Abstract
Introduction
Allogeneic serum from blood donors is starting to be used to treat patients with dry eye disease (DED). However, the optimal dose is not known. We therefore aimed to evaluate the clinical efficaciousness and user-friendliness of micro-sized versus conventional-sized allogeneic serum eye drops (SEDs).
Methods
In a randomized trial, patients with DED first receive micro-sized SEDs (7 µl/unit) for 1 month, followed by a 1-month washout, before receiving conventional-sized SEDs (50 µl/unit) for 1 month; or vice versa. The primary endpoint was the Ocular Surface Disease Index (OSDI) score. Secondary endpoints were tear break-up time (TBT), tear production (TP), and presence of corneal punctate lesions (CP). The user-friendliness of both application systems was also compared. A linear mixed model for cross-over design was applied to compare both treatments.
Results
Forty-nine patients completed the trial. The mean OSDI score significantly improved from 52 ± 3 to 41 ± 3 for micro-sized SEDs, and from 54 ± 3 to 45 ± 3 for conventional-sized SEDs. Non-inferiority (margin = 6) of micro-sized SEDs was established. We demonstrate a significant improvement for TBT in case of conventional-sized SEDs and for CP in both treatment groups. TP trended towards an improvement in both treatment groups. The user-friendliness of the conventional drop system was significantly higher.
Conclusions
For the first time, non-inferiority of micro-sized allogeneic SEDs was established. The beneficial effect of both SED volumes was similar as measured by the OSDI score. Although user-friendliness of the micro drop system was significantly lower, it is an attractive alternative as it saves valuable donor serum.
Trial Registration
ClinicalTrials.gov (NCT03539159).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Clinical data on the efficacy of allogeneic serum eye drops (SEDs) is scarce and shows heterogeneous responses for the subjective Ocular Surface Disease Index (OSDI) score. Our study was performed in a large cohort and shows both objective and subjective improvements. |
No literature is available on how much serum is needed to achieve a measurable effect. We demonstrate that as little as 7 µl is sufficient. |
What was learned from the study? |
For the first time, we show in a large group of almost 50 naïve patients with dry eye disease (DED) that a large subjective improvement was observed for both drop sizes (OSDI), but notably, a significant objective improvement (tear break-up time, corneal punctate lesions, tear production). |
Micro-sized and conventional-sized SEDs show similar clinical efficacy. However, due to its smaller drop size, the micro drop system uses less serum and is therefore an attractive system, as it saves valuable donor serum. |
Introduction
Allogeneic serum eye drops (SEDs), which are obtained from donor serum, are increasingly being used to treat patients with dry eye disease (DED). Until now, autologous SEDs have mostly been used, but have a number of hindrances with respect to collection, production, and standardization [1, 2]. From a clinical perspective, the definition of DED, as formulated by global DED experts is: “Dry eye disease is a multifactorial disease characterized by a persistently unstable and/or deficient tear film causing discomfort and/or visual impairment, accompanied by variable degrees of ocular surface epitheliopathy, inflammation, and neurosensory abnormalities” [3].
DED is caused by a disturbed tear film due to disfunction of Lacrimal glands, Meibomian glands, conjunctiva or eye lids, with secondary consequences for the cornea [4, 5]. Additionally, many systemic autoimmune diseases can cause moderate-to-severe DED [6].
Management of DED is complicated because of its multifactorial etiology associated with many mechanisms. In the Netherlands, management of DED follows a stepwise approach. The first step includes ocular lubricants of various types followed by treatment with immunosuppressive eye drops. The following step includes bandage contact lenses or even scleral contact lenses or punctum plugs. If these treatments are insufficient, SEDs are considered. SEDs offer a potential advantage over conventional therapies, as serum not only serves as a tear substitute to provide lubrication but also contains additional components to mimic natural tears more closely [7]. Although the data are heterogeneous, literature suggests that serum could be a viable treatment for DED [8,9,10].
