Abstract
This literature review will provide a critical narrative overview of the highlights and potential pitfalls of the reported animal models for limbal stem cell deficiency (LSCD) and will identify the neglected aspects of this research area. There exists significant heterogeneity in the literature regarding the methodology used to create the model and the predefined duration after the insult when the model is supposedly fully fit for evaluations and/or for testing various therapeutic interventions. The literature is also replete with examples wherein the implementation of a specific model varies significantly across different studies. For example, the concentration of the chemical, as well as its duration and technique of exposure in a chemically induced LSCD model, has a great impact not only on the validity of the model but also on the severity of the complications. Furthermore, while some models induce a full-blown clinical picture of total LSCD, some are hindered by their ability to yield only partial LSCD. Another aspect to consider is the nature of the damage induced by a specific method. As thermal methods cause more stromal scarring, they may be better suited for assessing the anti-fibrotic properties of a particular treatment. On the other hand, since chemical burns cause more neovascularisation, they provide the opportunity to tap into the potential treatments for anti-neovascularisation. The animal species (i.e., rats, mice, rabbits, etc.) is also a crucial factor in the validity of the model and its potential for clinical translation, with each animal having its unique set of advantages and disadvantages. This review will also elaborate on other overlooked aspects, such as the anaesthetic(s) used during experiments, the gender of the animals, care after LSCD induction, and model validation. The review will conclude by providing future perspectives and suggestions for further developments in this rather important area of research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The validity of a limbal stem cell deficiency (LSCD) animal model depends primarily on the choice of animal species, the method employed for LSCD induction, and the validation techniques used to confirm the presence of LSCD. |
The literature is replete with diverse examples of specific LSCD animal models, highlighting the challenges in achieving a consistent and reproducible representation of LSCD in animal research. |
While each method of LSCD induction, e.g., chemical, thermal and surgical, has its own set of advantages and disadvantages, the unique biological response characteristic of each method can be leveraged for studying different aspects of LSCD. |
The other often-overlooked aspects of LSCD animal research are considerations regarding age and gender selection, sample size calculations, logistics, choice of anaesthetics, reporting of adverse events, and post-intervention care and follow-up. |
Establishing a universally accepted definition of LSCD for animal research remains a challenge; however, diagnostic techniques such as impression cytology and imaging combined with clinical slit lamp assessment emerge as promising tools to address this unmet need. |
Introduction
Limbal stem cells (LSCs) represent a population of adult stem cells localised within the basal layer of the limbal epithelium and are essential in maintaining the structural integrity and optical clarity of the cornea [1]. Direct damage to LSCs and/or the destruction of the limbal niche microenvironment leads to limbal stem cell deficiency (LSCD), an entity characterised by failure of the ocular surface, with myriad findings including persistent/recurrent epithelial defects, corneal neovascularisation, chronic ocular surface inflammation, and scarring, which often lead to pain and blindness [2]. LSCD can present unilaterally or bilaterally, and can be partial or total, with various acquired and hereditary causes. Iatrogenic causes comprise a significant portion of acquired LSCD, attributed in particular to glaucoma surgeries performed with or without anti-metabolites [3]. Given the wide range of pathologies giving rise to LSCD, estimating its prevalence has been somewhat challenging. This is because the incidence of occupational and domestic as well as assault-related injury, the main cause of LSCD, varies significantly across different parts of the world [4]. Reports from the Western world have documented an annual occurrence ranging between 2.29 and 3.81 × 10–6 cases per million population, predominantly attributed to factors such as contact lens overuse and Stevens–Johnson syndrome [4, 5]. Conversely, in other parts of the world, chemical injuries resulting from workplace-related incidents comprise a significant portion of LSCD aetiology, reported to be responsible for as much as 84% of all unilateral LSCD cases [6, 7].
The definitive treatment of LSCD involves replenishment of limbal epithelial stem cells by means of autologous or allogeneic transplantation [8]. In this context, animal models serve as indispensable tools for the development and evaluation of novel treatment modalities for this debilitating ocular surface disease. Moreover, animal models can also assist in unravelling fundamental biological mechanisms underlying LSCD pathogenesis and offer insights into the identification of novel biomarkers essential for diagnostic and prognostic purposes, but also for monitoring progression of disease and assessing response to treatment. The fidelity of animal models in accurately replicating human LSCD is essential in the expeditious translation of discoveries in preclinical studies into human application. However, the current repertoire of LSCD animal models have significant limitations in precisely replicating the human clinical presentation, thus highlighting the need for more standardised, reproducible, and effective models for understanding LSCD pathophysiology. Notably, there exists a significant heterogeneity and inconsistency in the literature regarding the methodology used to create LSCD models. Studies also diverge in their definition of LSCD as well as the temporal interval for deeming the model fully fit for evaluation and/or for testing various interventions and efficacy assessment in drug development. This literature review will provide a critical narrative overview of the highlights and potential pitfalls of the reported animal models for limbal stem cell deficiency (LSCD) and highlight the neglected aspects of this area of research, but will also provide future perspectives and suggestions for further developments.
This critical narrative literature review article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Animals Used for LSCD Research
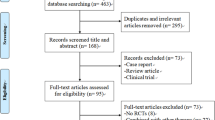
When choosing an appropriate animal model for a specific research study, it is essential to take into consideration the degree of resemblance between the anatomical dimensions of the target organ in the selected animal species and those in humans [9]. Additionally, a thorough evaluation of the costs associated with procurement and maintenance is fundamental. Ideally, it is considered best practice for the ocular dimensions of the preferred test animal to closely approximate those of humans, considering that the surgical manipulations and clinical evaluations would be technically challenging in smaller animals. Furthermore, specimens obtained from small animals would demand analytical methods with unusually high sensitivity, imposing an additional financial burden. Equally vital to the selection process is the biochemical similarity of the eye as well as the availability of reagents and research kits specific to the species of the chosen animal. The general trend is that smaller animals, such as mice and tadpoles, are used for understanding fundamental biological mechanisms underlying ocular surface wound healing and LSCD. In comparison, larger animals such as rabbits are more commonly employed for tapping into the therapeutic potential of novel treatment modalities (Fig. 1 and Supplementary Material).
A comparative pie-chart analysis of limbal stem cell deficiency (LSCD) induction methods and research objectives in studies involving rabbit (A), rat (B), and mouse (C) models. A detailed account of the methodology used to construct this figure along with an exhaustive list of publications is provided in the Supplementary Material. NaOH sodium hydroxide
Mice
Mice hold a preeminent position in laboratory animal research due to the similarity of their eyes to human eyes. The most popular strain employed in LSCD research is the C57BL6 mouse with a corneal diameter of 2.6 ± 0.2 mm and total corneal and epithelial thickness of 116 ± 7.6 µm and 40.59 ± 5.8 µm, respectively [10]. A fundamental advantage inherent in utilising mice for experimental investigations lies in the possibility of genetically engineered mouse strains. This provides researchers with the opportunity to replicate key features of human genetic conditions and explore the role of individual genes and the molecular pathways underpinning the disease process. Nonetheless, while transgenic mice models may be advantageous in offering exceptional reproducibility of the model, they are constrained by cost and time considerations [11]. The increasing trend in the use of mice in animal studies is also linked to advancements in biochemical techniques that require smaller tissue samples and the availability of a wide array of analytical kits and reagents to study mouse models [12]. However, the small size of the mouse eye demands a more significant number of animals per experiment than analogous experiments involving rat eyes [12]. Likewise, considering that the mouse eye measures one-fifth of an average human eye, surgical manipulations harbour the risk of unintended injury and perforation [13]. Moreover, the handling of tissue specimens for histopathological examinations may be equally challenging. A significant disparity between murine models and humans is that they lack a comparable anatomical structure akin to the palisades of Vogt, along with niche-like attributes responsible for the accommodation and safeguarding of corneal stem cells, a characteristic inherent to the human cornea [14, 15]. Unlike human corneas, research has also revealed that the entire mouse cornea is home to epithelial stem/progenitor cells in addition to the limbus, an essential consideration in determining the method for LSCD induction [15, 16]. It is also noteworthy that different strains of mice exhibit varied wound-healing responses; however, the overall severity of scarring in mice is comparatively milder when contrasted with rats and rabbits [12, 17].
Rats
The most frequently employed strain is the Sprague Dawley rat, characterised by an average corneal diameter ranging from 5 to 6 mm [12, 18]. Akin to the mouse limbal niche, the rat limbal niche is characteristic in that its full maturation potentially extends into the postnatal life, with some corneal basal epithelial cells maintaining their stem cell function before becoming exclusively localised within the limbal area [19]. Intriguingly, while side population (SP) cells are reportedly absent in the central corneas of human and rabbits, an interesting study demonstrated a higher abundance of SP cells in the central corneal epithelium of rats in comparison to their limbal region [20]. Despite these observations, the precise origin of SP cells, specifically whether they exclusively possess epithelial stem cell attributes, remains unclear [19, 21].
Rats are particularly favored in research due to their cost-effectiveness and ease of breeding, making them exceptionally suitable for a wide range of wound healing investigations. In contrast to mice and rabbits, which require injectable anaesthesia, rats can be given inhalational anaesthesia, conferring a higher degree of control over the anaesthesia process, with reduced mortality [12].
Rabbits
Rabbits have been widely used as a model for various ocular diseases due to the structural similarity between their eyes and those of humans. They have a corneal thickness of 300–400 µm and a slightly larger corneal diameter measuring 13.5–14 mm and 15 mm in the vertical and horizontal meridians, respectively [22]. Among rabbit strains, New Zealand White rabbits (Oryctolagus cuniculus) are the most commonly used, and the optimal age for acquisition typically falls within the range of 6–12 weeks [22]. Since the size of the rabbit cornea mirrors that of humans, diagnostic tools developed for human use, such as anterior segment optical coherence tomography and in vivo confocal microscopy, can be readily applied in studying rabbit corneas [9]. Furthermore, surgical procedures intended for inducing LSCD or for therapeutic purposes can be more readily performed. Rabbit eyes have also been shown to respond to injuries similarly to humans, albeit with a more severe and less predictable inflammatory response [12, 23]. Despite the many similarities, however, rabbit eyes differ from human eyes in their slower blink rate and the presence of a nictating membrane that exerts extra frictional force onto the nasal aspect of the ocular surface, often leading to asymmetrical development of the pannus [24]. Arguably, the nictating membrane in the rabbit eye can also provide some degree of protection against ocular surface injury, mainly when the chemical agent is administered without the animal being anaesthetised, such as in the case of whole-body or topical exposure [25]. Hence, the nictating membrane may need to be removed or sutured to its origin for wider exposure during chemical administration. In contrast to other mammalian species, where the corneal epithelium undergoes a continuous turnover process approximately every 1–2 weeks, the central epithelium in rabbit eyes can persist for extended durations in limbus-deficient models [26]. This phenomenon underscores the remarkable self-maintenance capability of rabbit cornea conferred by its central corneal epithelium.
