Abstract
Introduction
The aim of this work is to investigate the dynamic changes of capsular-intraocular lens (IOL) adhesion in plate-haptic hydrophilic and loop-haptic hydrophobic eyes.
Methods
Cataract eyes that met the inclusion criteria were randomly assigned to receive implantation of a plate-haptic hydrophilic or loop-haptic IOL. The anterior capsular adhesion, posterior capsular adhesion, and the configurations of the capsular bend were evaluated using swept-source optical coherence tomography at 1 day, 1 week, 1 month, and 3 months postoperatively.
Results
In total, 66 eyes of 66 patients were eligible for the analysis: 33 in the plate-haptic group and 33 in the loop-haptic group. The contact between the anterior capsule and IOL in the plate-haptic group was earlier than that in the loop-haptic group upon comparing the measurements taken at 1 day and 1 week (p = 0.001, p = 0.003, respectively). The complete attachment of the posterior capsule and IOL in the plate-haptic group was significantly greater at 1 week, 1 month, and 3 months (p = 0.001, p = 0.000, p = 0.001, respectively). The capsular bend index of the plate-haptic group was significantly greater than that of the loop-haptic group at each time points except at 1 day (p = 0.007, p = 0.049, p = 0.005, respectively). Furthermore, a new type of capsular bend, “cocked adhesion,” was observed in the plate-haptic eyes.
Conclusions
The plate-haptic IOL demonstrated excellent capsular adhesion compared to the loop-haptic IOL, which was probably attributed to haptic compressibility. A special cocked configuration of the capsular bend in plate-haptic IOL was observed for the first time. Further studies are warranted to confirm the effect of the new type of capsular bend.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Capsular-intraocular lens (IOL) adhesion is a critical factor affecting the optical performance and clinical outcomes following cataract surgery. |
Haptic design has also been described as an important factor influencing the long-term capsular bend configuration. |
Plate-haptic design IOLs has been widely used. However, few studies focus on the dynamic changes between the plate-haptic IOL and capsule. |
What was learned from the study? |
This study demonstrated that capsule adhesion to plate-haptic IOL was excellent compared to loop-haptic IOL. |
A special configuration of capsular bend was observed. These features presumably reshaped our understanding of capsular-IOL evolution postoperatively. |
Introduction
The dynamic process involving intraocular lenses (IOLs) and capsular bag is a critical factor affecting the optical performance and clinical outcomes following cataract surgery. Several studies have emphasized that the strong adhesion between the IOL and lens capsule prevents posterior capsule opacification (PCO) formation and anterior capsule contraction [1] attributed to lens epithelial cell(LEC) proliferation and migration. Capsular-IOL adhesion seems to be the key for understanding the biological behavior of the capsular-IOL complex.
Postoperative capsular adhesion with IOL results from many factors, including IOL design, IOL materials [2], surgery [3], and axial length [4]. Previous studies have confirmed that the capsular apposition to the IOL was impacted by the IOL design [5]. Most of the studies focused on the optic edge design [6, 7]. Haptic design has also been described as an important factor influencing the long-term capsular bend configuration [8]. The configuration of the haptic could affect the friction between the IOL and capsular bags [9].
At present, plate-haptic design IOLs have been used in clinical practice for many years. Considering the plate-haptic design, bifocal, trifocal, astigmatism correction, and trifocal astigmatism correction IOL has been widely used. The plate-haptic toric IOLs tended to be more stable intraoperatively [10, 11]. However, few studies exist concerning the dynamic changes between the plate-haptic IOL and capsule.
To our knowledge, no studies have focused on the plate-haptic IOL changes with the capsule. Thus, we investigated the capsular–IOL interactions in plate- and loop-haptic eyes.
Methods
This prospective study was conducted at the Eye Hospital of Wenzhou Medical University, Hangzhou, between July 2020 and July 2021. This prospective study was approved by the Institutional Review Board/Ethics Committee of the eye hospital affiliated Wenzhou Medical University. Practices and research were conducted in accordance with the tenets of the Declaration of Helsinki. The study was registered at www.clinicaltrials.gov and the clinical trial accession number is NCT05148741. Informed consent to participate in the study was obtained from all patients.
