Abstract
Introduction
The study aimed to evaluate comparability in terms of efficacy, safety and immunogenicity of Sun’s ranibizumab biosimilar with reference ranibizumab in patients with neovascular age-related macular degeneration (nAMD).
Methods
This prospective, randomised, double-blind, two-group, parallel-arm, multicentre, phase 3 comparative study included patients with nAMD ≥ 50 years, randomised (in a 2:1 ratio) in a double-blind manner to receive 0.5 mg (0.05 mL) intravitreal injection of either Sun’s ranibizumab or reference ranibizumab in the study eye every 4 weeks until week 16 (total of four doses).
Results
Primary endpoint results demonstrated equivalence in the proportion of patients who lost fewer than 15 letters from baseline best-corrected visual acuity (BCVA) to the end of week 16 (99% of patients in Sun’s ranibizumab and 100% in reference ranibizumab; p > 0.9999), with the proportional difference (90% confidence interval) at −1% (−2.51, +0.61) lying within a pre-specified equivalence margin. Visual acuity improved by 15 or more letters in 43% of Sun’s ranibizumab group and 37% of the reference ranibizumab group (p = 0.4267). The mean increase in BCVA was 15.7 letters in Sun’s ranibizumab group and 14.6 letters in the reference ranibizumab group (p < 0.001 within both groups and p = 0.5275 between groups). The mean change in central macular thickness was comparable between groups (p = 0.7946). Anti-ranibizumab antibodies were found in one patient of the reference ranibizumab group, while neutralising antibodies were not found in any patients. Both products were well tolerated.
Conclusion
Sun’s ranibizumab biosimilar is found to be therapeutically equivalent to reference ranibizumab in patients with nAMD. There were no additional safety or immunogenicity concerns.
Trial Registration
CTRI/2020/09/027629, registered on 07 September 2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Ranibizumab, a recombinant, humanised, monoclonal antibody fragment, is an approved drug for treatment of neovascular age-related macular degeneration (nAMD). Lack of insurance coverage for intravitreal injections and catastrophic out-of-pocket expenditure in India leads to a major issue of affordability and accessibility of such treatments. |
The Vitreo Retina Society of India survey on biosimilars observed an increase in the use of ranibizumab biosimilar by retina physicians in India, with over 100,000 injections used up to 2020. |
Increasing the affordability and accessibility of ranibizumab while maintaining the utmost quality and safety is an important public health need. Therefore, this double-blind, comparative, phase 3 clinical trial aimed to assess the efficacy, safety and immunogenicity of Sun’s ranibizumab relative to the original biological product in Indian patients with nAMD. |
What was the hypothesis of the study? |
To establish equivalence with a 5% significance level and 80% in the primary endpoint, i.e. no significant difference in the proportion of patients who lost fewer than 15 letters (approximately three lines) from baseline best-corrected visual acuity to the end of week 16 between Sun’s ranibizumab and reference ranibizumab, and the 90% confidence interval of the proportional difference fell within the pre-specified equivalence margin of 15%. |
What was learned from the study? |
Sun’s ranibizumab biosimilar is therapeutically equivalent to reference ranibizumab based on primary endpoint results. Overall, this study showed safety and efficacy profiles similar to those of the reference (innovator) ranibizumab. Sun’s ranibizumab was well tolerated, with no new safety or immunogenicity concerns. |
Introduction
Age-related macular degeneration (AMD) is a neurodegenerative retinal disease which is progressive in nature, leading to vision impairment, and is a major cause of irreversible blindness in patients aged ≥ 50 years in the developed world [1, 2]. Neovascular AMD (nAMD), also known as wet (exudative) AMD, is a process of abnormal growth of new vessels arising from choroidal vasculature to the neurosensory retina through Bruch's membrane. This choroidal neovascularisation (CNV) differentiates wet AMD from early or dry AMD [3, 4].
In India, the prevalence of AMD ranges from 1.4 to 3.1%, with the most common demographic factor affecting the prevalence of AMD being advanced age (> 65 years) [5]. The global prevalence of any AMD within an age range of 45 to 85 years was 8.7% [6]. Approximately 10–15% of patients with AMD eventually develop nAMD [3], of which 80% develop severe vision loss [7].