Other disadvantages pertaining to the use of rabbit models are their higher procurement and maintenance costs in comparison to rats and mice, the limited availability of polyclonal antibodies against proteins of interest, and the reduced availability of genetically engineered strains [12]. Moreover, the respiratory centre in rabbits is reportedly more susceptible to anaesthetics, increasing the risk of respiratory suppression when anaesthesia is administered [27]. This phenomenon in rabbits is frequently associated with a heightened risk of mortality, particularly when surgical procedures are performed on sick animals using anaesthetics with a narrow safe-dose range [28]. Another crucial aspect of using New Zealand White rabbits, and hence an albino strain, is the lack of stromal melanocytes [23]. On a positive note, albino strains offer improved imaging of whole flat mounts of the cornea owing to the lack of iris pigmentation, which would typically adhere to the inner surface of the cornea and impede the imaging process. However, these strains reportedly have significant disparities in their biological response to wound healing, drug effects, and drug distribution compared to their pigmented counterparts [23]. Since melanocytes constitute a pivotal cellular component of the limbal niche, the extent to which LSCD models in pigmented or non-pigmented strains may diverge in their similarity to human LSCD remains uncertain.
Other Animals
Frog (Xenopus) models of LSCD have also been proposed, partly due to the similarity in corneal development and morphology when compared with humans [29]. However, the minute size of their corneas makes it challenging to monitor LSCD clinically. An additional limitation associated with using Xenopus species as an experimental model is the protracted maturation period required for the development of the tadpole cornea, spanning several months [12]. Moreover, small-scale tissue sizes also limit the handleability of tissues for histopathological examination, posing a challenge during tissue dissection and excision.
The zebrafish is another potential model that can be exploited in LSCD research. These animals are relatively cheap and are amenable to live imaging due to their physical transparency [12]. As in mice, they can be genetically manipulated, providing the opportunity to study the effects of altered genes [30]. Moreover, their post-fertilisation maturation into adulthood is rapid. However, these models are constrained by their minute tissue sizes, leading to potential issues like those with small and limited specimens encountered in other small animals.
Other studies have employed larger animal models for LSCD research such as the Boer or Guanzhong dairy goats [31,32,33,34]. In these studies, LSCD was achieved mainly through surgical removal of the limbus, which was occasionally supplemented with the application of NaOH [31, 34]. Nonetheless, as with other large animals, these models have significant limitations including the lack of inbred strains, substantial costs associated with procurement and maintenance, the difficulty with handling larger animals, and the lack of a wide range of analytical reagents for comprehensive evaluations that are more readily available in murine models [35].
Methods of LSCD Induction
Physical/Surgical Trauma
Surgical approaches for creating LSCD models range from simple limbus to limbus epithelial scraping by a blunt spatula to wide limbal dissection coupled with the removal of a 5-mm segment of tissue on both sides of the limbus. A recent systematic review indicates that surgical/physical methods may be more likely to achieve the desired LSCD outcome in a more reproducible and consistent manner [36]. On the other hand, surgical techniques can indeed be technically challenging and pose challenges in standardising the treatment consistently among different operators and laboratories [28].
Epithelial Debridement
This model has mainly been employed in mice and involves the use of a blunt metal spatula with a 0.3-mm tip for scraping the entire corneal epithelium from limbus to limbus [37,38,39,40]. It is advantageous in that it limits the injury to the epithelium, with less inflammation, neovascularisation, and scarring, making it an ideal model for ascertaining the mechanisms through which a specific treatment influences the outcome [37]. However, this method is limited by its ability only to induce partial LSCD [37, 38]. Furthermore, achieving complete corneal epithelial removal with a spatula can present challenges when attempting to standardise and execute the procedure in a reproducible manner, due to potential variations in the surgical handling of the tissue among different operators [38]. It is important to note that when employing a dulled blade for debridement, the basement membrane and the basal surface of basal cells remain largely undisturbed [39, 40]. This preservation of structural integrity may impose constraints on experiments intended to evaluate myofibroblast formation [12].
Limbectomy
The conventional procedure for limbectomy typically involves dissecting the limbus to a depth of approximately 30% and then surgically removing a 2-mm segment from both sides of the limbus. Following this, the peripheral cornea and the scleral and conjunctival tissues within the dissection boundary are excised [41,42,43].
Several reports have demonstrated the retention of intact limbal epithelium when surgical limbectomy is performed as a standalone procedure [8, 44, 45]. In their seminal study, Huang and Tseng observed that only 33% of their rabbits developed corneal vascularisation 6 months after complete surgical limbectomy. However, when they combined limbal removal with corneal epithelial removal, this figure increased dramatically, to 96% [46]. Likewise, complete thermal obliteration of the limbus deliberately extending to the depth of the ciliary body proved inadequate in inducing corneal neovascularisation even 4 months after the initial insult in a murine model [15]. These observations provide compelling evidence for the recent discovery of corneal-committed cells resident within the cornea capable of dedifferentiating and repopulating the stem cell pool [46, 47]. Given the possibility that the corneal limbus might not be the sole niche housing stem cells, approaches targeting limbus removal should be supplemented with the removal of the corneal epithelium [15, 16, 48]. To address this issue, investigators have recently combined surgical limbectomy with the application of NaOH in addition to limbal epitheliectomy, aiming to cause more extensive injury to stem cells residing within the cornea and limbus [31, 49, 50].
There may be a learning curve associated with surgical limbectomy, which may result in inconsistencies across the created models over the course of the study within and between different operators and laboratories [44]. Furthermore, surgical limbectomy demands more vigilance during and after the procedure than other physical methods, such as physical scraping or the use of the AlgerBrush [28]. This heightened vigilance is crucial to alleviate the risk of unintended perforation and entry into the anterior chamber associated with surgical limbectomy. It is also noteworthy that surgical limbectomy in laboratory animals does not evoke the customary inflammatory response observed after chemical or thermal injury in humans [51]. This holds particular significance, as the extent of the inflammatory reaction plays a crucial role in dictating the fate of stem cells following such injury. Notably, a comparative study demonstrated that surgical excision leads to less limbal hyperaemia, corneal oedema, and neovascularisation than that with alkali exposure in New Zealand rabbit eyes [45].
AlgerBrush
The AlgerBrush is a motorised instrument used to remove corneal rust rings following removal of a metallic foreign body and can also be used during pterygium surgery for shaving fibrovascular tissue from the corneal surface. It has recently emerged as a valuable tool in inducing LSCD in rabbits, rats, and mice [44, 52]. Since it requires less force and yields a more uniform and reproducible injury, it has been found more advantageous for limbal and corneal epithelial removal when compared to a blunt spatula [38]. The procedure typically entails two passes, with the lateral side of the burr facing the limbal and corneal region, with each pass taking approximately 5–6 s, complemented by thorough rinsing of the ocular surface [38].
The device offers three distinct burr types, each featuring 0.5- and 1-mm-diameter pointed burr and 2.5-mm-diameter rounded burr (Table 1). The selection of burr size for AlgerBrush usage varies depending on the animal model under consideration. While the 0.5-mm burr was more frequently used in mice owing to the small size of their eyes [38, 53, 54], the 2.5-mm rounded burr was found more effective in removing corneolimbal epithelium in rabbits when compared to the pointed 1-mm burr [44]. It is imperative to note, however, that factors other than the size of the burr, such as the burr speed, pressure exerted, angle of the burr, and residence time, are also crucial in determining the degree and extent of the injury [12].
The injury inflicted by the AlgerBrush primarily encompasses the surface epithelium and the basement membrane, exerting minimal impact on the underlying stroma when compared to chemical methods, thanks to a pressure-sensitive clutch preventing stromal penetration [40, 57]. Consequently, this mitigates the risk of excessive inflammation and scarring, facilitating interventions targeting LSCD and making it easier to assess post-intervention outcomes [52]. However, it is worth noting that less inflammation and scarring may pose a limitation in replicating real-life scenarios, especially when attempting to simulate injury resulting from chemical trauma. The LSCD model induced by a rotating burr is sustainable, lasting at least 3 months after the induction [52]. Its application is easy even in the hands of less experienced operators; however, the learning curve can still hinder achieving consistent and reproducible outcomes across different operators and laboratories.
The use of the AlgerBrush was discredited by some authors due to its inefficiency in achieving complete removal of the limbal and corneal epithelium [38, 54]. To avoid incomplete epithelial removal, other authors have suggested monitoring the degree of epithelial debridement using fluorescein stain and thoroughly rinsing the ocular surface after the procedure [44]. This precautionary measure is essential due to the inherent tendency of the rotating burr to displace cells towards the periphery of the resulting wound, potentially resulting in the re-engraftment of dislodged cells back onto the ocular surface when the animal resumes blinking [12]. The ability of the AlgerBrush to effectively remove the basement membrane has also been a subject of debate, as highlighted in a study conducted by Stepp et al. [12]. Notably, while the rotating burr was found to completely eliminate the basement membrane at the central region of the mouse cornea, it yielded only a partial effect in the case of rat corneas [12, 40]. In contrast, Boote et al. observed that the basement membrane was left intact after a single application of the rotating burr in mouse eyes [58]. However, a second round of the AlgerBrush coupled with the exertion of pressure onto the cornea led to complete denudation of the basement membrane, along with minimal removal of anterior stromal tissue [58].
Akin to other physical methods that directly disrupt the microarchitecture of the limbal niche, it is plausible that using a rotating burr may limit the efficacy of cellular therapies by potentially impeding the engraftment of transplanted cells within their natural microenvironment [56]. Another drawback of the AlgerBrush is the potential for stromal injury or perforation stemming from excessive pressure or overtreatment and the risk of bleeding when procedures are conducted at a very slow pace [38, 52].
Chemical Injury
A wide array of chemicals has been employed to induce LSCD in animal models, ranging from sulphur mustard gas to n-heptanol, ethanol, and sodium hydroxide (NaOH) [36]. Each chemical has distinct properties and differs significantly in terms of its effectiveness in inducing LSCD. The depth and the extent of the injury also depend not only on the specific chemical agent but also on other factors such as exposure time, concentration, and the mode of application. NaOH is among the widely used chemicals for inducing LSCD, with varying concentrations, application methods, and exposure times reported in the literature. Ethanol will not be discussed in this section owing to its inadequacy in effectively removing limbal epithelial cells, necessitating its combination with limbectomy procedures or alkali burns [44].
