Abstract
Introduction
Immune checkpoint inhibitors have made tremendous progress over the last decade in the treatment of cutaneous melanoma, but their application in uveal melanoma treatment is less successful, owing in part to the immunological privilege of the eye and the liver, the most frequent site of metastasis. Nevertheless, the therapeutic outcomes reported currently are less pessimistic.
Methods
In this review, we provide an overview of recent studies of immune checkpoint inhibitors in uveal melanoma and its metastasis and classify studies in this field into three groups: monotherapy of immune checkpoint inhibitors, dual-agent immune checkpoint inhibitors, and immune checkpoint inhibitors combined with other systemic or regional therapies.
Results
Briefly, monotherapy with immune checkpoint inhibitors performed poorly. Dual-agent immune checkpoint inhibitors had slightly better outcomes than traditional treatments, especially in specific patient populations. As for the combination therapy, the combination with other systemic therapies did not show superiority over dual-agent immune checkpoint inhibitors, but combination with hepatic regional therapies was quite promising. Moreover, research on emerging checkpoints is currently limited to the stage of mechanistic studies.
Conclusion
We propose that immune checkpoint inhibitors remain alternative treatments for patients with uveal melanoma, but factors such as cost-effectiveness should also be taken into account. The combination therapy with immune checkpoint inhibitors deserves to be further explored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
No immunotherapy regimen except tebentafusp has shown meaningful efficacy in patients with uveal melanoma with metastasis. |
Monotherapy comprising programmed cell death protein 1 (PD-1), programmed death ligand 1 (PD-L1), or cytotoxic T-lymphocyte associated protein 4 (CTLA-4) inhibitors has shown little clinical benefit in patients with metastatic uveal melanoma. |
Dual-agent checkpoint inhibitors plus the maintenance of a single-agent checkpoint inhibitor are alternative choices for patients with metastatic uveal melanoma. |
Systemic or regional therapies in combination with checkpoint inhibitors are widely studied in ongoing clinical trials, while hepatic regional therapy with adjuvant immune checkpoint inhibitors has shown therapeutic potential for uveal melanoma patients with metastatic disease. |
Therapies for metastatic uveal melanoma targeting emerging checkpoints including lymphocyte-activation gene 3 (LAG3) are being explored in preclinical studies. |
Introduction
Uveal melanoma (UM) is a rare form of melanoma that arises from melanocytes in the uvea. The incidence has ranged from < 1 to > 9 cases per million from 1970 to the 2010s, and varies by geography and race. In northern Europe and Oceania, the incidence is close to 10 per million population, while it is < 1 per million population in Asia and Africa [1]. Over 90% of these tumors reside in the choroid, with a small proportion in the ciliary body and the iris [2]. The incidence of UM varies by race, with significantly greater incidence in White people than in Asian or Black people [3]. Even though the majority of patients with UM are diagnosed with the tumor in situ [4], nearly half of them will ultimately develop distant metastases despite primary ocular treatment. Metastases of UM most frequently involve the liver (93%), with other sites including the lungs (24%), bones (16%), and soft tissues (11%) [5]. With the limited efficacy of metastatic uveal melanoma (MUM) treatment, the overall survival (OS) of patients with MUM is poor [6]. OS rates at 1 and 2 years after the detection of MUM are 43% and 8%, respectively [7, 8]. For those who have received almost all the therapies, the median OS is estimated at 1.07 years [6].
There is no consensus thus far to define standardized management for UM. Brachytherapy and enucleation are commonly used worldwide for the primary foci, while other therapeutic modalities, including laser treatment, regional approaches for metastases, and various systemic therapies, are also widely considered [1]. Nevertheless, in the field of immunotherapy, immune checkpoint inhibitors (ICIs), which have been particularly notable in the development of treatment for advanced cutaneous melanoma (CM) in recent decades [9], are not highly utilized in MUM, partially owing to the immunological privilege of the eye and the liver, the most frequent site of metastasis (Fig. 1). The blood–retina barrier [10] and various immunosuppressive molecular mechanisms including the release of transforming growth factor beta (TGF-β), expression of Fas-ligands, and decreased expression of major histocompatibility complex (MHC) class Ia [11, 12] make ocular immunotherapy almost impossible. As the most common site of metastasis, the liver also possesses immunosuppressive properties as a result of various liver-resident cells including dendritic cells, hepatic stellate cells, Kupffer cells, regulatory T cells (Treg cells), and liver sinusoidal endothelial cells [13,14,15]. In addition, both the mutational burden [16] and programmed death ligand 1 (PD-L1) expression [17] are low in UM cells. Thus, ICIs are often considered mediocre for treating MUM by many oncologists and are not prioritized in clinical practice. Nevertheless, outcomes from recently published clinical data and research have been less pessimistic than expected, demonstrating treatment effects with the use of ICIs in different regimens that are not inferior to common therapeutic modalities (Fig. 2).
Uveal melanoma in the immune-privileged environment of the eye and the liver. The blood–retina barrier mechanically and the regulation of molecular expression in aqueous humor chemically contribute to immunological privilege of the eye. Immunological privilege in the liver depends primarily on liver-resident cells. MHC major histocompatibility complex, IDO indoleamine 2,3-dioxygenase, MIF macrophage migration inhibitory factor, TGF-β transforming growth factor beta, Treg cells regulatory T cells
Different ICI-related therapies for uveal melanoma and its liver metastases. ICIs are applied to uveal melanoma and its liver metastases mainly in the form of monotherapy, dual-agent therapy, and in combination with other systemic or regional therapies. ICIs immune checkpoint inhibitors, PD 1 programmed cell death protein 1, PD L1 programmed death ligand 1, CTLA-4 cytotoxic T-lymphocyte associated protein 4
In the meantime, emerging strategies for immunotherapy including cancer vaccines [18, 19], cell therapy [20,21,22], oncolytic virus [23,24,25], and immune-mobilizing monoclonal T-cell receptors against cancer (ImmTAC) [26,27,28] are attracting widespread research attention and showing potential in treating UM. Critically, tabentafusp, the newest ImmTAC, which can redirect CD3+ T cells to gp100-expressing UM cells, has achieved inspiring improvements in clinical outcomes [1]. It has been approved in countries such as the United States and countries of the European Union for the treatment of specific patients and has become the star that has gained the most attention from researchers in the field. It seems that oncologists' sights have moved to these new therapeutic methods rather than stopping at ICIs. Therefore, the future of ICIs in UM, regarding both the research value and clinical applications, is unknown.
This review is aimed at providing clinicians and researchers with the latest resources and perspectives on the future of ICIs in MUM, as well as calling for further investigations in this field.
Methods
In this review, we summarize recent studies, in particular clinical trials and retrospective studies, concerning monotherapy with ICIs, dual-agent ICIs, or ICIs combined with other therapies for treating MUM.