Allogeneic SEDs are explored as an alternative to autologous due to greater standardization and uniformity. Based on several clinical studies [2, 11,12,13,14,15,16,17,18], allogeneic SEDs are now used as standard of care in countries such as Australia, Austria, Denmark, Germany, Poland, South Africa, the Netherlands, and United Kingdom.
Commonly, SED administration systems have a conventional drop size of about 50 µl, which is more than five times the volume of the tear film [19]. This amount potentially washes away most of the tear film, creating irritation and reflex tears. Application of a smaller eye drop would fit the eye, potentially leading to less damage of the tear film and creating less irritation and reflex tears. No prior data exist on the required drop size for SEDs, and it is unknown whether micro drops are as effective and user friendly as conventional drops for the treatment with serum of DED. We therefore hypothesized that a micro drop of approximately the volume of the tear film, which is 8 ± 3 µl [20], could be clinical effective.
We aimed to demonstrate the clinical effectiveness of SEDs in a large group of naïve patients with DED and that the effect is independent of the drop size, i.e., the effectiveness of micro-sized allogeneic SEDs of 7 µl and conventional-sized SEDs of 50 µl is not different.
Methods
Trial Design
The study was a prospective, randomized, non-inferiority, investigator masked, cross-over, multicenter clinical study conducted in the Netherlands. Ethics approval was obtained from the hospital Commission for Research in Humans (approval number 2017-3999). Research was performed in adherence to the Declaration of Helsinki. The study was registered at ClinicalTrials.gov under number NCT03539159. All patients gave written informed consent.
Participants
Patients were considered eligible for participation in the study if they had DED (diagnosis was based on objective and subjective complaints), suffered from punctate lesions, were not previously treated with SED and, as per the commission for research in humans, the age limit was set at 16 years. Patients were excluded if they exhibited corneal erosions more than punctate lesions, had a history of unstable herpes simplex virus (HSV) keratitis or were treated for HSV, suffered from untreated Meibomian gland disease, had an active (systemic) microbial infection (to exclude the effect of a treatment targeting (systemic) microbial infection at the same time), were currently using contact lenses, were pregnant, lactating, or intended to become pregnant in the next 3 months, or were unable or unwilling to give informed consent. The use of corticosteroids, ciclosporin, or other immunosuppressive eye drops was not allowed. The use of lubricants (artificial tears, gels, and ointments), anti-infection and glaucoma eye drops was allowed and recorded throughout the study period. Patients were instructed to maintain an interval of at least 30 min before using SEDs.
The multicenter study was conducted in an outpatient setting at the Department of Ophthalmology of the following participating hospitals in the Netherlands: Radboud University Medical Center in Nijmegen, Leiden University Medical Center, University Clinic for Ophthalmology in Maastricht, University Medical Center Utrecht, Amsterdam Medical Center Amsterdam and The Rotterdam Eye Hospital. Ophthalmologists at the participating hospitals enrolled the patients. Because no sex differences were expected for outcome measures, the ophthalmologist enrolled both male and female patients.
Intervention: Collection, Production and Use of SEDs
Collection
Collection of sera for the production of allogeneic SEDs was performed as described before [2]. In short, sera were collected from male donors conform Dutch Guideline for Donor Criteria. These sera were released when the donors returned after at least 4 months, and were again tested negative for all screening tests (quarantine period). Besides, each donation was tested for human HSV type 1 and 2, Cytomegalovirus and Varicella zoster virus because these viruses can cause significant morbidity in case of application in the eye. Donations were also labeled “Parvovirus B19-tested”, which means that in two separate blood samples from the donor, with an interval of minimal 6 months, IgG antibodies against Parvovirus B19 were detected.