Sodium Hydroxide
Models of NaOH exposure to induce LSCD generally involve the application of a pre-soaked circular filter paper of various sizes (Table 2) onto the ocular surface in direct contact with the central cornea, the limbus, or a combination of both. The width of the filter paper varies depending on the ocular dimensions of the experimental animal as well as the primary area of intended injury. An alternative method for limbal and corneal NaOH exposure was proposed with the use of custom-size filter papers (2 × 4 mm) that were laid onto the corneal-limbal regions for a predetermined duration, a rather less-controlled exposure when compared to the use of circular filter papers [79]. Another modification was the use of a sterile cotton swab pre-soaked with 1 N sodium hydroxide (NaOH), which was then applied to the rabbit’s eye for a duration of 30 s [80]. Notably, applying flat filter papers may be challenging with highly curved corneas of mice [72]. Furthermore, the use of filter papers may cause unintended injury to the fornix and adjacent conjunctiva [81]. To overcome these limitations, Shadmani et al. proposed the use of punch-trephine for a well-circumscribed and localised exposure [82]. Similarly, Schultz et al. utilised a well with an internal diameter of 12 mm which was firmly pressed onto the cornea and subsequently filled with 1 mL of 2 N NaOH and left intact for 60 s [83]. More recently, Żuk and associates topically administered a 0.1-mL volume of NaOH with a concentration of 10% onto the corneal surface for 10 s [84]. Holan et al. adopted a similar approach by instilling ten drops of 0.25 N NaOH on the corneal surface of rabbit eyes over the course of 60 s [85]. Likewise, two studies reported the use of topical NaOH (0.1 N and 0.15 mM) for inducing LSCD in mouse eyes [13, 86]. Despite the ease of application with the topical eye drop method, particularly in small animals, this method provides less control over the time of exposure, with an increased risk of unintended injury to adjacent conjunctiva, fornix, and eyelids [82]. Furthermore, it is presumably less likely to induce a full-blown picture of LSCD due to quick spread to other unrelated ocular surface areas, drainage from the nasolacrimal duct, and rapid dilution with the basal and reflex tear secretion.
In numerous studies, the conventional approach entails exposure to an extended region encompassing the whole circumference of the cornea in addition to the limbus using filter papers [65, 66, 71]. Notably, however, such an approach may result in severe consequences, including corneal stromal scarring, corneal ulcers, and in extreme cases, penetration of the chemical into the anterior chamber, giving rise to widespread, undesirable side effects such as damage to the ciliary body, contractable uveitis, and phthisis bulbi, which may jeopardise the efficacy of the treatment under investigation and/or animal dropout from the study [71]. On the other hand, exposure solely to the central cornea, described as central alkali burn (CAB) by Sprogyte et al., has been shown to heal without conjunctivalisation and, therefore, may not necessarily lead to LSCD, making it more suitable for corneal wound healing research [87,88,89]. Hence, limiting the contact of chemicals exclusively to the limbal area (limbal alkali burn) may be a prudent strategy, as it not only ensures the effective depletion of stem cells in this region but also serves to mitigate the aforementioned complications [90]. To this end, researchers have adopted the use of doughnut-shaped filter papers, crafted using punch trephines of various sizes to achieve the desired dimensions, with the aim of preventing exposure to the central cornea (Fig. 2) [71,72,73, 75, 77, 91]. In contrast to circular-shaped filter papers, the use of doughnut-shaped filter papers alleviates the issue with improper fit along the limbal circumference due to the convexity of the central cornea potentially causing fit issues along the limbal area. Nevertheless, it is essential to acknowledge the presence of committed corneal epithelial cells, which may migrate to the limbus and undergo dedifferentiation to become putative limbal stem cells, thereby repopulating the limbal stem cell pool [16, 47]. This may be a concern, particularly when limbal approaches are not supplemented with mechanical disruption of the limbal microarchitecture and corneal epithelial debridement. In view of this concern, Ma et al. advocated a standardised procedure involving the application of 1 N NaOH for 30 s to the albino rabbit, followed by corneal epithelial debridement [48].
A figure showing application of filter paper on a rabbit’s eye (A). For chemical injury, a sodium hydroxide (NaOH)-soaked filter paper may be applied over the entirety of the corneal and limbal surface (B) or, alternatively, they may be crafted to achieve a doughnut shape (C) using punch trephines for application exclusively to the limbal circumference. The application show in the figure is on a rabbit’s eye
The exposure time is among the other important determinants of the extent of injury in an LSCD animal model. Kethiri et al. posit that the duration of ocular surface exposure to NaOH should be restricted to a maximum of 30 s in animal models [13]. Prolonged exposures beyond this timeframe have been associated with adverse outcomes such as the development of corneal ulcers, increased susceptibility to infections, decreased palpebral fissure height, and the potential for subsequent perforations [51]. Conversely, shorter exposure durations will likely yield partial LSCD rather than total LSCD. It should be emphasised, however, that 45 s of exposure could be closer to what a patient would experience in a real-life situation [13]. To investigate the effect of varying NaOH exposure times in rabbit eyes, a group employed different time regimes to induce chemical burns of varying severity, specifically employing durations of 25 s to generate a mild burn and 45 s to generate a severe chemical burn, the latter of which resulted in more corneal stromal disruption and diminished transparency [92]. Nonetheless, it should be noted that exposure time is only one variable amongst a plethora of variables affecting the final outcome with exposure to NaOH. Other reported determinants governing the efficacy of an alkali-induced LSCD model are the concentration and volume of NaOH solution, the area of exposure (e.g., the diameter of the filter paper), mode of delivery, clearance method, and, notably, the ambient temperature and humidity [89, 93].
The concentration of NaOH can be titrated depending on the depth and extent of the desired iatrogenic injury. In their report, Villabona-Martinez et al. suggest that while a 15-s application of 0.5 N or 0.6 N NaOH may be optimal for fibrotic damage to the epithelium and the stroma, a concentration of 0.75 N of NaOH applied for 15 s would be more ideal for a full-thickness response involving Descemet’s membrane and the endothelium without causing corneal neovascularisation (NV) [93]. However, if the objective is to provoke a full-thickness reaction with persistent epithelial defects and corneal NV, 1 N NaOH may be the preferred concentration [93]. Nonetheless, one should be aware that these recommendations by Villabona-Martinez et al. are based upon a standard exposure time of 15 s with 5-mm circular filter paper followed by thorough rinsing with balanced salt solution [93].
There are numerous advantages and disadvantages associated with the use of NaOH in inducing LSCD in animal models. Alkalis cause chemical burns similar to those observed after domestic and industrial accidents, with widespread injury to the ocular surface [44]. They also effectively remove the basement membrane of the cornea [94]. Neovascularisation in alkali models of LSCD tends to be more pronounced, making it an ideal choice for studying and developing strategies to combat corneal neovascularisation. [45] However, the use of NaOH ultimately gives rise to variable phenotypes of LSCD, and the depth and extent of the elicited injury are difficult to control, which is a significant challenge, particularly when dealing with small animals such as mice [38, 94]. Complications with the use of NaOH tend to be more pronounced and occur with greater frequency, while the risk of damage beyond the limbus to the sclera and posterior ocular structure is heightened [28, 36]. Interestingly, significant disparities have also been observed in the responses of rabbit and mouse eyes to ocular surface NaOH exposure when compared with specimens obtained from human eyes afflicted with LSCD, with the latter showing more pronounced vascularisation, inflammation, and goblet cell formation [13]. Nonetheless, it should be emphasised that in the aforementioned study, total LSCD could only be reliably established in half of the experimental animals, likely due to topical single-drop application of NaOH on rabbit and mouse eyes, raising questions about the methodology employed for inducing LSCD.
n-Heptanol
n-Heptanol has been widely utilised for the purpose of removing corneal epithelial cells. However, various studies have demonstrated that the use of n-heptanol alone often leads to re-epithelialisation [66]. Additionally, its effectiveness in removing limbal epithelial cells is considerably lower [44]. However, when combined with surgical limbectomy, the success rate for LSCD development increased to 96% [41]. As a result, n-heptanol is rarely used in isolation and is commonly employed in conjunction with surgical limbectomy, debridement, or AlgerBrush application [44, 95,96,97,98]. One advantage of n-heptanol is that it selectively removes the epithelium without affecting the stroma, thereby preserving the stromal microenvironment [97]. Various exposure regimens have been proposed, ranging from 1–2 min to as long as 5 min [95, 97, 98]. Although n-heptanol was reported to successfully remove the corneal epithelium when applied for 60 and 120 s, longer durations of up to 300 s are required to eradicate the limbal basal cells [41].
Sulphur Mustard
Sulphur mustard (SM) vapour is a reactive alkylating agent that is a potential irritant to the ocular surface. Its exposure is characterised by a biphasic tissue response, namely the acute and the delayed phases, documented in both humans and animal models [99]. The delayed response, occurring as early as 2 weeks after experimental exposure, leads to LSCD. Its effects are likely driven by protracted inflammation in the limbal stroma, impairment of corneal sensory innervation, and trophic effects on the limbal niche [100, 101]. Various exposure methods have been defined, ranging from topical application to whole-body exposure [25, 99, 102]. However, due to the hazardous nature of SM vapour and its significant environmental risk to laboratory staff, it is a less preferred method for inducing LSCD [36]. Additionally, the damage caused by SM vapour extends beyond the limbus and affects the corneal endothelial layer, which undermines its validity as an appropriate LSCD model [25]. A report also noted that limbal epithelial cells exhibiting slow cycle characteristics may be more resistant to SM toxicity than the more terminally differentiated epithelial cells found in the central cornea [103]. As a result, SM exposure leads to a spectrum of LSCD severity, ranging from complete healing to instances of partial and total LSCD in both humans and rabbits, raising doubts about its suitability for studying total LSCD [100, 103].
Other Methods
Thermal Injury
Thermal injury has only been documented in one study in conjunction with rotating burr shaving of the limbal and corneal epithelium. The authors observed a more severe LSCD phenotype with pronounced corneal scarring, advocating the utility of the model in studies where the objective is to investigate stromal responses after thermal injury to the ocular surface [38]. However, inherent limitations of the proposed thermal method are the risk of perforation, the difficulty in optimising the temperature at the tip of the cautery, and the lack a standard technique for delivering heat throughout the whole circumference of the limbus.
