Abstract
Introduction
Macular diseases are major contributors to visual impairment and blindness worldwide. This study introduces PocDoc, a digital version of the conventional Amsler grid, aimed at enhancing the screening and monitoring of macular diseases. We conducted a comprehensive evaluation to compare the effectiveness of PocDoc against the conventional method.
Methods
Our comparative analysis involved two distinct phases. Initially, we assessed the capability of both PocDoc and the conventional method in detecting central visual field abnormalities. This phase included a cohort of 72 healthy and 155 eyes affected by various conditions such as age-related macular degeneration (AMD), uveitis, polypoidal choroidal vasculopathy (PCV), and macular telangiectasia. We primarily focused on the area of compromise and observed the correlation between the results obtained from both methods, measuring their concordance using a correlation coefficient. In the second phase, we evaluated the accuracy of both methods in diagnosing AMD. This involved a group of 127 eyes, including 70 healthy and 57 AMD-affected eyes. We determined the sensitivity, specificity, and overall accuracy of each method in diagnosing AMD.
Results
In the initial phase, both PocDoc and the conventional Amsler grid demonstrated a high correlation in detecting central visual field defects across various macular diseases (correlation coefficient > 0.9). In the second phase, focused on AMD diagnosis, PocDoc showed a sensitivity of 50%, specificity of 100%, and an overall accuracy of 78%. Comparatively, the conventional method exhibited a sensitivity of 49%, specificity of 100%, and accuracy of 77%.
Conclusion
PocDoc’s digital Amsler grid exhibits comparable effectiveness to the conventional method in both detecting visual field abnormalities across a range of macular diseases and specifically in the diagnosis of AMD. The high correlation in results, combined with the digital advantages of PocDoc, such as ease of use and potential for telemedicine applications, suggests its viability as a valuable tool in the screening and monitoring of macular diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
The study addresses the need for effective screening and monitoring tools for macular diseases, focusing on the potential benefits of digital solutions. This is particularly relevant given the prevalence and economic burden of conditions like age-related macular degeneration (AMD) and other macular diseases. |
The study hypothesized that PocDoc, a digital version of the Amsler grid, could be as or more effective than the conventional Amsler grid in detecting central visual field abnormalities and diagnosing macular diseases like AMD |
What was learned from the study? |
The study outcomes revealed that PocDoc exhibited a high correlation with the conventional Amsler grid in detecting central visual field defects across various macular diseases. Specifically, in diagnosing AMD, PocDoc showed a comparable effectiveness to the conventional method |
The findings suggest that digital tools like PocDoc can effectively complement or even enhance traditional methods in the screening and monitoring of macular diseases. The integration of digital tools in clinical practice could also pave the way for advancements in telemedicine and remote monitoring, enhancing patient access and care |
Introduction
Visual impairment (VI) is a major global health concern affecting approximately 596 million people in 2020 [1]. The main causes of VI are cataract, age-related macular degeneration (AMD), glaucoma, diabetic retinopathy, and uncorrected refractive error. The number is expected to increase with increasing life expectancy, leading to greater burden on resources in the hospitals and clinics. To address this, mobile applications such as E-health apps which contain various eye tests have been developed to allow for self-monitoring, early detection and monitoring progression [2,3,4,5,6].
Patients with certain conditions such as AMD, epiretinal membrane, and macular hole can present with central distortion of vision (metamorphopsia) and relative scotoma. Of these, AMD constitutes one of the leading causes of irreversible VI in developed countries [7]. Prevalence of dry AMD is roughly around 10–15% in the general population, and of these about 10–15% patients with high-risk AMD convert to the “wet” variant—also known as neovascular AMD or nAMD [8, 9]. The advent of newer and more potent anti-vascular endothelial growth factor (anti-VEGF) agents has dramatically improved the prognosis of nAMD and stressed the importance of early detection and therapy in such patients [10]. Moreover, even with conditions such as epiretinal membrane or macular holes, timely detection and surgical intervention when required could improve the visual outcomes significantly.
The Amsler grid is one of the most commonly used tools for the qualitative assessment of metamorphopsia and relative central scotoma, suitable for self-assessment or use in a busy clinic. It consists of equally spaced vertical and horizontal lines forming a grid. This grid, measuring 10 cm by 10 cm and divided into 0.5-cm squares, is typically held at reading distance with one eye covered. At this distance, the grid’s dimensions correspond to the central 12.5° of the visual field. Any distortions and missing areas observed on the grid can indicate the need for a closer examination of the macula by an ophthalmologist, especially in cases of new onset or recurrent diseases [11].