There are three types of CNV based on its appearance on fluorescein angiography: type 1 (occult), when the neovascularisation is located below the retinal pigment epithelium and demonstrates occult leakage; type 2 (classic), where the abnormal growth of neovascular vessels penetrates the retinal pigment epithelium and grows in the subretinal space; and type 3 (retinal angiomatous proliferation), where neovascularisation develops within the neurosensory retina and progresses posteriorly into the subretinal space [4].
Although nAMD is a multifactorial disease, of these factors, vascular endothelial growth factor (VEGF) drives the development of CNV by promoting angiogenesis and vascular permeability [8, 9]. Therefore, VEGF is the principal target for treatment of nAMD, and anti-VEGF agents such as pegaptanib sodium, ranibizumab, aflibercept, brolucizumab, faricimab and conbercept are approved for treatment for nAMD [10, 11], while bevacizumab is used as an off-label treatment [12, 13].
Ranibizumab, a recombinant, humanised, monoclonal antibody fragment, acts by binding and neutralising all active forms of VEGF, leading to the inhibition of the CNV process in nAMD [14]. It has been approved by the United States Food and Drug Administration since 2006 and the European Medicines Agency since 2007 for the treatment of nAMD [15, 16].
In developing countries, lack of insurance coverage for intravitreal injections and burden of out-of-pocket expenditure becomes a major barrier to the accessibility of such treatments. In India, affordability and accessibility of ranibizumab are still a major issue despite efforts through differential pricing to make ranibizumab (Accentrix®, Novartis India Ltd, Mumbai, India) significantly cheaper than in the developed world. The off-label use of intravitreal bevacizumab (Avastin; Genentech, South San Francisco, CA, USA and Roche, Basel, Switzerland) is much cheaper in India, but with a major risk of endophthalmitis, as evidenced by a recent outbreak in India due to the use of counterfeit vials [17].
The purpose of developing biosimilar drugs is to improve the accessibility of such treatments at low cost without compromising the treatment quality [18]. The World Health Organization has defined biosimilar drugs as biotechnological products with comparable quality to approved reference products supported by clinical and nonclinical evaluation with an approved reference product [19]. A few prospective and retrospective clinical trials have established the efficacy, safety and immunogenicity of biosimilar ranibizumab for the treatment of several macular disorders including nAMD, diabetic macular edema, retinal vein occlusion and myopic CNV. At least two biosimilars of ranibizumab are approved in India, which has substantially reduced the cost of ranibizumab and improved access to these treatments [20, 21].
The Vitreo-Retina Society of India survey on biosimilars revealed increased use of ranibizumab biosimilars by retina physicians in India, with over 100,000 injections used up to 2020 [22]. In order to further increase the affordability and accessibility of ranibizumab while maintaining the utmost quality and safety, a prospective comparative trial of biosimilar ranibizumab with innovator ranibizumab is an important public health need.
Sun Pharmaceutical Industries Limited, Mumbai, India, has developed a ranibizumab biosimilar product, hereinafter referred to as Sun’s ranibizumab, demonstrating similarity to the original biological product (Accentrix®) in extensive analytical and nonclinical analyses, and has conducted a double-blind, comparative, phase 3 clinical trial evaluating the efficacy, safety and immunogenicity of Sun’s ranibizumab in comparison with the original biological product in patients with nAMD [23]. Sun’s ranibizumab was approved by the Central Drugs Standard Control Organisation (CDSCO) on 24 March 2023 [24] for the treatment of nAMD.
Methods
Study Design
This prospective, randomised, double-blind, two-group, parallel-arm, multicentre, phase 3 comparative study was designed to evaluate the efficacy, safety and immunogenicity of Sun’s ranibizumab compared to reference ranibizumab (Accentrix®) in patients with nAMD (Clinical Trial Registry—India; CTRI number: CTRI/2020/09/027629). The first patient was enrolled on 29 October 2020 and the last patient visit was on 29 October 2021.
The study was conducted at 19 centres distributed geographically across India. The study protocol was approved by the registered institutional ethics committee (IEC) of the respective study sites and CDSCO, New Drugs and Clinical Trial Rules 2019. The study was conducted in accordance with the Declaration of Helsinki, the International Council for Harmonisation–Good Clinical Practice guidelines and relevant regulatory guidelines. The list of study sites and their respective IEC is provided in the Supplementary Material. All patients provided written informed consent before participation in the study.