Psoralen AMT
Psoralen AMT (Sigma-Aldrich, St. Louis, MO, USA), a planar tricyclic compound that forms cross-links between thymine bases upon exposure to light, has been employed as a topical agent to deplete corneal stem cells in frog eyes [28]. When applied topically, it interferes with DNA replication and cell division, invoking a state of stem cell deficiency in the cornea [104]. Although it stands out as a rapid, easily applicable, controllable, and single treatment option for inducing damage to limbal stem cells, it has not yet been explored in larger-scale animal models. It has also been shown to cause a delay in eye development in the treated eye, an effect that may confound the validity of the model [28].
UV Light
An interesting LSCD model was proposed by Das et al. based on repeated exposure to a standardised UV-B light in mice to emulate the ocular surface exposure to solar UV-B radiation in outdoor workers [105]. Their UV-B dose in experimental mice was equivalent to 4.5–5.2 h of occupational or environmental sunlight exposure for outdoor workers during summertime in different parts of the world [106]. Although the proposed model may be representative of a real-life situation, it is somewhat impractical considering that controlled exposure for precisely 20 min/day during the same daytime hours for a duration of 10 weeks was necessary. Furthermore, their findings in UV-B-exposed mice indicated the development of partial LSCD with cellular and structural alterations in the limbal area rather than the total depletion of limbal epithelial stem cells.
Benzalkonium Chloride
Given its well-documented cytotoxicity, benzalkonium chloride (BAC) has also been utilised as a chemical agent to induce LSCD in mouse eyes. In a study conducted by Lin et al., various concentrations of BAC (0.1%, 0.25%, and 0.5%) were applied to the mouse eyes four times a day over a 28-day period [107]. On the 28th day, the continuous exposure to 0.5% BAC resulted in the development of LSCD, as evidenced by clinical manifestations such as corneal conjunctivalisation and neovascularisation, the presence of goblet cells on the cornea, and the loss of putative stem cell markers [107]. Nonetheless, the long-term sustainability of this model after cessation of BAC exposure, particularly in achieving total LSCD, remains unknown. Moreover, such effects of BAC could be specific to mouse eyes, necessitating further studies involving other animal models.
Congenital LSCD
The majority of animal models employed in the study of LSCD have traditionally focused on acquired LSCD, while research into congenital LSCD has remained relatively limited. A well-established model for mimicking congenital LSCD involves the utilisation of the heterozygous Pax6+/− mouse, which serves as a primary model for aniridia and the associated keratopathy; however, its concordance with human aniridia is debated [108, 109]. Notably, Wang et al. recently proposed a novel method to induce congenital LSCD through forced eyelid opening immediately after birth [110]. The authors posit that prematurely removing the eyelid ditch at birth would impair the protective function of the eyelids on the vulnerable and still immature ocular surface tissues, thereby leading to limbal stem cell loss [110]. Subsequent to this intervention, the animals were followed up for 1 month, at the conclusion of which they were euthanised to validate the LSCD model. The methodology was reportedly easy to perform, and the ensuing inflammation was identified as the primary driver of the long-term development of an LSCD-like phenotype akin to keratitis-induced LSCD observed in humans [110]. Nonetheless, to what extent the proposed model may resemble the primary cause of LSCD in practicality, namely ocular surface chemical and thermal injury, warrants further investigation.
Methods of Model Validation
The in vivo validation of LSCD entails a wide range of methods, ranging from slit lamp examinations to various imaging techniques and impression cytology. Although the latter can be used to perform immunological and molecular assays using cells harvested from the corneal surface while the animal is alive, definitive histological diagnosis requires euthanising the animal. Subsequently, the presence of LSCD can be confirmed through various techniques, including biochemical assays, immunofluorescence, immunohistochemistry, enzyme-linked immunosorbent assay (ELISA), and others, all of which fall beyond the scope of this review [36]. Hence, this section will only elaborate on methods available for LSCD validation using clinical investigations performed while the animal is still alive.
Slit Lamp Examination
The clinical diagnosis of human LSCD relies heavily on slit lamp examination, looking for specific signs of conjunctivalisation of the corneal surface, signs indicative of epithelial dysfunction such as persistent or recurrent epithelial defects, neovascularisation, and ocular surface inflammation and scarring [111]. Various scoring schemes have been proposed to grade features of LSCD in animal models that take into account the degree of limbal involvement, corneal epithelial irregularity, corneal opacity, and corneal neovascularisation, along with the area and the delay in fluorescein staining [51, 70, 73, 112, 113]. These scoring schemes serve as crucial tools for quantifying and standardising the evaluation of LSCD features in research settings, facilitating consistency and reproducibility and ensuring comparability across different studies. Notably, while some of these grading schemes were originally developed specifically for animal studies, most were initially designed for human LSCD evaluation and subsequently modified for animal research. Given the inherently subjective nature of such grading systems, they are prone to potential misinterpretation and subjective variability [2]. Furthermore, subtle signs of LSCD may be overlooked, further highlighting the importance of supplementing clinical observations with more objective assessment methods.
An often overlooked aspect in clinical examination of LSCD animal models is the assessment of the eyelids after the initial insult. This is important, as cicatricial lid abnormalities, such as entropion or ectropion, may directly influence the outcome of a tested treatment modality in an animal model [24]. Likewise, tear film integrity may also be compromised due to the destruction of glands supplying all three layers of the tear film [113]. Therefore, the presence or absence of such abnormalities should be reported and, more ideally, graded using standardised grading scales.
Impression Cytology
The identification of goblet cells on the corneal surface through impression cytology is widely regarded as the gold standard for diagnosing LSCD. However, reports show that goblet cells are absent in 35–65% of human cases, particularly in patients with extensive ocular surface damage associated with squamous metaplasia and keratinisation [114]. Therefore, while the presence of goblet cells is confirmatory for LSCD, their absence does not imply absence of LSCD. Alternatively, impression cytology samples can also be used to differentiate the corneal or conjunctival origins of harvested cells via immunostaining for biomarkers such as cytokeratins 3 and 12 for cornea and 7, 13, and 19 for conjunctiva [2]. An overview regarding the specificity of each biomarker and its reliability in identifying LSCD is, however, beyond the scope of this review.
Various factors are implicated in influencing the sensitivity of impression cytology including the amount of pressure exerted during sampling, location of sampling, filter pore size, and surfactant treatment [2, 111]. Furthermore, impression cytology is constrained by its ability to sample only superficial cells [115]. Notably, it should be kept in mind that the origin of goblet cells in murine models may be corneal stem cells, complicating its interpretation in animal models [16]. Overall, its limited sensitivity and the lack of spatial resolution renders impression cytology an impractical tool for grading disease [8, 111]. Nevertheless, the non-invasive nature of impression cytology, coupled with its ability to provide valuable in vivo data, including the ability to delineate cell origins through immunological and molecular assays, has rendered it an indispensable tool in the realm of LSCD research [111, 116].
Anterior Segment Optical Coherence Tomography
Anterior segment optical coherence tomography (AS-OCT) is a non-invasive technique that provides real-time in situ imaging of tissues. While it boasts a lower resolution than in vivo confocal microscopy, AS-OCT offers the advantage of significantly shorter scan acquisition times and a larger field of view. In the context of LSCD research in animal models, it has been used to measure corneal and limbal thickness along with corneal epithelial thickness [26, 74, 75]. Furthermore, AS-OCT has proven invaluable in visualising the degree of corneal scarring and oedema, monitoring the progression of the healing process, and confirming the successful surgical removal of limbal tissue at an appropriate depth in animal models [26, 59, 64, 93].
Recently, the degree of corneal neovascularisation in LSCD was demonstrated using AS-OCT angiography in humans; however, no study to date has explored its utility in animal models of LSCD [117]. Since corneal neovascularisation is not a specific sign of LSCD, the use of AS-OCT angiography in LSCD diagnosis may be somewhat limited. However, it may hold promise as a tool for quantifying the extent and degree of corneal neovascularisation in animal studies, thus warranting further investigation [2].
In Vivo Confocal Microscopy
Although in vivo confocal microscopy (IVCM) can be effectively used for the analysis of the limbal microarchitecture, epithelial cell morphology, and the integrity of corneal subbasal nerve plexus, aiding in LSCD diagnosis, it is limited in distinguishing between various epithelial phenotypes overlying the cornea [114]. Additionally, the morphological features of goblet cells as detected by IVCM are a subject of controversy, with some reports claiming them as having a hypo-reflective cytoplasm, while others indicate a hyper-reflective cytoplasm [2]. Furthermore, there are no definitive IVCM criteria established for the diagnosis of LSCD in animal models, and its findings may only be used to support the diagnosis [2]. Nonetheless, IVCM offers several advantages as a rapid, non-invasive, and repeatable in vivo technique. It proves beneficial in monitoring the progression of disease and response to therapy, and provides quantitative data that can be instrumental in validating an LSCD model [111, 114]. It has also been shown to aid in visualising findings suggestive of LSCD, such as enhanced epithelial reflectivity, corneal neovascularisation, and corneal stromal inflammatory cells in a rabbit animal model [67]. Thus, while IVCM may not serve as the sole diagnostic criterion for LSCD, it plays a valuable role as an adjunctive clinical test in both clinical evaluation and research contexts.
Other Considerations
Age of the Animals
The animal’s age may be pivotal in determining how the local tissue responds to the iatrogenic insult. As in humans, younger animals tend to exhibit a more pronounced inflammatory response, which may, in turn, affect the outcome of the model and the success of the intervention under investigation [22]. Notably, older animals may be more desirable where excessive inflammatory response to the insult is a notable concern. Furthermore, it is essential to acknowledge that the ageing process may also have an impact on the structural and phenotypic properties of the limbal niche [36].
Gender Selection
Studies vary significantly in their selection of gender in laboratory animal research, with a notable trend toward a male bias, which can be attributed in part to their increased availability [36]. Amongst the factors to note are the increased susceptibility to persistent epithelial defects and the presence of fewer ocular surface goblet cells in the female sex [118]. This raises questions regarding the generalisability of research findings obtained from male animals to the female gender. Conversely, it is essential to consider that hormonal fluctuations within female animals may also exert a notable influence on the characteristics and magnitude of the wound-healing response, an effect that is not present in male animals. Another technical consideration in gender selection is the issue with male animals being more aggressive when housed in groups, which carries the risk of inflicting harm upon cage mates [93, 119]. Group housing of littermates rather than random allocation of animals as cage mates could be a solution to remedy this potential problem [119].
