediate vision was 2.4-fold greater with Pilo 1.25% than with vehicle.
Potential limitations of this study include the fact that participant completion of the PPSQ, survey, and interview spanned 175 days after the last VIRGO study visit, instead of the planned 14 days, which may have affected their recollection of efficacy and adverse events and could explain why (for example) the proportion of respondents who were able to stop using their eyeglasses appears lower in this study (54%) than in the VIRGO study (79% [12]). On the other hand, completion of the PPSQ, survey, and interview immediately after completion of the VIRGO study (when the experiences and perceptions were still fresh in the participants’ minds) could have introduced a bias favoring Pilo 1.25%. Both possibilities should be considered when interpreting the current findings, along with the fact that the primary endpoint provided a straightforward metric for satisfaction but did not account for the intensity/importance of satisfaction/dissatisfaction in different aspects between the interventions. Moreover, because Pilo 1.25% causes pupil constriction, the study participants could have deduced which intervention they received during the VIRGO study, which in turn could have impacted their responses regarding satisfaction and experience with Pilo 1.25% vs. vehicle. Consistent with this possibility, three of four interviewees who used Pilo 1.25% during VIRGO believed they had used Pilo 1.25%, and all interviewees who used the vehicle control believed they had used the vehicle. The small subset of exit interview participants who received Pilo 1.25% (n = 4) should be considered as well when interpreting the qualitative insights for depth and generalizability, along with the possibility that some nuances in the interviewees’ response (for example) may not have been captured in the analysis. However, the interview sample was considered to be sufficient for the objective of collecting participant descriptions of treatment experience and satisfaction, as it supplements data from the PPSQ and exit survey, and the interviews (conducted by trained/experienced interviewers who were masked to treatment) were audio-recorded and transcribed verbatim before analysis to minimize the risk of bias. It is also worth noting that participants were asked about the benefits of the eyedrop used for 14 days during the VIRGO study, but a previously published study indicates that the peak responder rate was not reached until day 14 [11]. In addition, distance vision was not specifically evaluated herein, although it was previously shown not to be negatively affected by Pilo 1.25% in randomized, placebo-controlled, phase 3 studies [11, 12]. Similarly, night vision was not evaluated herein, but Pilo 1.25% was recently shown to reduce driving performance at night (as expected) [26], consistent with the current product labeling advising the user to exercise caution when driving at night and performing other hazardous activities in poor illumination [10]. Finally, the exclusion of participants who withdrew from the VIRGO study could have introduced a selection bias, as those excluded individuals may have withdrawn due to negative experiences or poor responses to the treatment. However, the number of participants who withdrew from VIRGO was the same in both treatment groups (n = 3 each; 2.6%), perhaps arguing against this possibility.
Despite the aforementioned limitations, the lack of long-term (e.g., ≥ 1-year) studies of the efficacy and safety/tolerability of Pilo 1.25%, and the fact that (to our knowledge) no clinical studies comparing the effectiveness and safety of Pilo 1.25% with those of other correction methods have been conducted to date, the findings of the PPSQ, exit survey, and exit interviews showed consistently better outcomes with Pilo 1.25% than with vehicle. The study findings are in line with those of previously published interview- or discussion-based studies that explored the experience of living with and managing presbyopia and identified limitations and negative impacts of current treatments (mostly eyeglasses) [6, 27], supporting the use of Pilo 1.25% as a treatment option in the presbyopia landscape. As with any new medical therapy, proper follow-up is advised while Pilo 1.25% is used as presbyopia treatment. Due to rare cases of retinal detachment reported with miotics, including Pilo 1.25%, all patients (especially those with pre-existing retinal disease) should also undergo a retinal examination before initiating Pilo 1.25% treatment for presbyopia [10].
Conclusions
The impact of presbyopia varies based on an individual’s unique and dynamic vision needs throughout their day. This study met the objective and provided a better understanding of the patient experience with presbyopia and its management with Pilo 1.25% used BID. Overall, findings of the PPSQ, exit survey, and exit interviews were consistent in demonstrating improved near vision and satisfaction with Pilo 1.25% over vehicle when participants performed daily activities. Notably, improvements in intermediate vision were also reported. The current results validate those from the VIRGO study and additionally provide valuable insight on the participants’ expectations and satisfaction regarding treatment, as well as experiences before, during, and after receiving the study intervention. The mixed methods approach of this work (questionnaire, close-ended survey, and open-ended interviews) allowed for a wider range of feedback and greater recognition of the impact of Pilo 1.25% vs. vehicle across all items covered in the questionnaire, survey, and interviews. These study findings further support the use of Pilo 1.25% as a noninvasive treatment option for presbyopia in meeting the dynamic and situational vision needs of patients.