Production
Production of SEDs was performed as described before [2] and as detailed in the Supplementary Material: Production of allogeneic serum eye drops (SEDs). Briefly, blood was drawn and left to clot for 6–24 h at room temperature, centrifuged twice, expressed into an empty collection container and frozen (< − 25 °C). A pool of eight thawed sera was sterile filtered using the Opticap XL5 filter assembly (MIL0000L1715633, Merck KGaA, Darmstadt, Germany), aliquoted and stored at ≤ − 25 °C. Micro-sized SEDs were produced by aliquoting undiluted serum in the mu-Drop system (mu-Drop BV, Apeldoorn, the Netherlands). Conventional-sized SEDs were produced by aliquoting undiluted serum in the Augentropf Meise eye drop systems (Heinz Meise GmbH, Schalksmühle, Germany).
Use of SEDs
Patients were instructed to thaw one mu-Drop vial immediately before use or to thaw one Meise vial for usage on the next day and to keep the vial refrigerated (at 2–6 °C) for a maximum period of 24 h or a maximum of 8 h at room temperature. Patients were instructed to apply the SEDs six times a day (six mu-Drop applicators or one Meise applicator a day), independent of the eye drop system used. However, when appropriate, lowering the dose to 3–4 times a day was allowed.
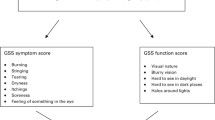
Outcome Measurements
At baseline, patient characteristics such as sex, age, diagnosis, and their current medication for treatment of dry eyes were recorded. Additionally, the OSDI (a validated scoring system that determines the degree of discomfort that a patient experiences, ranging from 0 (no symptoms) to 100 (severe dry eye symptoms all of the time)), tear break-up time (TBT) (abnormal TBT ≤ 5 s), tear production (TP) (abnormal TP ≤ 5 mm/5 min) were determined and percentage of punctate lesions (CP) was estimated. This estimation was preferred over the Oxford Grading System (OGS), since the enrolled patients typically fall in OGS category 4/5. Briefly, TBT, TP and CP were assessed in both eyes because both eyes were treated with SEDs. During each study visit, first, visual acuity was determined. Secondly, after a drop of fluorescein dye was placed in the inferior conjunctival fornix, the number of CP was estimated using a split lamp as the percentage of CP staining of the total corneal area. Thirdly, the TBT (i.e., the time in seconds between the last blink and the occurrence of the first dry spots on the cornea) was measured. Finally, the Schirmer’s test was used to measure the TP; without topical anesthesia, a strip of filtration paper was placed on the temporal conjunctiva between closed eyelids of both eyes. After 5 min, the number of millimeters of wet paper indicated the tear production of each eye.
Primary and secondary outcomes were measured at the start of the study, after 1 month of treatment with the first type of SEDs, after 1 month washout where they used the therapy as before enrollment in the study and after 1 month of treatment with the other type of SEDs. A flow figure is included in the Supplementary Material to clarify the examination points (Supplementary Figure S2: scheme of the sequence, period and treatment crossover).
The OSDI score was the primary outcome measurement. The secondary outcome measurements, assessed in both eyes, were TBT, TP and CP, as described above. During SED treatment, the ease of use of both application systems was judged by the patients daily. A score between 0 (very dissatisfied) and 10 (perfect) was recorded in a diary over both 30-day treatment periods, to evaluate progression over time.
Adverse events (AEs) and serious adverse events (SAEs) were recorded. The severity and imputability were assessed. A Safety Committee was installed to evaluate a summary of reported AEs and SAEs. All outcome measurements were entered into a database built with the electronic data capture software Castor (Castor EDC, Amsterdam, the Netherlands).
Sample Size: Power Calculation
The primary objective was to assess whether the use of micro-sized SEDs was non-inferior to conventional-sized SEDs. The micro-sized SEDs were concluded to be non-inferior if the difference in OSDI score between the micro-sized and conventional-sized SEDs was less than the predefined margin of 6. If the upper bound of the two-sided 95% confidence interval (CI) around the difference in mean improvement was < 6, non-inferiority is established.