Sample Size and Logistics
The number of animals allocated per group depends on the chosen animal model, particularly when the research entails a wide array of analyses necessitating a substantial quantity of tissue specimens. Due to the small size of the mouse cornea, experiments involving mouse eyes may require more animals per experiment than analogous experiments performed in rat and rabbit eyes [12]. Another pivotal consideration is the logistical aspects that can potentially influence the number of animals manageable within a designated timeframe and, consequently, the maximum number of animals that can be enrolled in a study. This is governed not only by the time required to establish an efficient animal model with the chosen method but also by the amount of time that should be dedicated to performing various procedures, including imaging, photography, and tear collection, among others. Indeed, Li et al. reported that, even in the skilled hands of a proficient research surgeon, a maximum of three eyes can be effectively treated in a single day using the AlgerBrush [44]. However, even though these considerations are noteworthy, particularly for logistics and time management, they should not directly influence the sample size calculations in LSCD research.
The general recommendation is that a minimum of six eyes should be enrolled per group for toxicological studies and 8–12 per group for research studies [22, 93]. Likewise, in order to maximise uniformity and comparability over the course of the study, the number of animals per study should be kept within the range of 20 and 30 [22]. However, it should be emphasised that these figures, as rough estimates, may only serve as guidance, and therefore a statistical sample size calculation should be performed to ensure the validity and generalisability of the results.
Post-intervention Tarsorrhaphy and Contact Lens Placement
A tarsorrhaphy procedure may be undertaken primarily to mitigate the risk of animals engaging in vigorous eye-rubbing activity or experiencing injury inflicted by their cage mates, particularly in group-housed laboratory animals [75, 120]. However, it must be emphasised that the protective function of tarsorrhaphy may fall short of the desired levels, unlike that observed in humans [24]. Tarsorrhaphy can also be combined with bandage contact lenses to safeguard the integrity and viability of surgical interventions such as ocular surface implants, explants, or grafts [95, 121]. Nevertheless, it is essential to note that the radius of curvature of the cornea in experimental animals may not align with the specifications of commercially available contact lenses, thereby giving rise to fitting issues. While this issue is particularly conspicuous in mice and rats, the radius of anterior corneal curvature in the rabbit is also smaller than that in humans (7.0–7.5 mm vs 7.5–8.0 mm), emerging as a potential problem when contact lenses are required or recommended for post-injury interventions [22, 122]. Although noted amongst the alternative approaches for graft protection and fixation on the ocular surface, the use of fibrin glue has been observed to elicit pronounced ocular surface inflammation in rabbit eyes [121]. Alternatively, botulinum toxin may be used to produce iatrogenic upper eyelid ptosis for similar purposes [120].
Temporal Interval After LSCD Induction
An adequate temporal interval should be observed between the induction of the LSCD model and the implementation of the proposed intervention (e.g., stem cell therapy) as well as between the intervention and the endpoint for assessing treatment outcomes. While performing interventions very early after model creation may be technically and economically more feasible, it would yield limited translational value due to the substantial ocular surface inflammation typically observed during the initial weeks following injury [36]. Likewise, it is doubtful that a patient would undergo a surgical procedure involving any form of stem cell transplantation immediately following a severe ocular surface injury in a realistic clinical context. Equally important is the careful consideration of the timeframe between the intervention and the trial endpoint. This decision demands a delicate equilibrium, ensuring an adequate follow-up period for accurate assessment of treatment outcomes while avoiding unnecessarily prolonged follow-up durations that could result in increased costs and prolonged suffering.
Studies have demonstrated that signs of LSCD in rabbits begin to develop within the first 2–3 weeks after injury, while a full-blown picture of LSCD is documented within a timeframe spanning 1–3 months after the initial insult [13, 50, 93, 123,124,125,126]. A total LSCD develops slightly earlier in mice and rats, generally 1 to 2 months after the initial insult [13]. Hence, the time point at which LSCD is fully established should be taken into consideration for different species of animals when terminating the experiments for histological investigations or when initiating treatments.
Type of Anaesthesia
A commonly used anaesthesia combination, specifically xylazine and ketamine, has been demonstrated to lead to various ocular surface conditions in rodents, including prolonged inflammation, neovascularisation, corneal epithelial hyperplasia, and band keratopathy [127,128,129,130]. Notably, this occurrence has only been reported when the two anaesthetics were co-administered in rats and mice, and particularly when the exposure was during a juvenile period [129, 130]. The effects may be irreversible, and some rat species, such as Wistar, Long-Evans, and Fischer rats, may be more susceptible than others [131]. Although its precise mechanisms are not yet fully understood, this relatively underappreciated phenomenon merits attention, as certain findings bear a resemblance to those observed in LSCD and may, therefore, introduce artefactual complexities into the LSCD model. Potential strategies to circumvent this complication include the administration of yohimbine during either the induction or recovery phase of anaesthesia, dose titration of anaesthesia based on the age of the animal, utilisation of each anaesthetic as a single agent, or supplementation with 100% O2 during anaesthesia [129, 131, 132].
Reporting Adverse Events
Some of the adverse events that have been observed in relation to LSCD induction include corneal ulcers, infectious keratitis, endophthalmitis, corneal ectasia, corneal decompensation, hyphaemia, and hypopyon, all observed with much greater frequency in alkali LSCD models [67, 90, 113, 125]. Notably, Ma et al. had to exclude 29 rats out of a total sample of 80 due to severe hyphaemia, hypopyon, or perforation in an alkali model of LSCD [71]. However, adverse events and the exclusion of animals along with the reasons for exclusion have been rather underreported, appearing in only 12% of studies according to a recent systematic review on LSCD animal models [36]. Proper chronological documentation and reporting of adverse events is not only crucial for the validity and generalisability of a study, but it is also essential for providing guidance to other researchers in the field.
Future Directions and Suggestions for an Optimal Animal Model of Total LSCD
Unresolved questions that are key to an optimal animal model for total LSCD include the extent to which animal models can faithfully recapitulate real-life scenarios, the level of precision associated with current biomarkers used for LSCD validation, and the accuracy of animal models in assessing the effectiveness and safety of prospective treatment modalities intended for human application. An optimal animal model for LSCD research should ideally prioritise reproducibility and controllability while minimising damage to other anterior and posterior segment structures. It should at the same time incur sufficient damage to induce total LSCD without leading to partial injury and subsequent spontaneous healing. Likewise, it should aim to cause as little unwarranted harm and complications as possible, thereby minimising animal dropout and suffering. For ethical considerations, it is standard practice to incur damage in only one eye of the animal; however, it should be kept in mind that the contralateral untreated control eye may also exhibit secondary pathological changes, a phenomenon documented in mouse and rabbit eyes [62, 133].
With regard to animal selection, the use of mouse and rat animal models may be more feasible in exploring biological mechanisms related to LSCD, considering the availability of a wide array of analytical reagents and kits for these animal species (Fig. 3). In contrast, rabbit models may be better suited to studies in which the aim is to test a treatment modality intended for human application, particularly those involving biomedical devices.
In light of recent evidence regarding the presence of corneal-committed cells on the corneal surface, it is advisable that the inflicted injury in experimental models not be confined solely to the limbus but instead involve the entirety of the corneal epithelium as well (Fig. 3) [46, 47]. Removal of the corneal epithelium in addition to obliteration of the limbal stroma ensures the induction of total LSCD, precluding the possibility of these stem cells dedifferentiating and repopulating the limbal niche [109]. It is also worth noting that methods targeting the corneal surface exclusively without any impact on the limbus will yield only partial or no LSCD, a condition that is likely to heal spontaneously, even in the absence of any treatment.
One should be aware that different methods of LSCD induction may yield distinct biological responses, an important consideration when assessing the translational value of a study. Specifically, methods that involve the use of alkalis lead to a more pronounced inflammatory response and neovascularisation, making this method a suitable means for studies on neovascularisation-related aspects of LSCD [45]. On the other hand, mechanical removal of the limbus inflicts minor damage to the corneal matrix, thereby making it a valuable model for studies focused on investigating the behaviour of implanted stem cells on the corneal surface along with their therapeutic efficacy [45]. Conversely, thermal injury may lead to more scarring than mechanical or chemical injury, providing an avenue for investigation of antifibrotic treatments (Fig. 3) [38]. Because each method comes with its unique advantages and disadvantages, it is of paramount importance to consider primary research objectives when choosing the optimal animal and method for LSCD induction.
A precise definition for successful induction of LSCD in animal research is essential, but a universal definition is currently nonexistent. Establishing a robust LSCD definition that could be used in animal LSCD research entails the utilisation of various adjunctive tests that are currently in use in the clinics, such as impression cytology and imaging (e.g., IVCM). These methods not only can assist in establishing the diagnosis of LSCD in animal models, but also can prove useful in staging the severity of the damage. Notably, a recent systematic review on the translational relevance of animal models for LSCD demonstrated that impression cytology and in vivo imaging have been significantly underutilised, appearing in the study protocol of only 13% and 5% of the indexed studies, respectively [36]. Although these methods may not be sensitive enough for definitive LSCD diagnosis, they may prove instrumental in better characterising LSCD, documenting disease evolution, and evaluating the response to therapy [36].
The complex and multifaceted nature of LSCD presents a significant challenge in the realm of preclinical animal studies. As such, an ideal animal model that can be applied universally for investigating every aspect of LSCD is lacking. Furthermore, every model, whether induced by alkali exposure, surgical techniques, or other means, has its own set of limitations and advantages. Consequently, the absence of a universal and clinically relevant animal model underscores the urgent need for further extensive research in this domain to address this unmet need.
References
Osei-Bempong C, Figueiredo FC, Lako M. The limbal epithelium of the eye–a review of limbal stem cell biology, disease and treatment. BioEssays. 2013;35(3):211–9.
Le Q, Xu J, Deng SX. The diagnosis of limbal stem cell deficiency. Ocul Surf. 2018;16(1):58–69.
Sun Y, Yung M, Huang L, Tseng C, Deng SX. Limbal stem cell deficiency after glaucoma surgery. Cornea. 2020;39(5):566–72.
Bobba S, Di Girolamo N, Mills R, Daniell M, Chan E, Harkin DG, et al. Nature and incidence of severe limbal stem cell deficiency in Australia and New Zealand. Clin Exp Ophthalmol. 2017;45(2):174–81.
Shortt AJ, Tuft SJ, Daniels JT. Corneal stem cells in the eye clinic. Br Med Bull. 2011;100:209–25.
Vazirani J, Nair D, Shanbhag S, Wurity S, Ranjan A, Sangwan V. Limbal stem cell deficiency-demography and underlying causes. Am J Ophthalmol. 2018;188:99–103.