We conducted a search of PubMed and Embase using the following key search terms: “uveal melanoma,” “melanoma of the uvea,” “ocular melanoma,” “eye melanoma,” “choroidal melanoma,” “immune checkpoint inhibitor,” “checkpoint inhibitor,” “immune checkpoint blockers,” “checkpoint blockers,” “immune checkpoint blockade,” “checkpoint blockade,” “immune checkpoint inhibition,” “checkpoint inhibition,” “PD-L1 inhibitors,” “PD L1 inhibitors,” “PD-1 inhibitors,” “PD 1 inhibitors,” “programmed cell death protein 1 inhibitors,” “programmed death-ligand 1 inhibitors,” “programmed death ligand 1 inhibitors,” “PD-1 blockade,” “PD-L1 blockade,” “PD 1 blockade,” “PD L1 blockade,” “CTLA-4 inhibitors,” “CTLA 4 inhibitors,” “cytotoxic T-lymphocyte-associated protein 4 inhibitors,” “cytotoxic T lymphocyte associated protein 4 inhibitors,” and “immunotherapy.” Boolean operators “AND” and “OR” were used. The last access date was 10 December 2023. All papers in English discussing ICIs in UM were eligible for inclusion. Books and documents were excluded. Additionally, we searched ClinicalTrials.gov with the terms “uveal melanoma,” “ocular melanoma,” and “‘choroidal melanoma” to include clinical trials which were not reported on PubMed or Embase.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Current Status of Clinical Studies Regarding ICIs in Patients with MUM
ICIs as Monotherapy
In clinical studies concerning melanoma, patients with UM have always been excluded due to obvious differences between UM and common melanoma such as CM. However, after the cytotoxic T-lymphocyte associated protein 4 (CTLA-4) inhibitor ipilimumab was approved by the Food and Drug Administration (FDA) as the first drug for metastatic CM therapy in 2011 [29], research on the use of ICIs in cancer therapy has expanded to the field of UM. Unfortunately, the efficacy of single-agent ICIs in treating UM has not met expectations. Here, we present the most recent clinical studies of several inhibitors of immune checkpoint programmed cell death protein 1 (PD-1) (pembrolizumab and nivolumab), PD-L1 (avelumab), and CTLA-4 (ipilimumab) as monotherapy regimens (Table 1).
Monotherapy with PD-1 Inhibitors
Five patients with UM were treated with pembrolizumab in a terminated phase II trial [30]. Three patients had liver metastasis and the other two had prior chemotherapy. One with prior therapy and no liver metastasis achieved complete response (CR), two showed stable disease (SD), and the other two patients who had bulky liver involvement experienced rapid progression. In another study, the efficacy and safety of pembrolizumab as first-line therapy for MUM was assessed in a prospective cohort. Among 17 patients with histologically confirmed advanced UM without any prior systemic anticancer treatment, an overall response rate (ORR) of 11.7% and 3.8-month median progression-free survival (PFS) were observed, and patients with metastasis detected after more than 5 years after the diagnosis of the primary tumor had longer median PFS than those with an interval of less than 5 years (9.7 months vs. 2.6 months, P = 0.039) [31]. In addition, a retrospective study demonstrated limited efficacy of pembrolizumab, with a 4.5-month median PFS and an 11.5-month median OS in nine patients with stage IV UM (eight with metastasis) [32]. Nivolumab, another antibody against PD-1, was assessed in a large single-arm phase II trial with 1008 patients with melanoma whose disease progressed on or after treatment with ipilimumab (103 patients with ocular melanoma with an unknown proportion of UM or MUM) [33]. The median OS of those with ocular melanoma was 12.6 months, which is relatively low among all kinds of melanoma. Further, a retrospective study of 17 patients with MUM reported a median PFS of 5.8 months, a median OS of 10.5 months, and an ORR of 18% with nivolumab therapy [34]. Therefore, results indicate that pembrolizumab or nivolumab monotherapy may not be effective in patients with MUM.
Monotherapy with PD-L1 Inhibitors
Avelumab, an inhibitor of PD-L1, showed poor clinical activity in 16 patients with stage IIIc or IV unresectable metastatic ocular melanoma, with a 1.7-month median PFS and an inestimable median OS in phase Ib results from the JAVELIN Solid Tumor trial [35]. Although patients in this trial had prior standard therapy for metastasis and the proportion of UM was unknown, this monotherapy approach does not seem to demonstrate a clear clinical benefit in patients with MUM.
Monotherapy with CTLA-4 Inhibitors
Ipilimumab, an inhibitor of CTLA-4, showed no superior effects on MUM. The results of a randomized phase II trial comparing the efficacy of ipilimumab with bevacizumab plus nab-paclitaxel in 24 patients with unresectable metastatic melanoma (including the unknown proportion of MUM) demonstrated comparable limited therapeutic efficacy between these two regimens (median OS: 6.8 months vs. 4.6 months; median PFS: 3.1 months vs. 4.6 months; ORR: 8.3% vs. 25.0%) (NCT02158520). Obviously, the ipilimumab monotherapy regimen in MUM should not be reconsidered as it seems not even superior to chemotherapy combined with targeted drugs, both of which have limited effects.
To summarize, none of the ICI monotherapies in these studies resulted in a median OS of more than 1 year in patients with MUM. In light of the very limited clinical benefit from the studies mentioned above, the number of studies on ICI monotherapy in MUM has decreased in recent years. Nevertheless, the results of these studies are sufficient to suggest that monotherapy with existing ICIs has shown frustrating results in patients with MUM and that there is no evidence that monotherapy should be selected as first-line therapy. However, according to two single-arm clinical studies with small samples [30, 36], single-agent pembrolizumab or ipilimumab seems to have finite clinical benefit for patients with UM with low or no metastatic burden, respectively. More large-scale and high-quality trials are needed to validate this potential clinical benefit.
Dual-Agent ICIs
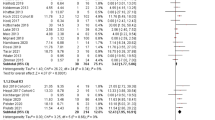
Due to the low effectiveness of monotherapy with conventional ICIs in treating MUM, trials and research are increasingly turning to dual-agent ICIs. Among these treatments, dual-agent anti-PD-1 and anti-CTLA-4 drugs seem to have substantial therapeutic prospects (Table 2).
Clinical Trials Demonstrating Improved Outcomes with Nivolumab Plus Ipilimumab
Piulats et al. conducted a multicenter single-arm phase II trial of nivolumab plus ipilimumab in 52 patients with systemic treatment-naïve MUM (78.8% of them with liver metastasis). Fifty of these patients had undergone local therapy (including enucleation procedure, brachytherapy, external radiotherapy, or conservative surgery) before enrollment in this trial. The treatment showed a 3.0-month median PFS and a 12.7-month median OS, and patients with extrahepatic disease had better survival than those with liver metastasis, although not statistically significant. In addition, the 12-month OS was 51.9% (95% CI, 38.3–65.5) in this trial [37]. A similar single-center phase II trial administered by Pelster et al. presented even better outcomes of 35 patients with MUM (80% with liver metastasis) [38]. The median PFS and the median OS of patients who underwent treatments with the combination of nivolumab and ipilimumab together with the maintenance of nivolumab for up to 2 years were 5.5 months and 19.1 months, respectively [38]. An ORR of 18% was reported. One case with a CR and five cases with partial response were also reported. Notably, dual-agent ICIs were found to have greater drug toxicity than ICI monotherapy. These two clinical trials mentioned above reported grade 3 or greater treatment-related adverse events (TRAEs) in 57.7% and 40% of participants, respectively. While both are viewed by investigators as having manageable toxicity, controlling the number of cycles of dual-agent use may be a way to reduce ICI-related side effects. Therefore, these clinical trials demonstrated that the combination of nivolumab and ipilimumab improved the prognosis of patients with UM, resulting in a higher observed median OS than the average OS of patients with UM receiving any treatment.