Sample size calculation was performed via the NCSS statistical software PASS. In this software, a power analysis for a one-sided non-inferiority t test for the difference between the paired improvements in OSDI under both treatments was executed. For this calculation, an indication of the SD of this difference was required. With an average OSDI of 35 ± 12 before treatment, based on literature [21,22,23], we estimated that the improvement OSDI SD in our study has an SD of 11 under both treatments. In a cross-over design, each patient generates data for both groups, which leads to a more efficient comparison. Conservatively assuming a moderate correlation between OSDI improvements for the two treatments, expressed as a correlation coefficient of 0.10, our estimate for the SD in the difference in improvement was 14.7. Based on this, an expected difference in improvement of 0 and the predefined non-inferiority margin < 6, using a one-sided alpha of 0.025 and a power of 80%, a sample size of 50 patients was needed for analysis. To compensate for early loss-to-follow-up of patients, inclusion of four additional patients were planned. Leading to a total target sample size for inclusion of 54 patients.
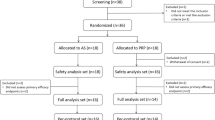
Randomization
The randomization scheme is shown in the Supplementary Figure S1: randomization scheme. Randomization was performed per hospital, with a 1-to-1 chance to be randomized in each group. The randomization list was generated in Castor, using a block size of four, by an independent clinical investigator with no involvement in the trial.
Study Conduct and Blinding
There were no interim analyses planned due to the long follow-up time and no major safety issues were suspected. Whereas patients allocated to the intervention group were aware of the allocated arm, physicians and outcome assessors were kept blinded to the allocation. Patients were instructed by independent clinical trial practitioners at the participating centers (not being the treating physician).
Statistical Analysis
Data are expressed as number of observations and percentage. Results are shown as the mean ± SD, the median with lower and upper quartiles (25th and 75th percentiles) or the estimated mean difference with a 95% confidence interval (CI), as indicated in the legends of the tables.
The intention-to-treat set (ITTS) consisted of all randomized patients in the study that met all eligible criteria. The per protocol set (PPS) consisted of all randomized patients in the study that met all eligible criteria, excluding patients with certain protocol violations. If a patient dripped SEDs less than 23 of the 30 days of the treatment period (dripped < 75% of the study days) data were excluded from the PPS only for that treatment period. The OSDI score was analyzed in the PPS (owing to the non-inferiority hypothesis). TBT, TP, and CP were analyzed in the ITTS. The analysis of the ease of use was performed based on all collected patients’ diary (total number of 52 groups). The safety analysis was performed based on the treatment that the patient actually received.
Statistical analysis was performed as briefly described below and as detailed in the Supplementary Material: Detailed statistical analysis. For the analysis of the OSDI score, a linear mixed model (LMM) for cross-over design was used and for the analysis of TBT, TP, and CP, a three-level random effects LMM for cross-over design was used, including two measurements per time point per patient (left and right eye). The ease of use of the systems was evaluated using the patients’ diaries. To compare the average score and the course over time of ease of use between both eye drop systems, a LMM was used with the optimal dependency structure, as detailed in the Supplementary Material. From the final model, the estimated marginal means over the 30 days were compared between the two treatment groups. Also, the estimated time course (slope) for both groups was compared. The incidence of AEs and SAEs was analyzed through tabulation, stratified by treatment group according to the actual received product.
All statistical analyses were performed using R Statistical Software (version 4.2.0) [24]. Important packages used for the analysis include ‘nlme’ [25] and ‘emmeans’ [26].