The inclusion criteria were as follows: (1) patients with age-related cataract who underwent uncomplicated cataract surgery, (2) axial length within the normal range (22–26 mm), (3) anterior capsule completely covering the IOL optics, (4) pupil could be fully dilated at least at 7 mm during each follow-up. The exclusion criteria included a history of corneal opacity, uveitis, glaucoma, high myopia, and other eye diseases; any other previous intraocular surgery; poor mydriasis; incomplete anterior capsulorrhexis overlapping the IOL optic; and being unavailable for follow-up.
Surgical Technique
Surgeries were performed by the same surgeon (Z.Y.E). Phacoemulsification was performed through a 2.0-mm clear corneal incision. Central continuous curvilinear capsulorhexis was performed and the IOL was implanted into the capsule bag horizontally, followed by viscoelastic material removal behind the optic. Topical steroidal eye drops (tobra-mycin and dexamethasone; Alcon Laboratories, Inc., Fort Worth, TX, USA) were administered after the surgery to all the patients four times a day and tapered for 1 month; antibiotic eye drops (levofloxacin; Santen, Inc., Suzhou, China) were prescribed for 2 weeks.
Intraocular Lens
The patients were divided into two groups based on the type of IOL: plate-haptic IOL (509 M, Carl Zeiss, Meditec, Jena, Germany) and loop-haptic IOL (SN6AWF, Alcon, Fort Worth, TX, USA). The characteristics of the plate- and loop-haptic IOLs are shown in Table 1.
Postoperative Measurements Using Swept-Source Optical Coherence Tomography (SS-OCT)
The Fourier-domain SS-OCT (Casia SS-1000, Tomey, Nagoya, Japan) is a commercially available SS-OCT with a swept-source laser wavelength of 1310 nm. It scans with a high speed of 30,000 A-scans/second and each image comprises 512 A- scans. Each three-dimensional radial scanning takes only 2.4 s and 128 cross-sectional images of the anterior segment are captured. Measurements and image analysis are performed by the same inspector. The standard SS-OCT scans were performed in all the eyes. The Capsular-IOL adhesion was evaluated by analyzing anterior and posterior capsule adhesion. Capsular bends were evaluated using the scans perpendicular to the haptic as 0° and ± 30° of the three lower optic districts (Fig. 1). As previous studies, the capsular bend index (CBI) represented the average bending degree of the capsule in different sections [7]. The bending of the capsule was recorded as 0 to 4 in three fixed sections (at the bottom of optic edge with an angle of 0° and ± 30° to the haptics). The three scores of the same eye were integrated into the CBI formula: \({\text{CBI}}=1/3{\sum }_{k=1}^{3}\mathrm{CK }\)(CK represented is the stage of capsular bend of different sections).
The mean postoperative change in the capsular bend until the 3-month follow-up time was evaluated using the following formula:
The follow-up examinations were performed at 1 day, 1 week, 1 month, and 3 months after the surgery.
Statistical Analysis
Pass 15.0 (NCSs, USA) was used to calculate the sample size. The CBI score was considered as the main parameter. The calculated sample size was 18 cases (18 eyes) in each group (alpha = 0.05; beta = 0.90). Considering the loss of follow-up rate as 20%, at least 23 eyes were included in each group.
Statistical analysis was performed using IBM SPSS Statistics ver. 26.0 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). The Kolmogorov–Smirnov test was used to determine the normality of the data distribution; paired t tests and Mann–Whitney U tests were used for the pairwise comparisons. Repeated measures analysis of variance was used for evaluating the parameters at different time points. A p value of less than 0.05 was considered statistically significant.
Results
Patient Characteristics
From July 2020 to July 2021, 80 patients (80 eyes) undergoing cataract surgery were enrolled and evaluated. We excluded one patient (one eyes) owing to vitreous hemorrhage; six patients (six eyes) were excluded owing to poor pupil dilation. Seven patients (seven eyes) failed to return for follow-up on time. Thus, in total, 66 eyes from 66 patients were eligible for inclusion in the study and underwent data analysis, including 33 eyes for each group. No statistically significant differences were observed in the age, axial length, and sex, except for the IOL diopter (Table 2). There were no significant differences in the intraocular pressure (IOP) during the follow-up time in the two groups.