PocDoc—a newly developed web-based application—consists of six various stand-alone tests such as visual acuity, contrast sensitivity, Amsler grid, colour vision, visual field, and red desaturation. PocDoc is developed to address the unmet need for comprehensive out-of-hospital monitoring of eye disease progression and remote monitoring by reducing the frequency required for follow-up consultation [6]. By implementing this approach, high-risk patients can execute these tests in non-clinical settings such as their homes, potentially relieving the current strain on hospital humanpower, and improve the comprehensiveness of monitoring these conditions.
The aim of this study is to propose and validate this digital tool—PocDoc—for assessing distortion of vision and scotomas using a purpose-built Amsler grid. We hypothesize that digital Amsler grid tool gives equal or similar results to the conventional one and in addition may even be able to quantify the degree of scotoma and distortion.
Methods
Study Design and Population
This prospective, comparative study was conducted in two distinct phases. A prospective observational study was conducted in a tertiary referral hospital in Singapore in which a total of 133 participants were recruited from the medical retina, uveitis, and glaucoma clinics from September 2022 to October 2023. The inclusion criteria of the study include participants who are < 90 years old and are fit to give informed consent while the exclusion criteria include participants who are unable to do the tests in PocDoc and those who are pregnant or breastfeeding. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and was approved by Domain Specific Review Board (DSRB). Informed consent was obtained from all individual participants involved in the study.
Intervention
PocDoc, a digital adaptation of the conventional Amsler grid, was developed for use on digital platforms. The application allows users to mark visual disturbances directly on a digital grid. This tool was designed to enhance patient engagement and enable longitudinal tracking of visual field changes. The PocDoc application contains seven variations of the Amsler grid test in which only type 1 was utilized in the study (Fig. 1B). The tests were administrated using Galaxy Tab S6 Lite, model number SM-P615, serial number R52NA10RQWK. Step-by-step instructions on how to administer the tests are provided in the instruction menu as shown in Fig. 1A.
Display of the Amsler Grid in the PocDoc app. A Instruction menu on the administration of digital Amsler grid and B the seven types available in PocDoc. There are seven charts of the Amsler grid each with dimensions of 10 cm × 10 cm. Chart 1—the lines are white in a black background. There are 20 small squares in each side of the grid. Thus, each side of the small squares measures 10 cm/20 = 5 mm. Each small square cast an angle of 20°/20 = 1° field when the grid is held at 33 cm from the eye. Chart 2—four diagonal white lines are placed over the chart 1 to help fixation in an eye with a central scotoma. Chart 3—it is similar to chart 1, except the fact that there are red (in place of white) lines over a black background. Red specifically stimulates the long wavelength cones. This chart is to pick up subtle red desaturation in diseases including bitemporal hemianopia in a pituitary tumor, toxic optic neuropathy, and toxic maculopathy. Chart 4—there is no line. Over a black background, there is a central large round white dot. In other spaces, there are multiple small random white dots. This chart is used to differentiate scotoma from metamorphopsia as there is no form appreciable for distortion. Chart 5—there is a square with 21 horizontal white lines on black background 5 mm apart. A central white dot is present for fixation. It is used to determine any specific meridian of metamorphopsia specifically in patients with reading difficulties. Chart 6—this is a modification of chart 5. Of the seven charts, only this chart has black lines on white background. The central lines are closer than the chart 5, helping to evaluate fine metamorphopsia near fixation. Chart 7—this is a modification of chart 1. There is a central area with smaller squares each one subtending 0.5° field. Small scotoma or area of metamorphopsia near the fixation can be demonstrated with this chart [22]
Procedures
Participants underwent Amsler grid testing using both the PocDoc platform and a traditional Amsler grid. Initially, an auto-refraction was performed to evaluate refractive errors, and participants were advised to wear any necessary corrective eyewear to achieve their best corrected visual acuity. The testing environment was controlled, maintaining room luminance at approximately 160 lx to provide consistent lighting conditions for all tests. Although the PocDoc app could not track eye fixation, participants were instructed to consistently focus on the central target during the examination. This approach aimed to standardize the testing procedure and enhance the reliability of detecting visual distortions or scotomas through the Amsler grid.