Results
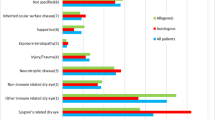
In total, 53 patients were eligible, consented, and were randomized. Forty-nine patients completed the study (Supplementary Figure S3: flow diagram showing patients inclusion, treatment, and analysis). One patient that had withdrawn during the wash-out period (due to the beneficial effects of serum treatment) was not replaced. Enrolment started in December 2018 and the last patient finished the study in May 2021. Table 1 shows the baseline patient characteristics of included patients in the study; the majority were female with an average age of 60 years. The patient population consisted of those suffering from severe dry eye disease (45%), Sjögren’s disease (36%), and graft-versus-host disease (19%). In Supplementary Table S1, the baseline ocular medication is specified per patient group. Almost all patients used lubricants and only a very small proportion of patients used glaucoma eye drops, pressure and pain reducing eye drops. The baseline OSDI score averaged 55 (± 22) and ranged from 16 (mild symptoms) to 100 (severe dry eye symptoms all of the time) indicating the inclusion of patients with mild-to-severe dry eyes. Patients showed a short tear film break-up time (median TBT was 2 s (1–4) and 87% of the patients had a TBT ≤ 5 s), low tear production (median TP was 3 mm/5 min (0–12) and 58% of the patients had a TP ≤ 5 mm/5 min) and corneal punctate lesions were present.
Primary Outcome Measurement: OSDI Score
A significant improvement in mean OSDI score was found for both micro-sized as well as for conventional-sized SEDs (Table 2). We investigated whether the use of micro-sized SEDs in this study cohort was non-inferior to conventional-sized drops. A non-significant difference between the two means (mean change for micro-sized SEDs minus mean change for conventional-sized SEDs) of − 2.60 (95% confidence interval − 9.16 to 3.97) was observed, establishing non-inferiority according to the pre-specified non-inferiority margin of 6 (p value for non-inferiority is 0.006).
Considerable variation was observed in response to SED treatment for individual patients (data not shown). Some patients exhibited a good or moderate response while others did not respond after SED treatment. Post hoc analyses were performed to investigate whether an underlying common factor could be noticed. We found that all patients diagnosed with graft-versus-host disease had a greater mean improvement in OSDI score. The results from the post hoc analysis are summarized in the Supplementary Material: Post hoc analysis.
Tear Break-Up Time, Tear Production, Percentage of Affected Surface After Staining of the Cornea
The results for the secondary ocular surface measurements are summarized in Table 3. A minor but significant improvement was observed for TBT in the conventional-sized SEDs group and for CP in both treatment groups, with no statistical difference observed between the treatment groups for TBT, TP, and CP.
Patient’s Evaluation of Ease of Use
The average ease of use of the conventional drop system (Meise system) was significantly higher as compared to the micro drop system (mu-Drop system) (Table 4). However, the ease of use, in time, gradually improved for the micro drop system as opposed to the conventional drop system, which remained unchanged (Fig. 1). Analysis of the differences in slopes shows a significant larger increase per day when using the micro drop application system compared to using the conventional drop system. An increase of the slope of 0.023 and 0.005 per day was calculated when using the micro drop system and the conventional drop system, respectively. The difference between the two treatments (0.018) was significant (95% CI 0.0046–0.0320).
Safety Evaluation
Twenty-eight AEs in 20 patients were observed during the study period. None of the reactions were considered as SAEs. Twenty-five AEs were mild, of which one was judged to be possibly related to SED treatment (astringent feeling in the right eye), ten were judged to be unlikely associated to the use of SEDs and 14 were judged to have no association. The one AE judged to be possibly related to SED treatment was reported when using the micro-sized drops. Three AEs were moderate, observed in one patient, all fully recovered, and were judged to be unlikely or not associated with the use of the SEDs.
Discussion
In this study we found, irrespective of the volume of SEDs applied, a significant subjective improvement after administration of both drop sizes SEDs (improvement in mean OSDI score). More importantly, for the first time, we show a significant improvement in objective measures (reduction in percentage of corneal punctate lesions). Non-inferiority of the 7-µl micro-sized SEDs was established when compared to conventional 50-µl sized SEDs.