Patient Selection
Eligible patients were of either gender aged ≥ 50 years, having active primary or recurrent subfoveal lesions with classic or occult CNV secondary to AMD which were confirmed based on fluorescein angiography at screening. The best-corrected visual acuity (BCVA), using the Early Treatment of Diabetic Retinopathy Study chart was 20/40 to 20/320 (Snellen equivalent) in the study eye before pupil dilation. If both eyes were eligible for inclusion, the eye with the better visual acuity was selected for treatment unless, based on medical reasons, the investigator deemed the other eye to be more appropriate for treatment.
Patients were excluded if they had received prior treatment with verteporfin, external-beam radiation therapy, transpupillary thermotherapy, intravitreal drug delivery (steroids or device implantation), anti-VEGF drugs, subfoveal laser photocoagulation, vitrectomy surgery, submacular surgery or other therapy/surgical intervention for AMD in the study eye. Ocular conditions meeting exclusion criteria included subfoveal fibrosis or atrophy, subretinal haemorrhage > 50% total lesion area involving the centre of the fovea, retinal pigment epithelial tear involving the macula, diabetic retinopathy and uncontrolled glaucoma (intraocular pressure ≥ 30 mmHg despite treatment) in the study eye. Patients with concurrent ocular conditions in either eye, concurrent systemic conditions, known hypersensitivity to ranibizumab or any of the components of study medication, uncontrolled hypertension (≥ 160/100 mmHg) or other medical/surgical condition interfering with participation in the study were likewise excluded.
Randomisation and Blinding
Patients were randomised (at a 2:1 ratio) in a double-blind manner to receive 0.5 mg (0.05 mL) intravitreal injection of either Sun’s ranibizumab or reference ranibizumab in the study eye every 4 weeks until week 16 (total of four doses). The randomisation schedule was generated centre-wise by the sponsor using statistical analysis system (SAS) version 9.4 software before the start of the study. A random permuted block size of 3 was considered for randomising patients in a 2:1 ratio between the two groups. Patients, investigators and the sponsor’s study team were blinded throughout the study regarding the assigned treatment.
Efficacy Assessment
The primary efficacy endpoint was the proportion of patients who lost fewer than 15 letters (approximately three lines) from baseline BCVA to the end of week 16. Visual acuity was assessed at the site using the Early Treatment of Diabetic Retinopathy study chart at a starting distance of 4 m, with repetition at 1 m as necessary.
Secondary efficacy endpoints were the proportion of patients who gained ≥ 15 letters from baseline BCVA to the end of week 16, mean change in BCVA from baseline to the end of week 16 and mean change in central macular thickness (CMT) as assessed by optical coherence tomography (OCT) from baseline to the end of week 16.
Safety Assessment
The safety endpoint was the proportion of patients with adverse events (AEs, coded according to the Medical Dictionary for Regulatory Activities [MedDRA] version 23.0) including any significant abnormality observed during ophthalmic and physical examination, laboratory parameters, vital signs, electrocardiogram and any hypersensitivity reactions reported throughout the study.
The OCT examinations were performed on the day of screening, baseline visit (day 1), week 4, week 8, week 12 and week 16. Slit-lamp examination, indirect ophthalmoscopy examination and intraocular pressure measurements were performed at all visits during the study.
Immunogenicity Assessment
Immunogenicity was evaluated by assessing the presence of serum anti-ranibizumab antibodies and neutralising anti-ranibizumab antibody (NAb) in all patients at baseline (pre-dose day 1), week 8 and week 16. A total of three samples (baseline [pre-dose day 1], week 8 and week 16), each of 6 mL, were collected from each patient.
Statistical Analysis
Sample Size and Equivalence Margin
The symmetric equivalence margin was considered according to the method of preserving 50% of the effect from the estimated active control in placebo-controlled clinical trials. Based on the predefined equivalence margin at ±15% (in agreement with regulatory authority), 2:1 randomisation ratio and assumed 15% attrition rate, approximately 160 patients were considered sufficient to establish equivalence for the primary endpoint to achieve a 5% significance level and 80% power.
The data for demographic and baseline characteristics were summarised by treatment group using descriptive statistics. Continuous data were presented as number of observations (n), mean, standard deviation (SD), median, minimum and maximum. Categorical variables (e.g. gender) were summarised using counts (%). For efficacy analysis, data sets including all randomised patients who were administered at least one dose of the assigned study product, returned for at least one post-baseline evaluation visit, and without major protocol deviation were considered.