Retrospective Studies with Controversial Findings Related to Dual-Agent ICIs
Several retrospective studies have also demonstrated slightly better clinical outcomes for patients treated with dual-agent ICIs [39, 40]. Retrospective data from 16 centers demonstrated a 3.0-month median PFS and a 16.1-month median OS in 64 patients with stage IV MUM (90.6% with liver metastasis) receiving ipilimumab plus nivolumab/pembrolizumab in any treatment line. Complete response and partial response were observed in 3.1% and 12.5%, respectively [41]. Another single-institution retrospective cohort of 47 patients with MUM (98% with liver metastasis) investigated two regimens, nivolumab 1 mg/kg + ipilimumab 3 mg/kg, and nivolumab 3 mg/kg + ipilimumab 1 mg/kg. The median PFS was 4.4 months and 3.0 months, respectively, which was not significantly different. However, only 4% of patients in this study achieved partial response, which may have been because researchers used magnetic resonance imaging (MRI) rather than computed tomography (CT) in order to sensitively assess tumor burden in the liver [42]. Additionally, 89 patients with MUM in 14 centers receiving this combined regimen had a 2.7-month median PFS and 15.0-month median OS [43]. However, the favorable OS or PFS from these retrospective data should be interpreted with caution, as they are inherently limited by the lack of a control group.
In contrast, a single-center retrospective study presented a controversial conclusion that among patients with MUM who received anti-PD-1/L1 + anti-CTLA-4 therapy versus anti-PD-1/L1 monotherapy, no significant difference was found in the clinical response rate, clinical PFS, or OS. The total median clinical PFS and median OS for these two regimens were 2.7 months and 10.0 months, respectively. The similar efficacy may have been because of the toxicity of combined ICIs, which limits the number of therapy cycles. However, as this was a single-center study from Canada, the results may not be generalizable to the broader population. Additionally, the demographic characteristics of patients differed between those receiving monotherapy and those with combination therapy. Among patients receiving single-agent anti-PD-1/L1, 54% were 65 years or older, whereas this proportion in those receiving anti-PD-1 + anti-CTLA-4 was 33%, which may reflect a drug selection bias by oncologists in this center [44]. Overall, the conclusions of these retrospective studies on the effect of dual-agent ICIs are somewhat controversial, and none are sufficiently convincing due to their small samples.
Cases Reported to Benefit from Dual-Agent ICIs
Significant efficacy has been reported in some rare cases [45]. Notably, both a 66-year-old woman [46] and a 53-year-old woman [47] with diffuse MUM treated with the combination of ipilimumab and nivolumab showed almost complete resolution of all metastatic sites. Genetic characteristics may play a role in therapeutic responses, as the former carried several germline single-nucleotide polymorphisms. Although not currently clinically informative, these findings could potentially guide future research.
Taken together, although not comparable to the efficacy approved for CM, dual-agent ICIs can lead to modest improvements in outcomes for patients with UM. These drugs result in more advantageous outcomes than monotherapy with anti-PD-1/L1 drugs or anti-CTLA- drugs in patients with UM, especially those with metastatic disease. Compared with patients with liver metastasis only, patients with diffuse metastases may benefit more from combined ICI therapy [48]. Thus, for patients with MUM who lack options, ICIs are worthy of consideration. Although there has not been a definite biomarker of prognostication for ICIs in MUM, several studies agreed that the lactate dehydrogenase (LDH) level is associated with ICI treatment response [34, 37, 44]. The low LDH values potentially indicate the benefit of treatment of ICIs in MUM [49]. In addition to ensuring both safety and efficacy, long-term maintenance of single-agent ICIs after several cycles of combined ICIs might be the best option for ICI-only therapy for patients with MUM. Especially for those with a low LDH level, therapy based on ICIs might be considered to a great extent.
Combination of ICIs and Other Therapies
In the absence of indications for the use of the bispecific protein tebentafusp, treatment with dual ICIs is sometimes considered in contemporary practice. However, owing to the limited durability of the therapeutic benefit of these agents, studies of other therapies combined with ICIs in patients with MUM have been conducted in recent years. Tremendous ongoing prospective clinical trials indicate the great promise of systemic or regional therapy with concomitant ICIs in patients with MUM (Table 3).
Combination of ICIs and Other Systemic Therapies
Epigenetic therapy is suggested to enhance the efficacy of immunotherapy by promoting the expression of additional human leukocyte antigens (HLA) and cancer antigens in tumor cells to upregulate their immunogenicity. Moreover, for immune checkpoint genes, the methylation of specific CpG sites is strongly associated with their messenger RNA (mRNA) expression levels [50]. In vitro experiments demonstrated that the histone deacetylase inhibitor entinostat could induce HLA and PD-L1 expression in UM cells [51]. The efficacy of treatment with entinostat together with pembrolizumab in 29 patients with stage IV MUM was assessed in the PEMDAC multicenter phase II trial, which showed an ORR of 14%, 2.1-month median PFS, and 13.4-month median OS [52]. The DNA demethylating agent decitabine (5-aza-2′-deoxycytidine), when combined with ICI therapy, also has the potential to treat unresectable liver-predominant metastases including MUM.
To date, clinical studies of other systemic therapies combined with ICIs have demonstrated very limited therapeutic efficacy. In two phase I trials [53, 54], intravenous coxsackievirus A21 (V937) plus ipilimumab, and arginine deprivation plus nivolumab and ipilimumab showed tolerable toxicity but lacked a meaningful clinical benefit in 11 and 9 patients with MUM, respectively. In addition, Zenella et al. reported three MUM cases treated with the mitogen-activated protein kinase kinase (MEK) inhibitor selumetinib and ICIs [55]. Among these patients, serious adverse events were observed and the efficacy of treatment could not be assessed.
Nevertheless, in vivo experiments and experience in the management of other tumors have indicated several potentially effective systemic treatment strategies. Kim et al. suggested that the combination of the rho-kinase (ROCK) inhibitor ripasudil, PD0L1 inhibitor, and local photodynamic therapy (PDT) could reduce the primary tumor burden and prevent metastasis in an orthotopic intraocular melanoma model [56]. A new virus-like drug conjugate (AU-011) and the inhibitor of the receptor for the hepatocyte growth factor (HGF) are also worth studying in systemic treatment combined with ICIs [57, 58].
In summary, with the exception of epigenetic therapy in combination with pembrolizumab, which demonstrated similar clinical benefits to dual-agent ICIs, systemic therapies with combined ICIs have not shown improvements in outcomes.
Combination of ICIs and Regional Therapies
Various liver-targeted therapies for hepatic metastases, as well as their combination with ICIs, have been investigated in this field. For example, in a single-center retrospective study of 42 patients with UM with liver metastasis receiving various treatments, Blomen et al. roughly divided patients into two cohorts: cohort 1 was treated with ICIs plus one of the liver-specific therapies (including surgical resection, selective internal radiation therapy [SIRT], transarterial chemoembolization [TACE] or chemosaturation), and cohort 2 was treated with any other regimens alone or in combination [59]. Compared with cohort 2, cohort 1 demonstrated a significant advantage in median OS (22.5 months vs. 11.4 months, P = 0.036). However, it is clear that different liver-specific therapies vary, and therefore there were limitations in dividing all patients into two cohorts. Additionally, after excluding patients who underwent metastasectomy, the difference was no longer statistically significant (P = 0.074).
SIRT concurrently with ICIs was assessed in several studies. In a multicenter single-arm phase I/II trial, a 5.5-month median PFS, 15-month median OS, and ORR of 20% were observed in 26 patients with UM with hepatic metastasis involving less than 50% of the liver. These patients were treated with hepatic artery infusions with a relatively low dose of yttrium-90 (Y-90) as well as ipilimumab and nivolumab (35 Gy for Y-90 and 1 mg/kg for ipilimumab) [60]. Another patient with MUM was even reported to be free of disease for at least 14 months after treatment with SIRT and ipilimumab [61]. Aedo-Lopez et al. conducted a real-world single-center retrospective cohort study of 32 patients with MUM to compare the safety and efficacy of SIRT with or without the combination of ipilimumab and nivolumab [62]. The median OS was 49.6 months for patients receiving SIRT with ICI, and 13.6 months for patients receiving SIRT only (P = 0.027). However, 44.4% of the patients treated with SIRT and ICIs experienced grade 3 or higher TRAEs, suggesting that ICIs might enhance the efficacy of SIRT at the risk of increasing adverse events. It should also be noted that in the combination therapy group, one third of the patients received ICI first and two thirds received SIRT first. Thus, the results of TRAEs should be interpreted with caution.