For the first time, the clinical efficacy of micro-sized drops for undiluted allogeneic serum eye drops was demonstrated. Aside from a significant improvement in OSDI score, the use of SEDs also resulted in a minor but significant improvement was observed for TBT for conventional-sized SEDs and a significant reduction in the percentage of affected surface after staining of the cornea in both treatment groups. No statistical difference was observed between the treatment groups. The results are in line with other studies performed with micro drop application systems for medicinal eye drops that showed comparable, and sometimes superior, efficacy to larger drop sizes [27,28,29,30]. No prior data exist on the use of micro SEDs. During the study, patients were asked to record a diary on the ease of use of both eye drop application systems. The ease of use of the micro-sized system was significantly lower. No information was collected on where the inconvenience lies (for example in the packaging, in the activation of the system, in the administration). It is important to note that although patients’ perception of user-friendliness was inferior for the micro-sized system, the ease of use improved somewhat over time, but always was lower than for the conventional-sized drop system. Apparently, extended use, and possibly improved training could further reduce the difference in ease of use score between the two application systems. Side effects occurred in similar frequencies in both groups.
The study included patients who are normally eligible for treatment with SEDs according to current criteria, i.e., these are the ‘real-life’ patients. Post hoc analysis gives direction where future research is needed. Our study, as well as another study from our group [2], suggests that there are patients that respond, and those that do not respond to SEDs, and it is worthwhile to determine if there is an underlying common factor. For this, follow-up studies including specific patient groups are needed.
An additional benefit of single-use micro drop system is a somewhat lower risk for microbiological outgrowth as compared to the conventional system, which is allowed be stored in the refrigerator for 24 h after opening. Furthermore, the use of micro SEDs, when used less than six times per day, results in less spillage, lowering the cost, and allowing for more patients to be treated with the same amount of serum. This is of particular importance when taking into account the long-term daily treatment of patients suffering from DED with SEDs, and the scarce availability of male AB serum.
The present study has some limitations. For the patients enrolled in this study, diagnosis was based on objective and subjective complaints. Consequently, the patient population was very heterogeneous, for example with an OSDI score ranging from 16 to 100. Nonetheless, due to the cross-over design, the etiology was equally distributed. In follow-up studies, it would be of interest to differentiate patients based on the OSDI in order to determine the clinical effectiveness of SEDs in a more homogeneous patient population.
In the present study, no placebo group was included because it was concluded that it is not ethical to not treat this patient group. Furthermore, in a cross-over design, each patient generates data for both groups. By adding a washout period, patients served as their own control group. Increased patient numbers would allow for more statistical power, as well as increased understanding of the effect of SED on secondary outcomes (TBT, CP, and ST). Additionally, although only a minority of patients were using glaucoma eye drops (Table S1), this could potentially introduce a confounding factor. The patients in this study were naïve patients, e.g., never used SEDs as a treatment for their symptoms before. In a cross-over design type of study, the patients are not truly naïve in the second treatment period of the study, introducing a period effect. However, a statistical correction was performed to adjust for this. Furthermore, the present study suggests that patients with a relatively higher baseline OSDI score, such as patients suffering from graft-versus-host disease, may have a greater mean improvement in OSDI score. Given the heterogeneous patient cohort, more data should be generated to specifically identify and segregate those patient groups that do and do not benefit from SED treatment both in terms of OSDI score improvement, as well as in terms of TBT and CP.
Conclusions
We conducted the largest clinical evaluation of allogeneic SEDs in naïve patients with DED, and our study shows a large subjective improvement after administration of micro-sized and conventional-sized SEDs in OSDI. Notably, for the first time, also a significant improvement was found in the objective measures TBT and CP and a trend for improvement in TP. The clinical efficacy was considered similar for both drop sizes, as measured by the OSDI score. The upside of the micro drop system is that due to its smaller drop size, less serum is used, thereby saving valuable donor serum, which makes the system an attractive alternative.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gabriel C, Marks DC, Henschler R, Schallmoser K, Burnouf T, Koh MBC. Eye drops of human origin-current status and future needs: report on the workshop organized by the ISBT working party for cellular therapies. Vox Sang. 2023;118(4):301–9.
van der Meer PF, Verbakel SK, Honohan Á, et al. Allogeneic and autologous serum eye drops: a pilot double-blind randomized crossover trial. Acta Ophthalmol. 2021;99:837–42.