Primary Efficacy Analysis
The proportion of patients who lost fewer than 15 letters (approximately three lines) from baseline BCVA to the end of week 16 between Sun’s ranibizumab and reference ranibizumab groups was summarised by count (%) and analysed by test for proportion (chi-square test).
To test equivalence, the two one-sided test procedure was used, equivalence was established at an alpha (α) significance level if a (1 − 2α) × 100% confidence interval for the difference in efficacy (new − current) was contained within the interval (−δ, δ). The objective of establishing equivalence was to demonstrate that the proportion of patients who lost fewer than 15 letters (approximately three lines) from baseline BCVA to the end of week 16 was not significantly different between the Sun ranibizumab and reference ranibizumab, and the 90% confidence interval (CI) of the difference was within the pre-specified equivalence margin of 15%. The 90% CI of the proportional difference included zero.
Secondary Efficacy Analysis
The mean change in BCVA and central macular thickness assessed by OCT in the study eye from baseline to end of week 16 were summarised with n, mean, SD, median, minimum and maximum. A two-sample t-test was used to assess the significant difference between the two groups. A paired t-test was used to evaluate the significant difference from baseline to week 16 in mean BCVA within each treatment group. The proportion of patients who gained ≥ 15 letters (approximately three lines) from baseline BCVA to the end of week 16 were summarised with count and percentage and analysed by a test for proportion (chi-square) to assess significant differences between treatment groups. All statistical analysis was performed using SAS version 9.4 software.
Results
Patient Disposition
Overall, 187 patients were screened, of which 161 patients were randomised to receive either Sun’s ranibizumab (n = 107) or reference ranibizumab (n = 54) from 19 geographically distributed centers across India. A total of 151 (93.8%) patients completed the study (Fig. 1).
Patient Demographics and Baseline Characteristics
Baseline demographic and disease characteristics were similar between the two groups in terms of gender distribution, age, height, weight, body mass index, BCVA (letters), intraocular pressure, type of lesion and type of CNV. The mean (±SD) age was 66.32 ± 9.64 years, with ~60% male patients. The overall mean (±SD) duration of nAMD was 95.18 ± 340.2 days. The mean (±SD) BCVA at baseline was 43.66 ± 12.35 letters, and ~50% had predominantly classic lesions. Around 84% of patients had an active primary lesion of nAMD (Table 1).
Primary Efficacy Endpoint
At week 16, 99% of the patients in Sun’s ranibizumab group and 100% of patients in the reference ranibizumab group had lost fewer than 15 letters from baseline BCVA. The proportional difference (90% CI) between the groups was −1% (−2.51, +0.61). The 90% CI of the proportional difference lay within the pre-specified equivalence margin of 15%, and the interval included zero. Further, the proportional difference between the Sun ranibizumab and reference ranibizumab groups was not significantly different (p > 0.9999) (Fig. 2).
Secondary Efficacy Endpoints
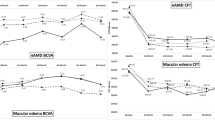
The mean (±SD) change in BCVA from baseline to the end of week 16 was −15.7 (±10.45) and −14.6 (±8.83) letters in Sun’s ranibizumab and reference ranibizumab groups, respectively (p <0.001 within both groups), with no significant difference between groups (p = 0.5275) (Fig. 3). The mean (±SD) change in CMT assessed by OCT from baseline to the end of week 16 was 100.9 (±143.10) μm and 107.3 (±141.63) μm in the Sun ranibizumab and reference ranibizumab groups, respectively, and there was no significant difference between groups (p = 0.7946) (Fig. 4). The proportion of patients gaining ≥ 15 letters was 43% and 37% in the Sun ranibizumab and reference ranibizumab groups, respectively, with no significant difference between groups (p = 0.4267) (Fig. 5).
Line chart for mean change in best-corrected visual acuity from baseline in the study eye at week 16. [1] Sun’s ranibizumab (N = 102) and reference ranibizumab (N = 53) at week 8, Sun’s ranibizumab (N = 102) and reference ranibizumab (N = 52) at week 12, and Sun’s ranibizumab (N = 100) and reference ranibizumab (N = 51) at week 16
Line chart for central macular thickness assessed by OCT from baseline in the study eye at the end of week 16. [1] Sun’s ranibizumab (N = 107) and reference ranibizumab (N = 54) at baseline and Sun’s ranibizumab (N = 100) and reference ranibizumab (N = 51) at week 16. CMT central macular thickness, OCT optical coherence tomography.