The potential benefit of radiotherapy combined with ICIs was assessed via retrospective data. Radiotherapy plus pembrolizumab in 22 patients with MUM had a 4.8-month median PFS and a 21.2-month median OS [63]. Grynberg et al. reported that radiotherapy could significantly enhance the efficacy of dual or single ICIs by comparing the clinical outcomes of ICI therapies with or without radiotherapy (median PFS: 22 months vs. 3 months; median OS: 26 months vs. 7.5 months: ORR: 44% vs. 10%) [64]. However, the credibility of these surprising results might be compromised by the differing ICI regimens and baseline patient profiles between the two groups. In the group of patients treated with the combination of radiotherapy and ICIs, the proportion receiving dual-agent ICIs was higher than that in the group of patients with ICIs only.
For other regional therapies, the ongoing CHOPIN randomized phase Ib/II trial has been exploring the clinical efficacy of melphalan percutaneous hepatic perfusion with ipilimumab plus nivolumab in patients with MUM and has defined the safe dose as ipilimumab 1 mg/kg and nivolumab 3 mg/kg [65, 66]. The SECIRA-UM trial also investigated combined radio-frequency ablation and ipilimumab in MUM, with a 3-month median PFS and 14.2/9.7-month median OS for two different doses of ipilimumab [67]. In addition, eight patients with MUM in a small retrospective study received a combination of TACE, ipilimumab, and nivolumab, with two and four patients achieving a partial response (PR) and SD, respectively [68].
Thus, according to the research described above, ICIs could play a promising role as adjuvant or neoadjuvant therapy for patients with UM with metastases where surgery, SIRT, or other local therapy is conducted as the core treatment.
To sum up, many studies are being conducted in the field of ICIs in combination with other systemic and regional therapies. Research reported so far has not demonstrated a greater clinical benefit of systemic treatment with combined ICIs over dual-agent ICIs. As an emerging therapeutic strategy, ICIs combined with epigenetic therapy have great potential, but additional research is needed. Notably, the combination of ICIs and regional therapies seems to have favorable clinical outcomes. Considering that surgical resection can provide substantial clinical benefits in patients with UM liver metastasis, it should still be preferred if indications are met [69]. Muraki et al. reported that a 53-year-old woman with multiple liver metastases of choroidal malignant melanoma underwent treatment with surgery and adjuvant nivolumab, with no recurrence appearing for 22 months [70]. Clinical studies of neoadjuvant or adjuvant ICIs with surgical resection should be conducted to validate their efficacy. Additionally, the combination of ICIs plus SIRT or radiotherapy has demonstrated even greater than 25-month median OS in current retrospective studies. However, safety should be carefully monitored, as studies have reported excessive toxicity in this combination therapy. Although larger prospective studies are warranted to confirm the efficacy, these regimens with proper doses could still be options for patients with MUM in the absence of a better alternative.
New Immune Checkpoint Targets
In addition to the well-known immune checkpoints CTLA-4 and PD-1/L1, and in light of the low response rate of their inhibitors in MUM, emerging immune checkpoints have been explored in preclinical studies.
Lymphocyte-Activation Gene 3 and Its Inhibitor
Lymphocyte-activation gene 3 (LAG3) which is closely related to CD4, expressed on the surface of T cells, natural killer (NK) cells, and plasmacytoid dendritic cells [71], is an inhibitory co-receptor that plays a crucial role in immune tolerance [72]. Souri et al. reported that LAG3 and its ligand galectin-3 are increasingly expressed in UM with monosomy 3/BAP1 loss [73]. With a similar conclusion, Kashyap et al. also found a potential association between higher LAG3 expression and shorter metastasis-free survival [74]. An in vivo experiment by Huis In 't Veld et al. showed a CR rate of 75% in a murine model with distant MC38 tumors after treatment with AU-011 and a LAG3 inhibitor [57]. Thus, by observing valuable results from in vitro and in vivo experiments, the clinical effect of antibodies against LAG3 in UM, especially in the process of tumor metastasis, deserves to be investigated and validated.
Other Potential Targets of Immune Checkpoint Inhibitors
Other emerging immune checkpoints have been noted for their targetable potential. In UM tissue, Stålhammar et al. observed a significant increase in T-cell immunoglobulin and ITIM domain (TIGIT)-positive cells in primary UM that eventually developed metastases compared with those that did not (P < 0.01). A correlation was also found between increased expression of both TIGIT and indoleamine 2,3-dioxygenase (IDO) [75]. Protein tyrosine phosphatase 1B (PTP1B) [76] and tumor necrosis factor-alpha-induced protein-8 like 2 (TNFAIP8L2) [77] were found to be highly expressed in most tumors (including UM) and associated with poor prognosis in patients with UM. The latter was also found to significantly affect the tumor immune microenvironment, such as the stem cell index and dendritic cell infiltration. However, the specific mechanism of these immune checkpoints is unclear, and further research needs to be carried out.
In general, although immune checkpoints are increasingly being discovered and thought to be targetable in UM therapy, exploration of these checkpoints is still limited to immunohistochemical analyses of tumor samples and initial mechanistic studies. There is still a long way to go in translating these potential druggable targets into therapeutic agents for treating UM.
Conclusion
While most studies have used median OS and median PFS as their primary outcome metrics for evaluating the efficacy of ICIs or other immunotherapies in patients with UM, PFS has not differed significantly among therapy modalities. Even the landmark tebentafusp trial achieved a median PFS of only 3.3 months and showed no superiority [78]. This is partially due to the fact that the effect of immunotherapies is often not immediate but is long-lasting, resulting in PFS with a similar duration. Thus, for patients with UM, who have a poor prognosis and no standard treatment yet, clinical decisions about various immunotherapies could also be made with reference to OS and other long-term metrics.
Clearly, with regard to OS, the therapeutic efficacy of single-agent ICIs, dual-agent ICIs, or therapy with concomitant ICIs is inferior to that of tebentafusp, which was assessed in an open-label phase III trial and demonstrated a 21.6-month median OS and a 1-year OS rate of 73% in patients with MUM [78, 79]. Nevertheless, this benefit was limited to HLA-A*02:01-positive patients only. In addition, cost-effectiveness is equally important for patients in choosing a treatment modality. As a newly developed and approved effective orphan drug, tebentafusp puts considerable financial pressure on the potential beneficiaries. In light of the current price, tebentafusp may not be beneficial for improving outcomes in patients with MUM. Using a three-state partitioned survival model, researchers found that, compared to a control group (monotherapy of pembrolizumab, ipilimumab, or dacarbazine), tebentafusp led to an increase of 0.47 quality-adjusted life years (QALYs) and an incremental cost of $444,280 for patients with MUM. The willingness-to-pay threshold for US payers was $200,000/QALY, which is far less than the incremental cost-effectiveness ratio (ICER) of tebentafusp ($953,230/QALY) [80].