Data Availability
AbbVie is committed to responsible data sharing regarding the clinical trials/studies we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (e.g., protocols, clinical study reports, or analysis plans), as long as the trials/studies are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial/study data for unlicensed products and indications. These clinical trial/study data can be requested by any qualified researchers who engage in rigorous, independent, scientific research, and will be provided following review and approval of a research proposal, Statistical Analysis Plan (SAP), and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time after approval in the USA and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvieclinicaltrials.com/hcp/data-sharing/.
References
Waring GO IV, Chang DH, Rocha KM, Gouvea L, Penatti R. Correlation of intraoperative optical coherence tomography of crystalline lens diameter, thickness, and volume with biometry and age. Am J Ophthalmol. 2021;225:147–56.
Mercer RN, Milliken CM, Waring GO IV, Rocha K. Future trends in presbyopia correction. J Refract Surg. 2021;37:S28–34.
American Optometric Association. Optometric clinical practice guideline—care of the patient with presbyopia. St. Louis: American Optometric Association; 2011.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e130–43.
Grzybowski A, Ruamviboonsuk V. Pharmacological treatment in presbyopia. J Clin Med. 2022;11:1385.
Stokes J, Shirneshan E, Graham CA, Paulich M, Johnson N. Exploring the experience of living with and managing presbyopia. Optom Vis Sci. 2022;99:635–44.
Berdahl J, Bala C, Dhariwal M, Lemp-Hull J, Thakker D, Jawla S. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439–50.
Wolffsohn JS, Davies LN, Sheppard AL. New insights in presbyopia: impact of correction strategies. BMJ Open Ophthalmol. 2023;8(1):e001122
Katz JA, Karpecki PM, Dorca A, et al. Presbyopia—a review of current treatment options and emerging therapies. Clin Ophthalmol. 2021;15:2167–78.
Allergan, an AbbVie company. Highlights of prescribing information—VUITYTM (pilocarpine hydrochloride ophthalmic solution) 1.25%, for topical ophthalmic use. 2023. https://www.rxabbvie.com/pdf/vuity_pi.pdf. Accessed 25 Jan 2024.
Waring GO IV, Price FW Jr, Wirta D, et al. Safety and efficacy of AGN-190584 in individuals with presbyopia: the GEMINI 1 phase 3 randomized clinical trial. JAMA Ophthalmol. 2022;140:363–71.
Kannarr S, El-Harazi SM, Moshirfar M, et al. Safety and efficacy of twice-daily pilocarpine HCl In presbyopia: the VIRGO phase 3, randomized, double-masked, controlled study. Am J Ophthalmol. 2023;253:189–200.
Wadhwa RR, Cascella M. Steady state concentration. [Updated 6 Mar 2023]. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK553132/.
Barnett M, McGee S, Pack W, Yuan J, Shirneshan E, Campbell J. No impact of headache or visual impairment adverse events following AGN-190584 observed on patient-reported outcomes. Denver: Association for Research in Vision and Ophthalmology (ARVO) 2022 Annual Meeting, 1–4 May 2022.
Evans DG, Coon C, Nichols KK, Shirneshan E, Campbell J. Interpreting clinically meaningful near vision improvement in presbyopia with AGN-190584 in the GEMINI 1 phase 3 trial. Boston: American Academy of Optometry (AAOpt) Academy 2021 Annual Meeting, 3–6 November 2021.
Wirta D, Christie W, Tauber J, Shirneshan E, Lee S, Campbell J. Assessing presbyopia impacts and coping behaviors with de novo PRO instruments in a phase 3 study of AGN-190584 (Pilocarpine 1.25%). Las Vegas: 2021 American Society of Cataract and Refractive Surgery Annual Meeting, 23–27 July 2021.
McCabe CM, Wirta D, Price FWJ, Lee S, Shirneshan E, Campbell JT. Patient-reported outcomes in pooled phase 3 studies of AGN-190584 (Pilocarpine 1.25%) for presbyopia. New Orleans: American Academy of Ophthalmology 2021 Annual Meeting, 12–13 November 2021.
Charmaz K. Grounded theory. In: Smith J, Harré R, Van Langenhove L, editors. Rethinking methods in psychology. London: Sage Publications; 1995. p. 27–49.
Lasch KE, Marquis P, Vigneux M, et al. PRO development: rigorous qualitative research as the crucial foundation. Qual Life Res. 2010;19:1087–96.
Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociol Methods Res. 2013;42:294–320.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2017;27:591–608.
Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Goertz AD, Stewart WC, Burns WR, Stewart JA, Nelson LA. Review of the impact of presbyopia on quality of life in the developing and developed world. Acta Ophthalmol. 2014;92:497–500.
Luo BP, Brown GC, Luo SC, Brown MM. The quality of life associated with presbyopia. Am J Ophthalmol. 2008;145:618–22.
McDonnell PJ, Lee P, Spritzer K, Lindblad AS, Hays RD. Associations of presbyopia with vision-targeted health-related quality of life. Arch Ophthalmol. 2003;121:1577–81.
Waring GO 4th, Brujic M, McGee S, et al. Impact of presbyopia treatment pilocarpine hydrochloride 1.25% on night-driving performance. Clin Exp Optom. 2023;1–8. https://doi.org/10.1080/08164622.2023.2279189.
Brujic M, Kruger P, Todd J, et al. Living with presbyopia: experiences from a virtual roundtable dialogue among impacted individuals and healthcare professionals. BMC Ophthalmol. 2022;22:204.
Acknowledgements
AbbVie and the authors thank all the trial investigators and the patients who participated in this study.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Michele Jacob, PhD, of Evidence Scientific Solutions (Philadelphia, PA, USA), and funded by AbbVie.
Funding
AbbVie funded this study and participated in the study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the publication. AbbVie also funded the journal’s Rapid Service fee. All authors had access to relevant data and participated in the drafting, review, and approval of this publication.
Author information
Authors and Affiliations
Contributions
Concept and design: Julie Whyte. Acquisition, analysis, or interpretation of data: Julie Whyte. Drafting of the manuscript: all authors. Critical revision of the manuscript for important intellectual content: all authors. Responsibility for the integrity of the data and the accuracy of the data analysis: all authors. Final approval of the publication: all authors.
Corresponding author
Ethics declarations
Conflict of Interest
Brian M Shafer has received consulting fees, honoraria, speaker fees, and/or travel reimbursement from Alcon, Allergan (an AbbVie company), CorneaGen, Harrow Pharmaceuticals, Tarsus, and Visus Therapeutics. Selina R McGee has received consulting fees, honoraria, speaker fees, and/or travel reimbursement from Allergan (an AbbVie company), Bausch + Lomb, Bruder, Cynosure, Dompe, EyeVance, Horizon, Kala Pharmaceuticals, Lumenis, Novartis, Ocuphire, Optovue, Osmotica, Oyster Point, Sun Pharmaceutical, Tarsus, Thea, and Versant. Cristos Ifantides has received consulting fees, honoraria, speaker fees, and/or travel reimbursement from Ace Vision Group, Acufocus Inc, Alcon, Allergan (an AbbVie company), Bausch + Lomb, BVI, Centricity Vision, Hu-Med Technologies, Johnson & Johnson, New World Medical, Spect Inc, Tarsus, Trefoil, Vision 2020 USA, Visus Therapeutics, and Zeiss. Cristos Ifantides’ spouse is an employee of AbbVie and may hold AbbVie stock. Blake K Williamson has received consulting fees from Allergan (an AbbVie company), Bausch + Lomb, BVI, Glaukos, Johnson & Johnson, New World Medical, Sight Sciences, Staar, and Zeiss. Shane Kannarr has received consulting fees, honoraria, speaker fees, and/or travel reimbursements from Alcon Vision, Allergan (an AbbVie company), Bausch + Lomb, Essilor, Johnson & Johnson, Kala Pharmaceuticals, Novartis, Osmotica, Sight Sciences, Sun Pharmaceutical, Tarsus, and Vision Source. Julie Whyte is a full-time employee of Endpoint Outcomes, a Lumanity company. Zuoyi Zhang, Travis Yanke, and Scott Schachter are or were full-time employees of AbbVie and may hold AbbVie stock.
Ethical Approval
The protocol was prospectively approved (on 17 December 2021) by the Western Copernicus Group Institutional Review Board (tracking number: 20216789) before any of the participants were contacted. The study was conducted in accordance with ethical principles of the Declaration of Helsinki and followed the guidelines of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use and applicable regulatory requirements. Individuals who agreed to participate provided written informed consent before initiating the companion study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shafer, B.M., McGee, S.R., Ifantides, C. et al. Understanding Perspectives on Presbyopia and Use of Pilocarpine HCl 1.25% Twice Daily from Participants of the Phase 3 VIRGO Study. Ophthalmol Ther 13, 1723–1742 (2024). https://doi.org/10.1007/s40123-024-00935-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00935-w