Safety
Of 14 AEs (16%) reported in the study, ocular AEs included eye irritation and retinal haemorrhage (one patient each) in the reference ranibizumab group and conjunctivitis and viral conjunctivitis (one patient each) in Sun’s ranibizumab group. The most common non-ocular AEs were hypertension (1.9% incidence) in Sun’s ranibizumab group and dyspepsia (3.7% incidence) in the reference ranibizumab group. Three serious adverse events (SAEs, dyspepsia [severe in intensity], urinary tract infection [severe in intensity] and hyponatraemia [life-threatening]) were reported in one patient in the reference ranibizumab group, and all three SAEs were resolved and were not related to reference ranibizumab. The current study had only one AE (hyperglycaemia) in Sun’s ranibizumab group, which was probably/likely related according to the investigator. None of the patients met the requirements for treatment discontinuation or dose withholding criteria due to any AE. No new ocular or non-ocular safety concerns were identified during the study (Table 2).
Immunogenicity
Only one patient was found to have anti-ranibizumab antibodies in the reference ranibizumab group at day 1 (mean relative light units = 79.0, signal-to-noise [S/N] ratio = 0.97, % inhibition = 27.5) and day 56 (week 8) (mean relative light units = 82.5, S/N ratio = 1.01, % inhibition = 26.7), with no substantial difference in titres at either time point. Assay for NAb was negative for this patient at both time points.
Discussion
Vascular endothelial growth factor is a pro-angiogenic factor known to mediate the pathogenesis of nAMD. Therefore, treatment strategies have seen a paradigm shift from laser coagulation and photodynamic therapy to the use of anti-VEGF agents to target the pathological process directly. Although anti-VEGF agents such as ranibizumab have become the accepted standard of care, their substantial costs impose a significant cost burden on patients and the health care system [25]. A study by Kelkar et al. reported 51.5% loss to follow-up and treatment non-compliance among patients with nAMD and diabetic macular edema treated with intravitreal anti-VEGF agents [26].
Biosimilar ranibizumab is about 30–40% less expensive than the innovator ranibizumab in India. Another anti-VEGF monoclonal antibody, bevacizumab, an anti-angiogenic in treating solid tumours, is used as an effective off-label treatment at low cost for nAMD [27]. However, multi-dose vial availability of bevacizumab is leading to problems in aliquoting and storage [18], and its association with cluster endophthalmitis has been a constant issue [28]. Also, a recent online survey of members of the Vitreo-Retinal Society of India reported an increase in the use of ranibizumab biosimilars from 41% in 2018 to 56% in 2020 (p = 0.2) and a simultaneous significant decline in the use of bevacizumab biosimilars from 9% in 2018 to 2% in 2020 (p = 0.04), indicating a progressive trend favoring ranibizumab biosimilar over bevacizumab biosimilar [22]. The cost-effectiveness of biosimilar ranibizumab and its minimal chance of contamination due to the availability in a single-dose vial suggests a gradual shift from the off-label use of bevacizumab to biosimilar ranibizumab in India [22].
The primary endpoint results for this study demonstrated equivalent proportions of patients who lost fewer than 15 letters from baseline BCVA to the end of week 16 (99% of patients in Sun’s ranibizumab and 100% in reference ranibizumab groups), with the proportional difference lying within the pre-specified equivalence margin.
This result is similar to innovator ranibizumab studies (96.4% and 94.6% of patients lost fewer than 15 letters at month 12 in the MARINA and ANCHOR studies [29, 30], respectively) and ranibizumab biosimilar studies in India (Reliance study [98.11% and 100% in ranibizumab biosimilar and reference ranibizumab groups, respectively, at week 16] and the ASSET study [98.4% and 97.60% in ranibizumab biosimilar at week 12 and week 24, respectively]) [21, 22].
The present biosimilar study with a short-term treatment duration of 16 weeks showed a significant improvement in BCVA in both the Sun ranibizumab and reference ranibizumab groups at week 16. This improvement in BCVA was higher than that in the MARINA study (increase of 7.2 letters) and ANCHOR study (increase of 10.7 letters) and was similar to the Reliance study (increase of 10.47 and 12.58 letters in test and reference groups, respectively, at week 16, and 12.11 and 15.66 letters in test and reference groups, respectively, at week 24). The likely explanation for these higher letter gains is the younger population (~66 years), lower baseline BCVA (~43 letters) and no prior medication history (due to exclusion criteria).