Unfortunately, no research has been published on whether ICIs are cost-effective in treating UM compared to other conventional therapies. For other types of melanoma, research has been conducted in several countries on the cost-effectiveness of single-agent or combined ICIs, drawing controversial conclusions [81,82,83,84]. For example, for patients with advanced melanoma in Iran, researchers compared ipilimumab, nivolumab, and the combination of ipilimumab and nivolumab with temozolomide, which showed ICERs of $40,365.53, $19,591.13, and $24,578 per QALY, respectively. None of these ICI regimens was found to be cost-effective when compared with the cost-effectiveness threshold of $3532 in Iran [81]. However, in analysis using similar models, the combination of nivolumab and ipilimumab for advanced melanoma in Japan was considered to be cost-effective [82]. Therefore, studies specifically focused on the cost-effectiveness of ICIs in UM are needed. Obviously, demographic/economic factors in different countries/regions should also be taken into account. Additionally, region-specific clinical data are more valuable when examining the cost-effectiveness of ICIs in UM in a certain country/region. Considering the apparent low incidence of UM, the availability of a large amount of region-specific clinical data is one of the major challenges for cost-effectiveness studies of ICIs in UM.
In conclusion, completed clinical trials have demonstrated that both dual-agent ICIs and SIRT plus ICIs are effective, with a manageable toxicity profile, in treating patients with MUM [37, 38, 60]. When the patients' genetic characteristics limit the option of tebentafusp, these two regimens should be considered for patients.
However, there still remain gaps and challenges for future research of ICIs in UM. Firstly, existing studies have mainly focused on patients with unresectable MUM, and thus studies discussing the combination of ICIs and liver metastasis resection are rare. Given the priority of surgery for patients with MUM, studies of ICIs as a neoadjuvant or an adjuvant therapy to surgery are critically needed. Additionally, according to the search results on ClinicalTrials.gov, many clinical trials focusing on the combination of ICIs and other systemic or regional therapies are recruiting patients. In these studies, the potential increase in TRAEs from combination therapies is noted and requires increased attention in monitoring and interpreting treatment safety metrics. The bias caused by treatment sequence for each patient must also be controlled. Furthermore, new checkpoint inhibitors are in the early stage of research, and additional clinical studies are needed. However, as patients with UM have frequently been excluded from trials in patients with melanoma in previous studies, separate cohorts of patients with UM should be included for future studies. Moreover, because of the poor prognosis of UM, slight improvements in OS or PFS in future studies would be promising. But results should be viewed with caution. Together with common tumor metrics for the measurement of outcomes, health economics metrics mentioned above, including QALYs and ICERs, should be emphasized as well when evaluating the advantages and disadvantages of a therapy. Finally, patient inclusion is also a major challenge for future clinical studies. In part because of the low incidence of UM, the number of patients enrolled in clinical trials to date has been limited, thus limiting the studies’ relevance for the ophthalmologist and the oncologist. Studies with large samples are expected.
To summarize, further studies are needed regarding the application of neoadjuvant or adjuvant ICIs together with other therapies and translation from emerging immune checkpoints to effective and economical ICIs. One of the most promising therapies is relatlimab, an inhibitor of LAG3, which has already shown advantages in other types of melanoma. Compared with nivolumab monotherapy, relatlimab provided greater benefit in combination with nivolumab for 714 patients with previously untreated metastatic or unresectable melanoma (UM was excluded) in a global randomized phase III trial [85]. For UM, a phase II single-institution trial investigating relatlimab plus nivolumab in 27 patients with MUM is ongoing, and its therapeutic effects are widely anticipated.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Jager MJ, Shields CL, Cebulla CM, Abdel-Rahman MH, Grossniklaus HE, Stern MH, et al. Uveal melanoma. Nat Rev Dis Prim. 2020;6(1):24. https://doi.org/10.1038/s41572-020-0158-0.
Rodrigues M, Koning L, Coupland SE, Jochemsen AG, Marais R, Stern MH, et al. So close, yet so far: discrepancies between uveal and other melanomas a position paper from UM cure 2020. Cancers. 2019;11(7):1032. https://doi.org/10.3390/cancers11071032.
Hu DN, Yu GP, McCormick SA, Schneider S, Finger PT. Population-based incidence of uveal melanoma in various races and ethnic groups. Am J Ophthalmol. 2005;140(4):612–7. https://doi.org/10.1016/j.ajo.2005.05.034.
Garg G, Finger PT, Kivelä TT, Simpson ER, Gallie BL, Saakyan S, et al. Patients presenting with metastases: stage IV uveal melanoma, an international study. Br J Ophthalmol. 2022;106(4):510–7. https://doi.org/10.1136/bjophthalmol-2020-317949.
Collaborative Ocular Melanoma Study Group. Assessment of metastatic disease status at death in 435 patients with large choroidal melanoma in the collaborative ocular melanoma study (COMS): COMS report no 15. Arch Ophthalmol (Chicago, Ill: 1960). 2001;119(5):670–6. https://doi.org/10.1001/archopht.119.5.670.
Rantala ES, Hernberg M, Kivelä TT. Overall survival after treatment for metastatic uveal melanoma: a systematic review and meta-analysis. Melanoma Res. 2019;29(6):561–8. https://doi.org/10.1097/cmr.0000000000000575.
Krantz BA, Dave N, Komatsubara KM, Marr BP, Carvajal RD. Uveal melanoma: epidemiology, etiology, and treatment of primary disease. Clin Ophthalmol (Auckland, NZ). 2017;11:279–89. https://doi.org/10.2147/opth.S89591.
Khoja L, Atenafu EG, Suciu S, Leyvraz S, Sato T, Marshall E, et al. Meta-analysis in metastatic uveal melanoma to determine progression free and overall survival benchmarks: an international rare cancers initiative (IRCI) ocular melanoma study. Ann Oncol: Off J Eur Soc Med Oncol. 2019;30(8):1370–80. https://doi.org/10.1093/annonc/mdz176.
Franklin C, Livingstone E, Roesch A, Schilling B, Schadendorf D. Immunotherapy in melanoma: recent advances and future directions. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2017;43(3):604–11. https://doi.org/10.1016/j.ejso.2016.07.145.
McMenamin PG, Saban DR, Dando SJ. Immune cells in the retina and choroid: two different tissue environments that require different defenses and surveillance. Prog Retin Eye Res. 2019;70:85–98. https://doi.org/10.1016/j.preteyeres.2018.12.002.
Taylor AW, Alard P, Yee DG, Streilein JW. Aqueous humor induces transforming growth factor-beta (TGF-beta)-producing regulatory T-cells. Curr Eye Res. 1997;16(9):900–8. https://doi.org/10.1076/ceyr.16.9.900.5043.
Ferguson TA, Griffith TS. The role of Fas ligand and TNF-related apoptosis-inducing ligand (TRAIL) in the ocular immune response. Chem Immunol Allergy. 2007;92:140–54. https://doi.org/10.1159/000099265.
Carvajal RD, Sacco JJ, Jager MJ, Eschelman DJ, Olofsson Bagge R, Harbour JW, et al. Advances in the clinical management of uveal melanoma. Nat Rev Clin Oncol. 2023;20(2):99–115. https://doi.org/10.1038/s41571-022-00714-1.
Krishna Y, McCarthy C, Kalirai H, Coupland SE. Inflammatory cell infiltrates in advanced metastatic uveal melanoma. Hum Pathol. 2017;66:159–66. https://doi.org/10.1016/j.humpath.2017.06.005.
Tosi A, Cappellesso R, Dei Tos AP, Rossi V, Aliberti C, Pigozzo J, et al. The immune cell landscape of metastatic uveal melanoma correlates with overall survival. J Exp Clin Cancer Res: CR. 2021;40(1):154. https://doi.org/10.1186/s13046-021-01947-1.
Bastian BC. The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annu Rev Pathol. 2014;9:239–71. https://doi.org/10.1146/annurev-pathol-012513-104658.
Javed A, Arguello D, Johnston C, Gatalica Z, Terai M, Weight RM, et al. PD-L1 expression in tumor metastasis is different between uveal melanoma and cutaneous melanoma. Immunotherapy. 2017;9(16):1323–30. https://doi.org/10.2217/imt-2017-0066.