Dynamic Changes in Capsule Adhesion with the IOL
Anterior Capsular Adhesion
The anterior capsule came in contact with the IOL earlier in the plate-haptic group compared to the loop-haptic group. Fisher’s exact test showed significant difference between the plate- and loop-haptic eyes considering anterior capsular-IOL adhesion upon comparing the measurements taken at 1 day and 1 week postoperatively (p = 0.001, p = 0.003, respectively). The most anterior capsules achieved perfect adhesion with the IOL in both the groups at 1 month and 3 months postoperatively (97 vs. 94%, p = 0.558) (Fig. 2).
Posterior Capsular Adhesion
Figure 3 summarizes the percentage of eyes with first found perfect adhesion between the posterior capsule and IOL optic at each follow-up time in both of the groups. No significant differences were observed between the complete attachment of the posterior capsule and IOL at 1 day after surgery in the plate- and loop-haptic groups. The difference was statistically significant at 1 week and 1 month postoperatively (p = 0.001, p = 0.000, respectively). At 3 months postoperatively, the posterior capsules were completely attached to the IOL in 32 eyes (97%) in the plate-haptic group, which was significantly greater than that in the loop-haptic group (p = 0.001). For the loop-haptic group, 15 eyes had incomplete contact between the IOL and the posterior capsule at 3 months after surgery.
Number (%) of eyes with posterior capsule-intraocular lens (IOL) adhesion at each follow-up between the plate-haptic and loop-haptic groups. N-A non-attached, I-A incomplete attachment, C-A completed attachment, NS no significance (p value > 0.05); **Statistically significant differences among groups (p value < 0.01). ***Statistically significant differences among groups (p value < 0.01)
CBI
The post-operative capsular bend formation of the plate-haptic group seemed quicker than that of the loop-haptic group throughout the follow-up time. The difference between them was significant at every time point except for 1 day (Table 3). The mean CBIRMS was similar during the 3 months after surgery between the two groups.
Types of Capsular Bends
Various configurations of capsular bends were observed at the 3 months’ follow-up time. As shown in Table 4, “Anterior adhesion” was found in more images of loop-haptic compared to the plate-haptic group. A new type of capsular bend, “Cocked adhesion” (posterior capsule bypassed the edge of the optic, fusing with the anterior capsule cocked from the surface of the IOL) was observed. The “Cocked” configuration accounted for 35% of the bends in 99 images of plate-haptic eyes, which was not observed in loop-haptic eyes.
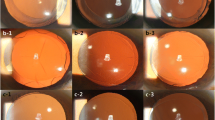
Figure 4 illustrates the changes in the SS-OCT images of a representative patient in the plate-haptic and loop-haptic groups. In an eye with a plate-haptic IOL, the anterior capsule was not contacting the optic at 1 day following the surgery. At 1 week, the anterior capsule was opposed to the optic. The posterior capsule had fully contacted the optic. The capsular bend was completed at 1 month. At 3 months, the anterior capsule and fused posterior capsule showed marked scattering of light combined with the trend of cocked from the optic.
In an eye with a loop-haptic IOL, the anterior and posterior capsule remained separate from the optic at 1 day and 1 week. At 1 month, the anterior capsule was contacted with the IOL and the capsular bend was formed. At 3 months, the completed capsular bend was parallel with the optic section.
Discussion
In this study, we analyzed the dynamic changes of capsular-IOL adhesion between plate-haptic hydrophilic and loop-haptic hydrophobic eyes and found that plate-haptic hydrophilic IOL demonstrated excellent postoperative capsule adhesion. Notably, a new type of capsular bend, “Cocked adhesion” was observed in plate-haptic eyes.
In our study, the speed of CBI formation was quicker in the plate-haptic IOL than in the loop-haptic IOL. The apposition of the plate-haptic IOL to the posterior capsule was complete in most patients at 1 month, while only half of the posterior capsule with loop-haptic IOLs were adherent at 1 month and 3 months postoperatively. Thus, the plate-haptic IOL had excellent capsular adhesion compared with the loop-haptic IOL. This can be the reason the plate-haptic toric IOL was more stable [10,11,12,13]. Previous studies revealed that toric IOL rotation occurs in the early stage following IOL implantation and also found prompt adhesion of the IOL capsule with the plate-type haptic could be attributed to excellent IOL stability [14].