In the conventional assessment, subjects covered one eye and fixated on a central point, reporting any distortions or scotomas. Patients were required draw along the lines that seemed distorted or curved and to draw a circular area around any blacked-out areas and areas that are blurry using a pen. The same protocol was followed using PocDoc on a digital device, allowing for direct interaction with the grid. Participants were required to undergo the test under the previously mentioned standardized conditions in which the participants were in a well-lit room with the brightness of the tablet set to the maximum. The tablet was also positioned perpendicular to the participant’s line of sight, and a standardized testing distance of approximately 30 cm was also maintained for the test. Participants who required glasses or contact lenses wore them during the administration of the tests. The participants were required to undergo the conventional test followed by PocDoc Amsler on the same visit. The results were recorded as the presence and absence of defects, including distortion, scotomas, central vision loss, and localized or minor disturbances as described in Table 2. See Supplementary Material for more detailed examples.
Data Collection and Statistical Analysis
The first phase encompassed a cross-sectional analysis comparing the digital Amsler grid (PocDoc) with the conventional Amsler grid in a mixed cohort. The second phase specifically evaluated the diagnostic accuracy for AMD. The study cohort included 227 eyes, consisting of 72 healthy eyes and 155 eyes with various macular pathologies, including AMD, uveitis, polypoidal choroidal vasculopathy (PCV), and macular telangiectasia. The primary endpoint was the presence of defects in the visual field area as identified by each method. McNemar test was used to determine if there were differences between both test [12].
Additionally, the total number of affected boxes within each patient's visual field, as well as the number of affected boxes by quadrant (superior nasal, superior temporal, inferior nasal, inferior temporal), were counted in both tests (Fig. 2). Concordance between PocDoc and the conventional grid was quantified using a Pearson correlation coefficient (r). Additionally, intra-class correlation (ICC) and Bland-Altam plots were done to evaluate the level of agreement. For the Bland-Altman plots, the y axis is the number of boxes affected as measured by the PocDoc Amsler grid test minus the number of boxes affected as measured by the conventional Amsler grid test, while the x axis represents the average number of boxes affected.
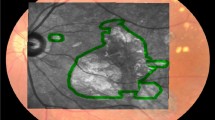
Comparative visualization of Amsler grid test results for three patients. This graphic displays the outcomes of both digital (left) and conventional (right) Amsler grid tests conducted on three different patients, each diagnosed with a distinct ocular condition: A dry age-related macular degeneration (AMD), B wet AMD, and C glaucoma
For the second—AMD diagnostic accuracy—phase, the cohort included 70 control eyes and 57 eyes diagnosed with AMD. Here, sensitivity, specificity, and diagnostic accuracy were calculated for each method. McNemar’s test was performed to compare the sensitivity of PocDoc against the traditional Amsler grid [12]. Contingency tables used for statistical analysis are available in Supplementary Material.
Results
Data were collected from 227 eyes (114 OD and 113 OS) from 133 participants (74 males and 59 females), with a mean age of 62 years, ranging from 18 to 89. The presenting complaints were mainly neovascular AMD and PCV; see Table 1. Fifty-five eyes had any type of defect, distortions being the most common (Table 2).
The Pearson correlation between the PocDoc and conventional Amsler grid for the entire grid was calculated as 0.982. Correlations for each of the four quadrants (superior nasal, superior temporal, inferior nasal, and inferior temporal) were 0.959, 0.971, 0.967, and 0.958, respectively. All were statistically significant at p < 0.001, suggesting a strong positive correlation between the results of both tests. Moreover, the ICC for the total count of compromised boxes was 0.98 (95% CI 0.974–0.984, p < 0.001), and Fig. 3 demonstrates the Bland-Altman plots assessing the agreement between both tests in the four quadrants (Fig. 3A–D) as well as the entire visual field (Fig. 3E).
Bland-Altman plots depicting variations between PocDoc Amsler grid and conventional Amsler grid results in the different quadrants of the central visual field. A Superior nasal visual field, B superior temporal visual field, C inferior nasal visual field, D inferior temporal visual field, and E the entire visual field
As seen in Fig. 3E, the total number of boxes affected in a patient’s entire visual field as measured by PocDoc Amsler grid testing would be, on average, 2.40 boxes less than for conventional Amsler grid testing for the same patient. After calculating the mean difference (bias) and the standard deviation of the differences, the limits of agreement on the Bland-Altman plot can be calculated as the mean difference ± 1.96 multiplied by the standard deviation of the differences.