Koch EAT, Schaft N, Kummer M, Berking C, Schuler G, Hasumi K, et al. A one-armed phase I dose escalation trial design: personalized vaccination with IKKβ-matured, RNA-loaded dendritic cells for metastatic uveal melanoma. Front Immunol. 2022;13: 785231. https://doi.org/10.3389/fimmu.2022.785231.
Bol KF, van den Bosch T, Schreibelt G, Mensink HW, Keunen JE, Kiliç E, et al. Adjuvant dendritic cell vaccination in high-risk uveal melanoma. Ophthalmology. 2016;123(10):2265–7. https://doi.org/10.1016/j.ophtha.2016.06.027.
Gezgin G, Visser M, Ruano D, Santegoets SJ, de Miranda N, van der Velden PA, et al. Tumor-infiltrating t cells can be expanded successfully from primary uveal melanoma after separation from their tumor environment. Ophthalmol Sci. 2022;2(2): 100132. https://doi.org/10.1016/j.xops.2022.100132.
Chodnicki KD, Prasad S. Ophthalmic implications of chimeric antigen receptor T-cell therapy. Semin Ophthalmol. 2021;36(4):329–34. https://doi.org/10.1080/08820538.2021.1897857.
Forsberg EMV, Lindberg MF, Jespersen H, Alsén S, Bagge RO, Donia M, et al. HER2 CAR-T cells eradicate uveal melanoma and T-cell therapy-resistant human melanoma in IL2 transgenic NOD/SCID IL2 receptor knockout mice. Can Res. 2019;79(5):899–904. https://doi.org/10.1158/0008-5472.Can-18-3158.
Liu S, Zhang J, Fang S, Zhang Q, Zhu G, Tian Y, et al. Macrophage polarization contributes to the efficacy of an oncolytic HSV-1 targeting human uveal melanoma in a murine xenograft model. Exp Eye Res. 2021;202: 108285. https://doi.org/10.1016/j.exer.2020.108285.
Li Y, He J, Qiu C, Shang Q, Qian G, Fan X, et al. The oncolytic virus H101 combined with GNAQ siRNA-mediated knockdown reduces uveal melanoma cell viability. J Cell Biochem. 2019;120(4):5766–76. https://doi.org/10.1002/jcb.27863.
Liu S, Li M, Sun F, Zhang J, Liu F. Enhancing the immune effect of oHSV-1 therapy through TLR3 signaling in uveal melanoma. J Cancer Res Clin Oncol. 2023;149(2):901–12. https://doi.org/10.1007/s00432-022-04272-y.
Carvajal RD, Nathan P, Sacco JJ, Orloff M, Hernandez-Aya LF, Yang J, et al. Phase I study of safety, tolerability, and efficacy of tebentafusp using a step-up dosing regimen and expansion in patients with metastatic uveal melanoma. J Clin Oncol Off J Am Soc Clin Oncol. 2022;40(17):1939–48. https://doi.org/10.1200/jco.21.01805.
Carvajal RD, Butler MO, Shoushtari AN, Hassel JC, Ikeguchi A, Hernandez-Aya L, et al. Clinical and molecular response to tebentafusp in previously treated patients with metastatic uveal melanoma: a phase 2 trial. Nat Med. 2022;28(11):2364–73. https://doi.org/10.1038/s41591-022-02015-7.
Middleton MR, McAlpine C, Woodcock VK, Corrie P, Infante JR, Steven NM, et al. Tebentafusp, A TCR/Anti-CD3 bispecific fusion protein targeting gp100, potently activated antitumor immune responses in patients with metastatic melanoma. Clin Cancer Res Off J Am Assoc Cancer Res. 2020;26(22):5869–78. https://doi.org/10.1158/1078-0432.Ccr-20-1247.
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23. https://doi.org/10.1056/NEJMoa1003466.
Johnson DB, Bao R, Ancell KK, Daniels AB, Wallace D, Sosman JA, et al. Response to Anti-PD-1 in uveal melanoma without high-volume liver metastasis. J Natl Compr Cancer Netw: JNCCN. 2019;17(2):114–7. https://doi.org/10.6004/jnccn.2018.7070.
Rossi E, Pagliara MM, Orteschi D, Dosa T, Sammarco MG, Caputo CG, et al. Pembrolizumab as first-line treatment for metastatic uveal melanoma. Cancer Immunol, Immunother: CII. 2019;68(7):1179–85. https://doi.org/10.1007/s00262-019-02352-6.
Jansen YJL, Seremet T, Neyns B. Pembrolizumab for the treatment of uveal melanoma: a case series. Rare Tumors. 2020;12:2036361320971983. https://doi.org/10.1177/2036361320971983.
Nathan P, Ascierto PA, Haanen J, Espinosa E, Demidov L, Garbe C, et al. Safety and efficacy of nivolumab in patients with rare melanoma subtypes who progressed on or after ipilimumab treatment: a single-arm, open-label, phase II study (CheckMate 172). Eur J Cancer (Oxford, England: 1990). 2019;119:168–78. https://doi.org/10.1016/j.ejca.2019.07.010.
Tacar SY, Selcukbiricik F, Yilmaz M, Erturk K, Murat Sarici A, Gulturk I, et al. Nivolumab for metastatic uveal melanoma: a multicenter, retrospective study. Melanoma Res. 2021;31(5):449–55. https://doi.org/10.1097/cmr.0000000000000744.
Keilholz U, Mehnert JM, Bauer S, Bourgeois H, Patel MR, Gravenor D, et al. Avelumab in patients with previously treated metastatic melanoma: phase 1b results from the JAVELIN Solid tumor trial. J Immunother Cancer. 2019;7(1):12. https://doi.org/10.1186/s40425-018-0459-y.
Fountain E, Bassett RL, Cain S, Posada L, Gombos DS, Hwu P, et al. Adjuvant ipilimumab in high-risk uveal melanoma. Cancers. 2019;11(2):152. https://doi.org/10.3390/cancers11020152.
Piulats JM, Espinosa E, de la Cruz ML, Varela M, Alonso Carrión L, Martín-Algarra S, et al. Nivolumab plus ipilimumab for treatment-naïve metastatic uveal melanoma: an open-label, multicenter, phase II trial by the Spanish multidisciplinary melanoma group (GEM-1402). J Clin Oncol: Off J Am Soc Clin Oncol. 2021;39(6):586–98. https://doi.org/10.1200/jco.20.00550.
Pelster MS, Gruschkus SK, Bassett R, Gombos DS, Shephard M, Posada L, et al. Nivolumab and ipilimumab in metastatic uveal melanoma: results from a single-arm phase II study. J Clin Oncol: Off J Am Soc Clin Oncol. 2021;39(6):599–607. https://doi.org/10.1200/jco.20.00605.
Klemen ND, Wang M, Rubinstein JC, Olino K, Clune J, Ariyan S, et al. Survival after checkpoint inhibitors for metastatic acral, mucosal and uveal melanoma. J Immunother Cancer. 2020;8(1): e000341. https://doi.org/10.1136/jitc-2019-000341.
Bol KF, Ellebaek E, Hoejberg L, Bagger MM, Larsen MS, Klausen TW, et al. Real-world impact of immune checkpoint inhibitors in metastatic uveal melanoma. Cancers. 2019;11(10):1489. https://doi.org/10.3390/cancers11101489.
Heppt MV, Amaral T, Kähler KC, Heinzerling L, Hassel JC, Meissner M, et al. Combined immune checkpoint blockade for metastatic uveal melanoma: a retrospective, multi-center study. J Immunother Cancer. 2019;7(1):299. https://doi.org/10.1186/s40425-019-0800-0.