The proportion of patients who showed improvement in BCVA by gaining ≥ 15 letters at week 12 (43% in Sun’s ranibizumab and 37% in reference ranibizumab group) in this study was also similar to the MARINA and ANCHOR studies (33.8% and 40.3% of patients, respectively, at month 12), the ASSET study (31.20% at month 24) and the Reliance study (25.47% vs 30.19% [at 16 weeks] and 32.08% vs 43.30% [at 24 weeks] in test and reference groups, respectively]).
The mean change in CMT assessed by OCT at week 16 was 100.9 μm in Sun’s ranibizumab and 107.3 μm in the reference ranibizumab group, which is in line with that observed in the ASSET study (125 μm at 6 months) and the Reliance study (78.22 μm and 89.33 μm at 16 and 24 weeks, respectively).
Sun’s ranibizumab was well tolerated and safe in patients with nAMD. Common ocular SAEs such as uveitis, presumed endophthalmitis, vitreous haemorrhage and severe ocular inflammation which were reported in the MARINA, ANCHOR, and SUSTAIN studies were not reported in our study [29,30,31].
Common non-ocular AEs associated with systemic VEGF inhibition were arterial thromboembolic events, hypertension, proteinuria and non-ocular haemorrhage [9, 13]. Hypertension and dyspepsia were also commonly reported. The reported adverse and serious adverse events were mostly attributed to medical history and concomitant medication. There were no additional safety or immunogenicity concerns in this study.
This study had some limitations. The efficacy and safety results of Sun’s ranibizumab were compared to reference ranibizumab for a relatively short period of 16 weeks; long-term data are required. Further, the study was not designed with the objective of establishing interchangeability. The pharmacokinetics of Sun’s ranibizumab have not been evaluated; however, the relevance of pharmacokinetics is limited considering the intravitreal administration, with limited absorption into the systemic circulation.
Conclusion
Sun’s ranibizumab biosimilar is therapeutically equivalent to reference ranibizumab based on primary endpoint results. Overall, this study showed safety and efficacy profiles similar to those of the reference (innovator) ranibizumab. Sun’s ranibizumab was well tolerated, with no new safety or immunogenicity concerns.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Marchesi N, Fahmideh F, Boschi F, Pascale A, Barbieri A. Ocular neurodegenerative diseases: interconnection between retina and cortical areas. Cells. 2021;10(9):2394.
Jiménez-Gómez Y, Alba-Molina D, Blanco-Blanco M, Pérez-Fajardo L, Reyes-Ortega F, Ortega-Llamas L, et al. Novel treatments for age-related macular degeneration: a review of clinical advances in sustained drug delivery systems. Pharmaceutics. 2022;14(7):1473.
Feldman BH, Shah VA, Leo KA, Tripathy K, Tsui JC, Elshatory YM, American Academy of Ophthalmology. Age-related macular degeneration. 2023. https://eyewiki.aao.org/Age-Related_Macular_Degeneration. Accessed 27 Mar 2023.
Leo AK, Tripathy K, Dumar AT, Do DV, Carlo Td, Bhagat N, et al. Choroidal Neovascularization: OCT Angiography Findings. Age-related macular degeneration. 2023. https://eyewiki.aao.org/Choroidal_Neovascularization:_OCT_Angiography_Findings#. Accessed 27 Mar 2023.
Likhar N, Mothe RK, Kanukula R, Shah C, Dang A. The prevalence of age-related Macular degeneration in Indian Population: a systematic review. Value Health. 2015;18(3):A180.
Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–16.
Woo SJ, Cho GE, Cho JH. Short-term efficacy and safety of ranibizumab for neovascular age-related macular degeneration in the real world: a post-marketing surveillance study. Korean J Ophthalmol. 2019;33(2):150–66.
Sharma K, Sharma NK, Singh R, Anand A. Exploring the role of VEGF in Indian age related macular degeneration. Ann Neurosci. 2015;22(4):232–7.
Grisanti S, Zhu Q, Tatar O, Lueke J, Lueke M, Tura A, et al. Differential expression of vascular endothelial growth factor-a isoforms in neovascular age-related macular degeneration. Retina. 2015;35(4):764–72.