The upper and lower limits from Fig. 3E suggest that for each patient, the PocDoc Amsler grid testing results would be between 29.48 boxes less and 24.67 boxes more than with conventional Amsler grid testing. In all five plots, the bias is consistently negative, which could suggest systematic bias resulting in PocDoc Amsler grid testing producing a lower number of affected boxes on average. Interestingly, the superior temporal visual field seen in Fig. 3A has the highest lower limit of agreement (– 8.818) and lowest upper limits of agreement (7.915).
Using a sample size of 127 eyes (70 healthy and 57 patients with AMD), a sub-analysis was conducted to calculate the accuracy metrics of both tests. In Table 3, the sensitivity and specificity for the conventional Amsler grid test were found to be 49.1% and 100%, respectively, while they were 50.9% and 100% for PocDoc Amsler grid test. No statistical differences were found between the sensitivities of the two tests (χ2 = 1, p value = 0.31). The overall accuracy was 77.2% for conventional Amsler grid test and 78.0% for PocDoc Amsler grid test. This demonstrated that the PocDoc Amsler grid test had slightly higher sensitivity, accuracy, and negative predictive value than the conventional Amsler grid test.
Discussion
Amsler grid is a useful screening tool for patients at high risk of developing nAMD [13], progression of epiretinal membrane [14], or development of full thickness macular hole in those with stage 1 hole or contralateral eyes of FTMH [15]. PocDoc, a digital Amsler grid, aligns with the emerging trend of utilizing digital platforms for AMD monitoring. Several digital Amsler grid applications are currently available commercially, such as the Foresee Home monitor [16], Alley (developed by Oculocare), and myVisionTrack (by Vital Art and Science) [17].
These applications have shown promising results in enhancing AMD monitoring, although they are not without limitations. For instance, the Home Monitoring of the Eye study highlighted the ForeseeHome monitor's effectiveness, noting a smaller decline in visual acuity from baseline to choroidal neovascularization (CNV) detection [18]. Similarly, an initial assessment of the Alley smartphone application in clinical practice demonstrated its efficacy in discriminating between different ocular conditions. These findings underscore the potential benefits of digital Amsler grid applications in early detection and continuous monitoring of AMD progression [17].
Consistent with the findings of previous studies by Faes et al. [19] and Bjerager et al. [17], our study reaffirms the high specificity of the Amsler grid, in both its conventional and digital forms (PocDoc), for detection of age-related macular degeneration (AMD). Faes et al. [19] reported a specificity of 0.97, while Bjerager et al. [17] found it to be 99% compared with healthy controls. Our study aligns with these findings, demonstrating a specificity of 100% for both PocDoc and the conventional Amsler grid. This high level of specificity is crucial in clinical practice as it indicates the strong ability of the Amsler grid to correctly identify individuals who do not have AMD, thereby reducing the likelihood of false-positive diagnoses.
Our study, however, presents a lower sensitivity (50% for PocDoc and 49% for the conventional grid) compared to the previous studies. Faes et al. [19] found a pooled sensitivity of 0.78, and Bjerager et al. [17] reported sensitivities of 67% and 71% with different control groups. However, the sensitivity of Amsler grid is highly variable and has been reported as low as 34% in some studies [20]. This variation in sensitivity might be attributed to several factors, including differences in study populations, specific types of AMD evaluated, and methodologies employed in visual field testing. The reasons behind this variation in sensitivity are multifaceted. Moreover, the lower sensitivity observed in our study reinforces the ongoing debate about the value of the Amsler grid in AMD screening and monitoring patients with AMD [17]. It suggests that the Amsler grid, while useful, may have inherent limitations in detecting all cases of AMD, especially in its early stages or less severe forms. This finding is critical as it aligns with the concerns raised by other authors regarding the Amsler grid’s effectiveness, particularly for early detection and screening in clinical settings.