Salaün H, de Koning L, Saint-Ghislain M, Servois V, Ramtohul T, Garcia A, et al. Nivolumab plus ipilimumab in metastatic uveal melanoma: a real-life, retrospective cohort of 47 patients. Oncoimmunology. 2022;11(1):2116845. https://doi.org/10.1080/2162402x.2022.2116845.
Najjar YG, Navrazhina K, Ding F, Bhatia R, Tsai K, Abbate K, et al. Ipilimumab plus nivolumab for patients with metastatic uveal melanoma: a multicenter, retrospective study. J Immunother Cancer. 2020;8(1): e000331. https://doi.org/10.1136/jitc-2019-000331.
Kelly D, Rose AAN, Muniz TP, Hogg D, Butler MO, Saibil SD, et al. Development of a metastatic uveal melanoma prognostic score (MUMPS) for use in patients receiving immune checkpoint inhibitors. Cancers. 2021;13(14):3640. https://doi.org/10.3390/cancers13143640.
Fadel CA, Kanakamedala S, Danak SU, Johnson AT. A rare case of metastatic uveal melanoma responding to immunotherapy. Cureus. 2022;14(6): e26146. https://doi.org/10.7759/cureus.26146.
Yu IS, Wee K, Williamson L, Titmuss E, An J, Naderi-Azad S, et al. Exceptional response to combination ipilimumab and nivolumab in metastatic uveal melanoma: Insights from genomic analysis. Melanoma Res. 2022;32(4):278–85. https://doi.org/10.1097/cmr.0000000000000810.
Miles B, Moth J, Mackey J. Usefulness of nivolumab plus ipilimumab immunotherapy for metastatic uveal melanoma. Proc (Baylor Univ Med Cent). 2020;34(1):118–9. https://doi.org/10.1080/08998280.2020.1825587.
Koch EAT, Petzold A, Wessely A, Dippel E, Gesierich A, Gutzmer R, et al. Immune checkpoint blockade for metastatic uveal melanoma: patterns of response and survival according to the presence of hepatic and extrahepatic metastasis. Cancers. 2021;13(13):3359. https://doi.org/10.3390/cancers13133359.
Waninger JJ, Fecher LA, Lao C, Yentz S, Green MD, Demirci H. Prognostic hematologic biomarkers following immune checkpoint inhibition in metastatic uveal melanoma. Cancers. 2022;14(23):5789. https://doi.org/10.3390/cancers14235789.
de Vos L, Carrillo Cano TM, Zarbl R, Klümper N, Ralser DJ, Franzen A, et al. CTLA4, PD-1, PD-L1, PD-L2, TIM-3, TIGIT, and LAG3 DNA methylation is associated with BAP1 -Aberrancy, transcriptional activity, and overall survival in uveal melanoma. J Immunother (Hagerstown, Md: 1997). 2022;45(7):324–34. https://doi.org/10.1097/cji.0000000000000429.
Sah VR, Karlsson J, Jespersen H, Lindberg MF, Nilsson LM, Ny L, et al. Epigenetic therapy to enhance therapeutic effects of PD-1 inhibition in therapy-resistant melanoma. Melanoma Res. 2022;32(4):241–8. https://doi.org/10.1097/cmr.0000000000000791.
Jespersen H, Olofsson Bagge R, Ullenhag G, Carneiro A, Helgadottir H, Ljuslinder I, et al. Concomitant use of pembrolizumab and entinostat in adult patients with metastatic uveal melanoma (PEMDAC study): protocol for a multicenter phase II open label study. BMC Cancer. 2019;19(1):415. https://doi.org/10.1186/s12885-019-5623-3.
Lutzky J, Sullivan RJ, Cohen JV, Ren Y, Li A, Haq R. Phase 1b study of intravenous coxsackievirus A21 (V937) and ipilimumab for patients with metastatic uveal melanoma. J Cancer Res Clin Oncol. 2023. https://doi.org/10.1007/s00432-022-04510-3.
Kraehenbuehl L, Holland A, Armstrong E, O’Shea S, Mangarin L, Chekalil S, et al. Pilot trial of arginine deprivation plus nivolumab and ipilimumab in patients with metastatic uveal melanoma. Cancers. 2022;14(11):2638. https://doi.org/10.3390/cancers14112638.
Zanella A, Doussot A, Puzenat E, Aubin F, Nardin C. MEK inhibitors combined with programmed cell death-1 blockade immunotherapy for metastatic uveal melanoma: is it warranted? Melanoma Res. 2020;30(6):606–7. https://doi.org/10.1097/cmr.0000000000000677.
Kim S, Kim SA, Nam GH, Hong Y, Kim GB, Choi Y, et al. In situ immunogenic clearance induced by a combination of photodynamic therapy and rho-kinase inhibition sensitizes immune checkpoint blockade response to elicit systemic antitumor immunity against intraocular melanoma and its metastasis. J Immunother Cancer. 2021;9(1): e001481. https://doi.org/10.1136/jitc-2020-001481.
Huis In ’t Veld RV, Ma S, Kines RC, Savinainen A, Rich C, Ossendorp F, et al. Immune checkpoint inhibition combined with targeted therapy using a novel virus-like drug conjugate induces complete responses in a murine model of local and distant tumors. Cancer Immunol Immunother: CII. 2023. https://doi.org/10.1007/s00262-023-03425-3.
Machiraju D, Hassel JC. Targeting the cMET pathway to enhance immunotherapeutic approaches for mUM patients. Front Oncol. 2022;12:1068029. https://doi.org/10.3389/fonc.2022.1068029.
Blomen CL, Kött J, Hartung TI, Torster LK, Gebhardt C. Combination of immune checkpoint inhibitors and liver-specific therapies in liver-metastatic uveal melanoma: can we thus overcome its high resistance? Cancers. 2021;13(24):6390. https://doi.org/10.3390/cancers13246390.
Minor DR, Kim KB, Tong RT, Wu MC, Kashani-Sabet M, Orloff M, et al. A pilot study of hepatic irradiation with Yttrium-90 microspheres followed by immunotherapy with ipilimumab and nivolumab for metastatic uveal melanoma. Cancer Biother Radiopharm. 2022;37(1):11–6. https://doi.org/10.1089/cbr.2021.0366.
Proietti I, Skroza N, Filippi L, Bernardini N, Mambrin A, Tolino E, et al. Long-term maintained response to selective internal radiation therapy in an oligometastatic uveal melanoma patient treated with concomitant anti-PD-1 therapy. Life (Basel, Switzerland). 2021;11(7):692. https://doi.org/10.3390/life11070692.
Aedo-Lopez V, Gérard CL, Boughdad S, Gautron Moura B, Berthod G, Digklia A, et al. Safety and efficacy of ipilimumab plus nivolumab and sequential selective internal radiation therapy in hepatic and extrahepatic metastatic uveal melanoma. Cancers. 2022;14(5):1162. https://doi.org/10.3390/cancers14051162.
Rossi E, Cellini F, Pagliara MM, Sammarco MG, Pedone RR, Lancellotta V, et al. Hepatic radiotherapy in addition to anti-PD-1 for the treatment of metastatic uveal melanoma patients. Cancers. 2023;15(2):493. https://doi.org/10.3390/cancers15020493.
Grynberg S, Stoff R, Asher N, Shapira-Frommer R, Schachter J, Haisraely O, et al. Radiotherapy may augment response to immunotherapy in metastatic uveal melanoma patients. Ther Adv Med Oncol. 2022;14:17588359221131520. https://doi.org/10.1177/17588359221131521.