Ahmmed AA, Ting DSJ, Figueiredo FC. Epidemiology, economic and humanistic burdens of ocular surface chemical injury: a narrative review. Ocul Surf. 2021;20:199–211.
Ghareeb AE, Lako M, Figueiredo FC. Recent advances in stem cell therapy for limbal stem cell deficiency: a narrative review. Ophthalmol Therapy. 2020;9(4):809–31.
Huang W, Tourmouzis K, Perry H, Honkanen RA, Rigas B. Animal models of dry eye disease: useful, varied and evolving (review). Exp Ther Med. 2021;22(6):1394.
Henriksson JT, McDermott AM, Bergmanson JP. Dimensions and morphology of the cornea in three strains of mice. Invest Ophthalmol Vis Sci. 2009;50(8):3648–54.
Howell GR, Libby RT, John SW. Mouse genetic models: an ideal system for understanding glaucomatous neurodegeneration and neuroprotection. Prog Brain Res. 2008;173:303–21.
Stepp MA, Zieske JD, Trinkaus-Randall V, Kyne BM, Pal-Ghosh S, Tadvalkar G, et al. Wounding the cornea to learn how it heals. Exp Eye Res. 2014;121:178–93.
Kethiri AR, Raju E, Bokara KK, Mishra DK, Basu S, Rao CM, et al. Inflammation, vascularization and goblet cell differences in LSCD: validating animal models of corneal alkali burns. Exp Eye Res. 2019;185: 107665.
Grieve K, Ghoubay D, Georgeon C, Thouvenin O, Bouheraoua N, Paques M, et al. Three-dimensional structure of the mammalian limbal stem cell niche. Exp Eye Res. 2015;140:75–84.
Li J, Xiao Y, Coursey TG, Chen X, Deng R, Lu F, et al. Identification for differential localization of putative corneal epithelial stem cells in mouse and human. Sci Rep. 2017;7(1):5169.
Majo F, Rochat A, Nicolas M, Jaoude GA, Barrandon Y. Oligopotent stem cells are distributed throughout the mammalian ocular surface. Nature. 2008;456(7219):250–4.
Pal-Ghosh S, Tadvalkar G, Jurjus RA, Zieske JD, Stepp MA. BALB/c and C57BL6 mouse strains vary in their ability to heal corneal epithelial debridement wounds. Exp Eye Res. 2008;87(5):478–86.
Li W, Li Q, Wang W, Li K, Ling S, Yang Y, et al. A rat model of autologous oral mucosal epithelial transplantation for corneal limbal stem cell failure. Eye Sci. 2014;29(1):1–5.
Li W, Hayashida Y, Chen YT, Tseng SC. Niche regulation of corneal epithelial stem cells at the limbus. Cell Res. 2007;17(1):26–36.
Umemoto T, Yamato M, Nishida K, Kohno C, Yang J, Tano Y, et al. Rat limbal epithelial side population cells exhibit a distinct expression of stem cell markers that are lacking in side population cells from the central cornea. FEBS Lett. 2005;579(29):6569–74.
Wolosin J, Akinci M, Taveras M, Turner H. Intraepithelial lymphocytes are a major component of ocular surface epithelial side populations. Invest Ophth Vis Sci. 2006;47(13):3954.
Gwon A. Chapter 13—the rabbit in cataract/IOL surgery. In: Tsonis PA, editor. Animal models in eye research. London: Academic Press; 2008. p. 184–204.
Peiffer RL, Pohm-Thorsen L, Corcoran K. CHAPTER 19—models in ophthalmology and vision research**supported in part by a grant from research to prevent blindness and the North Carolina Lions Foundation. In: Manning PJ, Ringler DH, Newcomer CE, editors. The biology of the laboratory rabbit. 2nd ed. San Diego: Academic Press; 1994. p. 409–33.
Ti SE, Anderson D, Touhami A, Kim C, Tseng SC. Factors affecting outcome following transplantation of ex vivo expanded limbal epithelium on amniotic membrane for total limbal deficiency in rabbits. Invest Ophthalmol Vis Sci. 2002;43(8):2584–92.
Kadar T, Horwitz V, Cohen M, Egoz I, Gutman H, Gez R, et al. Limbal stem cell deficiency (LSCD) in rats and mice following whole body exposure to sulfur mustard (SM) vapor. Exp Eye Res. 2022;223: 109195.
Li Y, Yang Y, Yang L, Zeng Y, Gao X, Xu H. Poly(ethylene glycol)-modified silk fibroin membrane as a carrier for limbal epithelial stem cell transplantation in a rabbit LSCD model. Stem Cell Res Ther. 2017;8(1):256.
Borkowski R, Karas AZ. Sedation and anesthesia of pet rabbits. Clin Tech Small Anim Pract. 1999;14(1):44–9.
Adil MT, Henry JJ. Understanding cornea epithelial stem cells and stem cell deficiency: lessons learned using vertebrate model systems. Genesis. 2021;59(1–2): e23411.
Adil MT, Simons CM, Sonam S, Henry JJ. Understanding cornea homeostasis and wound healing using a novel model of stem cell deficiency in Xenopus. Exp Eye Res. 2019;187: 107767.
Zeiss CJ. Translational models of ocular disease. Vet Ophthalmol. 2013;16(Suppl 1):15–33.
Yang X, Moldovan NI, Zhao Q, Mi S, Zhou Z, Chen D, et al. Reconstruction of damaged cornea by autologous transplantation of epidermal adult stem cells. Mol Vis. 2008;14:1064–70.
Zhang P, Ma XY, Huang DT, Yang XY. The capacity of goat epidermal adult stem cells to reconstruct the damaged ocular surface of total LSCD and activate corneal genetic programs. J Mol Histol. 2020;51(3):277–86.
Mi S, Yang X, Zhao Q, Qu L, Chen S, Meek KM, et al. Reconstruction of corneal epithelium with cryopreserved corneal limbal stem cells in a goat model. Mol Reprod Dev. 2008;75(11):1607–16.
Yin JQ, Liu WQ, Liu C, Zhang YH, Hua JL, Liu WS, et al. Reconstruction of damaged corneal epithelium using Venus-labeled limbal epithelial stem cells and tracking of surviving donor cells. Exp Eye Res. 2013;115:246–54.
Valdez-Garcia JE, Lozano-Ramirez JF, Zavala J. Adult white New Zealand rabbit as suitable model for corneal endothelial engineering. BMC Res Notes. 2015;8:28.
Delic NC, Cai JR, Watson SL, Downie LE, Di Girolamo N. Evaluating the clinical translational relevance of animal models for limbal stem cell deficiency: a systematic review. Ocul Surf. 2022;23:169–83.
Amirjamshidi H, Milani BY, Sagha HM, Movahedan A, Shafiq MA, Lavker RM, et al. Limbal fibroblast conditioned media: a non-invasive treatment for limbal stem cell deficiency. Mol Vis. 2011;17:658–66.
Afsharkhamseh N, Movahedan A, Gidfar S, Huvard M, Wasielewski L, Milani BY, et al. Stability of limbal stem cell deficiency after mechanical and thermal injuries in mice. Exp Eye Res. 2016;145:88–92.
Sta Iglesia DD, Stepp MA. Disruption of the basement membrane after corneal debridement. Invest Ophthalmol Vis Sci. 2000;41(5):1045–53.
Pal-Ghosh S, Pajoohesh-Ganji A, Tadvalkar G, Stepp MA. Removal of the basement membrane enhances corneal wound healing. Exp Eye Res. 2011;93(6):927–36.
Kruse FE, Chen JJ, Tsai RJ, Tseng SC. Conjunctival transdifferentiation is due to the incomplete removal of limbal basal epithelium. Invest Ophthalmol Vis Sci. 1990;31(9):1903–13.
Bardag-Gorce F, Oliva J, Wood A, Hoft R, Pan D, Thropay J, et al. Carrier-free cultured autologous oral mucosa epithelial cell sheet (CAOMECS) for corneal epithelium reconstruction: a histological study. Ocul Surf. 2015;13(2):150–63.
Zhao M, Zhang H, Zhen D, Huang M, Li W, Li Z, et al. Corneal recovery following rabbit peripheral blood mononuclear cell-amniotic membrane transplantation with antivascular endothelial growth factor in limbal stem cell deficiency rabbits. Tissue Eng Part C Methods. 2020;26(10):541–52.
Li FJ, Nili E, Lau C, Richardson NA, Walshe J, Barnett NL, et al. Evaluation of the AlgerBrush II rotating burr as a tool for inducing ocular surface failure in the New Zealand White rabbit. Exp Eye Res. 2016;147:1–11.
Zhang H, Lin S, Zhang M, Li Q, Li W, Wang W, et al. Comparison of two rabbit models with deficiency of corneal epithelium and limbal stem cells established by different methods. Tissue Eng Part C Methods. 2017;23(11):710–7.
Huang AJ, Tseng SC. Corneal epithelial wound healing in the absence of limbal epithelium. Invest Ophthalmol Vis Sci. 1991;32(1):96–105.
Nasser W, Amitai-Lange A, Soteriou D, Hanna R, Tiosano B, Fuchs Y, et al. Corneal-committed cells restore the stem cell pool and tissue boundary following injury. Cell Rep. 2018;22(2):323–31.
Ma DH, Chen JK, Zhang F, Lin KY, Yao JY, Yu JS. Regulation of corneal angiogenesis in limbal stem cell deficiency. Prog Retin Eye Res. 2006;25(6):563–90.
Lee HJ, Nam SM, Choi SK, Seo KY, Kim HO, Chung SH. Comparative study of substrate free and amniotic membrane scaffolds for cultivation of limbal epithelial sheet. Sci Rep. 2018;8(1):14628.
Chae JJ, Ambrose WM, Espinoza FA, Mulreany DG, Ng S, Takezawa T, et al. Regeneration of corneal epithelium utilizing a collagen vitrigel membrane in rabbit models for corneal stromal wound and limbal stem cell deficiency. Acta Ophthalmol. 2015;93(1):e57-66.
Kethiri AR, Singh VK, Damala M, Basu S, Rao CM, Bokara KK, et al. Long term observation of ocular surface alkali burn in rabbit models: quantitative analysis of corneal haze, vascularity and self-recovery. Exp Eye Res. 2021;205: 108526.
Afsharkhamseh N, Ghahari E, Eslani M, Djalilian AR. A simple mechanical procedure to create limbal stem cell deficiency in mouse. J Vis Exp. 2016;117: e54658.