The Amsler grid is valuable for ruling out AMD, relying solely on this method may lead to missed diagnoses, especially in cases where the disease is not advanced. Therefore, it is imperative that the Amsler grid be used in conjunction with other diagnostic tools and assessments to ensure a more comprehensive evaluation of AMD [21]. Our introduction of the digital Amsler grid, PocDoc, contributes to this discourse by offering a modernized tool that maintains the high specificity of the conventional method while addressing some of the limitations in traditional screening approaches. The digital format of PocDoc facilitates ease of use, enhances patient engagement, and provides opportunities for remote monitoring and data collection. However, as our findings indicate, further research and development are needed to improve its sensitivity and overall diagnostic capabilities, particularly in the early detection of AMD.
PocDoc adds another dimension to the evolving digital landscape of telemedicine. The correlation in specificity and sensitivity observed between PocDoc and the conventional test demonstrates that these tools can be used interchangeably. However, while they offer significant advantages in terms of patient engagement and remote monitoring capabilities, the question of optimizing sensitivity remains a common challenge.
It is essential to acknowledge the limitations of our study. First, technological limitations inherent in digital applications, such as screen resolution variability and user interface design, might influence the test results and user experience with PocDoc. Second, the effectiveness of PocDoc heavily relies on patient compliance, a common challenge observed with home monitoring applications. Inaccuracies in self-reporting and variations in the use of the digital tool could impact the reliability of the findings. This issue could be mitigated by integrating the use of PocDoc Amsler into regular check-ups conducted by trained optometrists and ophthalmic technicians. Such an approach would not only ensure more accurate assessments but also reduce the need for frequent doctor visits, thereby enhancing patient convenience and healthcare efficiency. Finally, although it is not a limitation in itself of the study, a critical consideration is in the lower sensitivity observed with both PocDoc and the conventional method, raising concerns about their ability to detect early-stage or less severe forms of AMD. This limitation is crucial as it highlights the potential challenges in using the Amsler grid for early detection of AMD.
Despite these limitations, it is noteworthy that PocDoc Amsler has demonstrated considerable agreement with the conventional paper Amsler grid. The added advantage of digitalization, including the ease of recording and comparing test results over time, offers a significant benefit in monitoring disease progression. This digital approach not only aids in maintaining comprehensive patient records but also facilitates early detection of any new changes or advancements in the condition, thereby contributing positively to patient management in AMD.
Conclusion
In conclusion, the development of digital Amsler grids such as PocDoc represents an advancement in AMD and macular disease screening and monitoring. While these tools show high specificity, efforts to improve their sensitivity are crucial. The integration of these digital solutions into a comprehensive diagnostic and monitoring strategy could significantly enhance patient care in ophthalmology.
Data Availability
The dataset used and/or analyzed during the current study is available from the corresponding author on reasonable request.
References
Burton MJ, Ramke J, Marques AP, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489–551. https://doi.org/10.1016/S2214-109X(20)30488-5.
Suo L, Ke X, Zhang D, et al. Use of mobile apps for visual acuity assessment: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2022;10(2): e26275. https://doi.org/10.2196/26275.
Maramba I, Chatterjee A, Newman C. Methods of usability testing in the development of eHealth applications: a scoping review. Int J Med Inform. 2019;126:95–104. https://doi.org/10.1016/j.ijmedinf.2019.03.018.
Zvornicanin E, Zvornicanin J, Hadziefendic B. The use of smart phones in ophthalmology. Acta Inform Med. 2014;22(3):206. https://doi.org/10.5455/aim.2014.22.206-209.
Rodin A, Shachak A, Miller A, et al. Mobile apps for eye care in canada: an analysis of the iTunes store. JMIR Mhealth Uhealth. 2017;5(6): e84. https://doi.org/10.2196/mhealth.7055.
Sah S, Liu R, Lai H, et al. Improving access to eye care in rural communities: PocDoc’s web-based visual acuity screening tool. Telemed J E Health. 2023. https://doi.org/10.1089/tmj.2023.0234.
Klein R, Klein BEK, Jensen SC, et al. Age-related maculopathy in a multiracial United States population. Ophthalmology. 1999;106(6):1056–65. https://doi.org/10.1016/S0161-6420(99)90255-5.
Colijn JM, Buitendijk GHS, Prokofyeva E, et al. Prevalence of age-related macular degeneration in Europe. Ophthalmology. 2017;124(12):1753–63. https://doi.org/10.1016/j.ophtha.2017.05.035.