Tsubota K, Pflugfelder SC, Liu Z, et al. Defining dry eye from a clinical perspective. Int J Mol Sci. 2020;21:9271.
Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Tsubota K, Yokoi N, Watanabe H, et al. A new perspective on dry eye classification: proposal by the Asia Dry Eye Society. Eye Contact Lens. 2020;46(Suppl 1):S2-s13.
Bustamante-Arias A, Ruiz Lozano RE, Rodriguez-Garcia A. Dry eye disease, a prominent manifestation of systemic autoimmune disorders. Eur J Ophthalmol. 2022;32:3142–62.
Rauz S, Koay SY, Foot B, et al. The Royal College of Ophthalmologists guidelines on serum eye drops for the treatment of severe ocular surface disease: executive summary. Eye (London). 2018;32:44–8.
Geerling G, Maclennan S, Hartwig D. Autologous serum eye drops for ocular surface disorders. Br J Ophthalmol. 2004;88:1467–74.
Noble B, Loh R, McLennanan S, et al. Comparison of autologous serum eye drops with conventional therapy in a randomised controlled crossover trial for ocular surface disease. Br J Ophthalmol. 2004;88:647–52.
Franchini M, Cruciani M, Mengoli C, et al. Serum eye drops for the treatment of ocular surface diseases: a systematic review and meta-analysis. Blood Transfus. 2019;17:200–9.
Chiang CC, Lin JM, Chen WL, Tsai YY. Allogeneic serum eye drops for the treatment of severe dry eye in patients with chronic graft-versus-host disease. Cornea. 2007;26:861–3.
Chiang CC, Chen WL, Lin JM, Tsai YY. Allogeneic serum eye drops for the treatment of persistent corneal epithelial defect. Eye (London). 2009;23:290–3.
Harritshøj LH, Nielsen C, Ullum H, Hansen MB, Julian HO. Ready-made allogeneic ABO-specific serum eye drops: production from regular male blood donors, clinical routine, safety and efficacy. Acta Ophthalmol. 2014;92:783–6.
Marks DC, Fisher J, Mondy P, Segatchian J, Dennington PM. Serum eye drop preparation in Australia: current manufacturing practice. Transfus Apher Sci. 2015;53:92–4.
Giannaccare G, Versura P, Buzzi M, Primavera L, Pellegrini M, Campos EC. Blood derived eye drops for the treatment of cornea and ocular surface diseases. Transfus Apher Sci. 2017;56:595–604.
Hung Y, Elder MJ, Rawstron JA, Badami KG. A retrospective crossover study of autologous and allogeneic serum eye drops for the management of ocular surface disease. Transfus Med. 2019;29:69–71.
Campos E, Versura P, Buzzi M, et al. Blood derived treatment from two allogeneic sources for severe dry eye associated to keratopathy: a multicentre randomised cross over clinical trial. Br J Ophthalmol. 2020;104:1142–7.
Lomas RJ, Chandrasekar A, Macdonald-Wallis C, Kaye S, Rauz S, Figueiredo FC. Patient-reported outcome measures for a large cohort of serum eye drops recipients in the UK. Eye (London). 2021;35:3425–32.
Van Santvliet L, Ludwig A. Determinants of eye drop size. Surv Ophthalmol. 2004;49(2):197–213.
Willcox MDP, Argüeso P, Georgiev GA, et al. TFOS DEWS II tear film report. Ocul Surf. 2017;15(3):366–403.
Labetoulle M, Chiambaretta F, Shirlaw A, Leaback R, Baudouin C. Osmoprotectants, carboxymethylcellulose and hyaluronic acid multi-ingredient eye drop: a randomized controlled trial in moderate to severe dry eye. Eye (London). 2017;31:1409–16.