Ksander BR, Kolovou PE, Wilson BJ, Saab KR, Guo Q, Ma J, et al. ABCB5 is a limbal stem cell gene required for corneal development and repair. Nature. 2014;511(7509):353–7.
Meyer-Blazejewska EA, Call MK, Yamanaka O, Liu H, Schlotzer-Schrehardt U, Kruse FE, et al. From hair to cornea: toward the therapeutic use of hair follicle-derived stem cells in the treatment of limbal stem cell deficiency. Stem Cells. 2011;29(1):57–66.
Puri S, Sun M, Mutoji KN, Gesteira TF, Coulson-Thomas VJ. Epithelial cell migration and proliferation patterns during initial wound closure in normal mice and an experimental model of limbal stem cell deficiency. Invest Ophthalmol Vis Sci. 2020;61(10):27.
Richardson A, Park M, Watson SL, Wakefield D, Di Girolamo N. Visualizing the fate of transplanted K14-confetti corneal epithelia in a mouse model of limbal stem cell deficiency. Invest Ophthalmol Vis Sci. 2018;59(3):1630–40.
Gao X, Guo K, Santosa SM, Montana M, Yamakawa M, Hallak JA, et al. Application of corneal injury models in dual fluorescent reporter transgenic mice to understand the roles of the cornea and limbus in angiogenic and lymphangiogenic privilege. Sci Rep. 2019;9(1):12331.
Boote C, Du Y, Morgan S, Harris J, Kamma-Lorger CS, Hayes S, et al. Quantitative assessment of ultrastructure and light scatter in mouse corneal debridement wounds. Invest Ophthalmol Vis Sci. 2012;53(6):2786–95.
Gong D, Yan C, Yu F, Yan D, Wu N, Chen L, et al. Direct oral mucosal epithelial transplantation supplies stem cells and promotes corneal wound healing to treat refractory persistent corneal epithelial defects. Exp Eye Res. 2022;215: 108934.
Sampaio LP, Hilgert GSL, Shiju TM, Santhiago MR, Wilson SE. Topical losartan and corticosteroid additively inhibit corneal stromal myofibroblast generation and scarring fibrosis after alkali burn injury. Transl Vis Sci Technol. 2022;11(7):9.
Wang Y, Gao G, Wu Y, Wang Y, Wu X, Zhou Q. S100A4 silencing Facilitates corneal wound healing after alkali burns by promoting autophagy via blocking the PI3K/Akt/mTOR signaling pathway. Invest Ophthalmol Vis Sci. 2020;61(11):19.
Ishizaki M, Zhu G, Haseba T, Shafer SS, Kao WW. Expression of collagen I, smooth muscle alpha-actin, and vimentin during the healing of alkali-burned and lacerated corneas. Invest Ophthalmol Vis Sci. 1993;34(12):3320–8.
Tripathi R, Giuliano EA, Gafen HB, Gupta S, Martin LM, Sinha PR, et al. Is sex a biological variable in corneal wound healing? Exp Eye Res. 2019;187: 107705.
Xiang J, Sun J, Hong J, Wang W, Wei A, Le Q, et al. T-style keratoprosthesis based on surface-modified poly (2-hydroxyethyl methacrylate) hydrogel for cornea repairs. Mater Sci Eng C Mater Biol Appl. 2015;50:274–85.
Gu S, Xing C, Han J, Tso MO, Hong J. Differentiation of rabbit bone marrow mesenchymal stem cells into corneal epithelial cells in vivo and ex vivo. Mol Vis. 2009;15:99–107.
Kobashigawa KK, Aldrovani M, Barros Sobrinho AAF, Silva P, Marcusso PF, Marinho-Neto FA, et al. Clinical features and corneal optical anisotropies in a rabbit model of limbal stem cell deficiency. Arq Bras Oftalmol. 2018;81(5):384–92.
Zhu J, Zhang K, Sun Y, Gao X, Li Y, Chen Z, et al. Reconstruction of functional ocular surface by acellular porcine cornea matrix scaffold and limbal stem cells derived from human embryonic stem cells. Tissue Eng Part A. 2013;19(21–22):2412–25.
Sanie-Jahromi F, Eghtedari M, Mirzaei E, Jalalpour MH, Asvar Z, Nejabat M, et al. Propagation of limbal stem cells on polycaprolactone and polycaprolactone/gelatin fibrous scaffolds and transplantation in animal model. Bioimpacts. 2020;10(1):45–54.
Du Y, Chen J, Funderburgh JL, Zhu X, Li L. Functional reconstruction of rabbit corneal epithelium by human limbal cells cultured on amniotic membrane. Mol Vis. 2003;9:635–43.
Jiang TS, Cai L, Ji WY, Hui YN, Wang YS, Hu D, et al. Reconstruction of the corneal epithelium with induced marrow mesenchymal stem cells in rats. Mol Vis. 2010;16:1304–16.
Ma Y, Xu Y, Xiao Z, Yang W, Zhang C, Song E, et al. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24(2):315–21.
Shadmani A, Razmkhah M, Jalalpoor MH, Lari SY, Eghtedari M. Autologous activated omental versus allogeneic adipose tissue-derived mesenchymal stem cells in corneal alkaline injury: an experimental study. J Curr Ophthalmol. 2021;33(2):136–42.
Bu P, Vin AP, Sethupathi P, Ambrecht LA, Zhai Y, Nikolic N, et al. Effects of activated omental cells on rat limbal corneal alkali injury. Exp Eye Res. 2014;121:143–6.
Rohaina CM, Then KY, Ng AM, Wan-Abdul-Halim WH, Zahidin AZ, Saim A, et al. Reconstruction of limbal stem cell deficient corneal surface with induced human bone marrow mesenchymal stem cells on amniotic membrane. Transl Res. 2014;163(3):200–10.
Bandeira F, Goh TW, Setiawan M, Yam GH, Mehta JS. Cellular therapy of corneal epithelial defect by adipose mesenchymal stem cell-derived epithelial progenitors. Stem Cell Res Ther. 2020;11(1):14.
Xiao YT, Xie HT, Liu X, Duan CY, Qu JY, Zhang MC, et al. Subconjunctival injection of transdifferentiated oral mucosal epithelial cells for limbal stem cell deficiency in rats. J Histochem Cytochem. 2021;69(3):177–90.
Di GH, Qi X, Xu J, Yu CQ, Cao QL, Xing ZJ, et al. Therapeutic effect of secretome from TNF-alpha stimulated mesenchymal stem cells in an experimental model of corneal limbal stem cell deficiency. Int J Ophthalmol. 2021;14(2):179–85.
Lin KJ, Loi MX, Lien GS, Cheng CF, Pao HY, Chang YC, et al. Topical administration of orbital fat-derived stem cells promotes corneal tissue regeneration. Stem Cell Res Ther. 2013;4(3):72.
Hong H, Huh MI, Park SM, Lee KP, Kim HK, Kim DS. Decellularized corneal lenticule embedded compressed collagen: toward a suturable collagenous construct for limbal reconstruction. Biofabrication. 2018;10(4): 045001.
Tananuvat N, Bumroongkit K, Tocharusa C, Mevatee U, Kongkaew A, Ausayakhun S. Limbal stem cell and oral mucosal epithelial transplantation from ex vivo cultivation in LSCD-induced rabbits: histology and immunologic study of the transplant epithelial sheet. Int Ophthalmol. 2017;37(6):1289–98.
Swarup A, Grosskopf AK, Stapleton LM, Subramaniam VR, Li B, Weissman IL, et al. PNP hydrogel prevents formation of symblephara in mice after ocular alkali injury. Transl Vis Sci Technol. 2022;11(2):31.
Shadmani A, Dhowre HS, Ercal O, Meng XQ, Wu AY. Corneal and limbal alkali injury induction using a punch-trephine technique in a mouse model. J Vis Exp. 2023. https://doi.org/10.3791/65609.
Schultz GS, Strelow S, Stern GA, Chegini N, Grant MB, Galardy RE, et al. Treatment of alkali-injured rabbit corneas with a synthetic inhibitor of matrix metalloproteinases. Invest Ophthalmol Vis Sci. 1992;33(12):3325–31.
Zuk M, Lobashova E, Zuk O, Wierzba S. Efficacy of systemic administration of riboflavin on a rabbit model of corneal alkali burn. Sci Rep. 2020;10(1):17278.
Holan V, Trosan P, Cejka C, Javorkova E, Zajicova A, Hermankova B, et al. A comparative study of the therapeutic potential of mesenchymal stem cells and limbal epithelial stem cells for ocular surface reconstruction. Stem Cells Transl Med. 2015;4(9):1052–63.
Moore JE, McMullen TC, Campbell IL, Rohan R, Kaji Y, Afshari NA, et al. The inflammatory milieu associated with conjunctivalized cornea and its alteration with IL-1 RA gene therapy. Invest Ophthalmol Vis Sci. 2002;43(9):2905–15.
Gulias-Canizo R, Lagunes-Guillen A, Gonzalez-Robles A, Sanchez-Guzman E, Castro-Munozledo F. (−)-Epigallocatechin-3-gallate, reduces corneal damage secondary from experimental grade II alkali burns in mice. Burns. 2019;45(2):398–412.
Uchiyama M, Shimizu A, Masuda Y, Nagasaka S, Fukuda Y, Takahashi H. An ophthalmic solution of a peroxisome proliferator-activated receptor gamma agonist prevents corneal inflammation in a rat alkali burn model. Mol Vis. 2013;19:2135–50.
Sprogyte L, Park M, Di Girolamo N. Pathogenesis of alkali injury-induced limbal stem cell deficiency: a literature survey of animal models. Cells. 2023;12(9):1294.
Magalhaes OA, de Alcantara RJA, Gomes JAP, Caiado-de-Castro-Neto J, Schor P. Titanium powder 3D-printing technology for a novel keratoprosthesis in alkali-burned rabbits. Transl Vis Sci Technol. 2022;11(8):14.
Gu C, Ni T, Verter EE, Redmond RW, Kochevar IE, Yao M. Photochemical tissue bonding: a potential strategy for treating limbal stem cell deficiency. Lasers Surg Med. 2011;43(5):433–42.
Gomes JA, Geraldes Monteiro B, Melo GB, Smith RL, Cavenaghi-Pereira-da-Silva M, Lizier NF, et al. Corneal reconstruction with tissue-engineered cell sheets composed of human immature dental pulp stem cells. Invest Ophthalmol Vis Sci. 2010;51(3):1408–14.