Sunness JS. The natural history of geographic atrophy, the advanced atrophic form of age-related macular degeneration. Mol Vis. 1999;5:25.
Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–31. https://doi.org/10.1056/NEJMoa054481.
Ayhan I, Doyle E, Zanker J. Measuring image distortions arising from age-related macular degeneration: an iterative Amsler grid (IAG). MedComm. 2022;3(1): e107. https://doi.org/10.1002/mco2.107.
Zhou X, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine. Wiley series in probability and statistics. 1st ed. Hoboken: Wiley; 2011. https://doi.org/10.1002/9780470906514.
Augustin AJ, Offermann I, Lutz J, et al. Comparison of the original Amsler grid with the modified Amsler grid: result for patients with age-related macular degeneration. Retina. 2005;25(4):443–5. https://doi.org/10.1097/00006982-200506000-00008.
Arndt C, Rebollo O, Séguinet S, et al. Quantification of metamorphopsia in patients with epiretinal membranes before and after surgery. Graefes Arch Clin Exp Ophthalmol. 2007;245(8):1123–9. https://doi.org/10.1007/s00417-006-0505-1.
Sakaguchi H, Ohji M, Kubota A, et al. Amsler grid examination and optical coherence tomography of a macular hole caused by accidental Nd:YAG laser injury. Am J Ophthalmol. 2000;130(3):355–6. https://doi.org/10.1016/S0002-9394(00)00547-X.
Chaikitmongkol V. Home monitoring for age-related macular degeneration. In: Chhablani J, editor. Choroidal neovascularization. Singapore: Springer; 2020. p. 363–73. https://doi.org/10.1007/978-981-15-2213-0_26.
Bjerager J, Schneider M, Potapenko I, et al. Diagnostic accuracy of the Amsler grid test for detecting neovascular age-related macular degeneration: a systematic review and meta-analysis. JAMA Ophthalmol. 2023;141(4):315. https://doi.org/10.1001/jamaophthalmol.2022.6396.
Chew EY, Clemons TE, Bressler SB, et al. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the eye (HOME) study. Ophthalmology. 2014;121(2):535–44. https://doi.org/10.1016/j.ophtha.2013.10.027.
Faes L, Bodmer NS, Bachmann LM, et al. Diagnostic accuracy of the Amsler grid and the preferential hyperacuity perimetry in the screening of patients with age-related macular degeneration: systematic review and meta-analysis. Eye. 2014;28(7):788–96. https://doi.org/10.1038/eye.2014.104.
Loewenstein A, Malach R, Goldstein M, et al. Replacing the Amsler grid. Ophthalmology. 2003;110(5):966–70. https://doi.org/10.1016/S0161-6420(03)00074-5.
Apte RS. Age-related macular degeneration. N Engl J Med. 2021;385(6):539–47. https://doi.org/10.1056/NEJMcp2102061. (Solomon CG. ed).
Tripathy K, Salini B. Amsler Grid. [Updated 2023 Aug 25]. 2024. https://www.ncbi.nlm.nih.gov/books/NBK538141/.
Acknowledgements
We thank the participants of the study and the Ng Teng Fong Healthcare Innovation Programme for their financial support.
Medical Writing/Editorial Assistance.
No medical writing or editorial assistance was employed in the preparation of this manuscript. The authors utilized ChatGPT 4.0 for spelling and grammar checks of certain sentences. However, all conceptual and intellectual contributions to this work were generated solely by the human authors.
Funding
The study was funded by NTF HIP grant (Grant Number: NTF_DEC2019_I_C1_C_02). No funding or sponsorship was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
Joewee Boon, William Rojas-Carabali, Yusra Asad, Jonathan Lim Tzien Yih, Rajesh Rajagopalan, Rupesh Agrawal have nothing to disclose.
Ethical Approval
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Institutional review board (IRB) approval was obtained from the National Healthcare Group Domain Specific Review Board (NHG-DSRB), reference number 2020/01182. Informed consent was obtained from all individual participants included in the study. All participants consented to the use of data for research and publication purposes.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Boon, J., Rojas-Carabali, W., Asad, Y. et al. Evaluation of a Digital Amsler Grid (PocDoc) for Macular Disease Screening: A Comparative Analysis with the Conventional Method. Ophthalmol Ther 13, 1289–1301 (2024). https://doi.org/10.1007/s40123-024-00910-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00910-5