We consider the differences between the two IOLs in haptic compressibility with capsule maybe the reason [9]. The plate-haptic configuration distributes the force along the capsular bag in four points, which could increase the force between the IOL and lens capsule. This stress could actively enhance the peripheral posterior capsule contact with the IOL. While the loop haptics contacted with capsule in two dictions, which produce less compressibility with capsule.
The experimental study of real-time lenticular imaging and quantified capsular dynamics during implantation of different IOLs revealed that the plate-type IOL demonstrated the highest values of capsular deformation compared to the loop haptic IOL [15]. This finding could be used to explain our result that the stress of the capsule was higher following plate-haptic IOL implantation. The strong deformation of the capsule could also result in better capsular stability of plate-haptic IOLs in high myopia eyes.
We found that the posterior capsule bypassed the edge of the optic and fused with the anterior capsule cocked from the surface of the IOL at 3 months postoperatively in a few of plate-haptic eyes. We defined the new configuration of the capsular bend as “cocked” configuration. The reason for this special configuration was uncertain since it was not reported in previous studies [16].
Hayashi et al. [17] speculated three stages of IOL fixation in the lens capsule. However, the subsequent evolution was overlooked once the capsular bend was formed. The Soemmering’s ring formed in the capsular bag periphery could reportedly result in redivision of the fusion of the capsular bend after 10 years following surgery [18]. As the proliferative pressure of the LECs exceeds the adhesive forces between the IOL and the capsule, the capsular bend may be ultimately eliminated.
To the best of our knowledge, this is the first study describing the special cocked configuration of the capsular bend in plate-haptic IOLs in the early stage postoperatively.
We speculated two factors for the “cocked” configuration capsule type formed in the plate-haptic IOL in the early stage postoperatively. First, the essential hydrophilic material in the plate-haptic IOL could result in strong capsulorhexis contraction and greater amount of ACO. The fibrosis of anterior capsule contraction could stretch the anterior zonula moving the posterior capsule upward and forward [1]. On the other hand, although the fibrosis of the anterior capsule was also found in the loop-haptic group, no “cocked adhesion” was observed. The wide plate haptic stretched backward by the anterior zonule could be another key factor. The cooperation of the two drive forces precipitated the configuration of the capsular bend attributed to the opposite direction of the optics.
Previous studies have supported the conclusion that strong adhesion of the capsular bend was most resistant to reopening of the bag owing to LECs proliferation from the capsule equator. This remained us that we should pay more attention of the relationship between the “cocked” capsular bend and PCO.
Several limitations exist in this study. Firstly, the number of patients was small and the duration of follow-up time was only 3 months. More samples and longer follow-up time are required in future studies. Secondly, although both the IOLs had a hydrophobic surface, the material of the IOLs were different. The plate-haptic IOL had a hydrophilic acrylic material with surface hydrophobicity, while the loop-haptic IOL had a hydrophobic acrylate material. Thirdly, part of the IOLs were unable to completely expose the optic edges even when the pupil was dilated over 7 mm. We speculated that this could be associated with the morphology of the preoperative crystalline lenses. We wish to identify the preoperative crystalline lens using plate-IOL tilt and decentration postoperatively.
Conclusion
In conclusion, plate-haptic IOLs demonstrated excellent capsular adhesion compared to loop-haptic IOL. After complete adhesion, a new capsular bend was generated at 3 months postoperatively. We named it “cocked” capsular bend. The “cocked” capsular bend was first observed in plate-haptic IOLs and warrants further attention.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nagata M, Matsushima H, Mukai K, Terauchi W, Gotoh N, Matsui E. Comparison of anterior capsule contraction between 5 foldable intraocular lens models. J Cataract Refract Surg. 2008;34(9):1495–8.
Sacu S, Menapace R, Buehl W, Rainer G, Findl O. Effect of intraocular lens optic edge design and material on fibrotic capsule opacification and capsulorhexis contraction. J Cataract Refract Surg. 2004;30(9):1875–82.
Sacu S, Findl O, Linnola RJ. Optical coherence tomography assessment of capsule closure after cataract surgery. J Cataract Refract Surg. 2005;31(2):330–6.
Zhao Y, Li J, Lu W, et al. Capsular adhesion to intraocular lens in highly myopic eyes evaluated in vivo using ultralong-scan-depth optical coherence tomography. Am J Ophthalmol. 2013;155(3):484-491.e1.