Kenneth TE, Kertes PJ. Ranibizumab in neovascular age-related macular degeneration. Clin Interv Aging. 2006;1(4):451–66.
Stewart MW. Aflibercept (VEGF Trap-eye): the newest anti-VEGF drug. Br J Ophthalmol. 2012;96(9):1157–8.
Grisanti S, Ziemssen F. Bevacizumab: off-label use in ophthalmology. Indian J Ophthalmol. 2007;55(6):417–20.
Kumar A, Tripathy K, Chawla R. Intraocular use of bevacizumab in India: an issue resolved? Natl Med J India. 2017;30(6):345–7.
Hernandez-Pastor LJ, Ortega A, Garcia-Layana A, Giraldez J. Ranibizumab for neovascular age-related macular degeneration. Am J Health Syst Pharm. 2008;65(19):1805–14. https://doi.org/10.2146/ajhp070342.
US Food and Drug Administration. (Lucentis®): full prescribing information. http://www.fda.gov/cder/foi/label/2006/1251561bl.pdf. Accessed 27 Mar 2023.
European Medicines Agency. Ranibizumab (Lucentis®): summary of product characteristics. [http://www.emea.europa.eu/humandocs/PDFs/EPAR/lucentis/H-715-PI-en.pdf. Accessed 27 Mar 2023.
Sengupta S. Current perspectives on use of anti-vascular endothelial growth factor agents for retinal disorders. Indian J Ophthalmol. 2021;69(2):209–10.
Chakraborty D, Mondal S, Boral S, Das A, Sinha TK, Majumdar S, et al. Biosimilar versus InnovAtor MoLecule of RAnibizumab in Neovascular Age-Related MaCular DEgeneration (The BALANCE Trial): real-world evidence. Clin Ophthalmol. 2023;17:1067–76.
Guidelines on evaluation of similar biotherapeutic products (SBPs). In: WHO Expert Committee on Biological Standardization: Sixtieth report. Geneva: World Health Organization; 2013: Annex 2 (WHO Technical Report Series, No. 977). https://www.who.int/biologicals/publications/trs/areas/biological_therapeutics/TRS_977_Annex_2.pdf. Accessed 27 Mar 2023.
Sharma S, Gupta V, Maiti A, Natesh S, Saxena S, Dave V, et al. Safety and efficacy of Razumab™ (world’s first biosimilar ranibizumab) in wet age-related macular degeneration: a post-marketing, prospective ASSET study. Int J Retina Vitreous. 2021;7(1):1.
Apsangikar P, Ghadge P, Naik M, Nair S, Payghan R. Randomised, double-blind, comparative clinical study of new ranibizumab biosimilar in neovascular (wet) age-related macular degeneration. Clin Ophthalmol. 2021:3087–95.
Sheth JU, Stewart MW, Khatri M, Gupta SR, Chawla S, Rajendran A, et al. Changing trends in the use of anti-vascular endothelial growth factor (anti-VEGF) biosimilars: Insights from the Vitreoretinal Society of India Biosimilars of Anti-VEGF Survey. Indian J Ophthalmol. 2021;69(2):352–6.
Ranibizumab biosimilar. Phase III, Comparative, Double Blind, Randomized, Multi-centric study to compare the Efficacy, Safety and Immunogenicity of Sun’s Ranibizumab with Reference Biologic in Patients with Neovascular Age-related Macular degeneration (wet AMD). (ranibizumab) Clinical Study Report (Mar 2022). Sun Pharmaceutical Industries Limited (SPIL), India.
Central Drugs Standard Control Organization, Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India. Permission to manufacture and market ranibizumab solution for injection (r-DNA origin) (MF/BIO/23/000020 dated 24 Mar 2023). Sun Pharmaceutical India Limited, Mumbai, India. https://cdsco.gov.in/opencms/opencms/system/modules/CDSCO.WEB/elements/download_file_division.jsp?num_id=MTAwNzY=. Accessed 24 Apr 2023.
ElSheikh RH, Chauhan MZ, Sallam AB. Current and novel therapeutic approaches for treatment of neovascular age-related macular degeneration. Biomolecules. 2022;12(11):1629.