Perényi K, Dienes L, Kornafeld A, et al. The effect of tear supplementation with 0.15% preservative-free zinc-hyaluronate on ocular surface sensations in patients with dry eye. J Ocul Pharmacol Ther. 2017;33:487–92.
Song H, Zhang M, Hu X, et al. Correlation analysis of ocular symptoms and signs in patients with dry eye. J Ophthalmol. 2017;12:47138.
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. (2022). https://www.R-project.org/.
Pinheiro J, Bates D, R Core Team. _nlme: Linear and nonlinear mixed effects Models_. R package version 3.1-162. (2023). https://CRAN.R-project.org/package=nlme.
Lenth R. _emmeans: Estimated marginal means, aka least-squares means_. R package version 1.8.6. (2023). https://CRAN.R-project.org/package=emmeans.
Shell JW. Pharmacokinetics of topically applied ophthalmic drugs. Surv Ophthalmol. 1982;26:207–18.
Urtti A. Delivery of antiglaucoma drugs: ocular vs systemic absorption. J Ocul Pharmacol. 1994;10:349–57.
Korte JM, Kaila T, Saari KM. Systemic bioavailability and cardiopulmonary effects of 0.5% timolol eyedrops. Graefe’s Arch Clin Exp Ophthalmol. 2002;240:430–5.
Nordstrom BL, Friedman DS, Mozaffari E, Quigley HA, Walker AM. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005;140:598–606.
Acknowledgements
We thank the participants of the study. We thank Sanquin Blood Bank, The Netherlands, for excellent assistance in this study. We thank the clinical laboratory scientists, research nurses, optometrists, and physicians of the participating hospitals for their assistance.
Funding
This work was supported by Sanquin Blood Bank. Publication, including the journal’s Rapid Service Fee, was also funded by Sanquin Blood Bank.
Author information
Authors and Affiliations
Contributions
Christie Vermeulen, Pieter F. van der Meer, Dirk de Korte, and Thomas R.L. Klei contributed to the study conception and design. Data collection was performed by Catharina A. Eggink, Yanny Y.Y. Cheng, Rudy M.M.A. Nuijts, Robert P.L. Wisse, Chantal M. van Luijk, Carla Nieuwendaal and Lies Remeijer, and statistical analysis was performed by Lars L.J. van der Burg and Nan van Geloven. The first draft of the manuscript was written by Christie Vermeulen and Pieter F. van der Meer provided critical input. Robert P.L. Wisse, Pieter F. van der Meer, Dirk de Korte, and Thomas R.L. Klei helped with the revisions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Christie Vermeulen, Lars L.J. van der Burg, Nan van Geloven, Catharina A. Eggink, Yanny Y.Y. Cheng, Rudy M.M.A. Nuijts, Chantal M. van Luijk, Carla Nieuwendaal, Lies Remeijer, Pieter F. van der Meer, Dirk de Korte, Thomas R.L. Klei declare that they have no conflicts of interest to disclose. The affiliation of Dr. Robert P.L. Wisse has changed after the completion of the manuscript. His new affiliation is Xpert Clinics Oogzorg, Zeist, The Netherlands.
Ethical Approval
This study adhered to the tenets of the Declaration of Helsinki and was approved by the hospital Commission for Research in Humans (approval number 2017-3999). The study was registered at ClinicalTrials.gov under number NCT03539159. Written informed consent was obtained from each patient prior to enrollment.
Additional information
Prior Presentation: Part of this work has previously been presented at the ISBT, June 4–8, 2022 Virtual Congress (poster presentation). Poster number ISBT2022-377.
Robert P.L. Wisse: The affiliation was at the time of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Vermeulen, C., van der Burg, L.L.J., van Geloven, N. et al. Allogeneic Serum Eye Drops: A Randomized Clinical Trial to Evaluate the Clinical Effectiveness of Two Drop Sizes. Ophthalmol Ther 12, 3347–3359 (2023). https://doi.org/10.1007/s40123-023-00827-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00827-5