Villabona-Martinez V, Sampaio LP, Shiju TM, Wilson SE. Standardization of corneal alkali burn methodology in rabbits. Exp Eye Res. 2023;230: 109443.
Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995;14(5):473–84.
Sugiyama H, Yamato M, Nishida K, Okano T. Evidence of the survival of ectopically transplanted oral mucosal epithelial stem cells after repeated wounding of cornea. Mol Ther. 2014;22(8):1544–55.
Espana EM, Ti SE, Grueterich M, Touhami A, Tseng SC. Corneal stromal changes following reconstruction by ex vivo expanded limbal epithelial cells in rabbits with total limbal stem cell deficiency. Br J Ophthalmol. 2003;87(12):1509–14.
Qiu T, Cui L, Xu JJ, Hong JX, Xiang J. Reconstruction of the ocular surface by autologous transplantation of rabbit adipose tissue-derived stem cells on amniotic membrane. Ann Transl Med. 2020;8(17):1062.
Reinshagen H, Auw-Haedrich C, Sorg RV, Boehringer D, Eberwein P, Schwartzkopff J, et al. Corneal surface reconstruction using adult mesenchymal stem cells in experimental limbal stem cell deficiency in rabbits. Acta Ophthalmol. 2011;89(8):741–8.
Kadar T, Amir A, Cohen L, Cohen M, Sahar R, Gutman H, et al. Anti-VEGF therapy (bevacizumab) for sulfur mustard-induced corneal neovascularization associated with delayed limbal stem cell deficiency in rabbits. Curr Eye Res. 2014;39(5):439–50.
Kadar T, Dachir S, Cohen L, Sahar R, Fishbine E, Cohen M, et al. Ocular injuries following sulfur mustard exposure–pathological mechanism and potential therapy. Toxicology. 2009;263(1):59–69.
Kadar T, Dachir S, Cohen M, Gutman H, Cohen L, Brandeis R, et al. Prolonged impairment of corneal innervation after exposure to sulfur mustard and its relation to the development of delayed limbal stem cell deficiency. Cornea. 2013;32(4):e44-50.
Dachir S, Rabinovitz I, Yaacov G, Gutman H, Cohen L, Horwitz V, et al. Whole body exposure of rats to sulfur mustard vapor. Drug Chem Toxicol. 2019;42(3):231–42.
Kadar T, Horwitz V, Sahar R, Cohen M, Cohen L, Gez R, et al. Delayed loss of corneal epithelial stem cells in a chemical injury model associated with limbal stem cell deficiency in rabbits. Curr Eye Res. 2011;36(12):1098–107.
Cimino GD, Gamper HB, Isaacs ST, Hearst JE. Psoralens as photoactive probes of nucleic acid structure and function: organic chemistry, photochemistry, and biochemistry. Annu Rev Biochem. 1985;54:1151–93.
Das P, Pereira JA, Chaklader M, Law A, Bagchi K, Bhaduri G, et al. Phenotypic alteration of limbal niche-associated limbal epithelial stem cell deficiency by ultraviolet-B exposure-induced phototoxicity in mice. Biochem Cell Biol. 2013;91(3):165–75.
Cejka C, Luyckx J, Cejkova J. Central corneal thickness considered an index of corneal hydration of the UVB irradiated rabbit cornea as influenced by UVB absorber. Physiol Res. 2012;61(3):299–306.
Lin Z, He H, Zhou T, Liu X, Wang Y, He H, et al. A mouse model of limbal stem cell deficiency induced by topical medication with the preservative benzalkonium chloride. Invest Ophthalmol Vis Sci. 2013;54(9):6314–25.
Ramaesh K, Ramaesh T, Dutton GN, Dhillon B. Evolving concepts on the pathogenic mechanisms of aniridia related keratopathy. Int J Biochem Cell Biol. 2005;37(3):547–57.
Latta L, Figueiredo FC, Ashery-Padan R, Collinson JM, Daniels J, Ferrari S, et al. Pathophysiology of aniridia-associated keratopathy: developmental aspects and unanswered questions. Ocul Surf. 2021;22:245–66.
Wang H, Han J, Hu F, Zhang C, Zhao K, Mu N, et al. Novel animal model of limbal stem cell deficiency induced by forcing eye-open at birth. Cornea. 2023;42(7):874–87.
Deng SX, Borderie V, Chan CC, Dana R, Figueiredo FC, Gomes JAP, et al. Global consensus on definition, classification, diagnosis, and staging of limbal stem cell deficiency. Cornea. 2019;38(3):364–75.
Sonoda Y, Streilein JW. Orthotopic corneal transplantation in mice–evidence that the immunogenetic rules of rejection do not apply. Transplantation. 1992;54(4):694–704.
Luengo Gimeno F, Lavigne V, Gatto S, Croxatto JO, Correa L, Gallo JE. Advances in corneal stem-cell transplantation in rabbits with severe ocular alkali burns. J Cataract Refract Surg. 2007;33(11):1958–65.
Park M, Mazalo J, Di Girolamo N. Insulin-like growth factor binding protein-7: a marker of conjunctivalization in an animal model of limbal stem cell deficiency. Ocul Surf. 2019;17(3):447–57.
Di Iorio E, Ferrari S, Fasolo A, Bohm E, Ponzin D, Barbaro V. Techniques for culture and assessment of limbal stem cell grafts. Ocul Surf. 2010;8(3):146–53.
Donisi PM, Rama P, Fasolo A, Ponzin D. Analysis of limbal stem cell deficiency by corneal impression cytology. Cornea. 2003;22(6):533–8.
Binotti WW, Nose RM, Koseoglu ND, Dieckmann GM, Kenyon K, Hamrah P. The utility of anterior segment optical coherence tomography angiography for the assessment of limbal stem cell deficiency. Ocul Surf. 2021;19:94–103.
Wang SB, Hu KM, Seamon KJ, Mani V, Chen Y, Gronert K. Estrogen negatively regulates epithelial wound healing and protective lipid mediator circuits in the cornea. FASEB J. 2012;26(4):1506–16.
Lidster K, Owen K, Browne WJ, Prescott MJ. Cage aggression in group-housed laboratory male mice: an international data crowdsourcing project. Sci Rep. 2019;9(1):15211.
Brown C. Temporary tarsorrhaphy in the rat. Lab Anim (NY). 2007;36(1):25–6.
Inamochi A, Tomioka A, Kitamoto K, Miyai T, Usui T, Aihara M, et al. Simple oral mucosal epithelial transplantation in a rabbit model. Sci Rep. 2019;9(1):18088.
Brown KD, Low S, Mariappan I, Abberton KM, Short R, Zhang H, et al. Plasma polymer-coated contact lenses for the culture and transfer of corneal epithelial cells in the treatment of limbal stem cell deficiency. Tissue Eng Part A. 2014;20(3–4):646–55.
Lee H, Lee JH, Hong S, Sunwoo JH, Kim HT, Kim ES, et al. Transplantation of human corneal limbal epithelial cell sheet harvested on synthesized carboxymethyl cellulose and dopamine in a limbal stem cell deficiency. J Tissue Eng Regen Med. 2021;15(2):139–49.
Hyun DW, Kim YH, Koh AY, Lee HJ, Wee WR, Jeon S, et al. Characterization of biomaterial-free cell sheets cultured from human oral mucosal epithelial cells. J Tissue Eng Regen Med. 2017;11(3):743–50.
Luengo Gimeno F, Lavigne V, Gatto S, Croxatto JO, Correa L, Gallo JE. One-year follow-up of epithelial corneal cell sheet allografts mounted on platelet poor plasma in rabbits. Mol Vis. 2009;15:2771–9.
Galindo S, Herreras JM, Lopez-Paniagua M, Rey E, de la Mata A, Plata-Cordero M, et al. Therapeutic effect of human adipose tissue-derived mesenchymal stem cells in experimental corneal failure due to limbal stem cell niche damage. Stem Cells. 2017;35(10):2160–74.
Zwick LS, Patrick DJ, Knupp LC, Ramos MF. Ketamine/xylazine anesthesia-related corneal lesions in rats with surgically implanted venous catheters utilized in nonclinical intravenous studies. Toxicol Pathol. 2021;49(3):598–601.
Tita B, Leone MG, Casini ML, Corubolo C, Bordi F, Guidolin D, et al. Corneal toxicity of xylazine and clonidine, in combination with ketamine, in the rat. Ophthalmic Res. 2001;33(6):345–52.
Guillet R, Wyatt J, Baggs RB, Kellogg CK. Anesthetic-induced corneal lesions in developmentally sensitive rats. Invest Ophthalmol Vis Sci. 1988;29(6):949–54.
Koehn D, Meyer KJ, Syed NA, Anderson MG. Ketamine/xylazine-induced corneal damage in mice. PLoS ONE. 2015;10(7): e0132804.
Turner PV, Albassam MA. Susceptibility of rats to corneal lesions after injectable anesthesia. Comp Med. 2005;55(2):175–82.
Zhou TE, Sayah DN, Noueihed B, Mazzaferri J, Costantino S, Brunette I, et al. Preventing corneal calcification associated with xylazine for longitudinal optical coherence tomography in young rodents. Invest Ophthalmol Vis Sci. 2017;58(1):461–9.
Lam WL, Chow PH, Chik KP, Yew DT. Bilateral biochemical and biophysical retinal changes after unilateral ocular trauma in the mouse. Neurosci Lett. 1996;218(1):1–4.
Funding
The authors acknowledge the support from the Scientific and Technological Research Council of Türkiye (TÜBİTAK Grant ID: 123S073) and Fight for Sight UK (5181/5182). No funding or sponsorship was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
Initiative: Eray Atalay, Francisco Figueiredo; Literature search: Eray Atalay, Burcugül Altuğ; Writing—Original draft preparation: Eray Atalay, Burcugül Altuğ, Mert Egemen Çalışkan, Semih Ceylan, Zeynep Serra Özler; Writing—Review and editing: Gustavo Figueiredo, Majlinda Lako, Francisco Figueiredo.
Corresponding author
Ethics declarations
Conflict of Interest
Eray Atalay, Burcugül Altuğ, Mert Egemen Çalışkan, Semih Ceylan, Zeynep Serra Özler, Gustavo Figueiredo, Majlinda Lako and Francisco Figueiredo declare that they have no competing interests.
Ethical Approval
This critical narrative literature review article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Atalay, E., Altuğ, B., Çalışkan, M.E. et al. Animal Models for Limbal Stem Cell Deficiency: A Critical Narrative Literature Review. Ophthalmol Ther 13, 671–696 (2024). https://doi.org/10.1007/s40123-023-00880-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00880-0