Tao A, Lu P, Li J, et al. High resolution OCT quantitative analysis of the space between the IOL and the posterior capsule during the early cataract postoperative period. Invest Ophthalmol Vis Sci. 2013;54(10):6991–7.
Kohnen T, Fabian E, Gerl R, et al. Optic edge design as long-term factor for posterior capsular opacification rates. Ophthalmology. 2008;115(8):1308-14.e1-3.
Nishi O, Nishi K, Akura J. Speed of capsular bend formation at the optic edge of acrylic, silicone, and poly(methyl methacrylate) lenses. J Cataract Refract Surg. 2002;28(3):431–7.
Sacu S, Findl O, Menapace R, Buehl W. Influence of optic edge design, optic material, and haptic design on capsular bend configuration. J Cataract Refract Surg. 2005;31(10):1888–94.
Meacock WR, Spalton DJ. Effect of intraocular lens haptic compressibility on the posterior lens capsule after cataract surgery. J Cataract Refract Surg. 2001;27(9):1366–71.
Zhu X, Meng J, He W, Rong X, Lu Y. Comparison of the rotational stability between plate-haptic toric and C-loop haptic toric IOLs in myopic eyes. J Cataract Refract Surg. 2020;46(10):1353–9.
Prinz A, Neumayer T, Buehl W, et al. Rotational stability and posterior capsule opacification of a plate-haptic and an open-loop-haptic intraocular lens. J Cataract Refract Surg. 2011;37(2):251–7.
Patel CK, Ormonde S, Rosen PH, Bron AJ. Postoperative intraocular lens rotation: a randomized comparison of plate and loop haptic implants. Ophthalmology. 1999;106(11):2190–5 (discussion 2196).
Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325–31.
Till JS, Yoder PR Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg. 2002;28(2):295–301.
Son HS, Shin KU, Kim D, et al. Lenticular imaging: a new experimental and quantitative analysis of capsular dynamics, “choi-apple view.” Transl Vis Sci Technol. 2019;8(3):22.
Meng J, He W, Rong X, Miao A, Lu Y, Zhu X. Decentration and tilt of plate-haptic multifocal intraocular lenses in myopic eyes. Eye Vis (Lond). 2020;7:17.
Hayashi H, Hayashi K, Nakao F, Hayashi F. Elapsed time for capsular apposition to intraocular lens after cataract surgery. Ophthalmology. 2002;109(8):1427–31.
Vock L, Menapace R, Stifter E, Georgopoulos M, Sacu S, Buhl W. Posterior capsule opacification and neodymium:YAG laser capsulotomy rates with a round-edged silicone and a sharp-edged hydrophobic acrylic intraocular lens 10 years after surgery. J Cataract Refract Surg. 2009;35(3):459–65.
Funding
This study was supported by research grants from the "Pioneer" and "Leading Goose" R&D Program of Zhejiang (Grant No. 2022C03070), the Science and Technology Plan Project of Wenzhou Science and Technology Bureau (Y20211009). The journal’s Rapid Service fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Conceptualization: Yune Zhao; Methodology: Yinying Zhao, Zhewen Zhang, Feng Huang; Formal analysis and investigation: Fuman Yang, Pingjun Chang, Dandan Wang; Writing—original draft preparation: Yinying Zhao and Zhewen Zhang; Writing—review and editing: Yinying Zhao and Yune Zhao; Funding acquisition: Yinying Zhao and Yune Zhao.
Corresponding author
Ethics declarations
Conflict of Interest
All named authors confirm that they have no competing interests to declare.
Ethical Approval
This prospective study was conducted at the Eye Hospital of Wenzhou Medical University, Hangzhou, between July 2020 and July 2021. This prospective study was approved by the Institutional Review Board/Ethics Committee of the eye hospital affiliated Wenzhou Medical University. Practices and research were conducted in accordance with the tenets of the Declaration of Helsinki. The study was registered at www.clinicaltrials.gov and the clinical trial accession number is NCT05148741. Informed consent to participate in the study was obtained from all patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhao, Y., Zhang, Z., Yang, F. et al. Dynamic Changes of Capsular-Intraocular Lens Adhesion in Plate-Haptic Hydrophilic and Loop-Haptic Hydrophobic Eyes. Ophthalmol Ther 13, 1527–1535 (2024). https://doi.org/10.1007/s40123-024-00933-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00933-y