Tong TML, Burgmans MC, Speetjens FM, van Erkel AR, van der Meer RW, van Rijswijk CSP, et al. Combining melphalan percutaneous hepatic perfusion with ipilimumab plus nivolumab in advanced uveal melanoma: first safety and efficacy data from the phase Ib part of the Chopin trial. Cardiovasc Intervent Radiol. 2023;46(3):350–9. https://doi.org/10.1007/s00270-022-03338-1.
Tong TML, van der Kooij MK, Speetjens FM, van Erkel AR, van der Meer RW, Lutjeboer J, et al. Combining hepatic percutaneous perfusion with ipilimumab plus nivolumab in advanced uveal melanoma (CHOPIN): study protocol for a phase Ib/randomized phase II trial. Trials. 2022;23(1):137. https://doi.org/10.1186/s13063-022-06036-y.
Rozeman EA, Prevoo W, Meier MAJ, Sikorska K, Van TM, van de Wiel BA, et al. Phase Ib/II trial testing combined radiofrequency ablation and ipilimumab in uveal melanoma (SECIRA-UM). Melanoma Res. 2020;30(3):252–60. https://doi.org/10.1097/cmr.0000000000000653.
Karivedu V, Eldessouki I, Taftaf A, Zhu Z, Makramalla A, Karim NA. Nivolumab and ipilimumab in the treatment of metastatic uveal melanoma: a single-center experience. Case Rep Oncol Med. 2019;2019:3560640. https://doi.org/10.1155/2019/3560640.
Mariani P, Piperno-Neumann S, Servois V, Berry MG, Dorval T, Plancher C, et al. Surgical management of liver metastases from uveal melanoma: 16 years’ experience at the Institut Curie. Eur J Surg Oncol: J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2009;35(11):1192–7. https://doi.org/10.1016/j.ejso.2009.02.016.
Muraki R, Morita Y, Ida S, Kitajima R, Furuhashi S, Kiuchi R, et al. Multimodal therapy with surgery and adjuvant nivolumab for late-onset multiple liver metastases of choroidal malignant melanoma: a case report. Surg Case Rep. 2020;6(1):187. https://doi.org/10.1186/s40792-020-00948-0.
Triebel F, Jitsukawa S, Baixeras E, Roman-Roman S, Genevee C, Viegas-Pequignot E, et al. LAG-3, a novel lymphocyte activation gene closely related to CD4. J Exp Med. 1990;171(5):1393–405. https://doi.org/10.1084/jem.171.5.1393.
Maruhashi T, Okazaki IM, Sugiura D, Takahashi S, Maeda TK, Shimizu K, et al. LAG-3 inhibits the activation of CD4(+) T cells that recognize stable pMHCII through its conformation-dependent recognition of pMHCII. Nat Immunol. 2018;19(12):1415–26. https://doi.org/10.1038/s41590-018-0217-9.
Souri Z, Wierenga APA, Kroes WGM, van der Velden PA, Verdijk RM, Eikmans M, et al. LAG3 and its ligands show increased expression in high-risk uveal melanoma. Cancers. 2021;13(17):4445. https://doi.org/10.3390/cancers13174445.
Kashyap S, Singh MK, Kumar N, Jha J, Lomi N, Meel R, et al. Implications of LAG3 and CTLA4 immune checkpoints beyond PD-1/PD-L1 as a potential target in determining the prognosis of uveal melanoma patients. Br J Ophthalmol. 2023. https://doi.org/10.1136/bjo-2022-322913.
Stålhammar G, Seregard S, Grossniklaus HE. Expression of immune checkpoint receptors Indoleamine 2,3-dioxygenase and T cell Ig and ITIM domain in metastatic versus nonmetastatic choroidal melanoma. Cancer Med. 2019;8(6):2784–92. https://doi.org/10.1002/cam4.2167.
Bai KH, Zhu MJ, Zhang YY, Li XP, Chen SL, Wang DW, et al. Multi-omics analyses of tumor-associated immune-infiltrating cells with the novel immune checkpoint protein tyrosine phosphatase 1B (PTP1B) in extracellular matrix of brain-lower-grade-glioma (LGG) and uveal-melanoma (UVM). Front Immunol. 2022;13:1053856. https://doi.org/10.3389/fimmu.2022.1053856.
Bai KH, Zhang YY, Li XP, Tian XP, Pan MM, Wang DW, et al. Comprehensive analysis of tumor necrosis factor-α-inducible protein 8-like 2 (TIPE2): A potential novel pan-cancer immune checkpoint. Comput Struct Biotechnol J. 2022;20:5226–34. https://doi.org/10.1016/j.csbj.2022.09.021.
Nathan P, Hassel JC, Rutkowski P, Baurain JF, Butler MO, Schlaak M, et al. Overall survival benefit with tebentafusp in metastatic uveal melanoma. N Engl J Med. 2021;385(13):1196–206. https://doi.org/10.1056/NEJMoa2103485.
Hassel JC, Piperno-Neumann S, Rutkowski P, Baurain JF, Schlaak M, Butler MO, et al. Three-year overall survival with tebentafusp in metastatic uveal melanoma. N Engl J Med. 2023. https://doi.org/10.1056/NEJMoa2304753.
Luo S, Xie C, Lin N, Lin D, Gu D, Lin S, et al. Cost-effectiveness analysis of an orphan drug tebentafusp in patients with metastatic uveal melanoma and a call for value-based pricing. Melanoma Res. 2023;33(6):525–31. https://doi.org/10.1097/cmr.0000000000000919.
Bashari N, Safaei Lari M, Darvishi A, Daroudi R. Cost-utility analysis of Pembrolizumab compared to other alternative immunotherapy and chemotherapy treatments for patients with advanced melanoma in Iran. Expert Rev Pharmacoecon Outcomes Res. 2023. https://doi.org/10.1080/14737167.2023.2263164.
Paly VF, Hikichi Y, Baker T, Itakura E, Chandran N, Harrison J. Economic evaluation of nivolumab combined with ipilimumab in the first-line treatment of advanced melanoma in Japan. J Med Econ. 2020;23(12):1542–52. https://doi.org/10.1080/13696998.2020.1830781.
Wang J, Chmielowski B, Pellissier J, Xu R, Stevinson K, Liu FX. Cost-effectiveness of pembrolizumab versus ipilimumab in ipilimumab-naïve patients with advanced melanoma in the United States. J Manag Care Spec Pharm. 2017;23(2):184–94. https://doi.org/10.18553/jmcp.2017.23.2.184.
Kohn CG, Zeichner SB, Chen Q, Montero AJ, Goldstein DA, Flowers CR. Cost-effectiveness of immune checkpoint inhibition in BRAF wild-type advanced melanoma. J Clin Oncol: Off J Am Soc Clin Oncol. 2017;35(11):1194–202. https://doi.org/10.1200/jco.2016.69.6336.
Tawbi HA, Schadendorf D, Lipson EJ, Ascierto PA, Matamala L, Castillo Gutiérrez E, et al. Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N Engl J Med. 2022;386(1):24–34. https://doi.org/10.1056/NEJMoa2109970.
Funding
The authors declare that no funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Hongbo Yin contributed to the study conception and design. Literature retrieval, collection and analysis were performed by Jinyu Wang, Zehua Li and Hongbo Yin. The first draft of the manuscript was written by Jinyu Wang and Zehua Li, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Jinyu Wang, Zehua Li, and Hongbo Yin declare that they have no competing interests.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, J., Li, Z. & Yin, H. The Future of Checkpoint Inhibitors in Uveal Melanoma: A Narrative Review. Ophthalmol Ther 13, 1103–1123 (2024). https://doi.org/10.1007/s40123-024-00913-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00913-2