Kelkar A, Webers C, Shetty R, Kelkar J, Labhsetwar N, Pandit A, et al. Factors affecting compliance to intravitreal anti-vascular endothelial growth factor therapy in Indian patients with retinal vein occlusion, age-related macular degeneration, and diabetic macular edema. Indian J Ophthalmol. 2020;68(10):2143–7.
Sharma A, Reddy P, Kuppermann BD, Bandello F, Lowenstein A. Biosimilars in ophthalmology: “is there a big change on the horizon?” Clin Ophthalmol. 2018;12:2137–43.
Stewart MW, Narayanan R, Gupta V, Rosenfeld PJ, Martin DF, Chakravarthy U. Counterfeit avastin in India: punish the criminals, not the patients. Am J Ophthalmol. 2016;170:228–31.
Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–908.
Antoszyk AN, Tuomi L, Chung CY, Singh A. Ranibizumab combined with verteporfin photodynamic therapy in neovascular age-related macular degeneration (FOCUS): year 2 results. Am J Ophthalmol. 2008;145(5):862–74.
Holz FG, Amoaku W, Donate J, Guymer RH, Kellner U, Schlingemann RO, et al. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118(4):663–71.
Acknowledgements
We thank the participants who volunteered for the study and teams at all participating sites. We thank the clinical operations team and clinical data management team of Sun Pharma Laboratories Limited, Mumbai.
Funding
Sponsorship for this study and its publication, including the journal’s Rapid Service Fee, was funded by Sun Pharmaceutical Industries Limited, Mumbai, India.
Author information
Authors and Affiliations
Contributions
Asim Ghosh, Usha Nikumbh, Chaitanya Shukla, Rohit Laul, Abhishek Dixit, Santosh Mahapatra, Sameera Nayak, Urmil Shah, Sandeep Parwal, Narendran Venkatapathy, Natasha Radhakrishnan, Anup Kelgaonkar, Sandeep Saxena, Divyansh Mishra, Vivek Dave, Perwez Khan, Manojkumar Saswade, Malli Shantilal, Kim Ramasamy, and Smitha Sreekanta were involved in conduct of the study. Maulik Doshi, Shilpi Dhawan and Lalit Lakhwani were involved in designing the study. Piyush Patel, Sapan Behera, and Mandodari Rajurkar were involved in data interpretation. Piyush Patel and Mandodari Rajurkar were involved in manuscript writing and finalising. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Authors Asim Ghosh, Usha Nikumbh, Chaitanya Shukla, Rohit Laul, Abhishek Dixit, Santosh Mahapatra, Sameera Nayak, Urmil Shah, Sandeep Parwal, Narendran Venkatapathy, Natasha Radhakrishnan, Anup Kelgaonkar, Sandeep Saxena, Divyansh Mishra, Vivek Dave, Perwez Khan, Manojkumar Saswade, Malli Shantilal, Kim Ramasamy, and Smitha Sreekanta were the study investigators and they received grants from the sponsor for conducting the study at their respective sites and declare no conflict of interest. Mandodari Rajurkar is a full-time employee of Sun Pharma Laboratories Limited. Maulik Doshi, Sapan Behera, Piyush Patel, Shilpi Dhawan, and Lalit Lakhwani were affiliated with Sun Pharma Laboratories Limited during the conduct of the study and are no longer part of the organisation and declare no conflict of interest.
Ethical Approval
The study was approved by the Drug Controller General of India and the IEC at each participating study site. The list of study sites and their respective IEC details is provided in the Supplementary Material. All patients provided written informed consent before participation in the study. The study was performed in accordance with the Declaration of Helsinki 1964 and its later amendments. All patients provided informed consent to participate in the study.
Additional information
Prior Presentations: Virtual poster presentation (poster no. P-184) of this study was made at the World Ophthalmology Congress, 9–12 September 2022.
Dr. Maulik Doshi, Dr. Sapan Behera, Dr. Piyush Patel, Dr. Shilpi Dhawan and Dr. Lalit Lakhwani were full time employees of Sun Pharma Laboratories Limited at the time of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ghosh, A.K., Nikumbh, U.S., Shukla, C.K. et al. Efficacy, Safety and Immunogenicity of Sun’s Ranibizumab Biosimilar in Neovascular Age-Related Macular Degeneration: A Phase 3, Double-Blind Comparative Study. Ophthalmol Ther 13, 1369–1382 (2024). https://doi.org/10.1007/s40123-024-00883-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00883-5